Abstract
Background and objectives: Thigh grafts are placed in hemodialysis patients who have exhausted all arm access sites. The goal of this study was to compare the survival, complication rates, and overall contribution of thigh grafts with arm grafts and fistulas in patients with at least one functional thigh graft during their dialysis history.
Design, setting, participants, & measurements: This longitudinal review of a prospectively acquired clinical database included 85 thigh graft recipients. The rates of survival, thrombosis, infection, and other complications were determined for a total of 268 fistulas, arm grafts, and thigh grafts placed in these patients.
Results: In this patient subset, thigh graft primary failure rate was lower than arm grafts and fistulas (3 versus 13 and 61%, respectively). Excluding primary failures, thigh grafts survived longer than both arm grafts and mature fistulas (53 versus 14 and 32%, at 3 years; 47 versus 3 and 11% at 5 years). Thigh grafts had a lower thrombosis rate than arm grafts (0.543 versus 1.457/patient-year) but similar rates of loss as a result of infection and surgical revision. In patients with previous arm accesses, thigh grafts contributed 51% of total dialysis time compared with 38 and 11% for arm grafts and fistulas.
Conclusions: Thigh grafts provide long-term, thrombosis- and infection-free dialysis access for patients with exhausted arm access sites. The decision for thigh graft placement should, therefore, be made as soon as there is evidence for unavailability of arm access sites so that catheter use can be minimized.
The primary goal of vascular access programs is to provide every dialysis patient with a permanent access and to avoid the use of tunneled central venous catheters. Toward this end, the Kidney Disease Outcomes Quality Initiative (K/DOQI) guidelines and the Fistula First initiative have emphasized the use of autogenous fistulas as the access of choice (1). Unfortunately, >50% of all fistulas fail to mature (2,3), and many patients are not candidates for fistula placement. As a result, 28% of hemodialysis patients in the United States undergo dialysis with synthetic grafts (4). Several studies have found that the longevity of mature fistulas is similar to synthetic grafts, with 2-year survival averaging 50 to 70% (5,6).
Recent trends in hemodialysis include increasing numbers of elderly patients, higher prevalence of diabetes and vascular disease, and, paradoxically, increased patient longevity (7). Within this population, is a subset of patients whose arm access sites are either unavailable for access placement as a result of poor vasculature or have been exhausted after years on dialysis. Physicians have to decide whether thigh grafts are a better alternative to catheters in these patients (8). Because grafts are preferable to catheters, it is conceivable that thigh grafts would benefit these patients. Thus, several studies have shown that the outcome of thigh grafts is similar to concurrent or historic arm grafts (9–12); however, there is a general reluctance to thigh graft placement because of the prevailing impression of poor performance or associated risks for infection or leg ischemia (9,11).
The goal of this study was to evaluate whether these objections to thigh graft use were true by comparing the survival and complication rates of thigh grafts with previous arm grafts and fistulas from the same subset of patients. We also determined the overall contribution of thigh grafts to dialysis time in patients with long dialysis vintage.
Materials and Methods
A team of nephrologists and surgeons at the Louisiana State University Health Sciences Center (LSUHSC) provides access-related care to >300 patients who undergo dialysis at 13 dialysis units in the Shreveport area. Since 1996, a vascular access database has been used to record prospectively all interventional procedures. Details of access placement, revision, and abandonment are obtained from the database and the dialysis units.
Patients undergo presurgical ultrasonographic mapping of both arms and legs to assess adequacy of vessels for access placement. For patients who are initiating dialysis, every attempt is made to create a fistula at the most distal location possible. When fistulas cannot be created because of small vessel sizes, thrombosis or occlusion of native vessels, fail to mature, or cease to function, synthetic grafts are placed in the arms. Since 2002, patients with access failure get bilateral venograms, and complicated patients with repeated fistula nonmaturation or access failure are discussed in conference with surgeons to determine the optimal access placement site. When arm access sites are unavailable or have been exhausted after failed access attempts or access abandonment, the thigh is considered as the site for graft placement. Fistulas are not placed in the thigh at this institution. After the failure of every access, the patient is reevaluated and an attempt is made to place a fistula or an arm graft, for example, using a deeper vein. Thus, it is possible for a patient to get an arm graft or a fistula after the loss of a given thigh graft.
Although there is no protocol for access monitoring at LSUHSC, nephrologists and dialysis unit nurses routinely evaluate accesses for dysfunction and refer patients for further evaluation. Clinical signs of dysfunction include low blood flows, high venous pressures; pain or excessive bleeding on dialysis; low urea reduction ratio; swelling of extremity or face, etc. Thrombosed and dysfunctional accesses are examined by the interventional staff and treated with thrombolysis and angiography. Stenosis of ≥50% is corrected by percutaneous transluminal angioplasty (PTA) or surgical revision.
Approval to review the database for research purposes was obtained from the institutional review board. Of the 674 patients with vascular accesses, a subset of 85 patients with at least one functional (used for dialysis) thigh graft was identified for this study. All information on patient demographics and access history, including all access placements, thromboses, surgical revisions, and abandonment, were extracted from the database.
Statistical Analysis
Because most of the 85 patients had more than one access placed during the previous 12 years, the generalized estimating equation model was used to test for autocorrelation of access outcomes (thrombosis and failure) within a patient. The model showed that the number of accesses in a patient as well as the number of thigh grafts in a patient was not correlated with access thrombosis or failure. We therefore used Kaplan-Meier survival analysis to compare the cumulative, thrombosis- and intervention-free survival of thigh grafts with arm grafts and fistulas. Cox proportional hazards model was used to test for significance of factors such as patient and graft characteristics on access survival.
Primary failure was defined as surgical failure, thrombosis, infection, or nonmaturation that prevented access use for hemodialysis. Access survival was defined as the difference between the dates of access placement and loss or abandonment. Reasons for access loss included thrombosis and/or failed PTA, failure to use access (e.g., inability to provide dialysis blood flows), and graft removal because of infection or pseudoaneurysm. Surgical revision was defined as jump bypass of stenosis or pseudoaneurysm, with at least one intact anastomosis of the previous graft. Surgical revision was not considered as graft loss except when both anastomoses were constructed at previously unused sites on the vasculature (i.e., a new graft was placed). Accesses were censored because of patient death, transplantation, loss to follow-up, or patency at end of study (May 15, 2008). Event rate was computed as the ratio between the number of events (thrombosis, PTA, or revision) and the duration of follow-up in patient-years. The Kruskal-Wallis test was used to compare event rates.
Results
We queried a prospective vascular access database that has been ongoing for 12 years for all patients with at least one successful thigh graft that was used for dialysis. Of a total of 674 patients with permanent accesses in the database, 85 met this criterion and contributed 268 accesses to the study. Most patients were black, 67% were female, and 41% had diabetes. Table 1 shows that thigh grafts comprised a sizable portion (38%) of the total accesses placed. Arm grafts and fistulas made up 43 and 18% of total accesses, respectively. Fistulas were included in this study so as to provide a complete access history from a patient's perspective rather than limiting the comparison to arm and thigh grafts. Most (81%) patients had only one thigh graft during their dialysis history. Patients were not older at the time of thigh graft placement but had been on dialysis, on an average, 2.9 and 2.1 years longer than at the time of fistula or arm graft placement, respectively. Women were significantly more likely to get thigh grafts compared with men; race and diabetes did not affect thigh graft placement.
Table 1.
Clinical characteristics of patients with fistulas, arm grafts, and thigh grafts
| Characteristic | Fistulas | Arm Grafts | Thigh Grafts | P |
|---|---|---|---|---|
| n (%) | 49 (18.3) | 116 (43.3) | 103 (38.4) | |
| Patient age at placement (years; mean ± SE) | 48.4 ± 1.9 | 47.6 ± 1.3 | 48.9 ± 1.4 | 0.80 |
| Time on dialysis (years; mean ± SE) | 1.2 ± 0.4 | 2.1 ± 0.3 | 4.1 ± 0.3 | <0.01 |
| Race (n [%]) | ||||
| black | 43 (17) | 112 (45) | 93 (38) | 0.07 |
| white | 6 (30) | 4 (20) | 10 (50) | |
| Gender (n [%]) | ||||
| female | 21 (13) | 72 (43) | 73 (44) | <0.01 |
| male | 28 (28) | 44 (43) | 30 (29) | |
| Diabetes (n [%]) | ||||
| yes | 17 (15) | 55 (48) | 42 (39) | 0.23 |
| no | 32 (21) | 61 (40) | 61 (40) | |
| Primary failure (including fistula nonmaturation) | 30 (61) | 15 (13) | 3 (3) | <0.01 |
Most (79%) study patients had arm accesses before thigh graft placement. Mean number of previous accesses was 2.4 (range 1.0 to 5.0). A thigh graft was the first access placed in 18 (21%) patients. A review of the ultrasonographic and surgical reports from these patients documented that arm accesses could not be placed because of the small diameter, thrombosis, or occlusion of native vessels.
Contrary to expectation, primary failure was less frequent for thigh grafts than arm grafts (3 versus 13%; P < 0.05). Only three of 103 thigh grafts failed within 30 days after placement as opposed to 15 of 116 arm grafts (Table 1). Thigh graft placement was not associated with increased postsurgical infection, limb ischemia, or other adverse events. Fistula maturation failure rate was 61%.
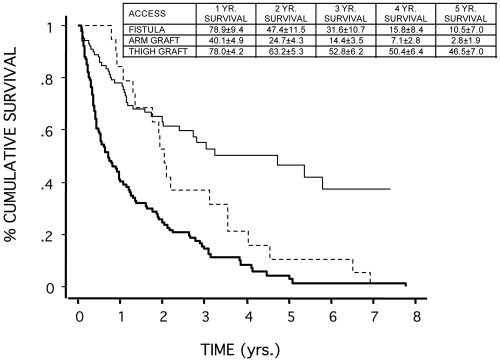
Total follow-up in the study was 393 patient-years. Figure 1 shows that when primary failures were excluded, thigh grafts had significantly better survival than arm grafts (78 versus 40% at 1 year and 53 versus 14% at 3 years). Almost half (47%) of thigh grafts were patent at 5 years compared with only 3% of arm grafts. Thigh graft survival at 1 year was similar to mature fistulas. Longitudinal follow-up for up to 8 years revealed that thigh grafts survived longer than fistulas (47 versus 11% at 5 years; P < 0.01). This divergence might have been missed in a cross-sectional study with shorter follow-up.
Figure 1.
Cumulative survival of all usable fistulas (dashed line), arm grafts (heavy line), and thigh grafts (thin line) from 85 study patients. Primary failures were excluded. Inset shows 1-, 2-, 3-, 4-, and 5-year survival rates (% survival ± SE).
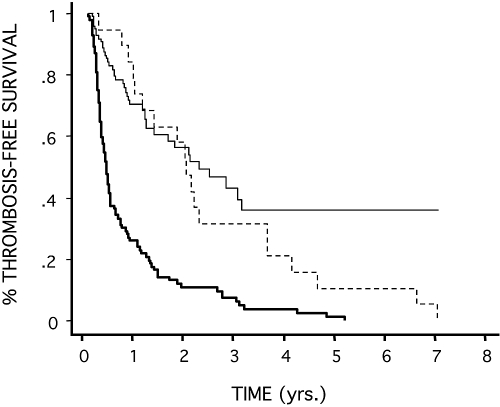
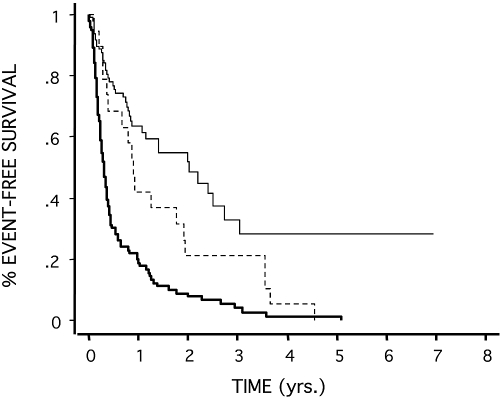
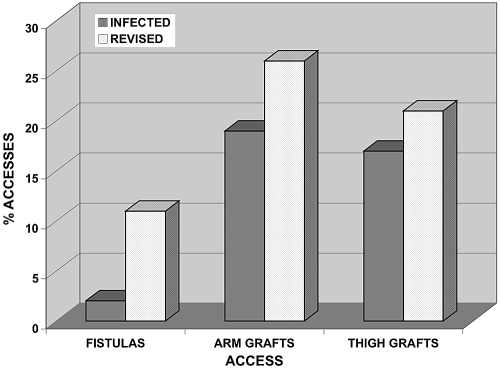
Synthetic grafts are known to be more prone to thrombosis than fistulas. In this study, we found that thigh grafts had significantly lower thrombosis, angiogram, and total PTA rates (Table 2) and, consequently, higher thrombosis-free and intervention-free survival than arm grafts and fistulas (Figures 2 and 3). Despite longer survival, thigh grafts had lower rates of infection and surgical revision as a result of stenosis and pseudoaneurysms than arm grafts (Table 2) but similar overall rates of loss (Figure 4).
Table 2.
Event rates for fistulas, arm grafts, and thigh grafts
| Parameter | Fistulas | Arm Grafts | Thigh Grafts | P |
|---|---|---|---|---|
| No. of accesses | 19 | 101 | 100 | |
| Thrombosis ratea | 0.237 | 1.457 | 0.543 | <0.01 |
| Angiogram rate | 0.693 | 0.521 | 0.338 | <0.01 |
| Total angioplasty rate | 0.930 | 1.977 | 0.881 | <0.01 |
| Revision rate | 0.099 | 0.264 | 0.157 | 0.45 |
| Infection rate | 0.020 | 0.521 | 0.100 | 0.47 |
Event rates are n/patient-year.
Figure 2.
Thrombosis-free survival of fistulas (dashed line), arm grafts (heavy line), and thigh grafts (thin line) from 85 study patients.
Figure 3.
Intervention-free survival of fistulas (dashed line), arm grafts (heavy line), and thigh grafts (thin line) from 85 study patients.
Figure 4.
Percentage of fistula, arm graft, and thigh graft loss as a result of infection and surgical revision.
Most (79%) study patients had previous arm access use; only 18 (21%) did not. Cumulative thigh graft survival was 76 versus 79% at 1 year, 62 versus 68% at 2 years, and 51 versus 59% at 3 years in patients with or without previous arm accesses, indicating that thigh graft survival was not influenced by previous access placement.
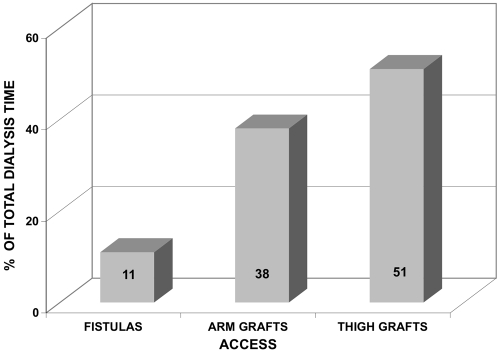
We determined the contribution of thigh grafts to the total time on dialysis. Figure 5 shows that thigh grafts accounted for 51% of total time on dialysis in patients with long dialysis vintage. There was a lot of variation from patient to patient; however, fistulas and arm grafts contributed 11 and 38% of total dialysis time, respectively.
Figure 5.
Contribution of fistulas, arm grafts, and thigh grafts to total dialysis time in patients with thigh graft placement as a result of exhaustion of all arm access sites.
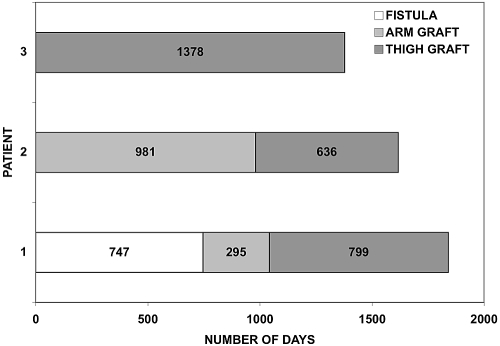
Figure 6 depicts access histories of three representative patients with >4 years of follow-up in the study. Thigh grafts made substantial contributions to dialysis regardless of previous access history. For instance, in the case of patient 1, the fistula and arm graft that preceded the thigh graft were used for 747 and 295 days, respectively. The thigh graft then extended permanent access use in this patient by 799 days. Patient 3, an example of patients with unavailable arm access sites, used the thigh graft for almost 4 years.
Figure 6.
Access histories of three representative patients in the study.
Discussion
A major finding of this study was that, in patients with exhausted arm access sites, thigh grafts had better long-term survival than fistulas and arm grafts. Low primary failure and thrombosis rates combined with fewer losses as a result of infection, and surgical revision contributed to increased thigh graft survival. This survival was independent of previous arm access placement. A consequence of this prolonged survival was that thigh grafts contributed substantially to the patient's total time on dialysis.
A major reason for thigh graft placement in this study was exhaustion of arm access sites (79% of patients). As with earlier studies, unavailability of arm access sites resulted in the thigh graft being the first access placed in 18 (21%) patients in this study (12,13). Women were more likely to get thigh grafts (Table 1), possibly because of poor arm vasculature, peripheral vascular disease, etc.
Primary failure rate was lower for thigh grafts than arm grafts (3 versus 13%). Others have reported primary failure rates of 13 to 15%, often as a result of postsurgical infection (9–12). Although we cannot explain the seemingly lower primary failure rate observed in our study, we believe that these losses are modest and should not be viewed as deterrents to thigh graft placement in patients without arm access sites.
The fistula maturation failure rate of 61% in patients who went on to get thigh grafts is similar to rates of 50 to 60% reported by others (2,3). In the setting of this longitudinal study, the high fistula maturation failure rate draws attention to patients who may not be candidates for fistula placement and/or successful maturation. These patients may be dependent on synthetic grafts as their only option for permanent access and hence at higher risk for exhaustion of arm access sites after 4 to 6 years on dialysis.
Various studies have reported that the outcome of thigh grafts was similar to concurrent or historic arm grafts (9–19). For example, Miller et al. (10) found that arm and thigh grafts had similar median cumulative survival (22.5 versus 27.6 months) in their prospective study. It is possible that the shorter follow-up of some of these studies may have caused underestimation of thigh graft survival.
A unique feature of this study was the longitudinal follow-up of up to 8 years of all patients with thigh graft placement and the inclusion of all access types in the analysis. This longitudinal follow-up was possible because of a prospectively acquired clinical database. We believe that our study enables proper estimation of fistula or thigh graft survival in comparison with the shorter lived arm grafts. Our analysis revealed that in this patient subset, thigh grafts survived longer than both arm grafts and fistulas at each of the years 1 through 5 (Figure 1). We recognize that the study patients constitute a special subset of dialysis patients who received thigh grafts because of the exhaustion or unavailability of arm access sites. Patients who had shorter dialysis vintage or longer lived fistulas and arm grafts, who did not get thigh grafts, were excluded. Although we cannot rule out the possibility that the thigh graft recipients in our study were a unique group of patients who had short-lived arm grafts and fistulas, the data show that survival and event rates of arm grafts and fistulas in our study are similar to those reported in the literature. Given that these are patients without usable arm access sites, this increased longevity of thigh grafts is of great significance.
The number of interventions that are required to maintain access patency add to the patient's morbidity and contribute to the cost of access care. Compared with arm grafts, thigh grafts had a lower thrombosis rate (1.457 versus 0.543/patient-year) and required fewer total PTAs (1.977 versus 0.881/patient-year) to maintain patency (Table 2). These rates are similar to those reported in the literature (10,11). We speculate that the larger diameter of arteries and veins in the thigh may play a role in the lower thrombosis rate observed. A consequence of the larger diameter and possibly higher blood flows associated with thigh grafts may be an increased risk for pseudoaneurysm formation. We did not find any evidence of such an increase. Despite longer survival, rates of surgical revision as a result of pseudoaneurysm formation were comparable for thigh and arm grafts in this study (Table 2, Figure 4).
This study shows that thigh grafts are not more prone to infection than arm grafts (17 versus 19%; Figure 4). Although few studies have reported thigh grafts to be at greater risk, most have reported similar values (16 to 18%) (10–18). The infection rate (which takes into account graft survival) was also within the published range of 0.10 to 0.15/patient-year (Table 2). Because the 5-year cumulative survival of thigh and arm grafts was 47 versus 3%, these findings suggest that thigh grafts provide longer infection-free dialysis.
The catheter infection rate at LSUHSC is 1.013/patient-year (unpublished observations), which is similar to rates reported in the literature (0.9 to 2.0/patient-year) (20). When infection rates of grafts and catheters are compared, our study confirms that grafts are a better option than catheters and that thigh grafts are a better option in patients without viable arm access sites.
A crucial finding in this study was the significant contribution made by thigh grafts to total dialysis time and hence to the longevity of these patients. The longitudinal study design enabled us to show that thigh grafts were used on an average for half of the patient's total time on dialysis (Figure 5) and that thigh grafts were valuable to these patients, both as the first and subsequent accesses (Figure 6). To our knowledge, no study has determined the relative contributions of the types and locations of accesses during the life of dialysis patients.
This study sheds light on the clinically important question regarding the access of choice for the patient who has exhausted upper extremity access sites or has repeated arm access failures. Surgeons and nephrologists are reluctant to place thigh grafts in these patients, opting instead for tunneled central venous catheters. The latter are recognized to be inferior to any type of vascular access because of higher rates of infection, lower blood flows resulting in inadequate dialysis, and greater risk for development of central vein stenosis and thrombosis (20,21). After repeated insertion and removal of central vein catheters in the neck, venous stenosis ensues, forcing the interventionalist to access the femoral veins. Central vein catheters in the thigh have a higher infection rate than those in the neck and an increased risk for deep vein thrombosis and may adversely influence thigh graft placement (22,23). One study reported that only 7% of patients without arm access sites and femoral catheter placements received thigh grafts. The rest remained catheter dependent (22). With this approach, valuable vascular real estate in the thigh is lost. On the basis of the results of this study, a more prudent approach would be to place a thigh graft in patients in whom repeated attempts at upper extremity access have failed. The higher primary surgical success with thigh grafts would cut down dialysis time with a catheter.
Would patients prefer a thigh graft over an arm graft if a fistula could not be constructed? Patients' views and preference for thigh grafts are currently unknown and have not been systemically evaluated. The thigh graft is cosmetically preferable than upper extremity grafts and fistulas because it is hidden from view when not in use. Patients could easily self-cannulate the thigh graft, and both arms are free for use during dialysis sessions. Conversely, cannulation of the thigh graft by dialysis personnel and the need for frequent observation of the graft during hemodialysis results in invasion of the patient's privacy. It is possible that with increased patient education on the survival and other benefits, thigh grafts may gain better acceptance.
Conclusions
This study shows that thigh grafts provide reliable, prolonged thrombosis- and intervention-free dialysis compared with both functional fistulas and arm grafts. Also, thigh grafts are not associated with increased risk for infection and pseudoaneurysm formation. Hence, we suggest that thigh grafts are an excellent option and should be considered in preference to catheters in patients who have exhausted all options for permanent access placement in both of the upper extremities.
Disclosures
None.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1..NKF K/DOQI clinical practice guidelines for vascular access. Am J Kidney Dis 48[ Suppl 1]: S248–S273, 2006 [DOI] [PubMed] [Google Scholar]
- 2..Miller PE, Carlton D, Deierhoi MH, Redden DT, Allon M: Natural history of arteriovenous grafts in hemodialysis patients. Am J Kidney Dis 36: 68–74, 2000 [DOI] [PubMed] [Google Scholar]
- 3..Dember LM, Beck GJ, Allon M, Delmez JA, Dixon BS, Greenberg A, Himmelfarb J, Vazquez MA, Gassman JJ, Greene T, Radeva MK, Braden GL, Ikizler TA, Rocco MV, Davidson IJ, Kaufman JS, Meyers CM, Kusek JW, Feldman HI, et al. : Effect of clopidogrel on early failure of arteriovenous fistulas for hemodialysis: A randomized controlled trial. JAMA 299: 2164–2171, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4..Ethier J, Mendelssohn DC, Elder SJ, Hasegawa T, Akizawa T, Aikiba T, Canaud BJ, Pisoni RL: Vascular access use and outcomes: an international perspective from the dialysis outcomes and practice patterns study. Nephrol Dial Transplant 23: 3219–3226, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5..Schild AF, Perez E, Gillaspie E, Seaver C, Livingstone J, Thibonnier A: Arteriovenous fistulae vs. arteriovenous grafts: A retrospective review of 1,700 consecutive vascular access cases. J Vasc Access 9: 231–235, 2008 [PubMed] [Google Scholar]
- 6..Snyder DC, Clericuzio CP, Stringer A, May W: Comparison of outcomes of arteriovenous grafts and fistulas at a single Veterans' Affairs medical center. Am J Surg 196: 641–646, 2008 [DOI] [PubMed] [Google Scholar]
- 7..Port FK, Orzol SM, Held PJ, Wolfe RA: Trends in treatment and survival for hemodialysis patients in the United States. Am J Kidney Dis 32[ Suppl 4]: S34–S38, 1998 [DOI] [PubMed] [Google Scholar]
- 8..Abreo KD, Ram SJ: Thigh grafts: A preferable alternative to catheters when upper extremity access sites are exhausted. Semin Dial 22: 469–471, 2009 [DOI] [PubMed] [Google Scholar]
- 9..Zibari GB, Rohr MS, Landreneau MD, Bridges RM, De Vault GA, Petty FH, Costley KJ, Brown ST, McDonald JC: Complications from permanent hemodialysis vascular access. Surgery 104: 681–686, 1988 [PubMed] [Google Scholar]
- 10..Miller CD, Robbin ML, Barker J, Allon M: Comparison of arteriovenous grafts in the thigh and upper extremities in hemodialysis patients. J Am Soc Nephrol 14: 2942–2947, 2003 [DOI] [PubMed] [Google Scholar]
- 11..Cull JD, Cull DL, Taylor SM, Carsten CG, Snyder BA, Youkey JR, Langan EM, Blackhurst DW: Prosthetic thigh arteriovenous access: Outcome with SVS/AAVS reporting standards. J Vasc Surg 39: 381–386, 2004 [DOI] [PubMed] [Google Scholar]
- 12..Akoh JA, Sinha S, Dutta S, Opaluwa AS, Lawson H, Shaw JF, Walker AJ, Rowe PA, McGonigle RJ: A 5-year audit of hemodialysis access. Int J Clin Pract 59: 847–851, 2005 [DOI] [PubMed] [Google Scholar]
- 13..Flarup S, Hadimeri H: Arteriovenous PTFE dialysis access in the lower extremity: A new approach. Ann Vasc Surg, 17: 581–584, 2003 [DOI] [PubMed] [Google Scholar]
- 14..Taylor SM, Eaves GL, Weatherford DA, McAlhany JC, Jr, Russell HE, Langan EM, 3rd: Results and complications of arteriovenous access dialysis grafts in the lower extremity: A five year review. Am Surg 62: 188–191, 1996 [PubMed] [Google Scholar]
- 15..Khadra MH, Dwyer AJ, Thompson JF: Advantages of polytetrafluoroethylene arteriovenous loops in the thigh for hemodialysis access. Am J Surg 173: 280–283, 1997 [DOI] [PubMed] [Google Scholar]
- 16..Korzets A, Ori Y, Baytner S, Zevin D, Chagnac A, Weinstein T, Herman M, Agmon M, Gafter U: The femoral artery-femoral vein polytrafluoroethylene graft: A 14-year retrospective study. Nephrol Dial Transplant 13: 1215–1220, 1998 [DOI] [PubMed] [Google Scholar]
- 17..Vogel KM, Martino MA, O'Brien SP, Kerstein MD: Complications of lower extremity arteriovenous grafts in patients with end stage renal disease. South Med J 93: 593–595, 2000 [PubMed] [Google Scholar]
- 18..Tashijan DB, Lipkowitz GS, Madden RL, Kaufman JL, Rhee SW, Berman J, Norris M, McCall J: Safety and efficacy of femoral-based hemodialysis access grafts. J Vasc Surg 35: 691–693, 2002 [DOI] [PubMed] [Google Scholar]
- 19..Englesbe MJ, Al-Holou WN, Moyer AT, Robbins J, Pelletier SJ, Magee J, Sung RS, Campbell D, Punch JD: Single center review of femoral arteriovenous grafts for hemodialysis: World J Surg 30: 171–175, 2006 [DOI] [PubMed] [Google Scholar]
- 20..Allon M: Dialysis catheter-related bacteremia: Treatment and prophylaxis. Am J Kidney Dis 44: 779–791, 2004 [PubMed] [Google Scholar]
- 21..Lee T, Barker J, Allon M: Tunneled catheters in hemodialysis patients: Reasons and subsequent outcomes. Am J Kidney Dis 46: 501–508, 2005 [DOI] [PubMed] [Google Scholar]
- 22..Maya ID, Allon M: Outcomes of tunneled femoral hemodialysis catheters: Comparison with internal jugular catheters. Kidney Int 68: 2886–2889, 2005 [DOI] [PubMed] [Google Scholar]
- 23..Falk A: Use of femoral vein as insertion site for tunneled hemodialysis catheters. J Vasc Interv Radiol 18: 217–225, 2007 [DOI] [PubMed] [Google Scholar]