Abstract
Acute kidney injury (AKI) is a common and serious condition, the diagnosis of which depends on serum creatinine measurements. Unfortunately, creatinine is a delayed and unreliable indicator of AKI. The lack of early biomarkers has crippled our ability to translate promising experimental therapies to human AKI. Fortunately, understanding the early stress response of the kidney to acute injuries has revealed a number of potential biomarkers. The discovery, translation and validation of neutrophil gelatinase-associated lipocalin, arguably the most promising novel AKI biomarker, are reviewed in this article. Neutrophil gelatinase-associated lipocalin is emerging as an excellent standalone troponin-like biomarker in the plasma and urine for the prediction of AKI, monitoring clinical trials in AKI and for the prognosis of AKI in several common clinical scenarios.
Keywords: acute kidney injury, acute renal failure, biomarkers, lipocalin, nephrotoxicity, neutrophil gelatinase-associated lipocalin
Acute kidney injury: definitions & pathophysiology
Acute kidney injury (AKI) refers to a common syndrome that results from multiple causative factors and occurs in a variety of clinical settings, with varied clinical manifestations, ranging from a minimal elevation in serum creatinine to anuric renal failure. AKI is characterized functionally by a rapid decline in the glomerular filtration rate (GFR), and biochemically by the resultant accumulation of nitrogenous wastes such as blood-urea nitrogen and creatinine. The term AKI has largely replaced acute renal failure, since the latter designation overemphasizes the failure of kidney function and fails to account for the diverse molecular, biochemical and structural processes that characterize the AKI syndrome.
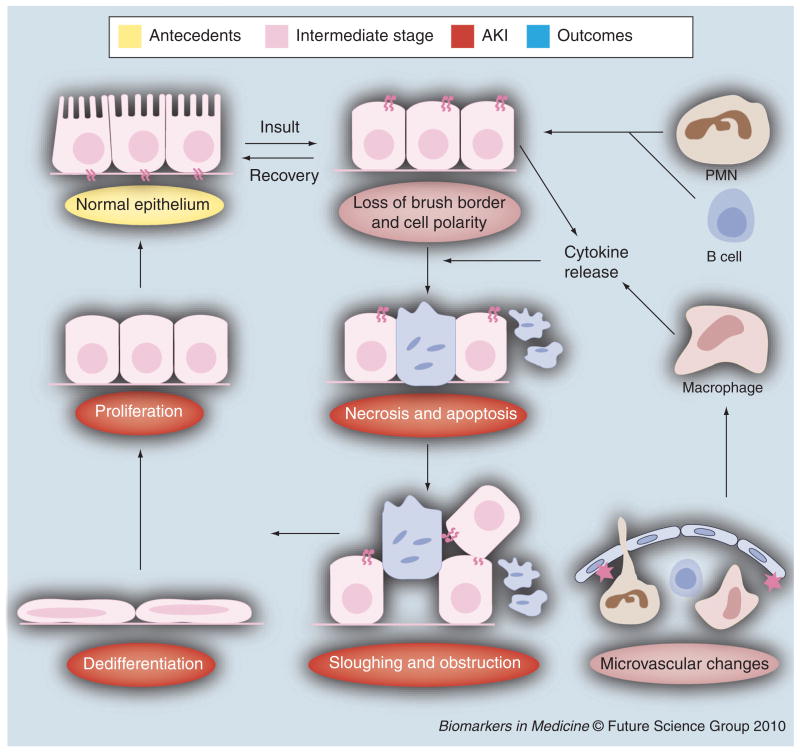
A conceptual framework of the clinical continuum of AKI has recently been proposed [1] and is illustrated in Figure 1. Color-coded circles depict the various stages in the development of AKI. Based on current diagnostic considerations, AKI (in red) is defined as a reduction in GFR, as reflected by biomarkers of functional injury such as serum creatinine. Antecedents of AKI (in yellow) include risk factors such as increasing age. Nested between the antecedents and AKI is an intermediate stage of kidney damage (in pink), representing a stage during which structural damage occurs without overt functional injury. Detection of this stage of damage requires emerging structural biomarkers as exemplified by neutrophil gelatinase-associated lipocalin (NGAL).
Figure 1. Clinical continuum of acute kidney injury.
The figure is color-coded to identify the various stages, and the biomarkers that correspond to them.
AKI: Acute kidney injury; GFR: Glomerular filtration rate; NGAL: Neutrophil gelatinase-associated lipocalin.
Appreciation of the critical significance of the intermediate-damage stage requires a brief review of the pathophysiology of AKI [2], as shown in Figure 2. The color-coded ellipses in Figure 2 reflect the reciprocal cellular changes occurring during each stage of the clinical AKI continuum. During the early-damage stage (in pink), only subtle and largely reversible changes, such as alterations in cell polarity and micro-vascular perturbations, are detected. A number of interventions applied at this stage have been successful in preventing and treating AKI in experimental studies. However, once AKI has set in (depicted in red), more severe and irreversible changes, such as cell death, desquamation and intratubular obstruction, become apparent. Although the kidney tubule cells do possess a remarkable ability to regenerate and repair after injury, most therapeutic interventions initiated in the established phase of AKI have been futile [2].
Figure 2. Pathophysiologic continuum of acute kidney injury.
The figure is color-coded to correspond to the various stages identified in Figure 1.
AKI: Acute kidney injury.
The need for a troponin-like biomarker for AKI
When a subject presents with symptoms of chest pain, the objective measurement of structural biomarkers, such as troponin, that are released from damaged myocytes can rapidly identify acute myocardial injury. This has allowed for timely therapeutic interventions and a dramatic decrease in mortality over the past few decades. By striking contrast, AKI is largely asymptomatic, and establishing the diagnosis in this increasingly common disorder currently hinges on functional biomarkers such as serial serum creatinine measurements. Unfortunately, serum creatinine is a delayed and unreliable indicator of AKI for a variety of reasons [1–4]. First, even normal serum creatinine is influenced by several nonrenal factors such as age, gender, muscle mass, muscle metabolism, medications, hydration status, nutrition status and tubular secretion. Second, a number of acute and chronic kidney conditions can exist with no increase in serum creatinine owing to the concept of renal reserve – it is estimated that over 50% of kidney function must be lost before serum creatinine rises. Third, serum creatinine concentrations do not reflect the true decrease in GFR in the acute setting, since several hours or days must elapse before a new equilibrium between the presumably steady-state production and the decreased excretion of creatinine is established. Fourth, an increase in serum creatinine represents a late indication of a functional change in GFR that lags behind important structural changes that occur in the kidney during the early-damage stage of AKI (Figures 1 & 2). Indeed, animal studies have identified several interventions that can prevent and/or treat AKI if instigated early in the course of disease, before the serum creatinine even begins to rise [2]. The lack of early biomarkers has hampered our ability to translate these promising therapies to human AKI. Also lacking are reliable methods to assess efficacy of protective or therapeutic interventions and early predictive biomarkers of drug toxicity.
A troponin-like biomarker of AKI that is easily measured, unaffected by other biological variables and capable of both early detection and risk stratification would represent a tremendous advance in the care of hospitalized patients, since the incidence of AKI in this population is estimated at a staggering 5–7% [2–6]. The incidence of AKI in the intensive care unit is even higher – approximately 25% – and carries an overall mortality rate of 50–80%. In a recent multinational study of AKI in nearly 30,000 critically ill patients, the overall prevalence of AKI requiring renal replacement therapy was 5.7% with a mortality rate of 60.3% [7]. An increase in morbidity and mortality associated with AKI has been demonstrated in a wide variety of common clinical situations, including those exposed to radiocontrast dye, cardiopulmonary bypass, mechanical ventilation and sepsis [6–9]. The negative influence of AKI on overall outcomes in critically ill patients is also well documented [10–12]. In addition, recent studies have revealed that AKI is a major risk factor for the development of nonrenal complications and it independently contributes to mortality [8]. Furthermore, the treatment of AKI represents an enormous financial burden to society, with annual AKI-associated medical expenses conservatively estimated at US$8 billion [13].
Characteristics of an ideal AKI biomarker
Desirable characteristics of AKI biomarkers are listed in Table 1. First, they should be noninvasive and easy to perform at the bedside or in a standard clinical laboratory, using easily accessible samples such as blood or urine. With respect to the sample source, the majority of AKI biomarkers described thus far have been measured in the urine. Urinary diagnostics have several advantages, including the noninvasive nature of sample collection, the reduced number of interfering proteins and the potential for the development of patient self-testing kits. However, several disadvantages also exist, including the lack of samples from patients with severe oliguria and potential changes in urinary biomarker concentration induced by hydration status and diuretic therapy. A commonly employed correction factor for urinary dilution is to express urinary biomarkers adjusted for urinary creatinine concentration in research studies. However, this correction may be inaccurate in the situation of AKI because creatinine production may be reduced in some forms of AKI [14], and both plasma and urine creatinine kinetics are significantly altered in the early phases of AKI [15].
Table 1.
Desirable characteristics of acute kidney injury biomarkers.
| Biomarker property NGAL | NGAL |
|---|---|
| Noninvasive to measure, using urine or blood | Yes |
| Rapid, inexpensive to measure | Yes |
| Results available while damage is limitable | Yes |
| Amendable to clinical assay platforms | Yes |
| Sensitive to establish an early diagnosis | Yes |
| High gradient to allow risk stratification | Yes |
| Specific to intrinsic AKI (versus prerenal) | Yes |
| Discerns AKI from chronic kidney disease | No |
| Increases proportional to degree of damage | Yes |
| Associated with a known mechanism | Yes |
| Identifies primary location of injury within kidney | Yes |
| Results predict clinical outcomes | Yes |
| Results predict efficacy of therapies | Yes |
| Results expedite drug development process | Yes |
AKI: Acute kidney injury; NGAL: Neutrophil gelatinase-associated lipocalin.
Plasma-based diagnostics have revolutionized many facets of medicine, as exemplified by the use of troponins for the early diagnosis of acute myocardial infarction. On the other hand, plasma biomarkers may be confounded by extra-renal sources as well as by subclinical changes in renal elimination. Thus, in the case of AKI, it is important and ideal to develop both urinary and plasma biomarkers.
Other desirable characteristics of clinically applicable AKI biomarkers include [16–19]:
They should be rapidly and reliably measurable using standardized clinical assay platforms;
They should be sensitive to facilitate early detection with a wide dynamic range and cut-off values that allow for risk stratification;
They should exhibit strong biomarker performance on statistical analysis, including accuracy testing by receiver-operating characteristic curves (ROC).
In addition to aiding early diagnosis and prediction, the biomarkers should be highly specific for AKI, and enable the identification of AKI subtypes and etiologies, as well as differentiating AKI from chronic kidney disease. AKI is traditionally diagnosed when the kidney’s major function (glomerular filtration) is affected, and indirectly measured by change in serum creatinine. However, prerenal factors, such as volume depletion, decreased effective circulating volume or alterations in the caliber of the glomerular afferent arterioles, all cause elevations in serum creatinine. Postrenal factors, such as urinary tract obstruction, similarly result in elevations in serum creatinine. Finally, a multitude of intrinsic renal diseases may result in an abrupt rise in serum creatinine, particularly in hospitalized patients. Other tests to distinguish these various forms of AKI, such as microscopic urine examination for casts and determination of fractional excretion of sodium, have been imprecise and have not enabled efficient clinical trial design. Availability of accurate biomarkers that can distinguish pre- and postrenal conditions from true intrinsic AKI would represent a significant advance.
Biomarkers may serve several other purposes in AKI [16–19]. Thus, they are also needed for:
Identifying the primary location of injury (proximal tubule, distal tubule, interstitium or vasculature);
Pinpointing the duration of kidney failure (AKI, chronic kidney disease or ‘acute-on-chronic’ kidney injury);
Identifying AKI etiologies (ischemia, toxins, sepsis or a combination);
Risk stratification and prognostication (duration and severity of AKI, need for renal replacement therapy, length of hospital stay and mortality);
Monitoring the response to AKI interventions.
Furthermore, AKI biomarkers may play a critical role in expediting the drug development process. The Critical Path Initiative, first issued by the US FDA in 2004, stated that “Additional biomarkers (quantitative measures of biologic effects that provide informative links between mechanism of action and clinical effectiveness) and additional surrogate markers (quantitative measures that can predict effectiveness) are needed to guide product development” [101].
Unsurprisingly, the pursuit of improved biomarkers for the early diagnosis of AKI and its outcomes is an area of intense contemporary research. For answers, we must turn to the kidney itself. Indeed, understanding the early stress response of the kidney to acute injuries has revealed a number of potential biomarkers [18–20]. The bench-to-bedside journey of NGAL, arguably the most promising novel AKI biomarker, is chronicled in this article.
Expression & structure of NGAL
Human NGAL was originally identified as a novel protein isolated from secondary granules of human neutrophils [21], and was subsequently demonstrated to be a 25-kDa protein covalently bound to neutrophil gelatinase [22]. Mature peripheral neutrophils lack NGAL mRNA expression, and NGAL protein is synthesized at the early-myelocyte stage of granulopoiesis during formation of secondary granules. NGAL mRNA is normally expressed in a variety of adult human tissues, including bone marrow, uterus, prostate, salivary gland, stomach, colon, trachea, lung, liver and kidney [23]. Several of these tissues are prone to exposure to micro-organisms, and constitutively express the NGAL protein at low levels. The promoter region of the NGAL gene contains binding sites for a number of transcription factors, including nuclear factor (NF)-κB [23]. This could explain the constitutive, as well as inducible, expression of NGAL in several of the nonhematopoietic tissues. Like other lipocalins, NGAL forms a barrel-shaped tertiary structure with a hydrophobic calyx that binds small lipophilic molecules [24]. The major ligands for NGAL are siderophores; small iron-binding molecules [25].
Functional roles of NGAL
Teleologically, NGAL comprises a critical component of innate immunity to bacterial infection. Siderophores are synthesized by bacteria to scavenge iron from the surroundings, and use specific transporters to recover the siderophore–iron complex, ensuring their iron supply. The siderophore-chelating property of NGAL therefore renders it a bacteriostatic agent [25–27]. Experimental evidence for this role is derived from mice that are genetically modified to lack the NGAL gene, which renders them more susceptible to Gram-negative bacterial infections and death from sepsis [28].
On the other hand, siderophores produced by eukaryotes participate in NGAL-mediated iron shuttling, which is critical to various cellular responses, such as proliferation and differentiation [26]. This property provides a potential molecular mechanism for the documented role of NGAL in enhancing the epithelial phenotype. During kidney development, NGAL promotes epithelial differentiation of the mesenchymal progenitors, leading to the generation of glomeruli, proximal tubules, Henle’s loop and distal tubules [29,30]. However, NGAL expression is also markedly induced in injured epithelial cells, including the kidney, colon, liver and lung. This is likely mediated via NF-κB, which is known to be rapidly activated in epithelial cells after acute injuries [31], and plays a central role in controlling cell survival and proliferation [32]. In the context of an injured mature organ, such as the kidney, the biological role of NGAL induction is one of marked preservation of function, attenuation of apoptosis and an enhanced proliferative response [33]. This protective effect is dependent on the chelation of toxic iron from extracellular environments, and the regulated delivery of siderophore and iron to intracellular sites.
Finally, NGAL is markedly induced in a number of human cancers, where it often represents a predictor of poor prognosis [34,35]. The NGAL gene is known to be induced by a number of tumor-promoting agents, including SV40 and polyoma virus, phorbol esters, the transforming factor neu, hepatocyte growth factor, retinoic acid, glucocorticoids and NF-κB [35]. The overexpressed NGAL protein binds to matrix metalloproteinase (MMP)-9, thereby preventing MMP-9 degradation and increasing MMP-9 enzyme activity. In turn, MMP-9 activity promotes cancer progression by degrading the basement membranes and extracellular matrix, liberating VEGF, and thus enabling angiogenesis, invasion and metastasis. Paradoxically, recent studies in some tumor cell lines have demonstrated that NGAL enhanced the epithelial phenotype, reduced tumor growth and suppressed metastasis – this prosurvival activity of NGAL is mediated by its ability to bind and transport iron inside the cells [34,35].
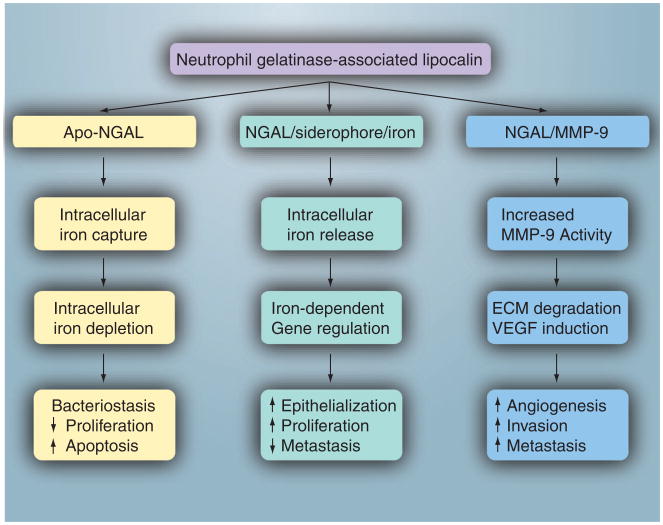
A potentially unifying hypothesis to reconcile these seemingly contradictory roles of NGAL in human biology is offered in Figure 3. Efficient mechanisms have evolved for the intracellular uptake of NGAL via receptors such as megalin, and for intracellular trafficking via endosomes. The subsequent molecular path taken by NGAL may be largely dependent on the type of molecule it is complexed with. NGAL that is devoid of siderophore and iron (holo-NGAL) rapidly scavenges intracellular iron. The resultant intra-cellular iron depletion results in a decrease in the mammalian cell’s proliferative ability and induction of apoptosis. On the other hand, when NGAL is bound to siderophore and iron, there is a rapid release of iron with regulation of iron-dependent molecular pathways, and downstream induction of proliferation and epithelial transformation. Finally, when NGAL is complexed with MMP-9 instead, there is enhancement of the active MMP-9 pool with resultant upregulation of MMP-9’s well known proangiogenic and proinvasive properties. Future studies aimed at further testing these hypotheses hold promise for advancing our understanding of NGAL biology.
Figure 3. The cellular role of neutrophil gelatinase-associated lipocalin may be dependent on the type of molecule it is complexed with.
Apo-NGAL: Neutrophil gelatinase-associated lipocalin that is devoid of siderophore or iron; ECM: Extracellular matrix.
NGAL for the prediction of AKI
Preclinical transcriptome profiling studies identified Ngal (also known as lipocalin 2 or lcn2) to be one of the most upregulated genes in the kidney very early after acute injury in animal models [36–38]. Downstream proteomic analyses also revealed NGAL to be one of the most highly induced proteins in the kidney after ischemic or nephrotoxic AKI in animal models [39–41]. The serendipitous finding that NGAL protein was easily detected in the urine soon after AKI in animal studies has initiated a number of translational studies to evaluate NGAL as a noninvasive biomarker in human AKI. In a cross-sectional study of adults with established AKI (doubling of serum creatinine) from varying etiologies, a marked increase in urine and serum NGAL was documented by western blotting when compared with normal controls [41]. Urine and serum NGAL levels correlated with serum creatinine and kidney biopsies in subjects with AKI who demonstrated intense accumulation of immunoreactive NGAL in cortical tubules, confirming NGAL as a sensitive index of established AKI in humans. A number of subsequent studies have now implicated NGAL as an early diagnostic biomarker for AKI in common clinical situations, as demonstrated in Tables 2 & 3 and detailed in the next section.
Table 2.
Urinary neutrophil gelatinase-associated lipocalin for the early prediction of acute kidney injury.
| Setting | Subjects (n) | Sensitivity | Specificity | AUC-ROC | Ref. |
|---|---|---|---|---|---|
| Cardiac surgery | 71 | 1.0 | 0.98 | 0.99 | [46] |
| Cardiac surgery | 81 | 0.73 | 0.78 | 0.8 | [49] |
| Cardiac surgery | 72 | 0.49 | 0.79 | 0.69 | [50] |
| Cardiac surgery | 426 | NR | NR | 0.61 | [51] |
| Cardiac surgery | 33 | 0.71 | 0.73 | 0.88 | [52] |
| Cardiac surgery | 196 | 0.82 | 0.9 | 0.93 | [93] |
| Cardiac surgery | 40 | 1.0 | 1.0 | 1.0 | [48] |
| Cardiac surgery | 50 | 0.93 | 0.78 | 0.96 | [53] |
| Radiocontrast administration | 100 | NR | NR | NR | [70] |
| Radiocontrast administration | 40 | 0.77 | 0.71 | 0.73 | [72] |
| Radiocontrast administration | 91 | 0.73 | 1.0 | 0.92 | [73] |
| Emergency room | 635 | 0.9 | 0.99 | 0.95 | [85] |
| Critical care | 150 | 0.77 | 0.72 | 0.78 | [77] |
| Critical care | 31 | 0.91 | 0.95 | 0.98 | [79] |
| Critical care | 451 | NR | NR | 0.71 | [80] |
| Kidney transplant | 63 | 0.9 | 0.83 | 0.9 | [64] |
| Kidney transplant | 91 | 0.77 | 0.74 | 0.81 | [65] |
AUC-ROC: Area under the receiver-operating characteristic curve; NR: Not reported.
Table 3.
Plasma neutrophil gelatinase-associated lipocalin for the early prediction of acute kidney injury.
| Setting | Subjects (n) | Sensitivity | Specificity | AUC-ROC | Ref. |
|---|---|---|---|---|---|
| Cardiac surgery | 71 | 0.7 | 0.94 | 0.91 | [46] |
| Cardiac surgery | 72 | NR | NR | 0.54 | [50] |
| Cardiac surgery | 120 | 0.84 | 0.94 | 0.96 | [92] |
| Cardiac surgery | 50 | 0.8 | 0.67 | 0.85 | [53] |
| Cardiac surgery | 100 | 0.79 | 0.78 | 0.8 | [54] |
| Radiocontrast administration | 91 | 0.73 | 1.0 | 0.91 | [73] |
| Critical care | 143 | 0.86 | 0.39 | 0.68 | [78] |
| Critical care | 307 | 0.73 | 0.81 | 0.78 | [81] |
| Critical care | 88 | 0.82 | 0.97 | 0.92 | [83] |
| Liver transplant | 59 | 0.68 | 0.8 | 0.79 | [84] |
AUC-ROC: Area under the receiver-operating characteristic curve; NR: Not reported.
NGAL in cardiac surgery-associated AKI
Operations involving cardiopulmonary bypass comprise the most frequent major surgical procedure performed in hospitals worldwide. AKI requiring dialysis represents the strongest independent risk factor for death in these patients [42]. Even a minor degree of postoperative AKI, as manifest by only a 0.2–0.3 mg/dl rise in serum creatinine from baseline, is associated with a significant increase in mortality after cardiac surgery [43]. In addition, AKI after cardiac surgery is associated with adverse outcomes, such as prolonged intensive care and hospital stay, dialysis dependency and increased long-term mortality [44]. The pathogenesis of cardiac surgery-associated AKI is complex and multifactorial [45]. It likely involves several major injury pathways that are largely non-modifiable. Mechanisms include ischemia-reperfusion injury (caused by low mean arterial pressures and loss of pulsatile renal blood flow), exogenous toxins (caused by contrast media, nonsteroidal anti-inflammatory drugs and aprotinin), endogenous toxins (caused by iron released from hemolysis), and inflammation and oxidative stress (from contact with bypass circuit, surgical trauma and intrarenal inflammatory responses). These mechanisms of injury are likely to be active at different times with different intensities and may act synergistically. There is a dearth of randomized controlled trials for the prevention or treatment of cardiac surgery-associated AKI, caused, at least in part, by the paucity of early predictive biomarkers. In several prospective studies in children who underwent elective cardiac surgery, AKI (defined as a 50% increase in serum creatinine) occurred 1–3 days after surgery [46–48]. By contrast, NGAL measurements by ELISA revealed a tenfold or more increase in the urine and plasma, within 2–6 h of the surgery, in those who subsequently developed AKI. Both urine and plasma NGAL were excellent independent predictors of AKI, with an area under the curve (AUC) of the ROC of over 0.9 for the 2–6 h urine and plasma NGAL measurements. These findings have now been confirmed in prospective studies of adults who developed AKI after cardiac surgery, and in whom urinary and/or plasma NGAL was significantly elevated by 1–3 h after the operation [49–56]. However, the AUC-ROCs for the prediction of AKI have been rather disappointing when compared with pediatric studies, and have ranged widely from 0.61 to 0.96. The somewhat inferior performance in adult populations may be reflective of confounding variables such as older age groups, pre-existing kidney disease, prolonged bypass times, chronic illness and diabetes [50,57]. The predictive performance of NGAL also depends on the definition of AKI employed, as well as on the severity of AKI [56]. For example, the predictive value of plasma NGAL postcardiac surgery was higher for more severe AKI (increase in serum creatinine over 50%; mean AUC-ROC 0.79) compared with less severe AKI (increase in serum creatinine over 25%; mean AUC-ROC 0.65). Similarly, the discriminatory ability of NGAL for AKI increased with increasing severity as classified by risk of renal dysfunction; injury to the kidney; failure of kidney function; loss of kidney function; and end-stage kidney disease (RIFLE) criteria [58]. Thus, the AUC-ROC improved progressively for discrimination of R (0.72), I (0.79) and F (0.80) category of AKI [56]. Furthermore, the predictive power of urinary NGAL for AKI after cardiac surgery varied with baseline renal function, with optimal discriminatory performance in patients with normal preoperative renal function [59]. Despite these numerous potential variables, a recent meta-analysis of published studies in all patients after cardiac surgery revealed an overall AUC-ROC of 0.78 for prediction of AKI, when NGAL was measured within 6 h of initiation of cardiopulmonary bypass and AKI was defined as a greater than 50% increase in serum creatinine [60].
NGAL in AKI after kidney transplantation
Acute kidney injury due to ischemia-reperfusion occurs, to some extent, almost invariably in deceased donor renal allografts, and even in some live donor transplants, often resulting in varying degrees of early renal dysfunction [61]. AKI leading to delayed graft function (DGF) complicates 4–10% of live donor and 5–50% of deceased donor kidney transplants. In addition to the well known complications of AKI and dialysis, DGF predisposes the graft to both acute and chronic rejection, is an independent risk factor for suboptimal graft function at 1 year post-transplant, and increases the risk of chronic allograft nephropathy and graft loss [62].
Neutrophil gelatinase-associated lipocalin has been evaluated as a biomarker of AKI and DGF (defined as dialysis requirement within the first postoperative week) in patients undergoing kidney transplantation. Protocol biopsies of kidneys obtained 1 h after vascular anastomosis revealed a significant correlation between NGAL staining intensity in the allograft and the subsequent development of DGF [63]. In a prospective multicenter study of children and adults, urine NGAL levels in samples collected on the day of transplant identified those who subsequently developed DGF (which typically occurred 2–4 days later), with an AUC-ROC of 0.9 [64]. This has now been confirmed in a larger multicenter cohort, in which urine NGAL measured within 6 h of kidney transplantation predicted subsequent DGF with an AUC-ROC of 0.81 [65]. Plasma NGAL measurements have also been correlated with DGF following kidney transplantation from donors after cardiac death [66].
NGAL in contrast-induced AKI
Studies of large adult cohorts have revealed that contrast-induced AKI is the third most common cause of hospital-acquired AKI, accounting for approximately 11% of cases [67]. Approximately half of these cases are in subjects undergoing cardiac catheterization and angiography, and approximately a third follow computed tomography [68]. Technological advances in diagnostic and interventional imaging techniques have contributed to an ever-increasing number of individuals being exposed to iodinated contrast media [69]. Progress in the development of strategies towards prevention and early treatment of cervical intraepithelial neoplasia has been hampered by several factors, including the inability to accurately identify high-risk patients and the paucity of early predictive biomarkers.
Several investigators have examined the role of NGAL as a predictive biomarker of AKI following contrast administration [70–73]. In a prospective study of children undergoing elective cardiac catheterization with contrast administration, both urine and plasma NGAL predicted contrast-induced nephropathy (defined as a 50% increase in serum creatinine from baseline) within 2 h after contrast administration, with an AUC-ROC of 0.91–0.92 [73]. In several studies of adults administered contrast, an early rise in both urine (4 h) and plasma (2 h) NGAL were documented, in comparison with a much later increase in plasma cystatin C levels (8–24 h after contrast administration), providing further support for NGAL as an early biomarker of contrast nephropathy [70–72]. A recent meta-analysis revealed an overall AUC-ROC of 0.894 for prediction of AKI, when NGAL was measured within 6 h after contrast administration and AKI was defined as an increase in serum creatinine of over 25% [60].
NGAL in AKI in the critical care setting
Acute kidney injury is a frequent complication in critically ill patients, and results in a hospital mortality of 45–60% [7,74]. This patient population is extremely heterogeneous, and the etiology and timing of AKI is often unclear. Up to 60% of patients may have already sustained AKI on admission to the intensive care unit [75]. Sepsis accounts for 30–50% of all AKI encountered in critically ill patients, and generally portends a poorer prognosis with lower survival [76]. Other etiologies for AKI in this setting include exposure to nephrotoxins, hypotension, kidney ischemia, mechanical ventilation and multiorgan disease. Each of these etiologies are associated with distinct mechanisms of injury that are likely to be active at different times with different intensities and may act synergistically.
Urine and plasma NGAL measurements have been demonstrated to represent early biomarkers of AKI in a heterogeneous pediatric intensive care setting, being able to predict this complication approximately 2 days prior to the rise in serum creatinine, with high sensitivity and AUC-ROCs of 0.68–0.78 [77,78]. Several studies have also examined plasma and urine NGAL levels in critically ill adult populations [79–84]. Urine NGAL, obtained on admission, predicted subsequent AKI in multitrauma patients with an outstanding AUC-ROC of 0.98 [79]. However, in a more mixed population of all critical care admissions, the urine NGAL on admission was only moderately predictive of AKI with an AUC-ROC of 0.71 [80]. In studies of adult intensive care patients, plasma NGAL concentrations on admission constituted a very good to outstanding biomarker for development of AKI within the next 2 days, with AUC-ROC ranges of 0.78–0.92 [81,83]. In subjects undergoing liver transplantation, a single plasma NGAL level obtained within 2 h of reperfusion was highly predictive of subsequent AKI, with an AUC-ROC of 0.79 [84]. Finally, in a study of adults in the emergency department setting, a single measurement of urine NGAL at the time of initial presentation predicted AKI with an outstanding AUC-ROC of 0.95 and reliably distinguished prerenal azotemia from intrinsic AKI, and from chronic kidney disease [85]. Thus, NGAL is a useful early AKI marker that predicts development of AKI, even in heterogeneous groups of patients with multiple comorbidities and with unknown timing of kidney injury. However, it should be noted that patients with septic AKI display the highest concentrations of both plasma and urine NGAL when compared with those with nonseptic AKI [80], a confounding factor that may add to the heterogeneity of the results in the critical care setting. A recent meta-analysis revealed an overall AUC-ROC of 0.73 for prediction of AKI, when NGAL was measured within 6 h of clinical contact with critically ill subjects, and AKI was defined as a greater than 50% increase in serum creatinine [60].
NGAL for monitoring trials in AKI
Owing to its high predictive properties for AKI, NGAL is also emerging as an early biomarker in interventional trials. For example, a reduction in urine NGAL has been employed as an outcome variable in clinical trials demonstrating the improved efficacy of a modern hydroxyethylstarch preparation over albumin or gelatin in maintaining renal function in cardiac surgery patients [86–88]. Similarly, the response of urine NGAL was attenuated in adult cardiac surgery patients who experienced a lower incidence of AKI after sodium bicarbonate therapy when compared with sodium chloride [89]. In addition, urinary NGAL levels have been utilized to document the efficacy of a miniaturized cardiopulmonary bypass system in the preservation of kidney function when compared with standard cardiopulmonary bypass [90]. Furthermore, adults who developed AKI after aprotinin use during cardiac surgery, displayed a dramatic rise in urine NGAL in the immediate postoperative period, attesting to the potential use of NGAL for the prediction of nephrotoxic AKI [91]. Unsurprisingly, NGAL measurements, as an outcome variable, are currently included in several ongoing clinical trials formally listed in ClinicalTrials.gov. The approach of using NGAL as a trigger to initiate and monitor novel therapies, and as a safety biomarker when using potentially nephrotoxic agents, is expected to increase. It is also hoped that the use of predictive and sensitive biomarkers, such as NGAL, as end points in clinical trials will result in a reduction in required sample sizes, and hence, the cost incurred.
NGAL for the prognosis of AKI
A number of studies have demonstrated the utility of early NGAL measurements for predicting the severity and clinical outcomes of AKI. In children undergoing cardiac surgery, early postoperative plasma NGAL levels strongly correlated with duration and severity of AKI, length of hospital stay and mortality [92]. In a similar cohort, early urine NGAL levels highly correlated with duration and severity of AKI, length of hospital stay, dialysis requirement and death [93]. In a multicenter study of children with diarrhea-associated hemolytic uremic syndrome, urine NGAL, obtained early during the hospitalization, predicted the severity of AKI and dialysis requirement with high sensitivity [94]. Early urine NGAL levels were also predictive of duration of AKI (AUC-ROC: 0.79) in a heterogeneous cohort of critically ill pediatric subjects [77].
In adults undergoing cardiopulmonary bypass, those who subsequently required renal replacement therapy were found to have the highest urine NGAL values soon after surgery [49–56]. Similar results were documented in the adult critical care setting [79–85]. Collectively, the published studies revealed an overall AUC-ROC of 0.78 for the prediction of subsequent dialysis requirement, when NGAL was measured within 6 h of clinical contact [60]. Furthermore, a number of studies conducted in the cardiac surgery and critical care populations have identified early NGAL measurements as a very good mortality marker [49–51,80,81,85], with an overall AUC-ROC of 0.71 in these heterogeneous populations [58]. In addition, there is now evidence for the utility of subsequent NGAL measurements in critically ill adults with established AKI. Serum NGAL measured at the inception of renal replacement therapy was an independent predictor of 28-day mortality, with an AUC of 0.74 [95]. Finally, in kidney transplant patients undergoing either protocol biopsies or clinically indicated biopsies, urine NGAL measurements were found to be predictive of tubulitis or other tubular pathologies [96], raising the possibility that NGAL represents a noninvasive screening tool for the detection of tubulointerstitial disease in the early months following kidney transplantation.
Clinical platforms for NGAL measurement
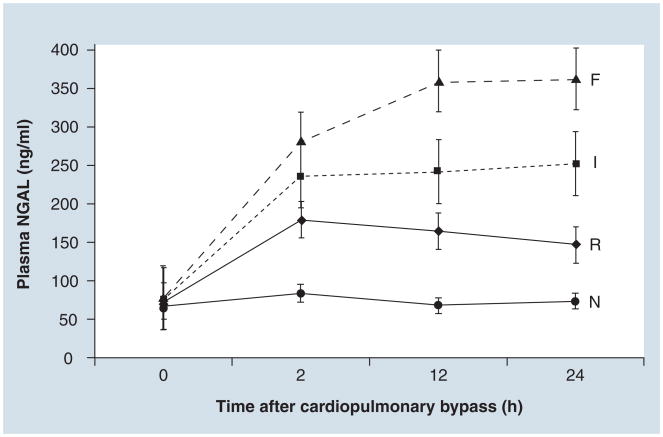
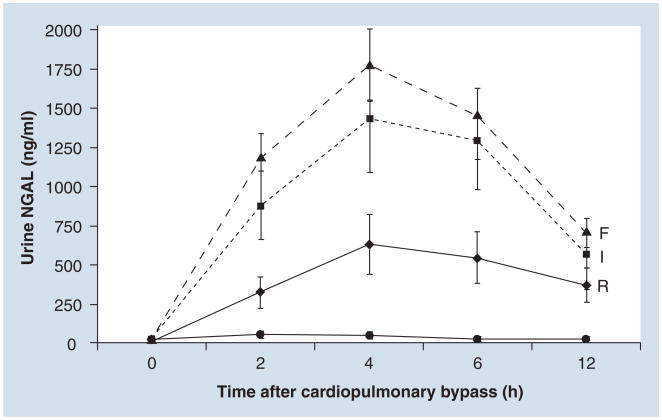
The majority of NGAL results described in the literature have been obtained using research-based ELISA assays that are currently available from commercial sources such as Bioporto (Gentofte, Denmark) and R&D Systems (MN, USA). These assays are accurate, but are not practical in the clinical setting. In these regards, a major advance has been the development of a point-of-care kit for the clinical measurement of plasma NGAL (Triage® NGAL device, Biosite Inc., CA, USA). In children undergoing cardiac surgery, the increase in plasma NGAL levels measured by the Triage device at various time points after cardiopulmonary bypass was proportional to the severity of AKI as classified by the RIFLE critieria (Figure 4). In terms of diagnostic accuracy, the 2 h plasma NGAL measurement demonstrated an AUC of 0.96, sensitivity of 0.84, and specificity of 0.94 for prediction of AKI using a cutoff value of 150 ng/ml [92]. Several additional publications have now confirmed the utility and accuracy of the Triage NGAL device in critically ill adults [54–56,81,83]. The assay is facile, with quantitative results available in 15 min, requires only microliter quantities of whole blood or plasma, and is currently being tested in multicenter trials for further validation. In addition, a urine NGAL immunoassay has been developed for a clinical platform (ARCHITECT® analyzer, Abbott Diagnostics, Abbott Park, IL, USA). In children undergoing cardiac surgery, the increase in urine NGAL levels determined by ARCHITECT analyzer at various time points after cardiopulmonary bypass was also proportional to the severity of AKI as classified by RIFLE criteria (Figure 5). The 2 h urine NGAL demonstrated an AUC of 0.95, sensitivity of 0.79 and specificity of 0.92 for prediction of AKI, using a cutoff value of 150 mg/ml [93]. This assay is also easy to perform as it has no manual pretreatment steps, a first result available within 35 min and requires only 150 μl of urine. A recent evaluation of the ARCHITECT urine NGAL assay demonstrated good precision, sensitivity and lot-to-lot reproducibility, and good short-term 2–8°C sample stability [97]. However, long-term storage requires a temperature of −70°C for optimal sample stability [97,98]. This assay is also currently undergoing multicenter validation in several clinical populations.
Figure 4. Plasma neutrophil gelatinase-associated lipocalin levels measured by Triage® neutrophil gelatinase-associated lipocalin device at various time points after cardiopulmonary bypass in subjects with no acute kidney injury (N), or with acute kidney injury (R, I or F) stratified by RIFLE criteria.
NGAL: Neutrophil gelatinase-associated lipocalin.
Post hoc analysis of data from reference [92].
Figure 5. Urine neutrophil gelatinase-associated lipocalin levels measured by ARCHITECT® analyzer at various time points after cardiopulmonary bypass in subjects with no acute kidney injury (N), or with acute kidney injury (R, I or F) stratified by RIFLE criteria.
NGAL: Neutrophil gelatinase-associated lipocalin.
Post hoc analysis of data from [93].
Biologic sources of urinary & plasma NGAL
The genesis and sources of plasma and urinary NGAL following AKI require further clarification. Although plasma NGAL is freely filtered by the glomerulus, it is largely reabsorbed in the proximal tubules by efficient megalin-dependent endocytosis [26]. Direct evidence for this notion is derived from systemic injection of labeled NGAL, which becomes enriched in the proximal tubule but does not appear in the urine of animals [41]. Thus, any urinary excretion of NGAL is likely only when there is a concomitant proximal renal tubular injury that precludes NGAL reabsorption and/or increases de novo NGAL synthesis. However, gene expression studies in AKI have demonstrated a rapid and massive upregulation of NGAL mRNA in the distal nephron segments – specifically in the thick ascending limb of Henle’s loop and the collecting ducts [26]. The resultant synthesis of NGAL protein in the distal nephron and secretion into the urine appears to comprise the major fraction of urinary NGAL. Supporting clinical evidence is provided by the consistent finding of a high fractional excretion of NGAL reported in human AKI studies [26,41]. The over-expression of NGAL in the distal tubule and rapid secretion into the lower urinary tract is in accord with its teleological function as an antimicrobial strategy. It is also consistent with the proposed role for NGAL in promoting cell survival and proliferation, given the recent documentation of abundant apoptotic cell death in distal nephron segments in several animal and human models of AKI [99,100].
With respect to plasma NGAL, the kidney itself does not appear to be a major source. In animal studies, direct ipsilateral renal vein sampling after unilateral ischemia indicates that the NGAL synthesized in the kidney is not introduced efficiently into the circulation, but is abundantly present in the ipsilateral ureter [26]. However, it is now well known that AKI results in a dramatically increased NGAL mRNA expression in distant organs [101], especially the liver and lungs, and the overexpressed NGAL protein released into the circulation may constitute a distinct systemic pool. Additional contributions to the systemic pool in AKI may derive from the fact that NGAL is an acute-phase reactant and may be released from neutrophils, macrophages and other immune cells. Furthermore, any decrease in GFR resulting from AKI would be expected to decrease the renal clearance of NGAL, with subsequent accumulation in the systemic circulation. The relative contribution of these mechanisms to the rise in plasma NGAL after AKI remains to be determined.
Limitations of NGAL as an AKI biomarker
Clearly, NGAL represents a novel predictive biomarker for AKI and its outcomes. However, NGAL appears to be most sensitive and specific in homogeneous patient populations with temporally predictable forms of AKI. Published studies have also identified age as an effective modifier of NGAL’s performance as an AKI biomarker, with better predictive ability in children (overall AUC-ROC 0.93) than in adults (AUC-ROC 0.78). Plasma NGAL measurements may be influenced by a number of coexisting variables including chronic kidney disease, chronic hypertension, systemic infections, inflammatory conditions, anemia, hypoxia and malignancies [34,35,102–104]. In the chronic kidney disease population, NGAL levels correlate with the severity of renal impairment. However, it should be noted that the increase in plasma NGAL in these situations is generally much less than those typically encountered in AKI. In addition, NGAL has been demonstrated to be expressed in human atherosclerotic plaques [105], as well as abdominal aortic aneurysms [106], which may also influence plasma NGAL measurements.
There is emerging literature suggesting that urine NGAL is also a marker of chronic kidney disease and its severity [3]. In this population, urine NGAL levels are elevated and significantly correlated with serum creatinine, GFR and proteinuria [107–109]. Urine NGAL has also been demonstrated to represent an early biomarker for the degree of chronic injury in patients with IgA nephropathy [110] and lupus nephritis [111–113], and may be increased in urinary tract infections [114]. However, the levels of urine NGAL in these situations are significantly blunted compared with that typically measured in AKI.
Limitations of studies examining NGAL as an AKI biomarker
Despite the optimism in the field, there are important limitations that exist in the published NGAL literature that must be acknowledged. First, the majority of studies reported were from single centers that enrolled small numbers of subjects. Validation of the published results in large multicenter studies will be essential. Second, most studies reported to date, did not include patients with chronic kidney disease. This is problematic, not only because it excludes a large proportion of subjects who frequently develop AKI in clinical practice, but also because chronic kidney disease, in itself, can result in increased concentrations of NGAL, thereby representing a confounding variable. Third, many studies reported only statistical associations (odds ratio or relative risk), but did not report sensitivity, specificity and AUCs for the diagnosis of AKI; these are essential to determine the accuracy of the biomarker. Fourth, only a few studies, with a relatively small number of cases, have investigated biomarkers for the prediction of AKI severity, morbidity and mortality – results of testing NGAL as a predictor of hard clinical outcomes in large multicenter studies are anxiously awaited. Finally, the definition of AKI in the published studies varied widely, but was based largely on elevations in serum creatinine, raising the conundrum of using a flawed outcome variable to analyze the performance of a novel assay. The studies of biomarkers such as NGAL for the diagnosis of AKI may have yielded different results had there been a true ‘gold standard’ for AKI. Instead, using AKI as defined by a change in serum creatinine, sets up the biomarker assay for lack of accuracy due to either false positives (true tubular injury but no significant change in serum creatinine) or false negatives (absence of true tubular injury, but elevations in serum creatinine caused by prerenal effects or any of a number of confounding variables that affect this measurement). In future studies, it will be crucial to understand the clinical outcomes of subjects who may be prone to AKI and are ‘NGAL-positive’ but ‘creatinine-negative’, since this will determine whether the biomarker is overtly sensitive. Since the gold standard for true AKI (tissue biopsy) is highly unlikely to be feasible, it is vital that future studies are large enough, and demonstrate the association between biomarkers and hard outcomes, such as dialysis, cardiovascular events and death, and that randomization to a treatment for AKI, based on high biomarker levels, results in an improvement in kidney function and a reduction of clinical outcomes. This should be the next priority in the field.
Future perspective
As an AKI biomarker, NGAL has successfully passed through the preclinical assay development and initial clinical testing stages of the biomarker development process. It has now entered the prospective screening stage, facilitated by the development of commercial tools for the measurement of NGAL in large populations and across different laboratories; but will any single biomarker suffice in AKI? In addition to early diagnosis and prediction, it would be desirable to identify biomarkers capable of discerning AKI subtypes, identifying etiologies, predicting clinical outcomes, allowing for risk stratification and monitoring the response to interventions. In order to obtain all of this desired information, a panel of validated biomarkers may be needed. The current status of NGAL, as an AKI biomarker for these indications, has been chronicled in this article. Other AKI biomarker candidates may include IL-18, kidney injury molecule-1, cystatin C and liver-type fatty-acid binding protein, to name a few [2–6]. The availability of a panel of AKI biomarkers could further revolutionize renal and critical care. However, such idealistic thinking must be tempered with the enormous technical and fiscal issues surrounding the identification, validation, commercial development and acceptance of multimarker panels. Deriving from the recent cardiology literature, a clinically useful biomarker should be easily measurable at a reasonable cost and with short turnaround times; provide information that is not already available from clinical assessment; and aid in medical decision making [115]. In this respect, as a stand-alone biomarker, troponin provides excellent diagnostic and prognostic information in acute coronary syndromes and acute decompensated heart failure [116]. If the current prospective multicenter studies of NGAL measurements with standardized laboratory platforms provide promising results, we may have already closed in on the ‘renal troponin’.
Executive summary.
Acute kidney injury is an increasingly common & serious clinical condition
Acute kidney injury (AKI) afflicts 5–7% of all hospitalized patients, and up to 30% of critically ill subjects.
The mortality rate of critically ill subjects with AKI remains very high – over 50%.
Serum creatinine is a delayed biomarker of kidney dysfunction in the acute setting.
Characteristics of an ideal AKI biomarker
Noninvasive, easy to perform, rapid turnaround time, able to utilize standardized clinical platforms.
High sensitivity and specificity for early detection.
Wide dynamic range and cutoff values to allow for risk stratification.
Can identify the etiology of AKI.
Prognosticate (predict need for dialysis, length of hospital stay and mortality).
Discovery of neutrophil gelatinase-associated lipocalin as an AKI biomarker
Preclinical transcriptome profiling in a number of AKI models revealed neutrophil gelatinase-associated lipocalin (NGAL) to be one of the most robustly upregulated genes in the kidney post-injury.
Downstream proteomic analyses revealed NGAL to be a highly induced protein in experimental AKI.
NGAL was easily and rapidly detected in the urine in animal models of AKI.
NGAL for the prediction of human AKI
Plasma and urine NGAL are excellent biomarkers for the early prediction of AKI following defined clinical injuries such as cardiopulmonary bypass, contrast administration and kidney transplantation.
Plasma and urine NGAL are excellent biomarkers for the early prediction of AKI, even in heterogeneous clinical situations where the timing of kidney injury is unknown, such as in the critical care or emergency settings.
NGAL levels can discriminate between true AKI and prerenal azotemia in unselected patients presenting for emergency care.
NGAL as an efficacy biomarker in AKI
Reduction in NGAL levels are becoming increasingly used as an efficacy marker in trials for the prevention and/or treatment of AKI.
NGAL is a promising biomarker for the prediction of and monitoring for nephrotoxic AKI.
NGAL for the prognosis of human AKI
Plasma and urine NGAL levels increase early in proportion to the duration and severity of the ensuing AKI in a variety of clinical scenarios.
Early plasma and urine NGAL concentrations are predictive of dialysis requirement, mortality and length of hospital stay in a variety of clinical AKI situations.
Clinical platforms for NGAL measurement
The Triage® NGAL Device measures plasma NGAL as a point-of-care platform.
The ARCHITECT® analyzer measures urine NGAL as a clinical laboratory platform.
Limitations of NGAL as an AKI biomarker
Plasma NGAL may be influenced by coexisting variables such as chronic kidney disease, systemic infections, systemic inflammatory conditions and malignancies.
Urine NGAL may be influenced by coexisting variables such as chronic kidney disease, renal inflammation and urinary tract infections.
Conclusion
NGAL is emerging as an excellent standalone troponin-like biomarker in the plasma and urine for the prediction of AKI and its clinical outcomes.
Footnotes
For reprint orders, please contact: reprints@futuremedicine.com
Financial & competing interests disclosure
Studies cited in this review that were performed by the author’s laboratory were supported by grants from the NIH (R01 DK53289, RO1 DK069749 and R21 DK070163). P Devarajan is a co-inventor on NGAL patents. Biosite® Inc. (CA, USA) has signed an exclusive licensing agreement with Cincinnati Children’s Hospital for developing plasma NGAL as a biomarker of acute renal failure. Abbott Diagnostics has signed an exclusive licensing agreement with Cincinnati Children’s Hospital for developing urine NGAL as a biomarker of acute renal failure. P Devarajan has received honoraria for speaking assignments from Biosite® Inc. and Abbott Diagnostics (IL, USA). The author has no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
Bibliography
Papers of special note have been highlighted as:
▪ of interest
▪▪ of considerable interest
- 1▪.Murray PT, Devarajan P, Level AS, et al. A framework and key research questions in AKI diagnosis and staging in different environments. Clin J Am Soc Nephrol. 2008;3:864–868. doi: 10.2215/CJN.04851107. Novel approach to clinical staging of acute kidney injury (AKI) [DOI] [PubMed] [Google Scholar]
- 2▪▪.Devarajan P. Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol. 2006;17:1503–1520. doi: 10.1681/ASN.2006010017. Comprehensive review of the pathophysiologic mechanisms that underlie AKI. [DOI] [PubMed] [Google Scholar]
- 3.Nickolas TL, Barasch J, Devarajan P. Biomarkers in acute and chronic kidney disease. Curr Opin Nephrol Hypertens. 2008;17:127–132. doi: 10.1097/MNH.0b013e3282f4e525. [DOI] [PubMed] [Google Scholar]
- 4.Devarajan P. Neutrophil gelatinase-associated lipocalin (NGAL): a new marker of kidney disease. Scand J Clin Lab Invest. 2008;68:89–94. doi: 10.1080/00365510802150158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5▪▪.Devarajan P. Neutrophil gelatinase-associated lipocalin – an emerging troponin for kidney injury. Nephrol Dial Transplant. 2008;23(12):3737–3743. doi: 10.1093/ndt/gfn531. Comprehensive review of neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker of AKI, in comparison with other novel biomarkers. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parikh CR, Devarajan P. New biomarkers of acute kidney injury. Crit Care Med. 2008;36(4 Suppl):159–165. doi: 10.1097/CCM.0b013e318168c652. [DOI] [PubMed] [Google Scholar]
- 7.Uchino S, Kellum JA, Bellomo R, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005;294(7):813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 8.Chertow GM, Soroko SH, Paganini EP, et al. Mortality after acute renal failure: models for prognostic stratification and risk adjustment. Kidney Int. 2006;70:1120–1126. doi: 10.1038/sj.ki.5001579. [DOI] [PubMed] [Google Scholar]
- 9.Hoste EA, Kellum JA. RIFLE criteria provide robust assessment of kidney dysfunction and correlate with hospital mortality. Crit Care Med. 2006;34(7):2016–2017. doi: 10.1097/01.CCM.0000219374.43963.B5. [DOI] [PubMed] [Google Scholar]
- 10.Radhakrishnan J, Kiryluk K. Acute renal failure outcomes in children and adults. Kidney Int. 2006;69(1):17–19. doi: 10.1038/sj.ki.5000094. [DOI] [PubMed] [Google Scholar]
- 11.Ympa YP, Sakr Y, Reinhart K, Vincent JL. Has mortality from acute renal failure decreased? A systematic review of the literature. Am J Med. 2005;118(8):827–832. doi: 10.1016/j.amjmed.2005.01.069. [DOI] [PubMed] [Google Scholar]
- 12.Bellomo R. The epidemiology of acute renal failure: 1975 versus 2005. Curr Opin Crit Care. 2006;12(6):557–560. doi: 10.1097/01.ccx.0000247443.86628.68. [DOI] [PubMed] [Google Scholar]
- 13.Fischer MJ, Brimhall BB, Lezotte DC, Glazner JE, Parikh CR. Uncomplicated acute renal failure and hospital resource utilization: a retrospective multicenter analysis. Am J Kidney Dis. 2005;46(6):1049–1057. doi: 10.1053/j.ajkd.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 14.Doi K, Yuen PS, Eisner C, et al. Reduced production of creatinine limits its use as marker of kidney injury in sepsis. J Am Soc Nephrol. 2009;20(6):1217–1221. doi: 10.1681/ASN.2008060617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Waikar SS, Bonventre JV. Creatinine kinetics and the definition of acute kidney injury. J Am Soc Nephrol. 2009;20(3):672–679. doi: 10.1681/ASN.2008070669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nguyen MT, Devarajan P. Biomarkers for the early detection of acute kidney injury. Pediatr Nephrol. 2008;23(12):2151–2157. doi: 10.1007/s00467-007-0470-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Devarajan P. Emerging biomarkers of acute kidney injury. Contrib Nephrol. 2007;156:203–212. doi: 10.1159/000102085. [DOI] [PubMed] [Google Scholar]
- 18.Devarajan P. Proteomics for biomarker discovery in acute kidney injury. Semin Nephrol. 2007;27:637–651. doi: 10.1016/j.semnephrol.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Devarajan P. Proteomics for the investigation of acute kidney injury. Contrib Nephrol. 2008;160:1–16. doi: 10.1159/000125893. [DOI] [PubMed] [Google Scholar]
- 20.Devarajan P, Parikh C, Barasch J. Case 31–2007: a man with abdominal pain and elevated creatinine. N Engl J Med. 2008;358(3):312. [PubMed] [Google Scholar]
- 21.Xu SY, Carlson M, Engström A, Garcia R, Peterson CG, Venge P. Purification and characterization of a human neutrophil lipocalin (HNL) from the secondary granules of human neutrophils. Scand J Clin Lab Invest. 1994;54(5):365–376. doi: 10.3109/00365519409088436. [DOI] [PubMed] [Google Scholar]
- 22.Kjeldsen L, Johnsen AH, Sengeløv H, Borregaard N. Isolation and primary structure of NGAL, a novel protein associated with human neutrophil gelatinase. J Biol Chem. 1993;286:10425–10432. [PubMed] [Google Scholar]
- 23.Cowland JB, Borregaard N. Molecular characterization and pattern of tissue expression of the gene for neutrophil gelatinase-associated lipocalin from humans. Genomics. 1997;45:17–23. doi: 10.1006/geno.1997.4896. [DOI] [PubMed] [Google Scholar]
- 24.Flower DR. Experimentally determined lipocalin structures. Biochim Biophys Acta. 2000;1482:46–56. doi: 10.1016/s0167-4838(00)00147-3. [DOI] [PubMed] [Google Scholar]
- 25.Goetz DH, Holmes MA, Borregaard N, et al. The neutrophil lipocalin NGAL is a bacteriostatic agent that interferes with siderophore-mediated iron acquisition. Mol Cell. 2002;10:1033–1043. doi: 10.1016/s1097-2765(02)00708-6. [DOI] [PubMed] [Google Scholar]
- 26▪.Schmidt-Ott KM, Mori K, Li JY, et al. Dual action of neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol. 2007;18:407–413. doi: 10.1681/ASN.2006080882. Comprehensive review of the functional roles of NGAL. [DOI] [PubMed] [Google Scholar]
- 27.Flo TH, Smith KD, Sato S, et al. Lipocalin 2 mediates an innate immune response to bacterial infection by sequestering iron. Nature. 2004;432:917–921. doi: 10.1038/nature03104. [DOI] [PubMed] [Google Scholar]
- 28.Berger T, Togawa A, Duncan GS, et al. Lipocalin 2-deficient mice exhibit increased sensitivity to Escherichia coli infection but not to ischemia-reperfusion injury. Proc Natl Acad Sci USA. 2006;103:1834–1839. doi: 10.1073/pnas.0510847103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang J, Goetz D, Li JY, et al. An iron delivery pathway mediated by a lipocalin. Mol Cell. 2002;10:1045–1056. doi: 10.1016/s1097-2765(02)00710-4. [DOI] [PubMed] [Google Scholar]
- 30.Yang J, Blum A, Novak T, Levinson R, Lai E, Barasch J. An epithelial precursor is regulated by the ureteric bud and by the renal stroma. Dev Biol. 2002;246:296–310. doi: 10.1006/dbio.2002.0646. [DOI] [PubMed] [Google Scholar]
- 31.Meldrum KK, Hilw K, Meldrum DR, et al. Simulated ischemia induced renal tubular cell apoptosis through a nuclear factor-κB dependent mechanism. J Urol. 2002;168:248–252. [PubMed] [Google Scholar]
- 32.Haussler U, von Wichert G, Schmid RM, et al. Epidermal growth factor activates nuclear factor-κB in human proximal tubule cells. Am J Physiol Renal Physiol. 2005;280:F808–F815. doi: 10.1152/ajprenal.00434.2003. [DOI] [PubMed] [Google Scholar]
- 33▪.Mishra J, Mori K, Ma Q, et al. Amelioration of ischemic acute renal injury by neutrophil gelatinase-associated lipocalin. J Am Soc Nephrol. 2004;15:3073–3082. doi: 10.1097/01.ASN.0000145013.44578.45. First study to demonstrate the role of NGAL as a renoprotective and therapeutic agent in animal models. [DOI] [PubMed] [Google Scholar]
- 34.Devarajan P. Neutrophil gelatinase-associated lipocalin: new paths for an old shuttle. Cancer Ther. 2007;5(B):463–470. [PMC free article] [PubMed] [Google Scholar]
- 35.Devarajan P. The promise of biomarkers for personalized renal cancer care. Kidney Int. 2010 doi: 10.1038/ki.2010.26. (In Press) [DOI] [PubMed] [Google Scholar]
- 36▪.Supavekin S, Zhang W, Kucherlapati R, et al. Differential gene expression following early renal ischemia-reperfusion. Kidney Int. 2003;63:1714–1724. doi: 10.1046/j.1523-1755.2003.00928.x. First transcriptomic study to report the induction of NGAL in AKI. [DOI] [PubMed] [Google Scholar]
- 37.Devarajan P, Mishra J, Supavekin S, Patterson LT, Potter SS. Gene expression in early ischemic renal injury: clues towards pathogenesis, biomarker discovery, and novel therapeutics. Mol Genet Metab. 2003;80(4):365–376. doi: 10.1016/j.ymgme.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 38.Yuen PST, Jo S-K, Holly MK, et al. Ischemic and nephrotoxic acute renal failure are distinguished by their broad transcriptomic responses. Physiol Genomics. 2006;25:375–386. doi: 10.1152/physiolgenomics.00223.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39▪▪.Mishra J, Ma Q, Prada A, et al. Identification of neutrophil gelatinase-associated lipocalin as a novel urinary biomarker for ischemic injury. J Am Soc Nephrol. 2003;4:2534–2543. doi: 10.1097/01.asn.0000088027.54400.c6. First study to identify NGAL as a biomarker of AKI in animal models. [DOI] [PubMed] [Google Scholar]
- 40.Mishra J, Mori K, Ma Q, et al. Neutrophil gelatinase-associated lipocalin (NGAL): a novel urinary biomarker for cisplatin nephrotoxicity. Am J Nephrol. 2004;24:307–315. doi: 10.1159/000078452. [DOI] [PubMed] [Google Scholar]
- 41.Mori K, Lee HT, Rapoport D, et al. Endocytic delivery of lipocalin-siderophore-iron complex rescues the kidney from ischemia-reperfusion injury. J Clin Invest. 2005;115:610–621. doi: 10.1172/JCI23056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chertow GM, Levy EM, Hammermeister KE, Grover F, Daley J. Independent association between acute renal failure and mortality following cardiac surgery. Am J Med. 1998;104:343–348. doi: 10.1016/s0002-9343(98)00058-8. [DOI] [PubMed] [Google Scholar]
- 43.Lassnigg A, Schmidlin D, Mouhieddine M, et al. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol. 2004;15:1597–1605. doi: 10.1097/01.asn.0000130340.93930.dd. [DOI] [PubMed] [Google Scholar]
- 44.Loef BG, Epema AH, Smilde TD, et al. Immediate postoperative renal function deterioration in cardiac surgical patients predicts in-hospital mortality and long-term survival. J Am Soc Nephrol. 2005;16:195–200. doi: 10.1681/ASN.2003100875. [DOI] [PubMed] [Google Scholar]
- 45.Bellomo R, Auriemma S, Fabbri A, et al. The pathophysiology of cardiac surgery-associated acute kidney injury (CSA-AKI) Int J Artif Organs. 2008;31(2):166–178. doi: 10.1177/039139880803100210. [DOI] [PubMed] [Google Scholar]
- 46▪▪.Mishra J, Dent C, Tarabishi R, et al. Neutrophil gelatinase-associated lipocalin (NGAL) as a biomarker for acute renal injury following cardiac surgery. Lancet. 2005;365:1231–1238. doi: 10.1016/S0140-6736(05)74811-X. First study to identify NGAL as a novel predictive biomarker of AKI in humans. [DOI] [PubMed] [Google Scholar]
- 47.Parikh CR, Mishra J, Thiessen-Philbrook H, et al. Urinary IL-18 is an early predictive biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2006;70:199–203. doi: 10.1038/sj.ki.5001527. [DOI] [PubMed] [Google Scholar]
- 48.Portilla D, Dent C, Sugaya T, et al. Liver fatty acid-binding protein as a biomarker of acute kidney injury after cardiac surgery. Kidney Int. 2008;73:465–472. doi: 10.1038/sj.ki.5002721. [DOI] [PubMed] [Google Scholar]
- 49.Wagener G, Jan M, Kim M, et al. Association between increases in urinary neutrophil-associated lipocalin and acute renal dysfunction after adult cardiac surgery. Anesthesiology. 2006;105:485–491. doi: 10.1097/00000542-200609000-00011. [DOI] [PubMed] [Google Scholar]
- 50.Koyner J, Bennett M, Worcester E, et al. Urinary cystatin C as an early biomarker of acute kidney injury following adult cardiothoracic surgery. Kidney Int. 2008;74(8):1059–1069. doi: 10.1038/ki.2008.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wagener G, Gubitosa G, Wang S, et al. Urinary neutrophil-associated lipocalin and acute kidney injury after cardiac surgery. Am J Kidney Dis. 2008;52(3):425–433. doi: 10.1053/j.ajkd.2008.05.018. [DOI] [PubMed] [Google Scholar]
- 52.Xin C, Yulong X, Yu C, et al. Urine neutrophil gelatinase-associated lipocalin and interleukin-18 predict acute kidney injury after cardiac surgery. Ren Fail. 2008;30:904–913. doi: 10.1080/08860220802359089. [DOI] [PubMed] [Google Scholar]
- 53.Tuladhar SM, Puntmann VO, Soni M, et al. Rapid detection of acute kidney injury by plasma and urinary neutrophil gelatinase-associated lipocalin after cardiopulmonary bypass. J Cardiovasc Pharmacol. 2009;53:261–266. doi: 10.1097/FJC.0b013e31819d6139. [DOI] [PubMed] [Google Scholar]
- 54.Haase-Fielitz A, Bellomo R, Devarajan P, et al. Novel and conventional serum biomarkers predicting acute kidney injury in adult cardiac surgery – a prospective cohort study. Crit Care Med. 2009;37(2):553–560. doi: 10.1097/CCM.0b013e318195846e. [DOI] [PubMed] [Google Scholar]
- 55.Haase M, Bellomo R, Devarajan P, et al. Novel biomarkers early predict the severity of acute kidney injury after cardiac surgery in adults. Ann Thorac Surg. 2009;88(1):124–130. doi: 10.1016/j.athoracsur.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 56.Haase-Fielitz A, Bellomo R, Devarajan P, et al. The predictive performance of plasma neutrophil gelatinase-associated lipocalin (NGAL) increases with grade of acute kidney injury. Nephrol Dial Transplant. 2009;24(11):3349–3354. doi: 10.1093/ndt/gfp234. [DOI] [PubMed] [Google Scholar]
- 57.Devarajan P. NGAL in acute kidney injury: from serendipity to utility. Am J Kidney Dis. 2008;52:395–399. doi: 10.1053/j.ajkd.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 58.Bellomo R, Ronco C, Kellum JA, et al. Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) group. Crit Care. 2004;8:R204–R212. doi: 10.1186/cc2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.McIlroy DR, Wagener G, Lee HT. Neutrophil Gelatinase-associated lipocalin and acute kidney injury after cardiac surgery: the effect of baseline renal function on diagnostic performance. Clin J Am Soc Nephrol. 2010;5(2):211–219. doi: 10.2215/CJN.04240609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60▪▪.Haase M, Bellomo R, Devarajan P, et al. Accuracy of neutrophil gelatinase-associated lipocalin (NGAL) in diagnosis and prognosis in acute kidney injury: a systematic review and meta-analysis. Am J Kidney Dis. 2009;54(6):1012–1024. doi: 10.1053/j.ajkd.2009.07.020. Meta-analysis of all published studies on NGAL as a biomarker of AKI and its clinical outcomes. [DOI] [PubMed] [Google Scholar]
- 61.Perico N, Cattaneo D, Sayegh MH, Remuzzi G. Delayed graft function in kidney transplantation. Lancet. 2004;364:1814–1827. doi: 10.1016/S0140-6736(04)17406-0. [DOI] [PubMed] [Google Scholar]
- 62.Halloran PF, Hunsicker LG. Delayed graft function: state of the art, November 10–11, 2000. Summit meeting, Scottsdale, Arizona, USA. Am J Transplant. 2001;1:115–120. [PubMed] [Google Scholar]
- 63.Mishra J, Ma Q, Kelly C, et al. Kidney NGAL is a novel early marker of acute injury following transplantation. Pediatr Nephrol. 2006;21:856–863. doi: 10.1007/s00467-006-0055-0. [DOI] [PubMed] [Google Scholar]
- 64▪.Parikh CR, Jani A, Mishra J, et al. Urine NGAL and IL-18 are predictive biomarkers for delayed graft function following kidney transplantation. Am J Transplant. 2006;6:1639–1645. doi: 10.1111/j.1600-6143.2006.01352.x. First study to report on the utility of NGAL as a biomarker in human kidney transplantation. [DOI] [PubMed] [Google Scholar]
- 65.Hall IE, Yarlagadda SG, Coca SG, et al. IL-18 and urinary NGAL predict dialysis and graft recovery after kidney transplantation. J Am Soc Nephrol. 2010;21(1):189–197. doi: 10.1681/ASN.2009030264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Kusaka M, Kuroyanagi Y, Mori T, et al. Serum neutrophil gelatinase-associated lipocalin as a predictor of organ recovery from delayed graft function after kidney transplantation from donors after cardiac death. Cell Transplant. 2008;17:129–134. doi: 10.3727/000000008783907116. [DOI] [PubMed] [Google Scholar]
- 67.Pannu N, Wiebe N, Tonelli M. Prophylaxis strategies for contrast-induced nephropathy. JAMA. 2006;295:2765–2779. doi: 10.1001/jama.295.23.2765. [DOI] [PubMed] [Google Scholar]
- 68.Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–936. doi: 10.1053/ajkd.2002.32766. [DOI] [PubMed] [Google Scholar]
- 69.Solomon R. Contrast media nephropathy – how to diagnose and how to prevent? Nephrol Dial Transplant. 2007;22(7):1812–1815. doi: 10.1093/ndt/gfm207. [DOI] [PubMed] [Google Scholar]
- 70.Bachorzewska-Gajewska H, Malyszko J, Sitniewska E, et al. Neutrophil-gelatinase-associated lipocalin and renal function after percutaneous coronary interventions. Am J Nephrol. 2006;26:287–292. doi: 10.1159/000093961. [DOI] [PubMed] [Google Scholar]
- 71.Bachorzewska-Gajewska H, Malyszko J, Sitniewska E, et al. Neutrophil gelatinase-associated lipocalin (NGAL) correlations with cystatin C, serum creatinine and eGFR in patients with normal serum creatinine undergoing coronary angiography. Nephrol Dial Transplant. 2007;22:295–296. doi: 10.1093/ndt/gfl408. [DOI] [PubMed] [Google Scholar]
- 72.Ling W, Zhaohui N, Ben H, et al. Urinary IL-18 and NGAL as early predictive biomarkers in contrast-induced nephropathy after coronary angiography. Nephron Clin Pract. 2008;108:c176–c181. doi: 10.1159/000117814. [DOI] [PubMed] [Google Scholar]
- 73▪.Hirsch R, Dent C, Pfriem H, et al. NGAL is an early predictive biomarker of contrast-induced nephropathy in children. Pediatr Nephrol. 2007;22:2089–2095. doi: 10.1007/s00467-007-0601-4. First study to report on the utility of NGAL as a biomarker of contrast-induced AKI in humans. [DOI] [PubMed] [Google Scholar]
- 74.Joannidis M, Metnitz B, Bauer P, et al. Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med. 2009;35(10):1692–1702. doi: 10.1007/s00134-009-1530-4. [DOI] [PubMed] [Google Scholar]
- 75.Guerin C, Girard R, Selli JM, et al. Initial versus delayed acute renal failure in the intensive care unit. A multicenter prospective epidemiological study. Am J Respir Crit Care Med. 2000;161:872–879. doi: 10.1164/ajrccm.161.3.9809066. [DOI] [PubMed] [Google Scholar]
- 76.Bagshaw SM, George C, Bellomo R. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47. doi: 10.1186/cc6863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zappitelli M, Washburn KM, Arikan AA, et al. Urine NGAL is an early marker of acute kidney injury in critically ill children. Crit Care. 2007;11:R84. doi: 10.1186/cc6089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wheeler DS, Devarajan P, Ma Q, et al. Serum neutrophil gelatinase-associated lipocalin (NGAL) as a marker of acute kidney injury in critically ill children with septic shock. Crit Care Med. 2008;36:1297–1303. doi: 10.1097/CCM.0b013e318169245a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Makris K, Markou N, Evodia E, et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) as an early marker of acute kidney injury in critically ill multiple trauma patients. Clin Chem Lab Med. 2009;47(1):79–82. doi: 10.1515/CCLM.2009.004. [DOI] [PubMed] [Google Scholar]
- 80.Siew ED, Ware LB, Gebretsadik T, et al. Urine neutrophil gelatinase-associated lipocalin moderately predicts acute kidney injury in critically ill adults. J Am Soc Nephrol. 2009;20(8):1823–1832. doi: 10.1681/ASN.2008070673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Cruz DN, de Cal M, Garzotto F, et al. Plasma neutrophil gelatinase-associated lipocalin is an early biomarker for acute kidney injury in an adult ICU population. Int Care Med. 2009;36(3):444–451. doi: 10.1007/s00134-009-1711-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bagshaw SM, Bennett M, Haase M, et al. Plasma and urine neutrophil gelatinase-associated lipocalin in septic versus non-septic acute kidney injury in critical illness. Int Care Med. 2009;36(3):452–461. doi: 10.1007/s00134-009-1724-9. [DOI] [PubMed] [Google Scholar]
- 83.Constantin JM, Futier E, Perbet S, et al. Plasma neutrophil gelatinase-associated lipocalin is an early marker of acute kidney injury in adult critically ill patients: a prospective study. J Crit Care. 2009 doi: 10.1016/j.jcrc.2009.05.010. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 84.Niemann CU, Walia A, Waldman J, et al. Acute kidney injury during Liver Transplantation as determined by neutrophil gelatinase-associated lipocalin. Liver Transplant. 2009;15:1852–1860. doi: 10.1002/lt.21938. [DOI] [PubMed] [Google Scholar]
- 85▪.Nickolas TL, O’Rourke MJ, Yang J, et al. Sensitivity and specificity of a single emergency department measurement of urinary neutrophil gelatinase-associated lipocalin for diagnosing acute kidney injury. Ann Intern Med. 2008;148:810–819. doi: 10.7326/0003-4819-148-11-200806030-00003. First study to demonstrate the utility of a single NGAL measurement to predict subsequent AKI and its clinical outcomes in the heterogeneous emergency department setting. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Boldt J, Brosch C, Ducke M, et al. Influence of volume therapy with a modern hydroxyethylstarch preparation on kidney function in cardiac surgery patients with compromised renal function: a comparison with human albumin. Crit Care Med. 2007;35:2740–2746. doi: 10.1097/01.CCM.0000288101.02556.DE. [DOI] [PubMed] [Google Scholar]
- 87.Boldt J, Brosch CH, Rohm K, et al. Comparison of the effects of gelatin and a modern hydroxyethylstarch solution on renal function and inflammatory response in elderly cardiac surgery patients. Br J Anaesth. 2008;100:457–464. doi: 10.1093/bja/aen016. [DOI] [PubMed] [Google Scholar]
- 88.Boldt J, Suttner S, Brosch C, et al. Cardiopulmonary bypass priming using a high dose of a balanced hydroxyethyl starch versus an albumin-based priming strategy. Anesth Analg. 2009;109(6):1752–1762. doi: 10.1213/ANE.0b013e3181b5a24b. [DOI] [PubMed] [Google Scholar]
- 89.Haase M, Fielitz-Haase A, Bellomo R, et al. Sodium bicarbonate to prevent acute kidney injury after cardiac surgery: a pilot double-blind, randomized controlled trial. Crit Care Med. 2009;37(1):39–47. doi: 10.1097/CCM.0b013e318193216f. [DOI] [PubMed] [Google Scholar]
- 90.Capuano F, Goracci M, Luciani R, et al. Neutrophil gelatinase-associated lipocalin levels after use of mini-cardiopulmonary bypass system. Interact Cardiovasc Thorac Surg. 2009;9(5):797–801. doi: 10.1510/icvts.2009.212266. [DOI] [PubMed] [Google Scholar]
- 91.Wagener G, Gubitosa G, Wang S, et al. Increased incidence of acute kidney injury with aprotinin use during cardiac surgery detected with urinary NGAL. Am J Nephrol. 2008;28:576–582. doi: 10.1159/000115973. [DOI] [PubMed] [Google Scholar]
- 92▪▪.Dent CL, Ma Q, Dastrala S, et al. Plasma NGAL predicts acute kidney injury, morbidity and mortality after pediatric cardiac surgery: a prospective uncontrolled cohort study. Crit Care. 2007;11:R127. doi: 10.1186/cc6192. First study to report on the utility of a point-of-care clinical kit for plasma NGAL measurements. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93▪▪.Bennett M, Dent CL, Ma Q, et al. Urine NGAL predicts severity of acute kidney injury after cardiac surgery: a prospective study. Clin J Am Soc Nephrol. 2008;3:665–673. doi: 10.2215/CJN.04010907. First study to report on the utility of a clinical laboratory platform for urine NGAL measurements. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Trachtman H, Christen E, Cnaan A, et al. Urinary neutrophil gelatinase-associated lipocalcin in D+HUS: a novel marker of renal injury. Pediatr Nephrol. 2006;21:989–994. doi: 10.1007/s00467-006-0146-y. [DOI] [PubMed] [Google Scholar]
- 95.Kumpers P, Hafer C, Lukasz A, et al. Serum neutrophil gelatinase-associated lipocalin at inception of renal replacement therapy predicts survival in critically ill patients with acute kidney injury. Crit Care. 2010;14:R9. doi: 10.1186/cc8861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Schaub S, Mayr M, Hönger G, et al. Detection of subclinical tubular injury after renal transplantation: comparison of urine protein analysis with allograft histopathology. Transplantation. 2007;84:104–112. doi: 10.1097/01.tp.0000268808.39401.e8. [DOI] [PubMed] [Google Scholar]
- 97.Grenier FC, Ali S, Syed H, et al. Evaluation of the ARCHITECT urine NGAL assay: assay performance, specimen handling requirements and biological variability. Clin Biochem. 2009 doi: 10.1016/j.clinbiochem.2009.12.008. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 98.Haase-Fielitz A, Haase M, Bellomo R. Instability of urinary NGAL during long-term storage. Am J Kidney Dis. 2009;53:564–565. doi: 10.1053/j.ajkd.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 99.Ma Q, Devarajan P. Induction of proapoptotic Daxx following ischemic acute kidney injury. Kidney Int. 2008;74:310–318. doi: 10.1038/ki.2008.192. [DOI] [PubMed] [Google Scholar]
- 100.Srichai MB, Hao C, Davis L, et al. Apoptosis of the thick ascending limb results in acute kidney injury. J Am Soc Nephrol. 2008;19:1538–1546. doi: 10.1681/ASN.2007101101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Grigoryev DN, Liu M, Hassoun HT, et al. The local and systemic inflammatory transcriptome after acute kidney injury. J Am Soc Nephrol. 2008;19:547–558. doi: 10.1681/ASN.2007040469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Mitsnefes M, Kathman T, Mishra J, et al. Serum NGAL as a marker of renal function in children with chronic kidney disease. Pediatr Nephrol. 2007;22:101–108. doi: 10.1007/s00467-006-0244-x. [DOI] [PubMed] [Google Scholar]
- 103.Malyszko J, Bachorzewska-Gajewska H, Malyszko JS, et al. Serum neutrophil gelatinase-associated lipocalin as a marker of renal function in hypertensive and normotensive patents with coronary artery disease. Nephrology (Carlton) 2008;13:153–156. doi: 10.1111/j.1440-1797.2007.00899.x. [DOI] [PubMed] [Google Scholar]
- 104.Malyszko J, Bachorzewska-Gajewska H, Sitniewska E, et al. Serum neutrophil gelatinase-associated lipocalin as a marker of renal function in non-diabetic patients with stage 2–4 chronic kidney disease. Ren Fail. 2008;30:1–4. doi: 10.1080/08860220802134607. [DOI] [PubMed] [Google Scholar]
- 105.Hemdahl A-L, Gabrielsen A, Zhu C, et al. Expression of neutrophil gelatinase-associated lipocalin in atherosclerosis and myocardial infarction. Arterioscler Thromb Vasc Biol. 2006;26:136–142. doi: 10.1161/01.ATV.0000193567.88685.f4. [DOI] [PubMed] [Google Scholar]
- 106.Folkesson M, Kazi M, Zhu C, et al. Presence of NGAL/MMP-9 complexes in human abdominal aortic aneurysms. Thromb Haemost. 2007;98(2):427–433. [PubMed] [Google Scholar]
- 107.Bolignano D, Lacquaniti A, Coppolino G, et al. Neutrophil gelatinase-associated lipocalin reflects the severity of renal impairment in subjects affected by chronic kidney disease. Kidney Blood Press Res. 2008;31:255–258. doi: 10.1159/000143726. [DOI] [PubMed] [Google Scholar]
- 108.Bolignano D, Coppolino G, Campo S, et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) is associated with severity of renal disease in proteinuric patients. Nephrol Dial Transplant. 2008;23:414–416. doi: 10.1093/ndt/gfm541. [DOI] [PubMed] [Google Scholar]
- 109.Bolignano D, Lacquaniti A, Coppolino G, et al. Neutrophil gelatinase-associated lipocalin (NGAL) and progression of chronic kidney disease. Clin J Am Soc Nephrol. 2009;4(2):337–344. doi: 10.2215/CJN.03530708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ding H, He Y, Li K, et al. Urinary neutrophil gelatinase-associated lipocalin (NGAL) is an early biomarker for renal tubulointerstitial injury in IgA nephropathy. Clin Immunol. 2007;123:227–234. doi: 10.1016/j.clim.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 111.Brunner HI, Mueller M, Rutherford C, et al. Urinary NGAL as a biomarker of nephritis in childhood-onset SLE. Arthritis Rheum. 2006;54:2577–2584. doi: 10.1002/art.22008. [DOI] [PubMed] [Google Scholar]
- 112.Suzuki M, Wiers KM, Klein-Gitelman MS, et al. Neutrophil gelatinase-associated lipocalin as a biomarker of disease activity in pediatric lupus nephritis. Pediatr Nephrol. 2008;23:403–412. doi: 10.1007/s00467-007-0685-x. [DOI] [PubMed] [Google Scholar]
- 113.Hinze CH, Suzuki M, Klein-Gitelman M, et al. Neutrophil gelatinase-associated lipocalin is a predictor of the course of global and renal childhood-onset systemic lupus erythematosus disease activity. Arthritis Rheum. 2009;60(9):2772–2781. doi: 10.1002/art.24751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Yilmaz A, Sevketoglu E, Gedikbasi A, et al. Early prediction of urinary tract infection with urinary neutrophil gelatinase associated lipocalin. Pediatr Nephrol. 2009;24(12):2387–2392. doi: 10.1007/s00467-009-1279-6. [DOI] [PubMed] [Google Scholar]
- 115.Braunwald E. Biomarkers in heart disease. N Engl J Med. 2008;358:2148–2159. doi: 10.1056/NEJMra0800239. [DOI] [PubMed] [Google Scholar]
- 116.Peacock WF, 4th, De Marco T, Fonarow GC, et al. Cardiac troponin and outcome in acute heart failure. N Engl J Med. 2008;358:2117–2126. doi: 10.1056/NEJMoa0706824. [DOI] [PubMed] [Google Scholar]
Website
- 201.US FDA. Challenges and Opportunities Report. 2004 March; www.fda.gov/ScienceResearch/SpecialTopics/CriticalPathInitiative/CriticalPathOpportunitiesReports/ucm077262.htm.