Abstract
Purpose
Meibomian gland dysfunction (MGD) is a common clinical problem that is often associated with evaporative dry eye disease. Alterations of the lipids of the meibomian glands have been identified in several studies of MGD. This prospective, observational, open label clinical trial documents the improvement in both clinical signs and symptoms of disease as well as spectroscopic behavior of the meibomian gland lipids after therapy with topical azithromycin ophthalmic solution.
Methods
Subjects with symptomatic MGD were recruited. Signs of MGD were evaluated with a slit lamp. Symptoms of MGD were measured by the response of subjects to a questionnaire. Meibum lipid (ML) lipid-lipid interaction strength, conformation and phase transition parameters were measured using Fourier transform infrared spectroscopy (FTIR).
Results
In subjects with clinical evidence of MGD changes in ordering of the lipids and resultant alteration of phase transition temperature were identified. Topical therapy with azithromycin relieved signs and symptoms and restored the lipid properties of the meibomian gland secretion towards normal.
Conclusions
Improvement in phase transition temperature of the meibomian gland lipid with the determined percent trans rotomer composition of the lipid strongly suggests that the ordering of the lipid molecules is altered in the disease state (MGD) and that azithromycin can improve that abnormal condition toward normal in a manner that correlates with clinical response to therapy.
Introduction
Meibomian gland dysfunction (MGD) is a common clinical problem responsible for symptoms and signs of eyelid irritation and is frequently a cause of evaporative dry eye.1 Alterations of the lipids of the meibomian glands with advancing age and disease have been documented in several studies using different analytical techniques.2,3 The identified changes in the lipids help to explain some of the abnormalities of tear film function in evaporative dry eye.4-6 Conventional therapy of meibomian gland dysfunction includes mechanical options of lid massage and lid expression as well as medicinal therapy of systemic tetracycline and doxycycline, but such therapeutic measures are often unsatisfactory or not well tolerated.7 Recent clinical trials have identified topical azithromycin as a potentially effective and well tolerated therapy of lid margin disease and meibomian gland dysfunction.8,9 Azithromycin has been classified as bacteriostatic at concentrations corresponding to and exceeding published tear and conjunctival levels.10 The prospective, observational, open-label clinical trial described in this report evaluated both the clinical signs and symptoms of meibomian gland dysfunction as well as the spectroscopically analyzed alterations in lipid behavior of the meibomian gland secretion in a group of subjects with symptomatic meibomian gland dysfunction unresponsive to lid massage and hygiene before and after therapy with topical azithromycin ophthalmic solution.
Materials and Methods
Subjects
Twenty two subjects diagnosed with symptomatic MGD that were unresponsive to lid massage following application of a hot compress to the eyelid were recruited to the clinical trial. Written informed consent was obtained from all donors. All protocols and procedures were reviewed by the Institutional Review Boards of the University of Louisville and the Louisville Veterans Administration Hospital and procedures were in accord with the Declaration of Helsinki. Subject demographics are summarized in Table I. Subject inclusion criteria were the presence of symptomatic meibomian gland dysfunction in subjects between ages 18 and 80 years of age who were not taking systemic nor topical antibiotics nor using topical anti-inflammatory medications. Exclusion criteria were the history of allergy to azithromycin, altered lid anatomy (with the exception of meibomian gland dysfunction), or inability to comprehend the informed consent or complete the requested therapy and follow-up. All subjects underwent a complete examination of the eyelids and anterior segment of the eye including measurement of intraocular pressure prior to entry into the study. Symptoms were measured on a four point categorical scale of none, mild, moderate, or severe according to the subject's response to questions regarding itching, burning, foreign body sensation, eyelid redness, and eyelid swelling (Table II). Signs were evaluated with slit lamp observed conjunctival injection, fluorescein tear breakup time, ocular surface staining with fluorescein, and evaluation of the eyelid margin and character of meibomian gland orifices (Table III). All signs were graded on a four point categorical scale as summarized in Table III with exception of tear breakup time which was measured in seconds following a complete blink after instillation of 5 μl of topical 1% fluorescein solution.
Table I.
Subject demographics
| N=22 |
| Age: 64 years mean (± 3 yr) [range 33 – 83 years] |
| Sex: 12 male 10 female |
| Race: 20 caucasian 1 african-american 1 asian |
Table II.
Grading of clinical symptoms (as used in Figure 1)
| Symptom | Grade 0 | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|---|
| Itching | none | awareness | desire to rub | frequent rub |
| FBS* | none | awareness | desire to rub | desire to close lid |
| Dryness | none | awareness | need for drop | frequent drops |
| Burning | none | awareness | need to rub | frequent rub |
| Swelling | none | noticeable | obvious | decrease in aperture |
FBS= foreign body sensation
Table III.
Grading of clinical signs (as used in Figure 2)
| Sign | Grade 0 | Grade 1 | Grade 2 | Grade 3 |
|---|---|---|---|---|
| Conjunctival redness | none | pink | light red | bright red |
| Lid margin debris | none | 1-5 crusts | 6-10 crusts | >10 crusts |
| Lid margin redness | none | pink | light red | bright red |
| MG expression | touch | light pressure | moderate pressure | occluded |
| MG secretion | clear | turbid | turbid with clumps | solid paste |
| MG plugging | Number of plugged orifices within the central 10 glands of lower lid | |||
| TBUT | Number of seconds to first breakup following complete blink | |||
Materials
Silver chloride windows for infrared spectroscopy were obtained from Crystran Limited, Poole, United Kingdom. All chemicals were purchased from Sigma-Aldrich Chemical Co., St Louis MO.
Collection of Tear Lipids
ML was obtained from twenty-two subjects as described in Kilp et al., 1986, 11 except that meibomian gland excreta were collected with a platinum spatula. Lid expression was performed with cotton tipped applicators following instillation of topical proparacaine and the expressate was collected on a platinum spatula for transfer directly to a silver chloride window and into 0.5 mL of tetrahydrofuran/methanol, 3:1, v:v (THF/MeOH) in a 9 mm micro vial with a Teflon cap (Microliter Analytical Supplies Ind., Suwanee, Georgia). Similar sampling of the expressed meibum was done at 2 and 4 weeks of therapy and 1 month following cessation of therapy. About 1 mg of ML was collected per individual for direct spectroscopic study. Subjects were instructed not to instill medication for at least eight hours prior to collection of lipid secretions.
Fourier Transform Infrared Spectroscopy
Infrared spectra were measured using a Nicolet 5000 Magna Series Fourier transform infrared spectrometer (Thermo Fisher Scientific, Inc., Waltham MA). The ML was placed on the AgCl window and placed in a temperature-controlled infrared cell holder. The cell was jacketed by an insulated water coil connected to a Neslab R-134A (NESLAB Instruments, Newton NH) circulating water bath. The sample temperature was measured and controlled by a thermistor touching the sample cell window. The water bath unit was programmed to measure the temperature at the thermistor and to adjust the bath temperature so the sample temperature was adjusted to the desired set point. The rate of heating or cooling (1°C/15 min) at the sample was also adjusted by the water bath unit. Temperatures were maintained within ± 0.01°C. Exactly 150 interferograms were recorded and averaged. Spectral resolution was set to 1.0 cm-1.
Infrared data analysis was performed with GRAMS/386 software (Galactic Industries, Salem, NH). The frequency of the CH2 band near 2850 cm-1 was used to estimate the content of trans and gauche rotomers in the hydrocarbon chains. The ν̃sym was calculated by first baseline leveling the OH-CH stretching region near 3,500 and 2,700 cm-1. The center of mass of the CH2 symmetric stretching band was calculated by integrating the top 10 % of the intensity of the band. The baseline for integrating the top 10% of the intensity of the band was parallel to the OH-CH region baseline.
Lipid CH2 groups in the hydrocarbon chains are present as gauche rotomers, prevalent in disordered hydrocarbon chains, or trans rotomers, more abundant in ordered hydrocarbon chains. Thus, lipid hydrocarbon chain order may be evaluated in terms of the amount of CH2 trans rotomers. The frequency of the CH2 symmetric stretch, ν̃sym, is dependent on the amount of trans or gauche rotomers12 and has been used to characterize lipid phase transitions2,12-20 to measure the trans rotomer content of lipid hydrocarbon chains with changes in temperature.2, 12–15,21 Since rotomers are either trans or gauche, phase transitions can be described by a two-state sigmoidal equation as described by Borchman et al.2 Lipid order at 33.4°C was calculated by extrapolating the ν̃sym at 33.4°C from the fit of the phase transition and then converting ν̃sym to the % of trans rotomers, a measure of lipid conformational order (see Borchman et al.2). The % trans rotomer data were used to calculate the phase transition enthalpy and entropy from the slopes of Arrhenius plots as described in Borchman et al.2 Arrhenius plots from tear-lipid phase transitions were linear with correlation coefficients greater than 0.998.
Treatment protocol
All subjects were provided 1% topical azithromycin ophthalmic solution (Azasitetm, Inspire Pharmaceuticals, Inc, Durham, NC) with instructions to use one drop twice daily for two days then once daily for the four week duration of the treatment phase of the study. Subjects were instructed not to instill medication the morning of examinations.
Matrix-assisted laser desorption/ionization (MALDI) time-of-flight mass spectrometry (TOF-MS)
To determine if azithromycin was present in meibum, mass spectra were acquired with a Voyager Biospectrometry DE instrument (PerSeptive Biosystems, Framingham, MA), that uses a pulsed nitrogen laser at 337 nm to induce ionization. The extraction voltage was 20 kV. The laser power level was adjusted to obtain high signal-to-noise ratios, while ensuring minimal fragmentation of the parent ions.
After infrared analysis, ML was removed from the AgCl window by the following protocol that used glass with care to avoid any plastic. Solvent in the micro-vial containing ML rinsed from the spatula as described in the Tear Lipid Collection Section was evaporated under a stream of nitrogen gas. The AgCl window with ML was placed ML side down into a 15 mL glass scintillation vial containing 1 mL hexane and purged with argon gas. The vial was sonicated in an ultrasonic bath (Branson 1510, Branson Ultrasonics, Danbury, CT) for 10 min. The hexane was decanted into the micro-vial containing the ML rinsed from the spatula. The hexane was evaporated under a stream of nitrogen gas. Methanol (1.5 mL) was added to the scintillation vial containing the AgCl window and purged with argon gas. The vial was sonicated in an ultrasonic bath (Branson Ultrasonics, Danbury, CT) for 10 min. The methanol was decanted into the micro-vial containing the ML rinsed from the spatula and was evaporated under a stream of nitrogen gas. THF/MeOH (1.5 mL) was added to the scintillation vial containing the AgCl window and purged with argon gas. The vial was sonicated in an ultrasonic bath (Branson Ultrasonics, Danbury, CT) for 10 min. The THF/MeOH was decanted into the micro-vial containing the ML rinsed from the spatula and was then evaporated under a stream of nitrogen gas until about 50 μL remained.
All of the solvent was equally applied to three spots, 2 μL at a time, onto a 100-spot stainless steel plate (Applied Biosystems, Foster City, CA). The sample was allowed to crystallize before the subsequent addition of sample. Another 20 μL THF/MeOH, was added to the sample vial taking care to wash sample off the sides. This rinse was spotted equally onto the three spots, 1 μL at a time, until no solvent remained in the vial.
Onto one spot was placed 1 μL, 0.09 M CsCl in water. Onto the other spot was placed 2 μL of silver trifluoro acetate (50 mM in THF/MeOH). After drying, 1 μL 2, 5-dihydro benzoic acid (DHB) (0.5 M THF/MeOH containing 0.1% trihydroacetic acid) was placed onto both spots and allowed to crystallize. The third spot was reserved for an unrelated study.
After lyophillization (Labconco Corporation, Kansas City, Missouri) at ambient conditions for at least 4 hours, positive ion spectra were acquired in the positive reflector mode. One mass spectrum represents the average of more than 1000 traces. The mass range sampled was 90-1500 Da.
Mass spectra were calibrated to the matrix band at 155.034 Da and the 678.506 Da band of protonated dimyristoylphosphatilycholine that was added to the samples as a calibration standard. If the 678.506 band was bound effectively to either silver or cesium, the bands at 786.4045 or at 810.405 were used, respectively.
Statistics
Data are presented as the average ± the standard error of the mean. Statistical significance was determined using Student's t-test or the correlation coefficient from the linear regression best fit. Values of p < 0.01 were considered statistically significant.
Results
Clinical
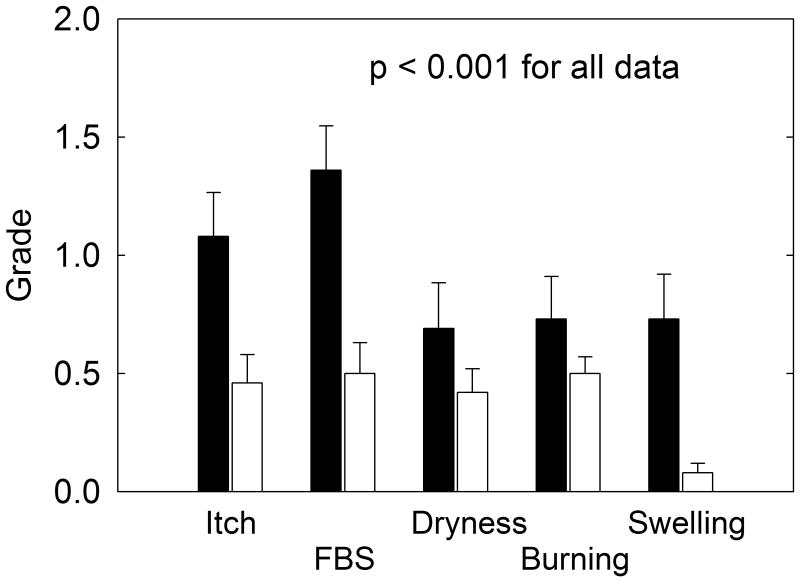
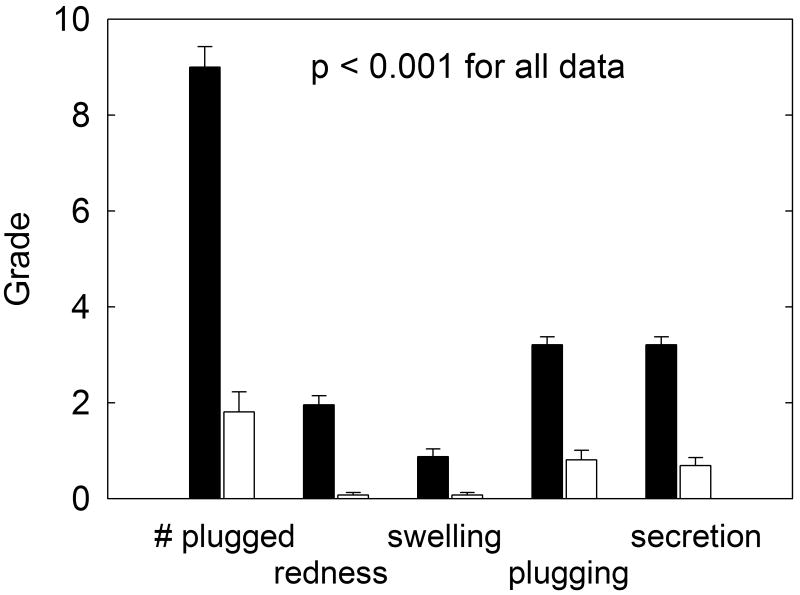
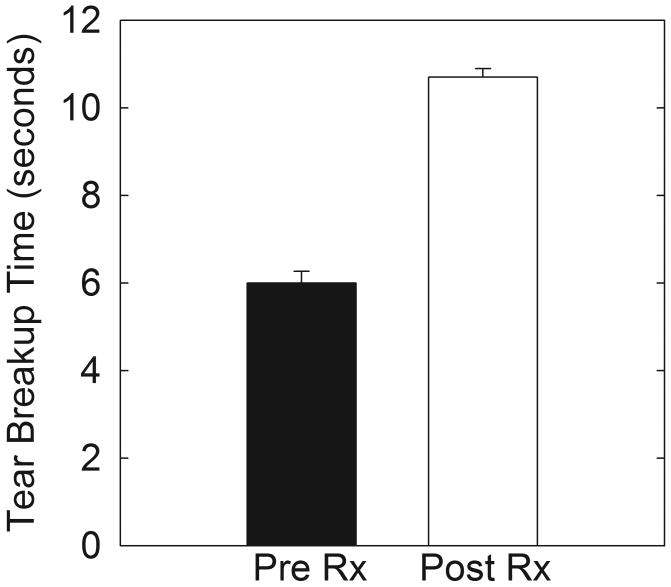
Of the twenty-two subjects enrolled in the study seventeen completed four weeks of therapy. Two subjects discontinued the medication due to stinging upon instillation and three subjects were lost to follow-up. Subject-reported global response to therapy demonstrated observable improvement at two weeks but greater response at four weeks of therapy as depicted in Table IV with all subjects describing relief or absence of symptoms at four weeks of therapy. Symptom improvement, as measured by mean score of severity, decreased for all evaluated symptoms by a statistically significant amount (p<0.001) as depicted in Figure 1 at four weeks of treatment. All signs of eyelid margin disease improved at four weeks including the number of obstructed glands, the amount of lid margin erythema, the ease of expression of the meibomian glands, and the character of the meibomian gland secretion (Figure 2). Improvement in tear breakup time was highly statistically significant at four weeks of therapy (p<0.001) (Figure 3).
Table IV.
Global Response to Therapy [n=34 eyes]
| Grade of Improvement | 2 weeks | 4weeks |
|---|---|---|
| (number of subjects) | ||
| 4 (resolution of symptoms) | 9 | 14 |
| 3 | 9 | 10 |
| 2 | 8 | 4 |
| 1 | 6 | 6 |
| 0 (no improvement) | 2 | 0 |
Figure 1.
Subjects with MGD reported global improvement in symptoms in response to 4 weeks of topical azithromycin therapy. Symptoms were assessed from a questionnaire. Subjects with MGD prior to treatment (filled bars). Subjects after 4 weeks of treatment (open bars).
*FBS= foreign body sensation
Figure 2.
Signs of MGD were restored in patients with MGD in response to 4 weeks of topical azithromycin therapy. (filled bars): Subjects with MGD prior to treatment. (open bars): Subjects after 4 weeks of treatment.
Figure 3.
Tear breakup time increased significantly after 4 weeks of topical azithromycin treatment (open bars) compared to patients with MGD prior to treatment (filled bars).
Lipid analysis of meibum
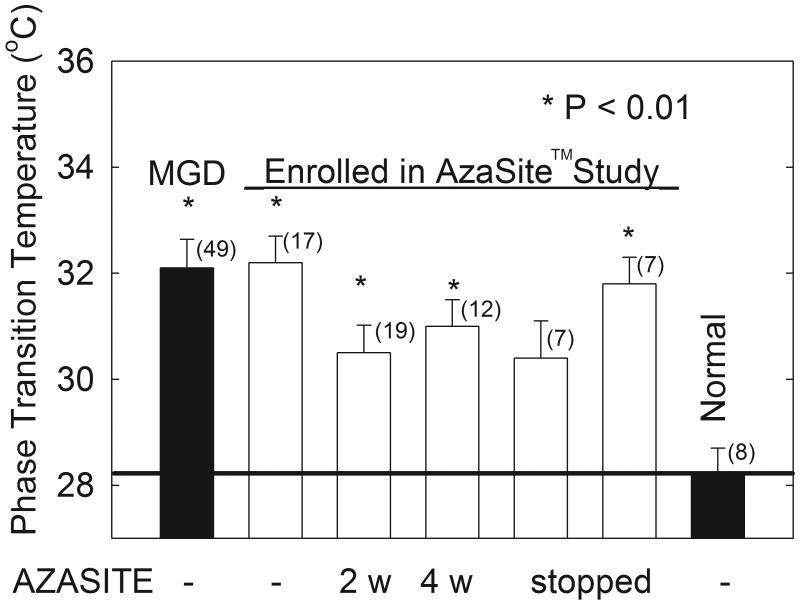
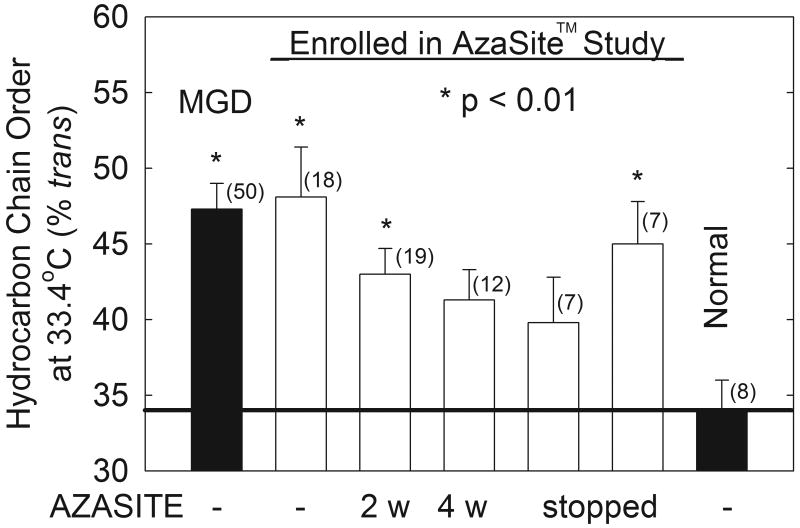
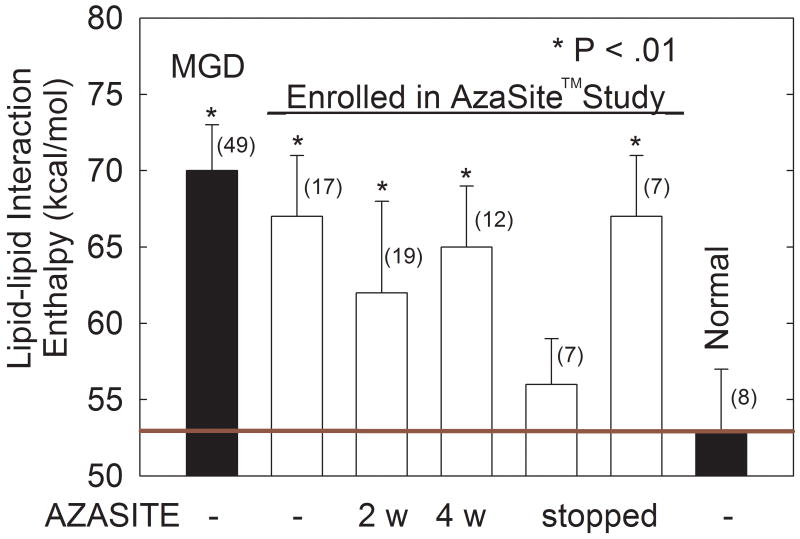
Phase transition parameters are summarized in Table V. Fourier transform infrared spectroscopy of the expressed meibomian gland secretion from subjects with MGD measured an increase in the phase transition temperature of meibum lipids that was significantly different from age matched controls identified in a previous study (p < 0.01, Figure 4, Manuscript submitted to Investigative Ophthalmology and Visual Sciences). The phase transition temperature profiles correlated well with the measured increase in lipid ordering determined as percent trans rotomer composition of the expressed lipids (Figure 5). The higher levels of both phase transition temperature and degree of lipid ordering (Figure 5) were comparable to data from a larger group of subjects with MGD obtained in a separate study (Manuscript submitted to Investigative Ophthalmology and Visual Sciences). Two weeks after treatment was stopped, the therapy significantly lowered the interaction enthalpy to a level indistinguishable from normal ML despite the large experimental deviations (Figure 6).
Table V.
Phase Transition Parameters
| Phase transition Parameter | MGD* | Enrolled Treatment Time (weeks) | Enrolled Post Treatment time (weeks) | Normal | |||
|---|---|---|---|---|---|---|---|
| (0) | (2) | (4) | (2) | (4) | |||
| Minimum Frequency (cm-1) | 2849.68 ± 0.06 | 2849.66 ± 0.09 | 2849.73 ± 0.06 | 2849.74 ± 0.09 | 2849.9 ± 0.1 | 2849.83 ± 0.09 | 2849.9 ± 0.1 |
| Maximum Frequency (cm-1) | 2853.48 ± 0.07 | 2853.5 ± 0.1 | 2853.31 ± 0.08 | 2853.5 ± 0.1 | 2853.7 ± 0.2 | 2853.46± 0.1 | 2853.5 ± 0.1 |
| Cooperativity | -8.5 ± 0.4 | -8.0 ± 0.4 | -8.8 ± 0.7 | -8.5 ± 0.4 | -7.8 ± 0.3 | -9 ± 1 | -9.2 ± 0.4 |
| Phase transition Temperature (°C) | 32.2 ± 0.5 | 31.3 ± 0.7 | 30.5 ± 0.5 | 31.0 ± 0.5 | 30.3 ± 0.7 | 31.8 ± 0.5 | 28.5 ± 0.5 |
| Enthalpy (Kcal/mol) | 157 ± 7 | 147 ± 5 | 145 ± 12 | 156 ± 2 | 151 ± 14 | 146 ± 8 | 149 ± 7 |
| Entropy (Kcal/mol/degree) | 0.51 ± 0.02 | 0.51 ± 0.02 | 0.48 ± 0.04 | 0.48 ± 0.03 | 0.55 ± 0.06 | 0.48 ± 0.03 | 0.50 ± 0.08 |
| Order (%) at 33.4°C | 47 ± 2 | 48 ± 3 | 43 ± 2 | 41 ± 2 | 40 ± 3 | 45 ± 2 | 36 ± 2 |
| Number of samples | 49 | 18 | 19 | 12 | 7 | 7 | 9 |
Figure 4.
ML phase transition temperature was statistically significantly reduced in subjects treated with topical azithromycin therapy for 4 weeks but the phase transition temperature did increase greater than one month after therapy was stopped (open bars). Comparison of data from a larger study previously shows the increase in the phase transition temperature of ML from subjects with MGD compared to ML from subjects without MGD (closed bars).
Figure 5.
ML hydrocarbon order at 33.4°C was statistically significantly different in MGD subjects after 4 weeks of topical azithromycin therapy but regressed during two months after therapy was stopped (open bars). Comparison of data from a larger study shows the increase in hydrocarbon order of ML from subjects with MGD compared to ML from subjects without MGD (normal) (closed bars). More order indicates stiffer lipids with stronger lipid-lipid interactions.
Figure 6.
The ML lipid-lipid interaction enthalpy at 33.4°C statistically significantly decreased on azithromycin therapy but returned to elevated levels two months after azithromycin was stopped (open bars). Comparison of data from a previous study shows the increase in lipid-lipid interaction enthalpy of ML from subjects with MGD compared to ML from subjects without MGD [normal] (closed bars). ML lipid-lipid interaction enthalpy was calculated from the enthalpy of the phase transition and the percentage of trans rotomers at 33.4°C.
The change in lipid spectroscopic behavior produced by topical azithromycin therapy at both two weeks and four weeks indicated a reduction in the abnormally elevated phase transition temperature and percent trans rotomer conformation of the lipids (Figs. 4 and 5). A statistically significant improvement in both parameters occurred at four weeks of therapy and a small but statistically insignificant trend for further improvement was noted at the measurement done after one month following discontinuation of therapy.
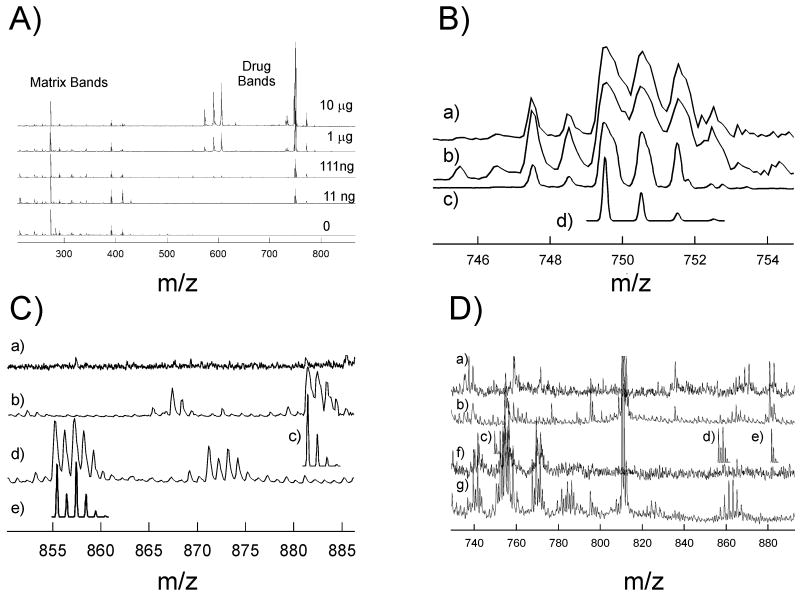
Measurement of azithromycin in meibum
MALDI-TOF spectroscopy was used to quantify azithromycin to determine if it was present in quantities capable of directly changing the conformation of ML. A concentration dependent control study (Fig. 6A) shows azithromycin bands beginning at 749.51 Da. The intensity of the bands was concentration dependent. As little as 11 ng or 15 ρmoles of azithromycin could easily be detected in control solutions. The three large bands near 591 Da could be due to a decomposition product of azithromycin. Cleavage of either of the hexopyranosides in the 11 and 13 positions (11-{[3,4,6-trideoxy-3-(dimethylamino)-β-D-xylo-hexopyranosyl]oxy}-1-oxa-6-azacyclopentadec or 13-yl 2,6-dideoxy-3-C-methyl-3-O-methyl-α-L-ribo-hexopyranoside) leaving a hydroxyl moiety on the main ring would result in an adduct with a molecular weight of 591.5 Da.
To determine if azithromycin could be detected under conditions used to measure ML by MALDI-TOF spectroscopy, 1 μg of azithromycin was analyzed with just DBH as a matrix (Fig. 6B, spectrum a). Four bands due to the isotopic distribution of mono-protonated azithromycin were resolved at 749.512, 750.512, 751.512 and 752.512 Da. The experimental isotopic distribution pattern (Fig. 7A, spectrum a) was similar to the calculated pattern (Fig. 6B, spectrum d). Similarly, isotopic bands were resolved when silver (Fig. 6B, spectrum b) or Cs (Fig. 6C, spectrum c) were present with the matrix. Silver may be used to resolve waxes, and cesium is used to reduce spectral complexity due to other cations such as sodium and potassium and also used to increased homogeneity in the crystals and to minimize the loss of matrix caused by the high vacuum in the ionization chamber.22
Figure 7.
MALDI-TOF spectra of ML and azithromycin.
A) Azithromycin sensitivity study. The relative intensity of the azithromycin bands beginning at 749 Da increased with increasing amounts of azithromycin. Azithromycin could be detected as low as 11 ng. The matrix was DBH.
B) Expanded 749 Da region of azithromycin spectra with different matrixes: a) DBH Cs matrix. b) DBH Ag matrix c) DBH matrix. d) Calculated isotopic distribution for azithromycin.
C) Expanded spectra with different matrixes: a) DBH matrix; b) DBH Cs matrix; d) DBH Ag matrix. c) Calculated isotopic distribution for azithromycin-Cs adduct. e) Calculated isotopic distribution for azithromycin-Ag adduct.
D) ML spectra. a) typical averaged spectra of ML with DBH/Cs matrix from subjects without MGD. b) typical averaged spectra of ML with DBH/Cs matrix from subjects with MGD. c) Calculated isotopic distribution for azithromycin d) Calculated isotopic distribution for azithromycin-Ag adduct e) Calculated isotopic distribution for azithromycin-Cs adduct f) typical averaged spectra of ML with DBH/Ag matrix from subjects without MGD. g) typical averaged spectra of ML with DBH/Ag matrix from subjects with MGD. When comparing spectrum a with b and spectrum f with g, no differences were found in regions where azithromycin would be expected (spectra c, d, e). We conclude from this observation that azithromycin concentration is below the detection limit of 1 ρmole per mg of ML or absent in ML from subjects treated with azithromycin.
Four bands were resolved at 855.42, 856.42, 857.42 and 858.42 Da due to the isotopic distribution of the azithromycin-silver adduct (Fig. 6C, spectrum d) and at 881.42, 882.42 883.42 and 883.42 due to the isotopic distribution of the azithromycin-Cs adduct (Fig. 6C spectrum b). The experimental isotopic distribution patterns (Fig. 6A, spectra b and d) were similar to the calculated pattern (Fig. 6B, spectra c and e), respectively. No bands were present in this region when silver or cesium were excluded from the matrix (Fig. 6C spectrum a).
Azithromycin bands were not resolved in ML as evident from the comparison of ML spectra from treated (Fig. 6D spectra a and f) and untreated (Fig. 6D spectra b and g) subjects when silver (Fig. 6D spectra a and b) or cesium (Fig. 6D spectra e and f) were used in the matrix. Azithromycin was visible with wax that was spiked with azithromycin (data not shown). We conclude that azithromycin is either present below the MALDI-TOF detection limit of 1 ρmole per mg of ML or is absent in ML from subjects treated with azithromycin.
Discussion
This study confirms the clinical response of MGD to topical azithromycin ophthalmic solution therapy and correlates the clinical improvement with analytical improvement in spectroscopic measures of lipid behavior.
Changes in lipid composition published by other investigators for subjects with MGD have recorded alterations in the neutral to polar lipid profile.23 Unsaturation of fatty acids associated with phospholipids in subjects with meibomianitis has been reported as have differences in the concentration of oleic acid in meibum from those with MGD when compared to normal subjects.24,25 These same investigators also found increases in the mono-unsaturated fatty acids from patient wax/sterol esters compared with normal subjects.26 Other changes especially in fatty acid composition with MGD have been observed.27,28 Such observed alterations in lipid composition in subjects with MGD could contribute to abnormalities in lipid behavior.
Of great interest is the demonstrated improvement in degree of lipid ordering and correlative change in phase transition temperature of meibum with therapy, particularly with respect to the amount of meibomian gland orifice plugging and the character of the meibomian gland secretion observed clinically. Phase transition temperature, although not equivalent to melting temperature, is an indication of the mobility of the lipid secretion and a lower phase transition temperature would likely be associated with greater movement of lipid secretion from the duct of the gland to the tear film and ocular surface.29 A higher content of trans rotomers (higher lipid order) would result in stronger lipid-lipid interactions. Stronger lipid-lipid interactions could result in a lower surface pressure which would impede ML spreading on the aqueous tear film surface causing lowered tear breakup time.30
The trend for improvement in the spectroscopic measures of lipid behavior even after discontinuation of topical azithromycin application may indicate that azithromycin persists in the eyelid tissue to influence meibomian gland function despite absence of measurable azithromycin in the meibum itself. Further investigations are needed to confirm this possibility. The duration of effect is consistent with data from previous studies in rabbits that demonstrated measureable presence of azithromycin in eyelid tissue up to twelve days after discontinuation of topical application when delivered in the Durasite vehicle.31
Azithromycin was not identified in meibomian secretions of treated subjects by MALDI-TOF techniques that were shown capable of identifying azithromycin in control samples spiked with azithromycin at a level of 1 ρmole/mg ML. It is possible that breakdown products of metabolized azithromycin were present but not identified by the MALDI-TOF method. Whether other analytic methods such as Raman spectroscopy or NMR might identify azithromycin in ML has not been determined and could be the focus of future studies. Isotopically labeled drug could be used in future studies.
The improvement in the signs of redness and swelling of the eyelid margin could result from the antibacterial effect of azithromycin reducing bacterial presence or to the known anti-inflammatory properties of azithromycin. The improvement of the degree of meibomian gland orifice plugging and the character of meibomian gland secretion is, however, more likely due to a physical change in the meibum. The mechanism of action of azithromycin on meibomian gland lipid may be related to inhibition of tissue or bacterial lipases that otherwise degrade the lipid structure.27,32,33 Indeed, it is known that the anti-lipase effect of azithromycin occurs with levels of drug that are less than levels required for bacterial eradication.33 Further studies to clarify the mechanism of action are needed.
Conclusion
This clinical trial indicates that topically applied azithromycin in durasite vehicle instilled on a once daily basis for four weeks achieves clinical control or improvement in symptoms and signs of MGD as well as improvement in the spectroscopically measured behavior of meibomian gland lipids. The correlation of improvement in phase transition temperature of the meibomian gland lipid with the determined percent trans rotomer composition of the lipid strongly suggests that the ordering of the lipid molecules is altered in the disease state (MGD) and that azithromycin can improve that abnormal condition toward normal in a manner that correlates with clinical response to therapy.
Acknowledgments
Supported by Public Health Service research grant EY017094-03 (Bethesda, MD., U.S.A.), the Kentucky Lions Eye Foundation, an unrestricted grant from Research to Prevent Blindness Inc., and a grant from Inspire Pharmaceuticals, Inc.
Much of this material is the result of work supported with resources and use of the facilities at the Louisville Veterans Affairs Medical Center, Louisville, KY. Dr Foulks is a member of the part-time staff of the Surgical Service, Department of Veteran Affairs Medical Center, Louisville, KY.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lemp M, Baudouin C, Baum J, et al. The definition and classification of dry eye disease: Report of the definition and classification subcommittee of the International Dry Eye WorkShop (2007) The Ocular Surface. 2007;5:75–92. doi: 10.1016/s1542-0124(12)70081-2. [DOI] [PubMed] [Google Scholar]
- 2.Borchman D, Foulks GN, Yappert MC, et al. Temperature-induced conformational changes in human tear lipids hydrocarbon chains. Biopolymers. 2007;87:124–133. doi: 10.1002/bip.20798. [DOI] [PubMed] [Google Scholar]
- 3.Wojtowicz JC, Butovich I, McCulley JP. Historical brief on human meibum lipids composition. The Ocular Surface. 2009;7:145–153. doi: 10.1016/s1542-0124(12)70309-9. [DOI] [PubMed] [Google Scholar]
- 4.Borchman D, Foulks GN, Yappert MC, et al. Factors affecting evaporation rates of tear film components measured in vitro. Eye Contact Lens. 2009;35:32–7. doi: 10.1097/ICL.0b013e318193f4fc. [DOI] [PubMed] [Google Scholar]
- 5.Mathers WD. Ocular evaporation in meibomian gland dysfunction and dry eye. Ophthalmology. 1993;100:347–51. doi: 10.1016/s0161-6420(93)31643-x. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan DA, Sullivan BD, Evans JE, et al. Androgen deficiency, meibomian gland dysfunction, and evaporative dry eye. Ann NY Acad Sci. 2002;966:211–22. doi: 10.1111/j.1749-6632.2002.tb04217.x. [DOI] [PubMed] [Google Scholar]
- 7.Paranjpe DR, Foulks GN. Therapy of meibomian gland disease. Ophthalmol Clin NA. 2003;16:37–42. doi: 10.1016/s0896-1549(02)00106-2. [DOI] [PubMed] [Google Scholar]
- 8.John T, Shah AA. Use of azithromycin ophthalmic solution in the treatment of chronic mixed anterior blepharitis. Ann Ophthalmol (Skokie) 2008;40:68–74. [PubMed] [Google Scholar]
- 9.Luchs J. Efficacy of topical azithromycin ophthalmic solution 1% in the treatment of posterior blepharitis. Adv Ther. 2008;25:858–70. doi: 10.1007/s12325-008-0096-9. [DOI] [PubMed] [Google Scholar]
- 10.Wagner RS, Jamison T, Bell B, et al. The pharmacodynamic properties of azithromycin in a kinetics-of-kill model and implications for bacterial conjunctivitis treatment. Adv Ther. 2008;25:208–17. doi: 10.1007/s12325-008-0034-x. [DOI] [PubMed] [Google Scholar]
- 11.Kilp H, Schmid E, Kirchner L, Pohl A. In: The Preocular Tear Film in Health, Disease and Contact Lens Wear. Holly FJ, editor. The Dry Eye Institute; Lubbock: 1986. p. 564. [Google Scholar]
- 12.Borchman D, Foulks GN, Yappert MC, et al. Spectroscopic evaluation of human tear lipids. Chem Phys Lipids. 2007;147:87–102. doi: 10.1016/j.chemphyslip.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Borchman D, Yappert MC, Herrell P. Structural characterization of human lens membrane lipid by infrared spectroscopy. Invest Ophthalmol Vis Sci. 1991;32:2404–2416. [PubMed] [Google Scholar]
- 14.Borchman D, Tang D, Yappert MC. Lipid composition, membrane structure relationships in lens and muscle sarcoplasmic reticulum membranes. Biospectroscopy. 1999;5:151–167. doi: 10.1002/(SICI)1520-6343(1999)5:3<151::AID-BSPY5>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 15.Borchman D, Yappert MC, Afzal M. Lens lipids and maximum lifespan. Exp Eye Res. 2004;79:761–768. doi: 10.1016/j.exer.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Borchman D, Cenedella RI, Lamba OP. Role of cholesterol in the structural order of lens membrane lipids. Exp Eye Res. 1996;62:191–197. doi: 10.1006/exer.1996.0023. [DOI] [PubMed] [Google Scholar]
- 17.Moore DJ, Wyrwa M, Reboulleau CP, et al. Quantitative IR studies of acyl chain conformational order in fatty acid homogeneous membranes of live cells of Acholeplasma laidlawii B. Biochemistry. 1993;32:6281–6287. doi: 10.1021/bi00075a023. [DOI] [PubMed] [Google Scholar]
- 18.Popova AV, Hincha DK. Intermolecular interactions in dry and rehydrated pure and mixed bilayers of phosphatidylcholine and digalactosyldiacylglycerol: a Fourier transform infrared spectroscopy study. Biophys J. 2003;85:1682–1690. doi: 10.1016/S0006-3495(03)74598-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Casal HL, Mantsch HH. Polymorphic phase behaviour of phospholipid membranes studied by infrared spectroscopy. Biochim Biophys Acta. 1984;779:381–401. doi: 10.1016/0304-4157(84)90017-0. [DOI] [PubMed] [Google Scholar]
- 20.Mantsch HH, McElhaney RN. Phospholipid phase transitions in model and biological membranes as studied by infrared spectroscopy. Chem Phys Lipids. 1991;57:213–226. doi: 10.1016/0009-3084(91)90077-o. [DOI] [PubMed] [Google Scholar]
- 21.Kóta Z, Debreczeny M, Szalontai B. Separable contributions of ordered and disordered lipid fatty acyl chain segments to CH2 bands in model and biological membranes: a Fourier transform infrared spectroscopic study. Biospectroscopy. 1999;5:169–178. doi: 10.1002/(SICI)1520-6343(1999)5:3<169::AID-BSPY6>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 22.Estrada R, Borchman D, Reddan J, et al. In Vitro and In Situ Tracking of Choline-Phospholipid Biogenesis by MALDI TOF-MS. Anal Chem. 2006;78:1174–1180. doi: 10.1021/ac051540n. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan DA, Sullivan BD, Evans JE, et al. Androgen deficiency, Meibomian gland dysfunction, and evaporative dry eye. Ann N Y Acad Sci. 2002;966:211–22. doi: 10.1111/j.1749-6632.2002.tb04217.x. [DOI] [PubMed] [Google Scholar]
- 24.Shine WE, McCulley JP. Polar lipids in human meibomian gland secretions. Curr Eye Res. 2003;26:89–94. doi: 10.1076/ceyr.26.2.89.14515. [DOI] [PubMed] [Google Scholar]
- 25.Shine WE, McCulley JP. Association of meibum oleic acid with meibomian seborrhea. Cornea. 2000;19:72–4. doi: 10.1097/00003226-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Dougherty JM, Osgood JK, McCulley JP. The role of wax and sterol ester fatty acids in chronic blepharitis. Invest Ophthalmol Vis Sci. 1991;32:1932–7. [PubMed] [Google Scholar]
- 27.Ong BL, Larke JR. Meibomian gland dysfunction: some clinical, biochemical and physical observations. Ophthalmic Physiol Opt. 1990;10:144–148. doi: 10.1111/j.1475-1313.1990.tb00968.x. [DOI] [PubMed] [Google Scholar]
- 28.Joffre C, Souchier M, Gregoire S, et al. Differences in meibomian fatty acid composition in patients with meibomian gland dysfunction and aqueous-deficient dry eye. Br J Ophthalmol. 2008;92:116–119. doi: 10.1136/bjo.2007.126144. [DOI] [PubMed] [Google Scholar]
- 29.Nagymihalyi A, Dikstein S, Tiffany JM. The influence of eyelid temperature on the delivery of meibomian oil. Exp Eye Res. 2004;78:367–370. doi: 10.1016/s0014-4835(03)00197-0. [DOI] [PubMed] [Google Scholar]
- 30.Holly FJ. Formation and rupture of the tear film. Exp Eye Res. 1973;15:515–25. doi: 10.1016/0014-4835(73)90064-x. [DOI] [PubMed] [Google Scholar]
- 31.Akpek EK, Vittitow J, Verhoeven RS, Brubaker K, Amar T, Powell KD, Boyer JL, Crean C. Ocular surface distribution and pharmacokinetics of a novel ophthalmic 1% azithromycin formulation. J Ocul Pharmacol Ther. 2009 Oct;25(5):433–9. doi: 10.1089/jop.2009.0026. [DOI] [PubMed] [Google Scholar]
- 32.Dougherty JM, McCulley JP, Silvany RE, Meyer DR. The role of tetracycline in chronic blepharitis-Inhibition of lipase production in staphylococci. Invest Ophthalmol Vis Sci. 1991;32:2970–5. [PubMed] [Google Scholar]
- 33.Molinari G, Guzman CA, Pesce A, Schito GC. Inhibition of Pseudomonas aeruginosa virulence factors by subinhibitory concentrations of azithromycin and other macrolide antibiotics. Jour Antimicrobial Chemo. 1993;31:681–8. doi: 10.1093/jac/31.5.681. [DOI] [PubMed] [Google Scholar]