Abstract
This study developed a new measure of medication affordability that examines out-of-pocket drug expenses relative to available household resources. The authors assessed the spending patterns of ~2.1 million poor households (≤100% federal poverty level) of adults aged 51 and older by Medicaid status. The data were drawn from the 2000–2001 Health and Retirement Study. Household spending was categorized into three broad types: basic living, health care, and discretionary. Older (aged 51 or older) poor households without Medicaid allocated about 72% of their total resources ($17,421, SE $783) to basic living needs. In comparison, those with Medicaid had scarcer total resources ($12,498, SE $423) and allocated 85% to basic living needs. Medication costs consumed the largest proportion of health care expenses for both types of poor households (Medicaid: $463, SE $67; non-Medicaid: $970, SE $102). After paying for basic living needs and health care costs, these families had, on average, only $16 left each week. Poor families have very few resources available for anything beyond basic living needs, even when they have Medicaid coverage. There is no great reservoir of discretionary funds to pay for increases in cost-sharing under Medicaid and Medicare Part D.
Keywords: Affordability, low-income, prescription drugs
INTRODUCTION
Although appropriate use of prescription drugs can substantially improve health status, accessing these treatments may sometimes consume catastrophic proportions of available income. Even modest drug cost-sharing has the potential to endanger a poor family’s ability to pay for the basic necessities of life when discretionary income is scarce (Nelson, Reeder, & Dickson, 1984; Soumerai, Ross-Degnan, Fortess, & Abelson, 1993). Recent surveys have shown that low-income households often cut back on basic necessities or take less medication than prescribed due to out-of-pocket drug costs (Mojtabai & Olfson, 2003; Piette, Heisler, & Wagner, 2004a; Rector & Venus, 2004; Safran et al., 2002, 2005). Family budgets in low-income households are very tight, dominated by basic living needs for housing, food, and transportation. Research has shown that incomes at even 200% of the federal poverty level (FPL) cannot be stretched to meet these basic living needs, much less accommodate increasing medication costs (Boushey, Brocht, Gundersen, & Bernstein, 2001).
Little is known, however, about how much low-income individuals can pay for medications without forcing families into financial crisis, yet the trend in public policy is to increase drug cost-sharing. Most states currently charge adult Medicaid recipients a co-payment for prescription drugs that ranges from a low of $0.50 to a high of $10 for branded drugs in the state of Arizona (Crowley, Ashner, & Elam, 2003). Over the course of a year, these co-payments may accumulate into considerable sums, as individuals in this population receive an average of over 35 prescriptions per year (Mathematica Policy Research, 2004). The new Medicare Modernization Act of 2003 (MMA) also requires cost-sharing of Medicare beneficiaries who enroll in the new drug benefit, including those with the lowest incomes. In general, cost-sharing was included in the policy to make the Medicare benefit similar in structure to private health insurance and to promote “personal responsibility” by making people accountable for part of the costs of their care. Dual-eligible (Medicare and Medicaid) beneficiaries with incomes less than 135% of the FPL ($12,920 for individuals in 2005) qualify for premium subsidies yet must pay $1 to $5 per prescription. Estimates of the out-of-pocket drug costs to dual-eligible beneficiaries range from $94 to $742 in 2006 (Mays, Brenner, Neuman, Cubanski, & Claxton, 2004; The Henry J. Kaiser Family Foundation, 2003). As the program evolves, cost-sharing is expected to increase, since the MMA stipulates that drug co-payments must be indexed to growth in per capita drug costs. In addition, since the majority of state Medicaid programs currently charge $0 or $1 prescription co-payments for generics, average levels of cost-sharing are expected to increase after dual-eligible beneficiaries transition to the Medicare drug benefit (Crowley, Ashner, & Elam, 2003).
Ability to pay given competing demand for resources is an important concept for understanding the true out-of-pocket burden of both routine and potentially catastrophic medication costs. The theory of welfare economics holds that individuals are the best judges of their welfare, but it also raises questions about what is reasonable for individuals to sacrifice. In the case of health care, it is widely accepted that individuals should be protected from catastrophic health care costs and not expected to endure impoverishment to cope with health care costs (Kawabata, Xu, & Carrin, 2002). In practice, health care spending is identified as catastrophic in at least two ways: (1) an absolute level of costs independent of available personal resources (e.g., the Medicare Part D specifies catastrophic drug costs as being greater than $5,100) or (2) a relative cost threshold determined explicitly according to available resources (Berki, 1986; Wyszewianski, 1986). The second view is less explored in policy and research, in part due to the lack of information about the costs of living. Nevertheless, accounting for necessary household expenditures may be a valuable way for assessing the true affordability of medications.
The affordability of prescription drug cost-sharing has been estimated in one of four ways. The first is the proportion of people reporting problems in purchasing prescribed medications due to cost (e.g., as measured in the Medicare Current Beneficiary Survey and the National Health Interview Survey; Craig, Kreling, & Mott, 2003; Kennedy, Coyne, & Sclar, 2004; Safran et al., 2005). A second method is to assess reductions in essential medication use following increases in co-payments (Soumerai, Ross-Degnan, Avorn, McLaughlin, & Choodnovskiy, 1991; Tamblyn et al., 2001). Both of these measures most likely underestimate the problem of affordability as they do not capture the many strategies families use to afford medications, such as reducing other household spending. The third approach is to calculate the proportion of people with large shares of income spent on medication costs (e.g., measured as a cost-to-income ratio; Gross et al., 1999). This measure is also problematic because income reported in household surveys does not generally reflect a household’s true purchasing power (Xu et al., 2003). There is also no consensus on the threshold that indicates when burdensome costs become catastrophic; estimates vary from 5% to more than 20% of household income (Goldman & Smith, 2001; Hwang, Weller, Ireys, & Anderson, 2001; Rogowski, Lillard, & Kington, 1997). None of these three approaches provides a nuanced picture of how much individuals can afford in out-of-pocket medication costs after paying for the basic living needs of food, housing, clothing, and transportation.
A fourth approach for measuring the burden of medication costs is to assess out-of-pocket drug expenses relative to the household’s capacity to pay given basic living expenditures, or its “effective income” (Xu et al., 2003). Effective income is the amount remaining from the household’s total resource consumption after expenditures for food, clothing, housing, and transportation.
The purpose of this pilot study is to examine the out-of-pocket medication spending of older poor families in relationship to their capacity to pay for anything else beyond basic living needs. We selected two groups for this study, poor families with Medicaid and those without Medicaid to demonstrate the extent to which Medicaid protects older adults against catastrophic medication costs. These groups are also important for understanding the performance of our measure under the circumstances of generous drug coverage, although our future goal is to assess catastrophic expenditure risk for at-risk groups. In addition, we assessed the sensitivity of the measure to self-assessed health status, although we anticipated significant differences in the out-of-pocket costs for only the non-Medicaid population due to the comprehensive drug coverage of Medicaid.
METHODS
We used the Health and Retirement Study (HRS), a longitudinal panel survey of adults aged 51 and older. The HRS has been sponsored by the National Institute on Aging since 1992 (Juster & Suzman, 1995; Willis, 1999). The survey gathers information on the economics, demographics, and health care of aging. Since economic well-being is a main focus, the HRS uses state-of-the-art survey bracketing techniques to provide high-quality data on income and wealth (Goldman & Zissimopoulos, 2003). The interviews are conducted in the home and follow-up surveys occur every other year. By design, the survey oversamples Blacks, Hispanics, and residents of Florida, and it provides sampling weights scaled to the Current Population Survey (CPS) for yielding United States population estimates for older adults. In 2000, 10,371 individuals participated in the HRS.
Our analysis merged the 2000 HRS core survey files with the 2001 supplemental HRS module, known as the Consumption and Activities Mail Survey (CAMS). The CAMS asks participants to estimate household spending for major budget items, such as mortgage, food, or clothing, and it was sent to 5,000 households interviewed in the 2000 HRS core survey (with a response rate of 77%). The merged data set provides a broad array of information on the demographics, health status, insurance status, health care, household expenditures, income, and medication use for approximately 3,800 households of older adults.
We restricted our study sample to households in which the main HRS respondent or the spouse/partner reported Medicaid coverage in 2000 or in which the household income was at or below 100% of the 2001 FPL. In addition, the household must have provided responses to the 2001 CAMS. We allowed for only one respondent per household and excluded households in which respondents died or entered nursing homes before the end of the observation period (n=11). For individual-level assessments, such as sex, age, or health, we selected the value reported by the main HRS respondent.
We applied the 2001 CPS inflation factor of 1.0285 to impute the 2001 income. All spending values were trimmed at the 95% quintile as the HRS does not topcode extreme and unlikely values and initial assessments showed that our measure was sensitive to outliers given the small sample (Institute for Social Research, 2002).
Our analysis categorized expenditures into three broad types that are patterned after those used in the Bureau of Labor Statistics Consumer Expenditure Survey: basic living needs, health-related expenses, and discretionary spending (Tan, 2000). This categorization scheme does not imply that health-related expenses are less important than basic living needs. Rather, the categories have been developed to show that increases in health care spending for people with fixed incomes can come only from resources that have been allocated to discretionary or basic living expenditures. Basic living expenditures comprised food, clothing, housing (mortgage/rent, home insurance, property tax, housing supplies/maintenance, utilities), and transportation (car payments, auto insurance, gas, and service maintenance). Discretionary expenditures comprised dining out, vacations, tickets, hobbies, contributions, and gifts. Health-related expenditures comprised prescription and over-the-counter drugs, hospital care, health professional services, lab tests, eye care, dental services, and health insurance premiums. We assessed the effective income of each household by summing all spending and subtracting basic living needs costs. Then we assessed the affordability of medication and other health care costs by comparing spending levels on these items to the household’s effective income.
We also conducted subanalyses of the sample stratified into single- and multiple-person households to isolate cases in which household spending was incurred solely by a single Medicaid recipient. These estimates are not reported here, but analyses showed similar relationships to those with the total sample and are available upon request. All estimates were generated using the survey’s sampling weights, and standard errors were corrected for the clustered sampling design.
RESULTS
We identified 647 respondents, representing nearly 1 million households of older adults with Medicaid coverage and another 1.1 million with poverty-level income who are not yet covered by Medicaid. Table 1 shows that the average 2001 household income for older poor families was $11,528 with Medicaid and $7,860 without Medicaid. Most of these households consisted of at least two people, and around 10% of them were supporting children. Compared to people in the non-Medicaid households, those in the Medicaid homes were more often of minority race and Hispanic ethnicity, had much lower levels of education, and less often owned their home. People in the Medicaid households also reported poorer levels of health; one in four (26.3%) rated their health status as poor compared to 9.3% of people in non-Medicaid homes.
TABLE 1.
Description of Study Population
| Medicaid | Non-medicaid (≤100% 2001 FPL) | |
|---|---|---|
| Population size (unweighted n) | 996,000 (297) | 1,147,000 (350) |
| 2001 household income (SE) | $11,582 ($856) | $7,860 ($266) |
| Household characteristics | ||
| Average number of co-residents | 2.1 | 2.5 |
| % with co-residents younger than 18 | 9.6 | 16.0 |
| Respondent characteristics | ||
| % aged ≥65 | 46.5 | 50.0 |
| % female | 78.0 | 79.3 |
| % race | ||
| White/Caucasian | 68.2 | 77.8 |
| Black/African American | 21.4 | 17.5 |
| Other | 10.3 | 4.7 |
| % Hispanic | 20.1 | 12.2 |
| % with less than high school diploma/GED | 62.8 | 37.8 |
| % self-reported health status | ||
| Poor | 26.3 | 9.3 |
| Good/fair | 61.1 | 53.9 |
| Very good/excellent | 12.6 | 36.8 |
| % covered by Medicare | 58.8 | 50.6 |
| % homeowner | 35.1 | 55.6 |
| % census region | ||
| Northeast | 19.7 | 17.1 |
| Midwest | 18.9 | 24.9 |
| South | 44.1 | 44.8 |
| West | 17.0 | 13.2 |
| Average household expenditures (SE) | $12,498 ($423) | $17,421 ($783) |
| Basic living needs expenses | ||
| Food | $3,079 ($214) | $2,788 ($138) |
| Housing | $5,471 ($199) | $6,795 ($356) |
| Clothes/personal care | $523 ($59) | $686 ($71) |
| Transportationa | $937 ($69) | $2,151 ($151) |
| Discretionary expensesb | $703 ($72) | $2,475 ($208) |
| Health care expenses | ||
| Prescription/over-the-counter medications | $463 ($67) | $970 ($102) |
| Health services | $175 ($25) | $735 ($86) |
| Medical supplies | $113 ($20) | $240 ($42) |
| Health insurance premiums | $346 ($34) | $956 ($82) |
Note. From 2000–2001 HRS/CAMS (Juster & Suzman, 1995).
Transportation expenses include car payments, auto insurance, gas, and service maintenance.
Discretionary expenses include dining out, vacations, tickets, hobbies, contributions, and gifts.
The average annual total expenditures for older poor households were $12,498 with Medicaid and $17,421 without Medicaid. For items classified as basic living needs, non-Medicaid families generally spent more than Medicaid families across the board but especially for housing ($6,795 versus $5,471) and transportation ($2,151 versus $937). Discretionary expenditures averaged around $703 for Medicaid families and $2,475 for non-Medicaid families. The highest category of health care expenses in both groups was prescription and over-the-counter medications (Medicaid: $463; non-Medicaid: $970), followed by health insurance premiums (Medicaid: $346; non-Medicaid: $956).
Figure 1 demonstrates that older poor households generally allocate most of their resources to basic living needs, regardless of absolute spending level or Medicaid status. Medicaid households at the top 90th quintile of spending devoted 82% of their resources to basic living needs expenditures, 8% to health-related expenses, and 10% to discretionary items. This proportional allocation remained fairly constant across the entire distribution of total spending in Medicaid households. In comparison, non-Medicaid households at the top 90th quintile of spending devoted 65% of their resources to basic living needs expenditures, 13% to health-related expenses, and 22% to discretionary items. However, in the bottom 10th quintile, the families without Medicaid spent a larger share of resources on health care (18%), followed by 11% on discretionary items after expending 71% on basic living needs.
FIGURE 1.
Household spending allocations of poor households aged 51 and over, 2001 (from 2000–2001 HRS/CAMS; Juster & Suzman, 1995).
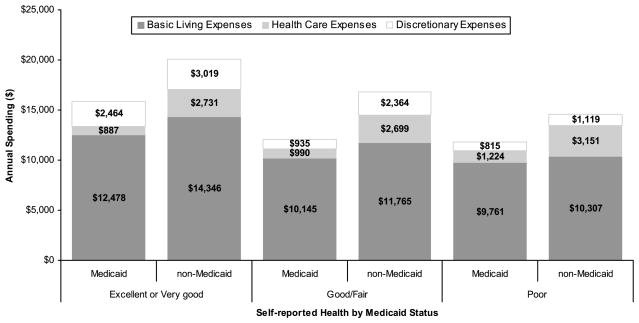
Figure 2 illustrates how poor health influences the household spending of poor families. In general, Medicaid households substantially spent substantially more for health care as health status declined, especially from good/fair ($990) to poor ($1,224). Conversely, as demand for medical care increased, spending for both basic living needs and discretionary items decreased, as did total spending. A similar pattern is also observed for the non-Medicaid households, although their average total spending amounts are always higher than the amounts spent by average Medicaid households at the same level of health status.
FIGURE 2.
Influence of health status on household spending of poor households aged 51 and over, 2001 (from 2000–2001 HRS/CAMS; Juster & Suzman, 1995).
After paying for the basic living needs of food, clothing, housing, and transportation, older households with Medicaid had about $1,800 per year available to pay for health care costs, including medications, and any discretionary expenses such as entertainment (Figure 3). Poor families without Medicaid had $5,229 per year available for nonbasic living needs expenditures. Figure 3 shows that the greater share of available resources (effective income) in older poor households are consumed by medical costs, particularly medications, as health status declines. For Medicaid families, medication expenditures increased dramatically from 9% to 30% of available resources as health status declined from excellent/very good to poor. Similarly, for non-Medicaid families, medication expenditures increased from 15% to 31% of effective income as health worsened. Other nondrug health care expenses were less sensitive to health status and fell within a range of 9% to 18% of non–basic living household expenditures in both Medicaid and non-Medicaid families.
FIGURE 3.
Proportion of effective income spent by poor households aged 51 and over on medical care, 2001 (from 2000–2001 HRS/CAMS; Juster & Suzman, 1995).
DISCUSSION
This study is the first to directly measure the burden represented by out-of-pocket medication expenses faced by low-income households after paying for basic living expenses of food, clothing, transportation, and housing costs. Our analysis illustrated that poor families have very few resources available for anything beyond basic living needs, even when they have Medicaid coverage. There was no great reservoir of discretionary funds to pay for increases in cost-sharing under Medicaid and Medicare Part D. We also found that these households spend a relatively large proportion of their available resources on medicines and other health care costs and that Medicaid provided less than comprehensive protection against these expenses. This pattern held true for both single-person and multiple-person Medicaid households. We found that the large allocation of household expenditures to medications increased considerably with worsening health, to a high of 30% of non–basic living needs expenditures in both Medicaid and non-Medicaid families reporting poor health. In other words, after paying for basic living expenses and health care costs, older Medicaid families in poor health had, on average, only $16 each week for any discretionary purposes. Older non-Medicaid families in poor health had only $22 left each week after paying for basic living needs and medical care costs. This burden will more than likely worsen in the future as individuals reporting poor health are at high risk for dying or requiring additional health care resources (Desalvo, Fan, McDonell, & Fihn, 2005).
Does our conceptual framework of “basic living needs” versus “discretionary” expenditures offer valid insights? Clearly, it is intuitively appealing to assess health care policies against the protection they offer to sick families in need of food, clothing, housing, and transportation. However, it may also be true that spending for basic living needs contains discretionary components (e.g., steak vs. hamburger). In fact, our analyses showed little evidence of optional spending within the basic living needs categories. For food costs, our single-person Medicaid homes spent only $38 per week, while the multiple-person Medicaid homes spent $75 per week to feed three people. It should be noted, however, that the consumption portion of the HRS does not identify whether food stamps were used for these expenses and helped in stretching the family budget for food. For housing costs, their monthly costs ranged from only $362 to $522. Single- and multiple-person non-Medicaid homes spent between $474 and $604 on monthly housing costs and $43 to $58 on weekly food purchases.
The results of this study should be interpreted in light of the strengths and weaknesses of the HRS data. We detected considerable discrepancies between the reported incomes of poor households and their reported expenditure levels. For instance, Medicaid households at the median of household income (~$7,689) reported approximately $11,030 in expenses. This finding has been noted elsewhere with other expenditure surveys of low-income families (Tan, 2000). A possible reason for the discrepancy is the under-reporting of income by respondents, although the HRS employs bracketed survey techniques to collect these income data that provide more reliable estimates (Juster & Suzman, 1995). Other possible explanations include poor families who may be drawing on their limited savings to make necessary expenditures, purchasing items on credit, or borrowing money or receiving assistance from family members or friends. Furthermore, our estimates of household expenditures are lower than those reported in the 2001 Consumer Expenditure Survey. In that survey, households with incomes of $5,000 to $9,999 spent, on average, $16,625 (compared to our $12,498), while those making $10,000 to $14,999 spent $20,642 (compared to our $17,421; U.S. Department of Labor Bureau of Labor Statistics, 2003).
Given the overall population focus of the HRS, our sample was highly selective, which resulted in relatively small sample sizes. Because of this, we limited our analysis to larger subgroups, such as spending quintiles, and we present only bivariate relationships. Future work should replicate these results with larger populations, account for overall wealth, and use multivariate techniques to explore the relationships between ability to pay and key demographic and socioeconomic factors.
It is particularly important to isolate the effects of poor health status on potentially catastrophic health care costs from those of other factors such as older age or lower income. In addition, the impact of out-of-pocket payments for medications is not fully captured by examining levels of spending. Some poor households without access to non-income resources must forego necessary care rather than incur further debt (Piette, Heisler, & Wagner, 2004b; Rector & Venus, 2004) Also, a frequently reported strategy for avoiding medication costs is to obtain free samples from physicians or to gain access to pharmaceutical company free care programs (Cox, Jernigan, Coons, & Draugalis, 2001). Households that relied upon such strategies to maintain required therapy would have reported lower levels of medication spending in our analyses (Soumerai, Ross-Degnan, Avorn, McLaughlin, & Choodnovskiy, 1991; Tamblyn et al., 2001). Similarly, households that forego medications because of costs would have spending levels that underestimate their required need. However, our estimate of $463 for out-of-pocket medication spending for dual-eligible beneficiaries in the HSR compares reasonably well with our internal estimate of $330 for the same group in the 2001 Medicare Current Beneficiary Survey and an external estimate of $510 from the 2003 Medical Expenditure Panel Survey (The Henry J. Kaiser Family Foundation, 2003). Last, our analysis did not account for spending on taxes, as these data are not captured in the HRS. This may have resulted in an overestimation of available income, but only for the few households with gross incomes above the taxation thresholds (Butrica, Goldwyn, & Johnson, 2005).
Our findings have implications for estimating how much older poor adults can afford to pay for medications, especially in light of their transition to the MMA rules after January 2006 (Crowley, Ashner, & Elam, 2003). Of particular concern are Medicaid households that had been paying $0.50 to $1.00 co-payments per prescription or even requesting Medicaid co-payment waivers. Even with the more generous coverage before Part D, they were still devoting between 9% and 30% of available non–basic living needs resources to medications. Given these slim margins, it is difficult to know how these households will manage the co-payment increases under the MMA. Those who continue to participate in Medicaid will likely face higher cost-sharing and, consequently, greater financial burden as states attempt to reign in escalating drug costs.
It is important to remember that our Medicaid-enrolled study population had fairly complete health and drug coverage. Disparities in household income and spending for health care are likely to be far greater for the poor and near-poor Medicare beneficiaries who are not eligible for Medicaid or for other public insurance programs with drug benefits. Policies that do not account for a household’s available resources and ability to pay for cost-sharing for medications may have serious negative consequences for important subgroups of the poor and near poor, even those with insurance coverage.
Footnotes
Publisher's Disclaimer: Full terms and conditions of use: http://www.informaworld.com/terms-and-conditions-of-access.pdf
This article may be used for research, teaching and private study purposes. Any substantial or systematic reproduction, re-distribution, re-selling, loan or sub-licensing, systematic supply or distribution in any form to anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents will be complete or accurate or up to date. The accuracy of any instructions, formulae and drug doses should be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims, proceedings, demand or costs or damages whatsoever or howsoever caused arising directly or indirectly in connection with or arising out of the use of this material.
Contributor Information
BECKY BRIESACHER, Division of Geriatric Medicine, University of Massachusetts Medical School, Worchester, Massachusetts, USA.
DENNIS ROSS-DEGNAN, Harvard Medical School and Harvard Pilgrim Health Care, Boston, Massachusetts, USA.
ALYCE ADAMS, Harvard Medical School and Harvard Pilgrim Health Care, Boston, Massachusetts, USA.
ANITA WAGNER, Harvard Medical School and Harvard Pilgrim Health Care, Boston, Massachusetts, USA.
JERRY GURWITZ, Division of Geriatric Medicine, University of Massachusetts Medical School, Worchester, Massachusetts, USA.
STEPHAN SOUMERAI, Harvard Medical School and Harvard Pilgrim Health Care, Boston, Massachusetts, USA.
References
- Berki SE. A look at catastrophic medical expenses and the poor. Health Affairs (Millwood) 1986;5(4):138–145. doi: 10.1377/hlthaff.5.4.138. [DOI] [PubMed] [Google Scholar]
- Boushey H, Brocht C, Gundersen B, Bernstein J. Hardships in America: The real story of working families. Washington, DC: Economic Policy Institute; 2001. [Google Scholar]
- Butrica BA, Goldwyn JH, Johnson RW. Understanding expenditure patterns in retirement. Washington, DC: The Urban Institute; 2005. [Google Scholar]
- Cox ER, Jernigan C, Coons SJ, Draugalis JL. Medicare beneficiaries’ management of capped prescription benefits. Medical Care. 2001;39(3):296–301. doi: 10.1097/00005650-200103000-00009. [DOI] [PubMed] [Google Scholar]
- Craig BM, Kreling DH, Mott DA. Do seniors get the medicines prescribed for them? Evidence from the 1996–1999 Medicare Current Beneficiary Survey. Health Affairs (Millwood) 2003;22(3):175–182. doi: 10.1377/hlthaff.22.3.175. [DOI] [PubMed] [Google Scholar]
- Crowley JS, Ashner D, Elam L. Medicaid outpatient prescription drug benefits: Findings from a national survey, 2003. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2003. [Google Scholar]
- Desalvo KB, Fan VS, McDonell MB, Fihn SD. Predicting mortality and healthcare utilization with a single question. Health Services Research. 2005;40(4):1234–1246. doi: 10.1111/j.1475-6773.2005.00404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman DP, Smith JP. Methodological biases in estimating the burden of out-of-pocket expenses. Health Services Research. 2001;35(6):1357–1364. discussion 1365–1370. [PMC free article] [PubMed] [Google Scholar]
- Goldman DP, Zissimopoulos JM. High out-of-pocket health care spending by the elderly. Health Affairs (Millwood) 2003;22(3):194–202. doi: 10.1377/hlthaff.22.3.194. [DOI] [PubMed] [Google Scholar]
- Gross DJ, Alecxih L, Gibson MJ, Corea J, Caplan C, Brangan N. Out-of-pocket health spending by poor and near-poor elderly Medicare beneficiaries. Health Services Research. 1999;34(1 Pt 2):241–254. [PMC free article] [PubMed] [Google Scholar]
- Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Affairs (Millwood) 2001;20(6):267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- Institute for Social Research. Data description 2001 Consumption and Activities Mail Survey (CAMS) Ann Arbor: University of Michigan; 2002. [Google Scholar]
- Juster RT, Suzman R. An overview of the health and retirement study. The Journal of Human Resources. 1995;30(supplement):S7–S56. [Google Scholar]
- Kawabata K, Xu K, Carrin G. Preventing impoverishment through protection against catastrophic health expenditure. Bulletin of the World Health Organization. 2002;80(8):612. [PMC free article] [PubMed] [Google Scholar]
- Kennedy J, Coyne J, Sclar D. Drug affordability and prescription non-compliance in the United States: 1997–2002. Clinical Therapeutics. 2004;26(4):607–614. doi: 10.1016/s0149-2918(04)90063-x. [DOI] [PubMed] [Google Scholar]
- Mathematica Policy Research. Statistical compendium: Medicaid pharmacy benefit use and reimbursement in 1999. Rockville, MD: Centers for Medicare & Medicaid Services; 2004. [Google Scholar]
- Mays J, Brenner M, Neuman T, Cubanski J, Claxton G. Estimates of Medicare beneficiaries’ out-of-pocket drug spending in 2006. Washington, DC: The Henry J. Kaiser Family Foundation; 2004. [Google Scholar]
- Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Affairs. 2003;22(4):220–229. doi: 10.1377/hlthaff.22.4.220. [DOI] [PubMed] [Google Scholar]
- Nelson AA, Jr, Reeder CE, Dickson WM. The effect of a Medicaid drug copayment program on the utilization and cost of prescription services. Medical Care. 1984;22(8):724–736. doi: 10.1097/00005650-198408000-00004. [DOI] [PubMed] [Google Scholar]
- Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: The treatments people forgo, how often, and who is at risk. American Journal of Public Health. 2004a;94(10):1782–1787. doi: 10.2105/ajph.94.10.1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piette JD, Heisler M, Wagner TH. Cost-related medication under-use: Do patients with chronic illnesses tell their doctors? Archives of Internal Medicine. 2004b;164(16):1749–1755. doi: 10.1001/archinte.164.16.1749. [DOI] [PubMed] [Google Scholar]
- Rector TS, Venus PJ. Do drug benefits help Medicare beneficiaries afford prescribed drugs? Health Affairs (Millwood) 2004;23(4):213–222. doi: 10.1377/hlthaff.23.4.213. [DOI] [PubMed] [Google Scholar]
- Rogowski J, Lillard LA, Kington R. The financial burden of prescription drug use among elderly persons. Gerontologist. 1997;37(4):475–482. doi: 10.1093/geront/37.4.475. [DOI] [PubMed] [Google Scholar]
- Safran DG, Neuman P, Schoen C, Kitchman MS, Wilson IB, Cooper B, et al. Prescription drug coverage and seniors: Findings from a 2003 national survey. Health Affairs (Millwood) 2005:W5-152–W5-166. doi: 10.1377/hlthaff.w5.152. [DOI] [PubMed] [Google Scholar]
- Safran DG, Neuman P, Schoen C, Montgomery JE, Li W, Wilson IB, et al. Prescription drug coverage and seniors: How well are states closing the gap? Health Affairs (Millwood), Supp Web Exclusives. 2002:W253–W268. doi: 10.1377/hlthaff.w2.253. [DOI] [PubMed] [Google Scholar]
- Soumerai SB, Ross-Degnan D, Avorn J, McLaughlin T, Choodnovskiy I. Effects of Medicaid drug-payment limits on admission to hospitals and nursing homes. New England Journal of Medicine. 1991;325(15):1072–1077. doi: 10.1056/NEJM199110103251505. [DOI] [PubMed] [Google Scholar]
- Soumerai SB, Ross-Degnan D, Fortess EE, Abelson J. A critical analysis of studies of state drug reimbursement policies: Research in need of discipline. Milbank Quarterly. 1993;71(2):217–252. [PubMed] [Google Scholar]
- Tamblyn R, Laprise R, Hanley JA, Abrahamowicz M, Scott S, Mayo N, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. Journal of the American Medical Association. 2001;285(4):421–429. doi: 10.1001/jama.285.4.421. [DOI] [PubMed] [Google Scholar]
- Tan L. Spending patterns of public-assisted families. Monthly Labor Review. 2000;123(5):29–35. [Google Scholar]
- The Henry J. Kaiser Family Foundation. Medicare and prescription drug spending chartpack (Report No. 6087) Washington, DC: The Henry J. Kaiser Family Foundation; 2003. [Google Scholar]
- U.S. Department of Labor, Bureau of Labor Statistics. Consumer expenditures in 2001 (Report No. 966) Washington, DC: Bureau of Statistics; 2003. [Google Scholar]
- Willis RJ. Theory confronts data: How HRS is shaped by the economics of aging and how the economics of aging will be shaped by the HRS. Labour Economics. 1999;9:119–145. [Google Scholar]
- Wyszewianski L. Financially catastrophic and high-cost cases: Definitions, distinctions, and their implications for policy formulation. Inquiry. 1986;23(4):382–394. [PubMed] [Google Scholar]
- Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJ. Household catastrophic health expenditure: A multicountry analysis. Lancet. 2003;362(9378):111–117. doi: 10.1016/S0140-6736(03)13861-5. [DOI] [PubMed] [Google Scholar]