Social deficits are a core symptom of autism spectrum disorders (ASD)(APA, 1994) and arguably present the greatest obstacle to a person’s ability to develop and apply the real life skills necessary to meet the typical demands of daily living. Research has shown that, whatever their overall level of functioning, both children and adults with ASD tend to have more pronounced impairments in adaptive social skills (from participating in social activities with friends to knowing proper table manners to following community or school rules) relative to other key areas of development such as communication and more general self-help skills (e.g., Gillham, Carter, Volkmar, & Sparrow, 2000; Klin, Saulnier, Sparrow, Cicchetti, Volkmar, & Lord, 2007; Kraijer, 2000). Moreover, deficits in adaptive social skills are consistently more severe than intelligence scores would predict (e.g., Liss, Harel, Fein et al., 2001; Loveland & Kelley, 1988; Schatz & Hamdan-Allen, 1995; Volkmar, Sparrow, Gourdreau, Cicchetti, Paul, & Cohen, 1987). This uneven profile of development is not shared by other developmentally delayed groups but appears to be unique to autism (Gillham et al., 2000; Rodrigue, Morgan, & Geffken, 1991).
Social deficits have been observed as early as the first year of life even before diagnoses. For example, compared to children not diagnosed with autism, children later diagnosed with ASD show fewer instances of orienting to name at 8 to 10 months of age (Werner et al., 2000), less eye contact at 12 months (Osterling, Dawson, & Munson, 2002), and decreased spontaneous imitation by 16 to 18 months (Werner et al., 2000). As social expectations increase in later childhood and adulthood, poor social awareness in ASD becomes more evident and is marked by difficulty in understanding and expressing emotions, deficits in the social aspects of language, as well as failure to notice or comprehend more subtle nonverbal social cues, and impairments in initiating and responding to social overtures (Bacon et al, 1998; Celani, Battacchi, & Arcidiacono, 1999; Rumsey, Rapoport, & Sceery, 1985; Sigman & Ruskin, 1999; Tager-Flusberg, Paul, & Lord, 2005; Wilkenson, 1998).
The negative effects of social impairments in ASD are both pervasive across multiple life domains and persistent, affecting quality of life throughout the lifespan. There is evidence from several studies that social abilities for children and adults with ASD contribute positively to communication skills currently and lack of social ability predicts poorer academic skills later in life (Sigman & Ruskin, 1999; Venter, Lord, & Schopler, 1992). In turn, greater social use of language and academic skills are related to better overall social adjustment in adulthood in terms of friendships, level of independent living, and work placements (Howlin, Goode, Hutton, & Rutter, 2004). Unfortunately, the majority of adults with ASD in the Howlin et al. (2004) study, all with IQs over 50, continued to struggle socially, with only 22% of the sample rated as having “good” to “very good” outcome and a majority rated as having “poor” to “very poor” outcome. Other studies of adult outcome report similar findings (e.g., Ballaban-Gil, Rapin, Tuchman, & Shinnar, 1996; Billstedt, Gillberg, & Gillberg, 2005; Eaves & Ho, 2008). In addition, persisting social impairments in adolescence and adulthood may increase vulnerabilities to psychiatric problems such as depression, anxiety, feelings of social isolation and loneliness (e.g., Bauminger & Kasari, 2000; Eaves & Ho, 2008; Ghaziuddin et al, 2002; Muller, Schuler, & Yates, 2008; Rumsey et al., 1985; Simonoff et al, 2008).
Predictors of Social Outcome
Age
For an optimal prognosis in ASD over the life course, the timing, intensity, and type of interventions must be informed by a longitudinal understanding of the problem. Research has begun to chart the developmental course of social outcome in ASD. Evidence of improvements in social deficits with age is beginning to accumulate from research assessing composite scores on the social domain of the Autism Diagnostic Interview-Revised (ADI-R; Lord, Rutter, & LeCouteur, 1994). Results from studies with sample sizes exceeding 40 are generally suggestive of modest declines in social deficits with increasing age whether comparisons are made retrospectively (e.g., lifetime vs. current symptoms)(Piven, Harper, Palmer, & Arndt, 1996; Seltzer et al, 2003), cross-sectionally with current symptoms across different age cohorts (Seltzer et al., 2003), or longitudinally with current symptoms for the same individuals at two points in time (McGovern & Sigman, 2005; Shattuck, Seltzer, Greenberg et al., 2007). Likewise, findings from studies of 40 participants or greater which used the social domain of the Vineland Adaptive Behavior Scales (Sparrow, Balla, & Cicchetti, 1984) to assess differences in abilities by age across different birth cohorts (Klin et al., 2007; Schatz & Hamdan-Allen, 1995) as well as longitudinally with the same individuals (Freeman, Del’Phomme, Guthrie, & Zhang, 1999), suggest that adaptive social abilities increase with age. However, the improvements seldom result in a move out of the autism spectrum (e.g., Shattuck et al., 2007), nor does progress keep pace with norms for typical development over time (Klin et al., 2007).
Some findings have not fit the general pattern of improvement with age. For example, adults with ASD had more social deficits than adolescents in the Seltzer et al. (2003) study but the source of disagreement is unclear. Due to the cross-sectional nature of this and other studies, it is impossible to determine whether age differences were due to birth cohort effects, natural maturation, or differences in sample selection. Contradictory findings from longitudinal studies are also difficult to interpret. Starr, Szatmari, Bryson, & Zwaigenbaum (2003), found that current social deficit totals on the ADI-R increased rather than decreased for 58 high-functioning 4 to 6 year-olds with ASD when measured two years later. These findings have little basis for comparison since other samples were comprised primarily of adolescents and adults (e.g., McGovern & Sigman, 2005; Shattuck et al., 2007). For samples which included young children, age at first measurement has varied greatly within and between studies (e.g., Freeman et al., 1999). As yet, current research gives little indication of how patterns of social abilities or disabilities in ASD might change with time from early childhood to adolescence and young adulthood, particularly in a prospective study. Discrepant findings among studies reflect the great variability in social outcome at the individual level within the autism spectrum as noted in some studies (e.g., Shattuck et al.,2007).
Diagnosis
Other research efforts have assessed the impact of various factors thought to explain some of the heterogeneity in social outcome within ASD. Individual characteristics and abilities have by far received the most attention. Diagnosis as a predictor of social outcome (e.g., on the Vineland) has been examined primarily in cross-sectional studies in order to determine whether individuals with ASD can be distinguished from those with other developmental disabilities based on adaptive behavior. Between-group comparisons in daily living and communication skills are inconsistent across studies, however, all of the studies with samples greater than 40 found that children and adults with autism show deficits in adaptive social behavior skills relative to other groups, including typically developing children (Rodrigue et al., 1991) as well as those with intellectual disabilities (Schatz & Hamdan-Allen, 1995), Down Syndrome (Rodrigue, Morgan, & Geffken, 1991), developmental language disorders (Liss et al., 1991), and a mix of other developmental disorders (Gillham, Carter, Volkmar, & Sparrow, 2000; Volkmar et al., 1993; Volkmar et al., 1987). These findings hold even when participants with ASD are matched by overall adaptive behavior skills (Rodrigue et al., 1991), age, and IQ (Liss et al., 2001). Other studies have employed different instruments to compare adaptive social behaviors across groups with identical results (see Kraijer, 2000 for a review).
Gillham et al (2000) qualifed their findings in that the adaptive social skills of children with PDD-NOS (but not autism) did not differ from those with other developmental disabilities perhaps due to more subtle social impairments in higher-functioning children. Only one study (Schatz & Hamdan-Allen, 1995) attempted to examine differences in rates of change over time by diagnosis (albeit indirectly through cross-sectional comparisons of age cohorts) and found that increasing age had similar positive effects on social skills both for children with ASD and those with intellectual disabilities only. None of the Vineland studies longitudinally assessed how differences in diagnosis affect the rate and pattern of change in social skills over time.
Cognitive Abilities
Cognitive skills, especially IQ and language abilities, are the most commonly measured predictors of social outcome in ASD. Longitudinal studies have found a significant relationship between cognitive abilities measured at an earlier time and later social outcome. Whether outcome is assessed in terms of a single indicator variable such as adaptive social behavior skills (McGovern & Sigman, 2005; Venter, Lord, & Schopler, 1992), or less standardized measures coding friendships, living arrangements, and employment or educational placements (Billstedt et al., 2005; Eaves & Ho, 2008; Gillberg & Steffenurg, 1987; Howlin et al., 2004), greater initial cognitive abilities generally predict a more positive social outcome later in life. Unfortunately, little research has focused on the predictive ability of early childhood cognitive factors on later outcome. Among the exceptions, the presence of speech before the age of 5 or 6 and IQ in late preschool or early school-age was related to better social outcome in adolescence and young adulthood in several studies (Billstedt et al., 2005; Howlin et al., 2000; Venter et al., 1992).
The relatively consistent findings linking cognitive abilities to social outcome, however, are tempered by results from other research. There is some evidence to suggest that the positive relationship between cognitive abilities and social outcome may provide diminished returns for higher-functioning individuals with ASD compared with lower-functioning individuals with ASD, and those with nonspectrum developmental delays regardless of IQ. As previously noted, both higher- and lower-functioning children with ASD showed greater impairments in adaptive social behavior compared to nonASD controls matched by IQ in the Liss et al. (1991) study, even though the gap between diagnostic groups in cognitive capacity and real life skills was more pronounced in the higher than the lower functioning ASD and nonASD groups. In another study, Schatz & Hamdan-Allen (1995) reported an interaction between diagnosis and IQ such that increases in nonverbal intelligence for children with ASD were associated with significantly smaller increases in adaptive skills relative to children with nonspectrum developmental delays.
Finally, several longitudinal studies of adolescent and adult outcome across multiple life domains found that intelligence was a stable predictor of poor prognosis in ASD for individuals with below average IQs, but outcome was highly variable for those with normal or near normal IQs. Within the normal to near normal group, social outcome was no better for those with the highest IQs (i.e., 100+) than for those with considerably lower cognitive abilities (Howlin et al., 2004). In another study, 23% of those with near normal IQs lived in group homes or other residential facilities (Ballaban-Gill et al., 1996). Such variability may explain why several studies that restricted their samples to higher-functioning individuals with ASD, failed to find a relationship between intellectual abilities and social outcome (Freeman et al., 1999; Klin et al., 2007; Szatmari et al., 2000). Optimal social outcome in adulthood for individuals with ASD may depend as much on adequate social support resources and services as on general intelligence (Howlin et al., 2004).
Environmental Resources
Scant attention has been given to the potential positive predictive value of environmental supports such as early childhood intervention services, family socioeconomic status, and other resources on subsequent social outcome. For example, families with higher socioeconomic status (SES) generally afford children greater access to a variety of services, goods, social connections, and cognitively stimulating learning experiences from infancy to young adulthood that are not typically available to children of lower SES families (Bradley & Corwyn, 2002). A few findings specific to ASD populations indirectly suggest the contribution of external environmental factors to better social adjustment. Benson, Karlof, & Siperstein (2008) found that higher levels of family SES were associated with increased home-based involvement and education by mothers of children with ASD. Higher SES may enable parents to better manage the responsibilities placed upon them which could be particularly important when children have special needs. In turn, more maternal involvement results in greater participation in social and recreational activities for individuals with ASD (Orsmond, Krauss, & Seltzer, 2004).
Individuals with ASD who received more total hours of a specific intervention and began participating at younger ages were more likely to have better expressive language outcome and to be placed in a mainstream rather than a special education classroom setting (Harris & Handleman, 2000; Stone & Yoder, 2001). Results from several studies show promise for the efficacy of mentored parent intervention approaches (Koegel, Bimbela, & Schreibman, 1996; Ozonoff & Cathcart, 1998). More generally, intervention research has shown that the social skills of individuals with ASD are amenable to change and show short-term improvement as a result of intervention efforts (see McConnell, 2002, and Rogers, 2000, for reviews). However, many intervention studies have focused on changes in very specific target skills. Often it is not known to what degree improvements will translate into better overall social functioning (White, Keonig, & Scahill, 2007--review) or, more specifically, into more practical adaptive social behavior skills, or whether positive behavioral changes will be long-term. Although measurement of change in intervention studies is becoming increasingly more sophisticated, small sample sizes continue to make generalization to a larger population difficult (see Scattone’s, 2007 review).
In summary, the existing literature on children with ASD has made a substantial contribution toward identifying various child and, to a lesser extent, environmental factors believed to affect subsequent socialization skills. However, these key factors are seldom considered in the same study. In addition, the literature provides little guidance on how the social skills of very young children develop within individuals over time, particularly with respect to the pattern and rate of change. This study attempted to begin addressing these gaps.
Purpose of Study
The main objective of the current study was to examine prospectively the development of social skills between ages 2 to 13 in a large sample of children initially diagnosed with autism, PDD-NOS, or nonspectrum developmental delays. The unique characteristics of the data for the present study allowed for the simultaneous consideration of multiple predictors affecting the long-term development of socialization skills among the diagnostic groups, beginning when the children were still toddlers. We chose adaptive social abilities as our outcome measure because such life skills are a better prognostic indicator of how well an individual with ASD can function in his or her environment than, for example, cognitive abilities. Specific aims were to examine differences between and within diagnostic groups with respect to: 1) the pattern of change over time; 2) the rate of progress over time; 3) the range of outcomes; and 4) early childhood predictors of outcome.
In light of findings from previous studies, we formulated a number of hypotheses. First, there is no evidence to suggest that the pattern of change would likely differ by diagnostic group. We predicted a pattern of steady increases in social age equivalent scores on average through age 13 regardless of diagnosis. However, the rate of change in social skills was expected to vary as a function of both environmental and child specific characteristics as existing research seems to suggest. Children initially diagnosed with autism at age 2 were expected to progress at a slower rate than children with PDD-NOS and nonspectrum delays. None of the three groups were expected to progress at a rate commensurate with typical development. Moreover, children with a higher nonverbal IQ at age 2, who received more hours of individual treatment through age 5, and whose mothers had more years of formal education, were also expected to experience greater gains in social skills over time. Language and nonverbal IQ at the first assessment were hypothesized to be weaker predictors of later social skills for children with PDD-NOS than for children with autism and nonspectrum developmental delays. This hypothesis is consistent with findings from previous research, because children with PDD-NOS in this sample had greater cognitive abilities as a group than children with autism (e.g., see Anderson et al., 2007; Lord et al., 2006). Finally, we expected substantial variation in outcomes within each diagnostic group.
Method
Participants
Eligible participants were consecutive referrals younger than 37 months of age from agencies across North Carolina and metropolitan Chicago serving very young children with developmental delays. All 221 families agreed to participate in the study initially. One later withdrew and six other families became ineligible for inclusion when the children reached the age of 36 months before the first assessment could be scheduled. With the exception of the children’s age, these seven families did not differ demographically from the other 97% of families who participated in the study. Participants consisted of 192 children (162 males, 30 females) referred for evaluation for possible autism and 22 non-autistic developmentally delayed children (DD: 10 males, 12 females) recruited in North Carolina. The autism referral group was comprised of children under age 3 from four North Carolina state-funded autism centers (n=111) or a Chicago autism clinic within a private university hospital (n=81). Exclusion criteria included moderate to severe sensory impairments or cerebral palsy, known genetic abnormalities, or poorly controlled seizures. Nearly one-half of the 214 participants (47%) received a diagnosis of autism at age 2, while the other half was divided between children with PDD-NOS (28%) and those without Autism Spectrum Disorders (25%). The nonspectrum group consisted of children with some degree of intellectual disability or a language delay (91%), while the remainder had other disabilities such as ADHD or a medical condition. There was a mix of children from rural and urban areas. Ethnic minorities, the majority of whom were African American, accounted for a sizeable proportion of the sample (33%). A third of the children had mothers with a high school education or less, while parent education for the remainder of the sample ranged from some college (29%) to completion of a college degree (38%).
All children were first seen around age 2, with a mean age of 29 months (S.D.=5.17). The number of subsequent assessments varied by site and referral status. The North Carolina autism referral group was assessed at approximately ages 2, 3, 5, and 9, while the other two groups were seen at three of the four time points (i.e., the DD group was not seen at age 3 and Chicago referrals were not seen at age 5). The age 13 assessment included 148 participants from the original sample and was completed through parental phone interviews and mailed questionnaires. Of the original 214 participants, five were lost to follow-up after the initial assessment and the remainder were lost by age 13 due to geographical location, unreachable status, or refusal to participate. Although African American families with less education were lost to the study at a higher rate than Caucasians and families with more education, attrition was not related to diagnosis, gender, nonverbal IQ, language level, or adaptive scores at the initial assessment. The current study includes the 190 children who were seen at least three times.
Measures
The full battery of diagnostic and psychometric instruments was administered at each assessment free of charge. Verbal feedback and a written report were provided to families. Written informed consent was obtained from parents prior to each assessment.
Diagnostic Instruments
The Autism Diagnostic Instrument-Revised is a comprehensive, standardized parent interview designed to distinguish children with ASD from non-ASD and developmentally delayed populations (Lord et al., 1994). Algorithm scores are totaled for each of three domains: social behaviors, communication, and repetitive interests. A toddler version of the ADI-R, which includes a number of additional items specific to the first two years of life, was given when the children were 2- and 3-years-old. The Autism Diagnostic Observation Schedule (ADOS) (Lord, Risi, Lambrecht et al., 2000) and one of its predecessors, the Pre-Linguistic Autism Diagnostic Observation Schedule (PL-ADOS) (DiLavore, Lord, & Rutter, 1995), acquire diagnostic information through direct observation of the child by a trained clinician. An algorithm calculates summary scores for the social and communication domains. Children in the current study were given the PL-ADOS at ages 2 and 3, which was scored using the algorithm for the Module 1 ADOS (for children without phrase speech).
Each member of the research clinical team established inter-rater reliability exceeding 90% exact agreement (kappa > 0.70) for all items on the ADI-R and 80% exact agreement (kappa > 0.60) on codes for the PL-ADOS and ADOS for three consecutive administrations before the study began. Reliability was maintained through consensus coding approximately every sixth administration with a second rater who was blind to referral status.
Following the two-part diagnostic evaluation, an overall best estimate diagnosis of autism, PDD-NOS, or other nonspectrum disability was jointly determined by two trained staff members, including Ph.D. level research associates, child psychiatrists, or clinical psychologists. The decision for the best estimate diagnosis was based on the clinicians’ summary reports, psychometric and diagnostic algorithm scores, as well as videotapes of the direct observation of the child. (For a more detailed description of the procedures, see Lord et al., 2006).
Diagnosis in the current study refers to the age 2 best estimate classification. Previous research with this sample showed that clinicians’ ratings of diagnosis at age 2, using all available information, provided a useful categorical measure that surpassed, as well as summarized, the standardized diagnostic instruments in predicting outcome at age 9 (e.g., Lord, et al., 2006). There are many ways to break down what are likely many continuous dimensions that contribute to diagnostic severity. Our purpose was not to reify distinctions between different DSM IV-based autism spectrum disorders but to identify relatively easily interpretable ways of representing diversity within potential subsets, building on previous research.
Psychometric Instruments
Social skills at each time point were assessed using the Vineland Adaptive Behavior Scales (Sparrow, Balla, & Cicchetti, 1984; Sparrow, Cicchetti, & Balla, 2005), a standardized, semi-structured, parent interview designed to assess adaptive functioning. The Vineland was administered immediately after the ADI-R, in most cases, by a clinician who was unfamiliar with results from the child’s earlier assessments. Age equivalents from the socialization domain were used in our analyses instead of raw scores for ease of interpretability and because of floor effects with the standard scores for many of the children with cognitive delays.
Age 2 nonverbal IQ scores were obtained from the Mullen Scales of Early Learning (MSEL: Mullen, 1985 MSEL: Mullen, 1995). The Infant MSEL is a normed measure of cognitive abilities for children below the 36-month level. The two nonverbal subscales include Fine Motor and Visual Reception (i.e., nonverbal cognition). One child in our sample did not reach a ceiling, so the Merrill-Palmer Scale of Mental Tests was administered (Stutsman, 1948).
Language at age 2 was assessed using the Sequenced Inventory of Communication Development-Revised (SICD-R: Hedrick, Prather, & Tobin, 1984), a standard measure of communicative development for children between the ages of 4 months and 4 years.
Treatment Measure
Parents completed diaries and then were interviewed about all educational and specific treatments received by their child. Two raters established reliability and coded the data. Individual speech therapy, for the purpose of this paper, was defined in terms of the total number of therapy hours received through age 5. Due to the relatively small numbers of families participating in mentored, parent-implemented structured teaching (MPST) (a home teaching program modeled after the TEACCH extended diagnostic services) and Applied Behavior Analysis (ABA) (n=28 in both cases), the number of hours in treatment through the child’s fifth year was divided into categories of “none,” “some,” and “more” (i.e., 0 hours, < 20 hours, & ≥ 20 hours for MPST; 0 hours, < 1667 hours, & ≥ 1667 hours for ABA). The categories of “some” and “more” represent groups above and below the median of the distribution, not including those with “none.” (See Mesibov, Shea, & Schopler, 2005, for details on the MPST approach).
Analyses
Growth curve analysis was used to examine growth in socialization age equivalents from age 3 to 13. A separate intercept and slope were calculated for each child as a control for the high correlations among repeated measures on the same individuals over time. The Autism, PDD-NOS, and nonspectrum diagnostic groups were compared with respect to: 1) the relative starting points at 36 months of age (intercept); 2) the rate of change from age 3 to 13 (slope); and 3) the pattern of change from age 3 to 13 (linear vs. quadratic trend). Covariates were added as fixed effects to examine how much they accounted for variation in the intercept and slope: age at testing, gender, ethnicity, mother’s education, site, hours of individual treatment through age 5, and age 2 nonverbal IQ and social skills. Age was centered at 36 months so the intercept could be interpreted as the mean social age equivalent at 3-years-old. Age 3 was used as the starting point for the growth curve models in order to control for socialization score at the first measurement by including it as a covariate. Growth curve analyses were carried out using Proc Mixed in SAS release 9.1.3 (SAS Institute, Inc., Cary, North Carolina).
The estimates for both the covariance and beta parameters were obtained by restricted maximum likelihood methods so that results would be unbiased (Verbeke & Molenberghs, 2000). To test for group differences in slopes and intercepts, we used t-statistics for each parameter, calculated as the ratio of the parameter estimate divided by the standard error. To examine whether rate of change in the verbal age equivalents over time differed significantly from zero, we used t-tests for linear combinations of variables representing the slopes.
A mixture modeling procedure called Proc Traj (Jones, Nagin, & Roeder, 2001) was used to focus more specifically on the variability in patterns of outcomes within the ASD subsample, as a compliment to the growth curve analyses. Proc Traj is an exploratory and analytic procedure written for use in SAS that identifies linear and nonlinear patterns in longitudinal data and classifies the sample into groups. We ran the procedure using an uncensored normal distribution for the age equivalent scores from age 2 to 13 to see if distinct subgroupings would emerge within the autism and PDD-NOS samples. We first compared the absolute value of the Bayesian Information Criterion (BIC) between respective models (smaller indicates a better fit) to determine the optimal number of groups (Jones et al., 2001). We added the additional criterion that subgroups generated by Proc Traj be comprised of at least 10 individuals whose group membership remained relatively stable regardless of which covariates (“risk” factors) were under consideration. T-tests were used to determine the significance of the individual parameter estimates for each risk factor. Odds ratios were calculated for the parameter estimates to assess the relative contributions of risk factors to group membership.
Results
Preliminary Analyses
Validation of Parent Report Measure
To affirm the concurrent validity of our parent report measure of social skills, we examined the correlations between children’s socialization scores on the Vineland with those from the socialization domain of the ADOS, which is based on a clinician’s direct observation of the child. Comparisons were available for the age 2, 3, 5, and 9 assessments. Higher scores on the Vineland indicate greater social skills while the reverse is true for the ADOS. Pearson correlations between the Vineland and ADOS were significant (p < .001) and moderate to high at each time period: age 2 (n=188), r = −.66; age 3 (n=159), r = − .69; age 5 (n=118), r = − .67; age 9 (n=150), r = −.70. We also ran the correlations separately for each diagnostic group with similar results, indicating substantial agreement between the measures.
Early Childhood Characteristics
Table 1 portrays various sample characteristics related to demographics, cognitive abilities at age 2, and treatment received through age 5 according to children’s diagnosis at the first assessment. Chi square analyses were conducted to test for differences in group proportions, while analysis of variance was used to test for group differences in means. The diagnostic groups did not differ by age, ethnicity, or mother’s education. Children with autism were significantly more delayed with respect to socialization skills, expressive and receptive language, and nonverbal IQ compared to the other two diagnostic groups at age 2. By age 5, the autism group had participated in significantly more hours of individual treatment than both the PDD-NOS and nonspectrum developmentally delayed groups. Finally, children with PDD-NOS had fewer socialization skills and tested lower in receptive and expressive language abilities at age 2 than children with nonspectrum delays. The analyses that follow sought to determine the impact of these early childhood factors on social skills in later years. We first examine variability between diagnostic groups.
Table 1.
Early Childhood Characteristics by Age 2 Diagnosis Means (standard deviations)
| Sample Characteristics1 | Age 2 Diagnosis |
||
|---|---|---|---|
| Autism N=93 | PDD-NOS N=51 | Nonspectrum2 N=46 | |
| Age of child in months | 29.6 (4.68) | 29.45 (5.67) | 29.35 (5.78) |
| Mother’s Education: | |||
| % high school or less | 25 | 34 | 46 |
| % some college | 30 | 29 | 22 |
| % college degree | 45 | 37 | 33 |
| Nonverbal IQ | 62.4 (17.36)a | 72.5 (20.53)b | 71.98 (23.58)b |
| Vineland Socialization AE3 | 8.1 (3.40)a | 11.43 (3.78)b | 14.00 (4.81)c |
| Expressive Language AE | 8.42 (5.53)a | 12.18 (6.10)b | 15.65 (7.20)c |
| Receptive Language AE | 6.2 (4.76)a | 13.3 (6.96)b | 18.2 (7.25)c |
| % Ethnic Minority | 33 | 35 | 26 |
| Total Hrs. of Individual Tx4 thru Age 5 | 664.1 (924.91) a | 282.6 (450.10) b | 301.6 (376.90) b |
| % with some Speech Tx thru Age 5 | 87 | 74 | 75 |
| % with some MPST Tx thru Age 5 | 20 a | 14 ab | 4 b |
| % with some ABA Tx thru Age 5 | 11 a | 10 ab | 4 b |
All characteristics were measured at the first assessment unless otherwise indicated.
The nonspectrum group includes all of the DD children as well as children referred for possible autism who did not receive ASD diagnoses at age 2.
Age equivalent in months.
Treatment.
Note: letter superscripts denote significance of group comparisons (i.e., no shared superscripts across two different groups indicates significant group differences of at least p < .05).
Socialization through age 13
Variability Between Diagnostic Groups
Growth curve analyses on a continuous outcome variable using the entire sample provided the statistical power to consider the relative contributions of multiple early childhood predictors as well as to examine diagnostic group differences in the rate and pattern of change in social skills from toddlerhood to mid adolescence. Prior to fitting the growth curve models in Table 2, a check for potential collinearity problems among the predictors revealed moderate correlations between adaptive social skills and other variables measured at age 2, including diagnosis (nonspectrum vs. ASD, r=.44) and nonverbal IQ (r=.46). We found that when the age 2 socialization skills control variable was added to the growth curve model, the coefficients for diagnosis and IQ changed by 1% and 26% respectively, while the Variance Inflation Factors were both moderately low (i.e., VIF < 3). In addition, the results of significance tests for the coefficients were virtually the same regardless of whether socialization skills were included as a covariate. Therefore, we felt justified in retaining all of the predictor variables listed in Table 2. However, the effects of early language abilities are considered separately by diagnosis in subsequent analyses, because language scores were moderately to highly correlated with having a diagnosis of autism and with socialization skills measured at age 2.
Table 2.
Growth Models for Changes in Social Skills from Age 3 to 13 by Diagnosis at Age 2
| Predictors | Model 1 | Model 2 | Model 3 | Model 4 |
|---|---|---|---|---|
| Coefficient (S.E.) | Coefficient (S.E.) | Coefficient (S.E.) | Coefficient (S.E.) | |
| Fixed Effects | ||||
| Intercept | 13.84*** (.64) | 11.27*** (.89) | 12.48*** (1.39) | 10.46* (2.59) |
| Age at Testing | .43*** (.04) | .31*** (.05) | .38*** (.05) | .70*** (.10) |
| Social Skills at Age 2 | .37* (.18) | .38* (.18) | ||
| Dx at Age 2: | ||||
| Autistic | --- --- | --- --- | --- --- | |
| PDD | 4.10** (1.46) | 1.51 (1.51) | 1.25 (1.52) | |
| Nonspectrum | 6.76*** (1.64) | 1.83 (1.95) | 1.54 (1.96) | |
| Site | ||||
| N.C. ref. for aut. | .50 (1.48) | .86 (1.62) | ||
| N.C. dd | 5.51 (3.03) | 5.65 (3.04) | ||
| Chicago | --- --- | --- --- | ||
| Nonwhite | −.10 (1.46) | −.07 (1.46) | ||
| Mother’s Education | −.17 (.58) | −.04 (.61) | ||
| Nonverbal IQ at Age 2 | .10** (.04) | .10** (.04) | ||
| MPST to Age 5 (> 20 hrs.) | --- --- | |||
| MPST to Age 5 (< 20 hrs.) | 1.87 (2.89) | |||
| MPST to Age 5 (none) | 2.19 (2.23) | |||
| Linear Slopes: | ||||
| Age* Autism | --- --- | --- --- | --- --- | |
| Age* PDD | .21** (.08) | .15* (.07) | .17* (.07) | |
| Age* Nonspectrum | .23** (.08) | .16* (.07) | .18* (.07) | |
| Age* Nonwhite | −.09 (.07) | −.09 (.07) | ||
| Age * Mother’s Education | .02 (.03) | .02 (.03) | ||
| Age* NVIQ | .01***(.00) | .01*** (.00) | ||
| Age* MPST (> 20 hrs.) | --- --- | |||
| Age* MPST (< 20 hrs.) | −.52* (.15) | |||
| Age* MPST (none) | −.35** (.10) | |||
| Variance | Variance | Variance | Variance | |
| Random Effects | ||||
| Slope | .20*** | .18*** | .13*** | .12*** |
N=190
p<.001,
p<.01,
p<.05
Table 2 shows four growth curve models from the least to the most inclusive as more covariates were added to the models. The coefficients of greatest interest are bolded in each. The intercept in Model 1 (14 months) is the predicted average socialization age equivalent score for the entire sample at 36 months of age. The age coefficient indicates significant gains in social skills over time for the sample as a whole. However, significant unexplained variance in the random slopes remained after accounting for age as can be seen at the bottom of the table. Note that the random intercepts were removed from the models. Because the residual variance accounted for all of the variability around the intercepts, the random intercepts could not be estimated.
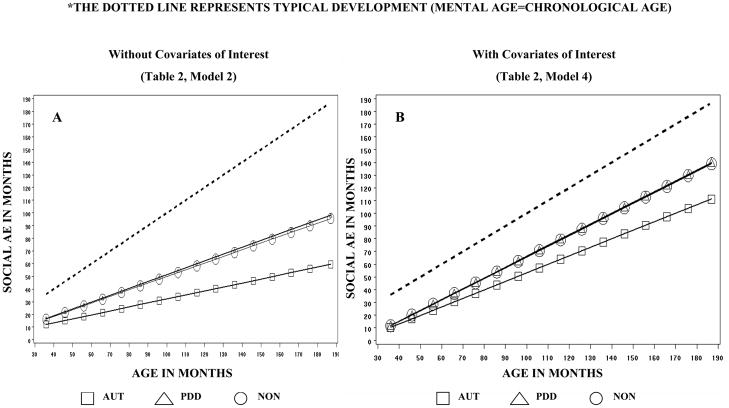
Age 2 diagnosis was added to Model 2. As indicated by the group-by-time interaction coefficients, change progressed at a linear rate (the nonsignificant quadratic effects were omitted) and these positive gains were significantly different from 0 for all three groups (p < .001). The same growth trends by diagnosis are depicted visually in Figure 1A. Although socialization skills on average remained well below age norms for all three groups, the trend was toward steady improvement over time for each of the diagnostic groups with no signs of leveling off at age 13. Also apparent in Figure 1A, are the steeper growth trajectories for the PDD-NOS and nonspectrum groups compared with the autism group. The positive group-by-age interactions in Model 2 of the table confirm that the nonspectrum and PDD-NOS children improved at a significantly faster rate than the children with autism. In other words, group inequalities between the autism and other diagnostic groups increased with time. Hence, as predicted, the pattern of growth was similar while the rate of change differed by diagnosis.
Figure 1.
Predicted Social Growth Trends by Age 2 Diagnosis
In Model 3 of Table 2, diagnostic group differences in growth trajectories remained after accounting for demographics, social, and cognitive abilities. A higher nonverbal IQ and better social skills at age 2 predicted greater social skills at age 3 (i.e., the intercept) and accounted for the differences in the group intercepts. Closer inspection revealed that the inclusion of age 2 social skills alone resulted in the reduction of group differences in the intercept to nonsignificance. Most importantly, as expected, a higher nonverbal IQ at age 2 predicted greater gains in socialization skills over time (i.e., there was a significant positive interaction between IQ and age). However, contrary to what was hypothesized, the three way interaction between IQ, diagnosis, and age, was not significant, indicating that a higher IQ had similar positive effects on social skills regardless of diagnosis. In addition, socialization skills for Caucasian children improved at a faster rate compared to minority children (not shown on Table 2) but ethnic differences were reduced to nonsignificance once nonverbal IQ and mother’s education were controlled. Gender was nonsignificant and was therefore removed from the model.
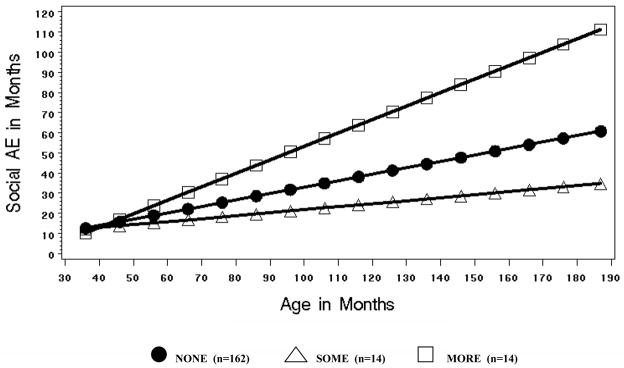
Model 4, which is visually portrayed in Figure 1B, tested whether the effects of individual treatment received through age 5 affected growth in socialization skills over the 11 year span when all other covariates were held at the mean. In fact, our hypothesis was partially confirmed. Although both speech therapy and ABA were not significant predictors (not shown on table), the interactions between time and the MPST therapy were positive and significant in the full model. In other words, children who participated in more MPST therapy hours through age 5, made significantly greater gains over time than their peers who had few or no sessions after controlling for age 2 nonverbal IQ, social skills, and demographics. While having been diagnosed with autism at age 2 continued to predict slower growth in socialization skills over time, the full model accounted for significant variability in the growth rate as can be seen graphically in the contrast between Figures 1A (Model 2) and 1B (Model 4). Whereas inequalities between the diagnostic groups became more pronounced with time in Figure 1A, this pattern was minimized somewhat in Figure 1B after accounting for factors such as early social and cognitive abilities, and treatment received. Moreover, the unexplained variance in the rate of change over time (i.e., the random slope variance) was reduced by 40% between Models 1 and 4 as shown at the bottom of Table 2.
To highlight the positive effects of the MPST therapy, Model 4 is again portrayed visually in Figure 2, however, the sample is grouped by therapy status instead of diagnosis, with the autism subsample serving as the reference group. In other words, Figure 2 graphically depicts the estimated growth trajectories for each of the three therapy conditions (“none,” “some” and “more” MPST sessions through age 5) for a child with autism whose social skills and nonverbal IQ are average for this sample. Initially, at 36 months there were no significant differences in social skills between those with none, some, and more therapy. Over time, differences in the rate of improvement between the “none” and “some” therapy groups were nonsignificant. However, the therapy group with more than 20 hours made increasingly greater gains relative to their counterparts so that, by age 13, therapy for a child initially diagnosed with autism, was predicted to add between 33 and 50 months to his or her socialization age equivalent score. Because all but one of the children receiving the MPST therapy were from North Carolina, we also ran the model with only the North Carolina subsample with identical results.
Figure 2.
Predicted Verbal Growth Trends by MPST Therapy Status
Variability Within Diagnostic Groups
Individual change over time
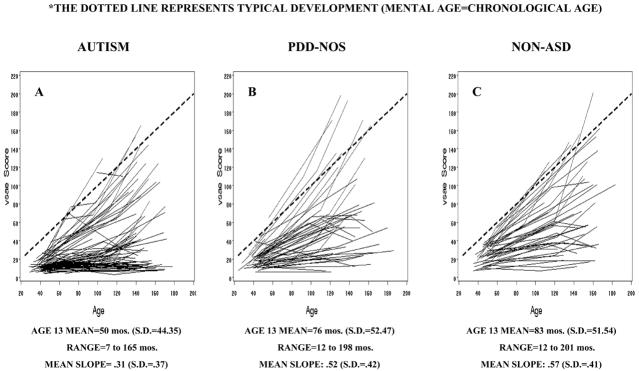
The importance of examining variation within diagnostic groups is visually apparent in Figures 3A, B, and C which chart the individual line plots of social age equivalent scores from 2 to 13+ years. The figures show a great deal of individual variability within each group that is otherwise masked by between-group comparisons. Despite the autism group’s substantially lower average social skills age equivalent score at 13 years and slower mean growth rate over time compared to the PDD-NOS and nonspectrum groups, the range of outcomes was substantial across diagnostic groups. Several children in both the autism and PDD-NOS groups were above age norms at 13. Variability in the autism group assumed a somewhat bimodal distribution, with a substantial proportion of children showing very little growth over time and a smaller proportion that cluster near or above the dotted line representing typical social development. For children in the PDD-NOS and nonspectrum groups, individual trajectories were more evenly distributed with fewer at the lower end of the range.
Figure 3.
Individual Social Skills Trajectories by Age 2 Diagnosis
Subgroups within diagnostic categories
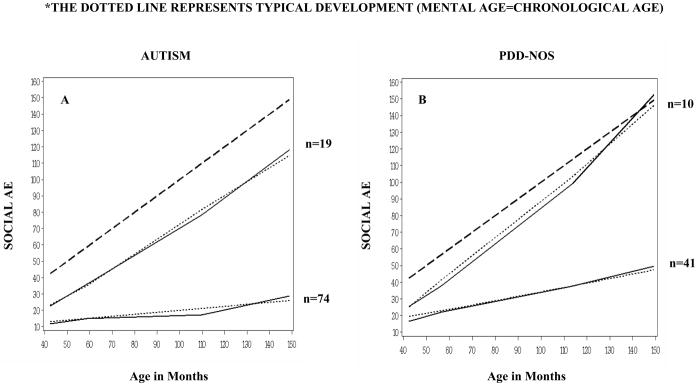
Variability within diagnosis for children with autism and PDD-NOS was further examined with growth mixture modeling using the Proc Traj procedure to determine whether natural subgroupings would emerge from the data over the eleven year period. Two subgroups were generated within each diagnostic group. The mean probability of an individual’s assignment to one group over another was .98 and .96 for the least improved autism and PDD-NOS groups respectively and .99 for the most improved groups in each case. Visual support for the goodness of model fit is shown in Figures 4A and 4B, where discrepancies between observed (solid lines) and expected values (dotted lines) are quite small.
Figure 4.
Social Skills Growth Trends
Children with an ASD by Amount of Improvement
Growth occurred in a linear fashion (once again, the quadratic terms were nonsignificant). Notably, the ”most improved” autism group, which comprised about 20% of the autism sample, showed dramatic increases in social skills over time, with scores improving to near age norms for typical development—an average increase of about 8 years, 11 months over the 11 year period. Similarly, the “most improved” PDD-NOS group scores progressed on average at a pace slightly higher than typical development (11 years, 6 months over the 11 year period). These social improvements were accompanied by changes in nonverbal IQ and diagnosis between ages 2 to 9, suggesting improvement over time for these children at a more global level. For example, the nonverbal IQs of the “most improved” autism and PDD-NOS groups increased an average of 20 and 16 points respectively from age 2 to 9. Moreover, the diagnoses for 58% (n=11) of the most improved autism group had changed from autism at age 2 to PDD-NOS (or nonspectrum in one case) by age 9. For children in the most improved PDD-NOS group, 40% received nonspectrum diagnoses by age 9 while 30% continued to be diagnosed with PDD-NOS. Interestingly, 30% (3 out of 10) of the children in the most improved PDD-NOS group did not fit the pattern with respect to changes in diagnosis. Specifically, they went from an initial PDD-NOS diagnosis to a full-blown autism diagnosis by age 9 yet they still enjoyed substantial improvement in their socialization skills over time. Finally, children in the least improved autism and PDD-NOS groups experienced much more modest increases in socialization skills over the 11-year period (M=21 months and M=38 months respectively).
Risk factors for subgroups
The purpose of adding early childhood “risk” factors to the Proc Traj analyses was twofold. First, we wanted to explore the question of why some children had greater social skills at age 13 compared to others with the same diagnosis at age 2. Second, we wanted to address the hypothesis that early language abilities would be more closely linked to social skills later in life for young children with autism and nonspectrum developmental delays than with PDD-NOS. Individual covariates were considered separately within each diagnostic group due to moderate to high correlations between expressive and receptive language abilities, diagnosis, and other covariates. In the analyses that follow, the likelihood of being placed in the least- or most-improved groups for each risk factor was assessed.
Stronger expressive but not receptive language skills at age 2 resulted in a higher likelihood of assignment to the most improved autism subgroup. (Note: there was a floor effect for receptive language with the overwhelming majority of children in both groups demonstrating little understanding of the meaning of words at the first assessment). Only one child with an autism diagnosis was beginning to express words verbally at age 2. Nevertheless, a majority of the children in the most-improved autism group (74%) were showing a clear readiness toward becoming verbal with age equivalents between 12 and 20 months compared to 22% in the least-improved autism group. For every one month increase in a child’s expressive language score at age 2, the odds were 1.17 times greater that he or she would be placed in the most improved autism group (p < .01). The odds ratios for age 2 socialization score (OR=1.38; p < .01) and nonverbal IQ (OR=1.06; p < .01) were similar. MPST therapy had the highest odds ratio for children with autism. For children with more hours of the MPST therapy, the odds of being assigned to the most improved group were 2.23 times greater (p < .05). There was a nonsignificant trend (p < .10) such that children with more educated mothers had higher odds of assignment to the autism group which made the greatest gains over time compared to children with less well-educated mothers. Race, site, gender, speech therapy, and ABA treatment were not significant risk factors for group assignment.
For children who were originally diagnosed with PDD-NOS, in contrast to the autism group, higher receptive language scores predicted a greater likelihood of assignment to the most improved group (OR=1.30; p < .01). Receptive language skills at the first assessment varied by group with 90% of the most-improved children beginning to demonstrate an understanding of word meanings at age 2 compared to fewer than half (44%) of the least-improved group. (There was little difference between the least- and most-improved groups in expressive language. Most were showing a readiness toward becoming verbal with mean age equivalents of 15 and 20 months respectively). Nonverbal IQ was once again positive and significant (OR=1.08; p < .05). However, mother’s education had the highest odds ratio for children with a PDD-NOS diagnosis. Specifically, for each unit increase in mother’s education, the odds were 2.27 times greater that a child would be in the group which made the most gains in social skills over time (p < .01). Race, site, gender, and the amount of individual treatment (i.e., speech, ABA) were nonsignificant. The effects of the MPST therapy could not be tested due to small sample size and too few participants receiving these services in both subgroups.
Children diagnosed with nonspectrum developmental delays were included in these analyses mainly to assess the predictive ability of early language skills on social outcome. For these children, greater language abilities at age 2 were marginally associated with better social outcome for expressive (p < .05) and receptive (p < .10) skills and the odds ratios were similar in each case (OR=1.15 for expressive and OR=1.09 for receptive).
MPST Therapy Post Hoc Analyses
Finally, we wanted to revisit the finding of a strong positive association between more hours of MPST therapy for the sample as a whole and subsequent socialization skills. Post hoc analyses first sought to uncover the ways in which the MPST therapy group with greater than 20 hours might have differed relative to those who received other kinds of treatment (but not MPST), such as ABA, or no MPST therapy through age 5. In other words, could the groups have differed systematically with respect to other characteristics that might account for the finding? Comparisons between those who received the most MPST therapy and the most ABA treatment revealed that the MPST sample was not significantly more advantaged in terms of demographics, cognitive and social functioning at intake, diagnostic scores on the ADOS, or in the amount of speech therapy received. In addition, it could not be determined whether the MPST group was more likely to be placed in a classroom setting at an earlier age than the ABA children, due to small numbers and low statistical power. Similar comparisons between the “more” MPST therapy group and those with little or no MPST therapy indicated no significant group differences except that children with autism received more hours of MPST therapy than children in the PDD-NOS or nonspectrum groups.
We were also interested in the generalizability of the findings with the MPST therapy variable. In other words, would the positive effects of having received more MPST therapy through age 5 hold for other developmental outcomes such as verbal ability skills? We revisited data from our previously published study (Anderson et al., 2007) predicting changes in verbal abilities from age 2 to 9 with the same sample of children. In fact, the results were very similar when we ran the full growth curve model with the same covariates as shown in Table 2, Model 4 (see Anderson et al., 2007 for a description of the verbal abilities measure). Verbal skills for children who received the most MPST therapy through age 5 improved at a faster rate (p<.05) over the seven year period than children who received little or no MPST therapy. (Once again, neither speech nor ABA therapy had significant effects on outcome). This finding lends greater credibility to the positive effects of the MPST therapy in the current study, particularly because the verbal outcome measure was based on direct testing while the Vineland data presented in the current study are based on parent report.
Discussion
The greatest contribution of the current study was the ability to conduct multiple, comprehensive assessments on a large sample of children over an 11 year period extending from toddler years to adolescence. The results offer hope to children with ASD and their families. Change occurred at a general level as growth in adaptive social abilities over time was associated with a decrease in social deficits, improvements in nonverbal IQ, and, in some cases, change to a less severe diagnosis. Other research has noted similar positive changes in IQ over time (e.g., Howlin et al., 2004; McGovern & Sigman, 2005). The substantial variation in social outcome from little to dramatic improvement was striking, especially given that ours was a relatively cognitively impaired sample in which developmental delays were identified at an early age. Notably, adaptive social skills for about one-quarter of the autism and PDD groups improved at a rate that neared or exceeded norms for typical development. At the same time, positive change for the majority was considerably more modest and below age norms for typically developing children. While most children with ASD can expect to experience some persisting social difficulties later in life, the finding that those most at risk for future problems can be identified and targeted for intervention as early as age 2 with a fair amount of accuracy, is encouraging. In other words, the rate of improvement in adaptive social skills from age 2 to 13 was not random but predictable on the basis of early childhood characteristics such as diagnosis and cognitive abilities as well as environmental resources such as mother’s education and the amount of parent-mediated treatment received.
Contrary to expectations and previous research, cognitive abilities in the current study, including nonverbal IQ and language skills, appeared to play an important role in promoting adaptive social behavior skills regardless of diagnosis, with some noteworthy qualitative differences. For children with autism, early signs of expressive communication at age 2 were key to a more positive social outcome. In contrast, more subtle, early receptive language skills that require an understanding of word meanings appear to be better predictors of social growth for more mildly impaired children who had received a PDD-NOS diagnosis at age 2. These findings are consistent with previous research linking early verbal abilities to subsequent social outcome (e.g., Billstedt et al., 2005; Shattuck et al., 2007).
Possibly the most encouraging finding was the positive relationship between environmental resources and accelerated gains in adaptive social skills over time. Mother’s level of education had greater predictive ability for children with PDD-NOS than with autism, perhaps because the less severe social disabilities in the former are more responsive to slight advantages in family socioeconomic status. More importantly, evidence supporting the ability of children with ASD to benefit from early intervention efforts was provided by the substantially greater increase in the age equivalent scores of 13 year-olds who participated in parent-implemented therapy sessions for 20 or more hours during early childhood, compared to those who had little or no such treatment. Our results concur with those of other parent intervention studies examining various outcomes (e.g., Koegel et al., 1996; Ozonoff & Cathcart, 1998), with the added finding that the positive effects both generalized to other skills such as verbal abilities and were present at least eight years later. More generally speaking, our results are supported by research and theory in the broader social competence literature which emphasizes the contribution of both child specific characteristics and environmental factors to social outcome (e.g., Iarocci, Yager, & Rose-Krasnor, 1997).
There are a number of limitations and caveats to this study. Families were not randomly assigned to different treatments, and there was no attempt to control or measure the quality of treatments children received. It is likely that families who chose to participate in MPST therapy for 20 hours or more were self-selected in terms of their interest and ability to work with their own children. This may in part be reflected in the greater social gains of children who received greater than 20 hours compared to those who received fewer hours or no structured teaching. Consequently, these findings cannot be interpreted as an indication of the superiority of MPST to ABA or other kinds of treatment. Nevertheless, they offer evidence of a significant treatment effect, perhaps confounded with other unmeasured characteristics of families, of a sustained, but relatively minimal parent-as-co-therapist intervention.
A further limitation is that findings from our study may not be representative of children first diagnosed with ASD at older ages. Moreover, children in our sample are likely to have more severe problems than children diagnosed with ASD today in part due to greater awareness and broadening of diagnostic criteria to include less severe presentation of symptoms in recent years (Fombonne, 2007). In addition, because attrition was greater in more socially disadvantaged families, the effects of demographic variables may have been underestimated. Furthermore, our outcome measure was based solely on parental report, however, results were supported by the finding that scores from the parent report measure were related to those from a direct observation instrument. Finally, future research will need to further examine which qualitative features of treatment as well as other environmental resources foster optimal social development in ASD. Observation into adulthood will be important since, as our results showed, improvements in adaptive social behavior skills may continue at a steady rate into adolescence with no indication of progress slowing. We plan to extend our findings to adulthood in future endeavors with this sample.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4. Washington, D.C: APA; 1994. [Google Scholar]
- Anderson DK, Lord C, Risi S, DiLavore P, Thurm A, Shulman C, Welch K, Pickles A. Patterns of growth in verbal abilities among children with autism spectrum disorder. Journal of Consulting and Clinical Psychology. 2007;75(4):594–604. doi: 10.1037/0022-006X.75.4.594. [DOI] [PubMed] [Google Scholar]
- Bacon A, Fein D, Morris R, Waterhouse L, Allen D. The responses of autistic children to the distress of others. Journal of Autism and Developmental Disorders. 1998;28 (2):129–142. doi: 10.1023/a:1026040615628. [DOI] [PubMed] [Google Scholar]
- Ballaban-Gil K, Rapin I, Tuchman R, Shinnar S. Longitudinal examination of the behavioral, language, and social changes in a population of adolescents and young adults with autistic disorder. Pediatric Neurology. 1996;15:217–223. doi: 10.1016/s0887-8994(96)00219-6. [DOI] [PubMed] [Google Scholar]
- Bauminger N, Kasari C. Loneliness and friendship in high-functioning children with autism. Child Development. 2000;71 (2):447–456. doi: 10.1111/1467-8624.00156. [DOI] [PubMed] [Google Scholar]
- Benson P, Karlof K, Siperstein G. Maternal involvement in the education of young children with autism spectrum disorders. Autism. 2008;12 (1):47–63. doi: 10.1177/1362361307085269. [DOI] [PubMed] [Google Scholar]
- Billstedt E, Gillberg C, Gillberg C. Autism after adolescence: Population-based 13-to 22-year follow-up study of 120 individuals with autism diagnosed in childhood. Journal of Autism and Developmental Disorders. 2005;35 (3):351–360. doi: 10.1007/s10803-005-3302-5. [DOI] [PubMed] [Google Scholar]
- Bradley R, Corwyn R. Socioeconomic status and child development. Annual Review of Psychology. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- Dawson G, Toth K, Abbott R, Osterling J, Munson J, Estes A, Liaw J. Early social attention impairments in autism: Social orienting, joint attention, and attention to distress. Developmental Psychology. 2004;40 (2):271–283. doi: 10.1037/0012-1649.40.2.271. [DOI] [PubMed] [Google Scholar]
- DiLavore P, Lord C, Rutter M. The Pre-Linguistic Autism Diagnostic Observation Schedule (PL-ADOS) Journal of Autism and Developmental Disorders. 1995;25:355–379. doi: 10.1007/BF02179373. [DOI] [PubMed] [Google Scholar]
- Eaves L, Ho H. Young adult outcome of autism spectrum disorders. Journal of Autism and Developmental Disorders. 2008;38:739–747. doi: 10.1007/s10803-007-0441-x. [DOI] [PubMed] [Google Scholar]
- Fombonne E. Epidemiological surveys of pervasive developmental disorders. In: Volkmar F, editor. Autism and Pervasive Developmental Disorders. New York: Cambridge University Press; 2007. pp. 33–68. [Google Scholar]
- Freeman BJ, Del’Homme M, Guthrie D, Zhang F. Vineland Adaptive Behavior scale scores as a function of age and initial IQ in 210 autistic children. Journal of Autism and Developmental Disorders. 1999;21(5):379–384. doi: 10.1023/a:1023078827457. [DOI] [PubMed] [Google Scholar]
- Ghaziuddin M, Ghaziuddin N, Greden J. Depression in persons with autism: Implications for research and clinical care. Journal of Autism and Developmental Disorders. 2002;32 (4):299–306. doi: 10.1023/a:1016330802348. [DOI] [PubMed] [Google Scholar]
- Gillberg C, Steffenburg S. Outcome and prognostic factors in infantile autism and similar conditions: A population-based study of 46 cases followed through puberty. Journal of Autism and Developmental Disorders. 1987;17:273–287. doi: 10.1007/BF01495061. [DOI] [PubMed] [Google Scholar]
- Gillham JE, Carter AS, Volkmar FR, Sparrow SS. Toward a definitional operational definition of autism. Journal of Autism and Developmental Disorders. 2000;30(4):269–278. doi: 10.1023/a:1005571115268. [DOI] [PubMed] [Google Scholar]
- Harris S, Handleman J. Age and IQ at intake as predictors of placement for young children with autism: A four- to six-year follow up. Journal of Autism and Developmental Disorders. 2000;30 (2):137–142. doi: 10.1023/a:1005459606120. [DOI] [PubMed] [Google Scholar]
- Hedrick DL, Prather EM, Tobin AR. Sequenced Inventory of Communication Development—Revised Edition. Seattle, WA: University of Washington Press; 1984. [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45(2):212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Howlin P, Mawhood L, Rutter M. Autism and developmental receptive Language disorder—a follow-up comparison in early adult life. II: Social, Behavioural, and psychiatric outcomes. Journal of Child Psychology and Psychiatry. 2000;41(5):561–578. doi: 10.1111/1469-7610.00643. [DOI] [PubMed] [Google Scholar]
- Iarocci G, Yager J, Elfers T. What gene-environment interactions can tell us about social competence in typical and atypical populations. Brain and Cognition. 2007;65:112–127. doi: 10.1016/j.bandc.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Jones B, Nagin D, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research. 2001;29:374–393. [Google Scholar]
- Klin A, Saulnier C, Sparrow S, Cicchetti D, Volkmar F, Lord C. Social and communication abilities and disabilities in higher functioning individuals with autism spectrum disorders: The Vineland and the ADOS. Journal of Autism and Developmental Disorders. 2007;37:748–759. doi: 10.1007/s10803-006-0229-4. [DOI] [PubMed] [Google Scholar]
- Koegel R, Bimbela A, Schreibman L. Collateral effects of parent training on family interactions. Journal of Autism and Developmental Disorders. 1996;26 (3):347–359. doi: 10.1007/BF02172479. [DOI] [PubMed] [Google Scholar]
- Kraijer D. Review of the adaptive behavior studies in mentally retarded persons with autism/pervasive developmental disorder. Journal of Autism and Developmental Disorders. 2000;30(1):39–47. doi: 10.1023/a:1005460027636. [DOI] [PubMed] [Google Scholar]
- Liss M, Harel B, Fein D, Allen D, Dunn M, Feinstein C, Morris R, Waterhouse L, Rapin I. Predictors and correlates of adaptive functioning in children with developmental disorders. Journal of Autism and Developmental Disorders. 2001;31 (2):219–230. doi: 10.1023/a:1010707417274. [DOI] [PubMed] [Google Scholar]
- Lord C, DiLavore P, Shulman C, Thurm A, Pickles A. Autism from 2 to 9. The Archives of General Psychiatry. 2006;63 (6):694–701. doi: 10.1001/archpsyc.63.6.694. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook E, Leventhal B, DiLavore P, Pickles A, Rutter M. The ADOS-G (Autism Diagnostic Observation Schedule-Generic): A standard measure of social and communication deficits associated with autism spectrum disorder. Journal of Autism and Developmental Disorders. 2000;30:205–223. [PubMed] [Google Scholar]
- Loveland KA, Kelley ML. Development of adaptive behavior in adolescents and young adults with autism and Down Syndrome. American Journal on Mental Retardation. 1988;93:84–92. [PubMed] [Google Scholar]
- McConachie H, Le Couteur A, Honey E. Can a diagnosis of Asperger syndrome be made in very young children with suspected autism spectrum disorder? Journal of Autism & Developmental Disorders. 2005;35:167–176. doi: 10.1007/s10803-004-1995-5. [DOI] [PubMed] [Google Scholar]
- McConnell S. Interventions to facilitate social interaction for young children with autism: Review of available research and recommendations for educational intervention and future research. Journal of Autism and Developmental Disorders. 2000;32 (5):351–372. doi: 10.1023/a:1020537805154. [DOI] [PubMed] [Google Scholar]
- McGovern CW, Sigman M. Continuity and change from early childhood to adolescence in autism. Journal of Child Psychology and Psychiatry. 2005;46:401–408. doi: 10.1111/j.1469-7610.2004.00361.x. [DOI] [PubMed] [Google Scholar]
- Mesibov G, Shea V, Schopler E. The TEACCH Approach to Autism Spectrum Disorders. New York, NY: Kluwer Academic/Plenum Publishers; 2005. [Google Scholar]
- Mullen EM. Manual for the Infant Mullen Scales of Early Learning. Cranston, R.I: T.O.T.A.L Child, Inc; 1985. [Google Scholar]
- Mullen E. Mullen Scales of Early Learning. Circle Pines, MN: American Guidance Service, Inc; 1989. [Google Scholar]
- Muller E, Schuller A, Yates G. Social challenges and supports from the perspective of individuals with Asperger syndrome and other autism spectrum disabilities. Autism. 2008;12 (2):173–190. doi: 10.1177/1362361307086664. [DOI] [PubMed] [Google Scholar]
- Mundy P, Sigman M, Ungerer J, Sherman T. Defining the social deficits of autism: The contribution of nonverbal communication measures. Journal of Child Psychology and Psychiatry. 1986;27(5):657–669. doi: 10.1111/j.1469-7610.1986.tb00190.x. [DOI] [PubMed] [Google Scholar]
- Orsmond G, Krauss M, Seltzer M. Peer relationships and social and recreational activities among adolescents and adults with autism. Journal of Autism and Developmental Disorders. 2004;34(3):245–256. doi: 10.1023/b:jadd.0000029547.96610.df. [DOI] [PubMed] [Google Scholar]
- Ozonoff S, Cathcart K. Effectiveness of a home program intervention for young children with autism. Journal of Autism and Developmental Disorders. 1998;28 (1):25–32. doi: 10.1023/a:1026006818310. [DOI] [PubMed] [Google Scholar]
- Paul R, Miles S, Cicchetti D, Sparrow S, Klin A, Volkmar F, Coflin M, Booker S. Adaptive behavior in autism and pervasive developmental disorder-not otherwise specified: Microanalysis of scores on the Vineland Adaptive Behavior Scales. Journal of Autism and Developmental Disorders. 2004;34 (2):223–228. doi: 10.1023/b:jadd.0000022612.18116.46. [DOI] [PubMed] [Google Scholar]
- Rodrigue JR, Morgan SB, Geffken GR. A comparative evaluation of adaptive behavior in children and adolescents with autism, Down Syndrome, and normal development. Journal of Autism and Developmental Disorders. 1991;21:187–196. doi: 10.1007/BF02284759. [DOI] [PubMed] [Google Scholar]
- Rogers S. Interventions that facilitate socialization in children with autism. Journal of Autism and Developmental Disorders. 2000;30 (5):399–409. doi: 10.1023/a:1005543321840. [DOI] [PubMed] [Google Scholar]
- Rose-Krasnor L. The nature of social competence: A theoretical review. Social Development. 1997;6 (1):11–135. [Google Scholar]
- Rumsey J, Rapoport J, Sceery W. Autistic children as adults: Psychiatric, social, and behavioral outcomes. Journal of the American Academy of Child Psychiatry. 1985;24:465–473. doi: 10.1016/s0002-7138(09)60566-5. [DOI] [PubMed] [Google Scholar]
- Scattonne D. Social skills interventions for children with autism. Psychology in the Schools. 2007;44 (7):717–726. [Google Scholar]
- Schatz J, Hamdan-Allen G. Effects of age and IQ on adaptive behavior domains for children with autism. Journal of Autism and Developmental Disorders. 1995;25(1):51–61. doi: 10.1007/BF02178167. [DOI] [PubMed] [Google Scholar]
- Seltzer M, Krauss M, Shattuck P, Orsmund G, Swe A, Lord C. The symptoms of autism spectrum disorders in adolescence and adulthood. Journal of Autism and Developmental Disorders. 2003;33 (6):565–581. doi: 10.1023/b:jadd.0000005995.02453.0b. [DOI] [PubMed] [Google Scholar]
- Seltzer M, Shattuck P, Abbeduto L, Greenberg J. Trajectory of development in adolescents and adults with autism. Mental Retardation and Developmental Disabilities. 2004;10:234–247. doi: 10.1002/mrdd.20038. [DOI] [PubMed] [Google Scholar]
- Shattuck P, Seltzer M, Greenberg J, Orsmond G, Bolt D, Kring S, Lounds J, Lord C. Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37:1735–1747. doi: 10.1007/s10803-006-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonoff E, Pickles A, Charman T, Chandler S, Loucas T, Baird G. Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of the American Academy of child and Adolescent Psychiatry. 2008;47 (8):921–929. doi: 10.1097/CHI.0b013e318179964f. [DOI] [PubMed] [Google Scholar]
- Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales (Survey Form) Circle Pines, Minn: American Guidance Service; 1984. [Google Scholar]
- Sparrow S, Cicchetti D, Balla D. Vineland Adaptive Behavior Scales–II (Survey Form) Circle Pines, MN: American Guidance Service; 2005. [Google Scholar]
- Starr E, Szatmari P, Bryson S, Zwaigenbaum L. Stability and change among high-functioning children with pervasive developmental disorders: A 2-year outcome study. Journal of Autism and Developmental Disorders. 2003;33:15–23. doi: 10.1023/a:1022222202970. [DOI] [PubMed] [Google Scholar]
- Stone W, Yoder P. Predicting spoken language in children with autistic spectrum disorders. Autism. 2001;5(4):341–361. doi: 10.1177/1362361301005004002. [DOI] [PubMed] [Google Scholar]
- Stutsman R. Guide for administering the Merrill-Palmer Scale of Mental Tests. New York: Harcourt, Brace and World; 1948. [Google Scholar]
- Szatmari P, Bryson SE, Boyle MH, Streiner DL, Duku E. Predictors of outcome among high functioning children with autism and asperger syndrome. Journal of child psychology and psychiatry. 2003;44:520–528. doi: 10.1111/1469-7610.00141. [DOI] [PubMed] [Google Scholar]
- Szatmari P, Bryson S, Streiner D, Wilson F, Archer L, Ryerse C. Two-year outcome of preschool children with autism or Asperger’s syndrome. American Journal of Psychiatry. 2000;157 (12):1980–1987. doi: 10.1176/appi.ajp.157.12.1980. [DOI] [PubMed] [Google Scholar]
- Szatmari P, Merette C, Bryson S, Thivierge J, Roy M, Cayer M, Maziade M. Quantifying dimensions in autism: A factor-analytic study. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41 (4):467–474. doi: 10.1097/00004583-200204000-00020. [DOI] [PubMed] [Google Scholar]
- Tager-Flusberg H, Paul R, Lord C. Language and communication in autism. In: Volkmar F, Paul R, Klin A, Cohen D, editors. Handbook of Autism and Pervasive Developmental Disorders. Indianapolis, IN: John Wiley & Sons, Inc; 2005. pp. 335–364. [Google Scholar]
- Venter A, Lord C, Schopler E. A follow-up study of high-functioning autistic children. Journal of Child Psychology and Psychiatry. 1992;33:489–507. doi: 10.1111/j.1469-7610.1992.tb00887.x. [DOI] [PubMed] [Google Scholar]
- Verbeke G, Molenberghs G. Linear Mixed Models for Longitudinal Data. New York, NY: Springer-Verlag; 2000. [Google Scholar]
- Volkmar FR, Carter A, Sparrow SS, Cicchetti DV. Quantifying social development in autism. Journal of the American Academy of Child and Adolescent Psychiatry. 1993;32:627–632. doi: 10.1097/00004583-199305000-00020. [DOI] [PubMed] [Google Scholar]
- Volkmar F, Sparrow S, Gourdreau D, Cicchetti D, Paul R, Cohen D. Social deficits in autism: An operational approach using the Vineland Adaptive Behavior Scales. American Academy of Child and Adolescent Psychiatry. 1987;26 (2):156–161. doi: 10.1097/00004583-198703000-00005. [DOI] [PubMed] [Google Scholar]
- White S, Koenig K, Scahill L. Social skills development in children with autism spectrum disorders: A review of the intervention research. Journal of Autism and Developmental Disorders. 2007;37:1858–1868. doi: 10.1007/s10803-006-0320-x. [DOI] [PubMed] [Google Scholar]
- Wilkenson K. Profiles of language and communication skills in autism. Mental Retardation and Developmental Disabilities. 1998;4:73–79. [Google Scholar]