Abstract
Objectives
to assess the impact of Medicare Part D in the nursing home (NH) setting.
Design
a population-based study using 2005–2006 prescription dispensing records, Poisson regressions with generalized estimating equations, and interrupted times series estimation with segmented regression methods.
Participants
a nationwide sample of long-stay Medicare enrollees in NHs (n=861,082)
Measurements
probability of Part D enrollment, changes in source of drug payments, changes in average number of monthly prescriptions dispensed per resident.
Results
In 2006, 81% of NH residents enrolled in Part D, 16% had other drug coverage, and 3% (n=11,000) remained without drug coverage, which was the same rate of no drug coverage as in 2005. NH residents who did not enroll in Part D were the oldest old (RR 0.82, p<.000), had no drug coverage in 2005 (RR 0.84, p<.001), and had high comorbidity burden (RR 0.94, p<.000). The proportion of prescription drugs paid out-of-pocket decreased from 11% in 2005 to 8% in 2006 (p<.001). Average monthly prescription use per resident in 2006 decreased by half a prescription relative to 2005 levels (9.6 scripts vs. 10.1 scripts, p<.003).
Conclusions
Part D decreased some out-of-pocket drug costs, but did not expand drug coverage in the NH population or reach some vulnerable segments. Part D was also associated with some disruption in NH drug use, especially right after implementation.
Keywords: Medicare, prescription drugs, nursing home
Introduction
Nursing home (NH) residents make up a sizeable but unknown proportion of the 23 million Medicare beneficiaries who enrolled into Medicare Part D in 2006.(1) Medicare Part D is a voluntary prescription drug benefit offered by the Medicare program but administered by private drug plans. Nearly 3.5 million elderly and disabled Americans receive care in NHs, with about half needing to stay in the facility for an extended period of time until death.(2, 3) Prescription drug therapies are a mainstay of care in NHs; residents receive an average of 8 different medications per month.(4) Annual spending for prescription drugs in NHs exceeded $12 billion in 2003, accounting for 11% of all spending for NH care.(3, 5) However, despite the special status of NH residents and their high need for prescription drugs, Part D had no separate system of enrollment for NH residents. NH residents with dual coverage through Medicare and Medicaid (approximately 66% of the population) were randomly-assigned, if they did not select a plan, into eligible Part D plans alongside their community-dwelling counterparts. Residents without Medicaid coverage could select a Part D plan from among the nearly 1,500 plans available to all Medicare beneficiaries.
The Medicare Prescription Drug, Improvement, and Modernization Act of 2003, which created Medicare Part D, mentioned NHs only in regard to ensuring convenient access to pharmacies.(6) Subsequent policies have evolved to accommodate NH residents in the prescription drug program. First, all plans qualifying as a Part D provider must be able to serve NH residents, which includes contracting with a long-term care pharmacy provider to offer required NH pharmacy services. For instance, NHs may require medications in blister pack packaging or medications delivered on an emergency basis 24-hours-a-day. Second, Part D plans must offer the same drug formulary to all enrollees regardless of residence in NHs.(7) Third, NHs cannot “require, request, coach, or steer” residents into a particular Part D plan,” although NHs may provide information and education on Part D to residents and family members.(7, 8) Fourth, NH residents may switch plans throughout the year. Lastly, NH residents with dual-Medicaid eligibility do not incur copays.
The impact of Part D on medication use would depend on whether the program expanded coverage to individuals previously without drug benefits or merely replaced existing and possibly more generous forms of drug coverage. Before Part D, about 80% of NH residents had prescription drug coverage, and most of it came from generous Medicaid programs.(9)After Part D, Medicare assumed most of the responsibility for the medication costs of dually-eligible NH residents. In addition, many states instituted wrap-around policies for coverage gaps in Part D such as medications excluded by Medicare (e.g., benzodiazepines) or those rejected by a Part D plan. NH residents could experience decreases in coverage and drug use if the state wrap-around policy was less generous than the previous Medicaid coverage. Previous studies have assessed only the adequacy of Part D formularies in covering medications commonly prescribed in NHs, and the potential implications of Part D for stakeholders in the long-term care marketplace.(10, 11) The purpose of this study is to assess: 1) enrollment into Part D and predictors of that enrollment; 2) changes in the sources of drug payments in NHs, particularly in out-of-pocket payments, before and after Part D; and 3) changes in overall prescription drug use in NHs, before and after Part D. To our knowledge, this is the first study of actual drug utilization in NHs before and after Part D.
Methods
Study population
We analyzed January 2005–December 2006 monthly prescription drug dispensing records provided by a large long-term care pharmacy provider. These data come from over 2.5 million unique individuals living in nearly 16,000 NHs from 48 states. These individuals have a variety of prescription drug plans, including private insurance, Medicaid, Medicare Part D, or no drug coverage at all. The drug dispensing data include all medications prescribed and administered to residents, including over-the-counter drugs and PRN medications (as needed). Research using these data has been previously described.(12) The data elements include the product identification code (national drug code), date of script, days’ supply, quantity dispensed, and payment source, as well as individual identifiers, basic demographics, limited to gender and age, and the state where the NH was located.
We excluded individuals who were not Medicare eligible (n= 626,067) or observed for less than 4 months (n=1,048,535). Short-stayers in NHs (< 4 months) may have their medications paid for by Medicare Part A, rather than Part D, as part of bundled per diem payments to the facility. In addition, prior research shows that short-stayers in NHs differ significantly from long-stay residents.(4) Preliminary analyses of the data showed uneven capture of payment sources for January 2005 and the first month of the Part D program (January 2006) so estimates related to payment sources for those months are not reported here. We also identified a subsample of residents who were observed for at least 1 month in 2005 and 2006 (n=459,577) for selected analyses.
Enrollment into Medicare Part D was determined from the sources of drug payments. The dispensing data provided the following source of payments for each dispensing: cash, Medicaid, third-party, facility/hospice, Medicare A & B, and Medicare D. Part D enrollees had at least 1 medication dispensed in 2006 that was paid for by Medicare D. Individuals who had no medication payments from Medicare D were categorized as having either third-party drug coverage or no drug coverage. Individuals without drug coverage had only cash payments for their medications in 2006, while those with third-party drug coverage had at least 1 medication in 2006 paid for from that source. Prescription use was characterized as a sum of all pharmacologic products dispensed each month, including over-the-counter products (e.g., vitamins), and combination products, which were counted as a single drug. Demographic characteristics were drawn from the first month of observation. State of residence came from the location of the nursing facility and was collapsed into the four major U.S. census regions: Midwest, Northeast, South and West. Comorbidity scores were generated from the national drug codes using a normalized Chronic Disease Score measure.(13)
Statistical analysis
We conducted all analyses using person-month level data. Interrupted times series estimation with segmented regression methods and autoregressive correlations of the first order were used for testing changes in the trend (slope and level) of drug use following the implementation date of the Part D program and controlling for pre-policy trends.(14) Advantages of this approach include an explicit method for using historical trends to test for a treatment effect. If Part D had any impact, the observations after January 2006 will display a distinctly different pattern of use from the pattern of use prior to that time. Disadvantages include the inability to test whether Part D rather than some other concurrent force caused any disruption observed after January 2006. The relative risk ratios of enrolling in Part D were calculated using Poisson regressions and generalized estimating equations to account for repeated measurements on the same individuals.(15) The entire sample was used in analyses to establish population-level patterns of costs and average drug use before and after Part D. Subgroup analyses were conducted by 2005 status of drug coverage (Medicaid, Third-party, or none) and by Part D enrollment status. The institutional review board of the University of Massachusetts Medical School exempted this research from review.
Results
We identified 861,082 long-stay Medicare enrollees in NHs who generated 2,535,684 person-months and 106,038,595 prescription records during the study period 2005–2006 (Table 1). About 13% of the population was under the age of 65 (entitled to the Medicare program through a disabling condition) and 36% were 85 years or older. Over two-thirds (69%) were female and the majority lived in facilities in the Midwest (34%) or South (30%). Among those observed in 2005, 11% had a chronic disease score that significantly exceeded the population average. At least 86% had some form of drug coverage in 2005. On average, these NH residents received 76 (SD 64) prescriptions in 2005.
Table 1.
Description of Study NH Population, n=861,082
| % Total Population | |
|---|---|
| Age | |
| <64 | 13 |
| 65–74 | 14 |
| 75–84 | 35 |
| 85+ | 36 |
| Unknown | 2 |
| Gender | |
| Male | 31 |
| Female | 69 |
| Unknown | 1 |
| Geographic Residence | |
| Northeast | 24 |
| Midwest | 36 |
| South | 28 |
| West | 11 |
| Unknown | 1 |
| Normalized Chronic Disease Score in 2005* | |
| <.50 | 15 |
| .50–1.50 | 74 |
| >1.50 | 11 |
| Drug coverage in 2005* | |
| Has drug coverage | 86 |
| -From Medicaid† | 62 |
| -From third-party† | 44 |
| No drug coverage (cash-only drug payments) | 3 |
| Status unknown (drug payments from only Medicare or hospice/facility) | 11 |
| Annual number of prescriptions in 2005*, mean (SD) | 76 (64) |
Includes only 459, 577 individuals with 2005 observations
Percentages do not equal 100% due to non-mutually exclusive categories.
Sources of Drug Payment and Enrollment Rates
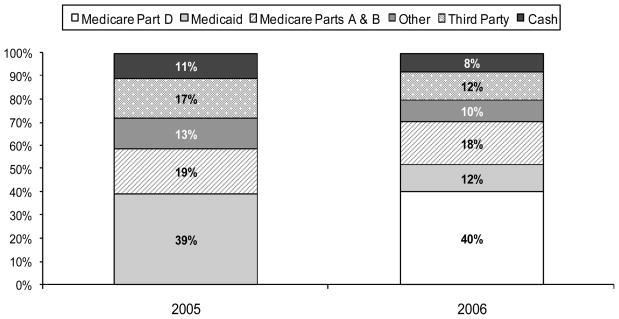
Figure 1 shows the changes in the sources of drug payments before and after Part D for the whole population. In 2005, 39% of all medications for NH residents were paid for by Medicaid, followed by Medicare Parts A and B (19%), third-parties (17%), other sources (13%), and cash (11%). In 2006, Medicare Part D became the main payer of NH drugs (40%), primarily by assuming payments from Medicaid and other third-party sources and also by assuming about 3% of the payments made previously out-of-pocket. Medicaid’s share of NH drug payments dropped by two-thirds between 2005 and 2006 (from 39% to 12%), third-parties’ share dropped by almost a third (17% to 12%), and cash payments also dropped by almost a third (11% to 8%). Only Medicare Parts A and B continued paying about the same proportion of NH drug payments in 2005 and 2006.
Figure 1.
Sources of Drug Payments for NH Residents, 2005–2006.
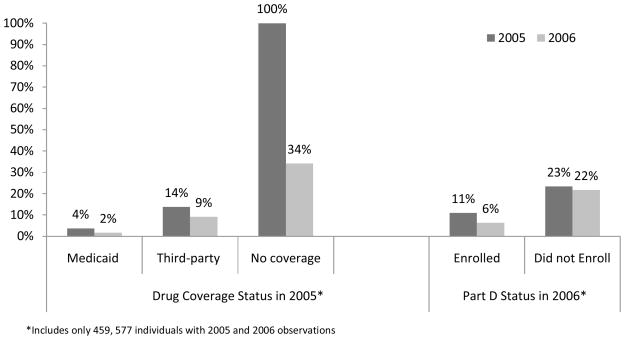
NH residents who had no drug coverage before Part D experienced the largest changes in drug costs paid of out-of-pocket. On average, their share of drug costs decreased from 100% in 2005 to 34% in 2006 (see Figure 2). In comparison, the out-of-pocket share decreased from 4% to 2% for those with Medicaid in 2005, and from 14% to 9% for those with third-party drug coverage in 2005. Overall, those who enrolled in Part D experienced declines in their share of out-of-pocket medication costs (11% in 2005 vs. 6% in 2006), while those who did not enroll experienced no difference (23% in 2005 vs. 22% in 2006).
Figure 2.
Changes in Share of Total Drug Costs Paid Out-of-Pocket by NH Residents.
In February 2006, 73% of the study NH population was enrolled in Part D and by December the enrollment rate was at 81%. Rates of drug coverage from sources other than Part D declined from 21% to 16% during the same period, while the proportion of the population without any drug coverage dropped from 6% to 3% by the end of the year.
Table 2 lists the characteristics of NH residents by their enrollment status into Part D. In the multivariate model, older age predicted nonenrollment (RR 0.82 for age 85 or older vs. younger than 65, p<.0001), as did higher comorbidity burden (RR 0.96 for CDS >1.50 relative to CDS <.50), p<.0001), and having private drug coverage (RR 0.85) or no drug coverage (RR 0.84) in 2005 relative to Medicaid, p<.001). In addition, male NH residents were less likely to enroll relative to females, as were NH residents in the Midwest and West relative to residents in the South.
Table 2.
Risk Factors for Part D Enrollment Status
| % Enrolled in Part D | Total Population* |
||
|---|---|---|---|
| Unadjusted relative risk ratios | Adjusted relative risk ratios | ||
| Age | |||
| <64 | 97 | Ref | Ref |
| 65–74 | 88 | 0.92 | 0.92‡ |
| 75–84 | 81 | 0.84‡ | 0.84‡ |
| 85+ | 78 | 0.82‡ | 0.82‡ |
| Gender | |||
| Male | 83 | Ref | Ref |
| Female | 83 | 1.00 | 1.02‡ |
| Residence | |||
| Northeast | 85 | 1.01‡ | 1.01‡ |
| Midwest | 82 | 0.99‡ | 0.99‡ |
| South | 83 | Ref | Ref |
| West | 82 | 0.98‡ | 0.98‡ |
| Normalized Chronic Disease Score in 2005 | |||
| <.50 | 87 | Ref | Ref |
| .50–1.50 | 83 | 0.96‡ | 0.99‡ |
| >1.50 | 82 | 0.94‡ | 0.96‡ |
| Drug coverage in 2005† | |||
| Medicaid | 97 | 1.56‡ | N/A |
| Third-party | 76 | 0.85‡ | N/A |
| No coverage | 70 | 0.84‡ | N/A |
Includes 459,577 individuals with 2005 and 2006 observations
Reference is all other coverage types.
p<0.001
N/A= N/A=Drug coverage in 2005 is not included in the full model due to endogeneity with covariates. Stratefied analyses by drug coverage status are available from authors.
Subgroup analyses with the same model specifications, showed similar results with the following exceptions. Among NH residents without any drug coverage in 2005, having a higher chronic disease score increased the likelihood of enrollment, data not shown. Among NH residents with private drug coverage in 2005, residence in the Northeast increased the likelihood of Part D enrollment relative to residence in the South, as did having a higher chronic disease score. For NH residents with Medicaid in 2005, residence in the South decreased the likelihood of Part D enrollment relative to residence in the other areas, data not shown.
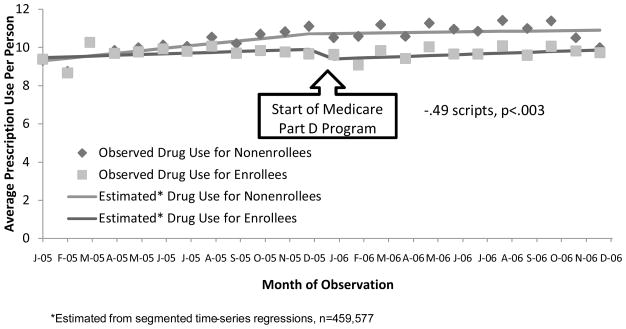
Part D and Average Prescription Drug Use
In the 12 months prior to implementation of Part D, the entire NH sample averaged 10.1 scripts per month. Times-series regressions show that after initiation of the Part D program, average use dropped by half a prescription relative to 2005 levels (−.49 scripts, p<.003) and did not resume pre-Part D levels until December of 2006 (data not shown). Figure 3 shows that average drug use dropped only for Part D enrollees relative to their 2005 levels (−.51 scripts, p<.006) while remaining stable for nonenrollees (−.05 scripts, p<.868). Residents without any drug coverage in 2005 experienced the largest decrease in average monthly drug use (−.77 scripts, p<.001, data not shown). (It should be noted that this group also had higher average use in 2005, 10.5 scripts, and this may have been a regression to the mean effect). In comparison, average monthly drug use changed by −.50 scripts (p<.002) for NH residents with Medicaid in 2005, and −.29 scripts (p<.003) scripts for residents with third-party drug coverage in 2005, data not shown.
Figure 3.
Changes in Prescription Use by NHs by Part D enrollment.
Discussion
The Medicare Part D prescription drug program was implemented to improve access to medications among all Medicare enrollees. Achievement of these goals was mixed in the NH setting. In this analysis of over 800,000 long-staying NH residents, we found a modest decrease of 3 percentage points (11% in 2005 vs. 8% in 2006, p<.05) in the proportion of prescription drugs paid for out-of-pocket. This finding compares to the 9%–13% relative out-of-pocket savings due to Part D observed in the community-setting.(16) This difference may have been due to the high proportion of NH residents with Medicaid, since that program generally requires little or no cost-sharing for medications. NH residents without drug coverage prior to Part D experienced the largest relief in drug costs, although they were a relatively small group (<3% of the study population.
The Part D program did not appear to have expanded drug coverage in the NH setting, unlike in the community-setting where rates of having no drug coverage dropped from 30% to 10% between 2005 and 2006.(17) Instead, the percentage of NH residents without any drug coverage remained at a stable 3% in the 1 year before and after Part D. Part D substituted for former sources of drug coverage, primarily Medicaid. It is possible, though, that temporary drug payment assistance, such as Medicare Part A, may have masked expansions in drug coverage.
The NH residents who did not enroll in Part D exhibited characteristics of some of the most vulnerable segment of the NH population, namely the oldest old (aged 85+), those without prior drug coverage, and those with the highest comorbidity burden. These findings are unique from those in the community-setting where Part D non-enrollers tended to be in better health status than the enrollers.(17) By the end of 2006, approximately 11,000 Medicare enrollees in NHs still had no drug coverage. Our analysis cannot explain this finding but it is troubling and suggests the need for facilitated Part D enrollment for all Medicare-eligible NH residents who have no evidence of other drug coverage.
Overall patterns of drug use in NHs were disrupted in the early months of Part D; initiation of the new program coincided with a statistically significant decrease in average monthly prescription use per resident of half a prescription relative to 2005 levels (10.1 vs. 9.6, p<.003). The reduction appears to have been temporary as average drug use gradually returned to 2005 levels by December of 2006. This finding is also different from the experience of Medicare enrollees in the community where, overall drug use increased slightly (1.1%) after Part D.(16) Our findings of a modest but temporary reduction in drug use in NHs are somewhat substantiated by a small survey of NH stakeholders (n=31) who reported that Part D increased the drug management processes in the NH setting and shifted drug use within therapeutic classes.(11, 18, 19) Part D plans often employed prior authorization, step therapy protocols, tiered formularies, and quantity limits. Furthermore, one long-term care pharmacy provider indicated a need to be more aggressive in seeking reimbursement for dispensed drugs as the magnitude of drug claims rejected by Part D plans grew.(11, 18) However, this same group also reported no overt changes in gross drug use in NHs following the implementation of Part D. It is yet to be determined if this temporary disruption in medication use caused any untoward consequences to the health of the NH population.
Lastly, the Part D program decreased but did not eliminate Medicaid’s burden in paying for the medications of dual-eligibles in NHs. The fact that Medicaid paid for 12% of the medications dispensed in 2006 to our study population indicates the scope of gaps in Part D coverage. Medicaid wrap-around coverage varies by state but generally covers medications rejected from coverage by the Part D provider or excluded by Medicare (e.g., benzodiazepines or prescription vitamins.)
It should be noted that our analyses were limited to NH residents whose prescriptions were dispensed by 1 long-term care pharmacy provider and these results may not be nationally representative of all Medicare enrollees in NHs. However, a comparison of the geographic residence of our study sample to that of the nursing home residents in the December 2006 CMS OSCAR Data survey shows a similar distribution (Northeast: 24% vs. 23%; Midwest 36% vs. 29%; South 28% vs. 34%, and West 11% vs. 14%).(20) Our study represents one of the first analyses of the effects of Part D on NH residents, and it reflects the observed experiences of nearly half of the entire Medicare population living in NHs.
Our approach has several strengths. First, we conducted these times-series analyses of changes in costs and drug utilization using an intention-to-treat study design, without regard for enrollment into Part D. This meant that we avoided introducing the selection bias inherent in comparing changes in drug use between individuals who selected into Part D and those who did not, a confounding potentially affecting the estimates of the non-Medicaid NH population. In addition, time-series analyses are robust to many of the threats to the validity of weaker observational designs, particularly in unmeasured changes in the composition of the study population or in survivor bias of cohort studies requiring a long observation in a NH population.(14)
Limitations of the study include the following. First, our dataset was quite limited in a number of potentially important characteristics of the nursing home residents; we did not have information on race, socio-economic status or education. Thus, we could not ascertain if certain NH populations experienced more difficulty in enrolling in Part D or more disruptions in drug use than other groups. The comorbidity scores were based on only medication use but these are validated and robust measures and the recommended approach when the pharmacy claims data are the only source of information on health status.(21) Secondly our times series were short, and far less than the 100 data points recommended to rule out seasonal effects, although this possibility is unlikely given the visual pattern of data.(14) Short time series are valuable though, especially in helping to specify the degree of the immediate impact and the persistence of any delayed impact, which is difficult or impossible to do with other study designs.(22)
Conclusions
We estimate that the Medicare Part D led to a modest benefit to the NH population limited to a modest decrease in out-of-pocket drug costs. This decrease most likely resulted from some additional generosity associated with the new benefit compared to former sources as we did not detect any expansion in new drug coverage for NH residents. The costs of Part D in the NH setting included a slight disruption in drug use in the early months after initiation. In addition, a substantial number of vulnerable NH residents did not enroll in the program and many remained without drug coverage throughout 2006. Overall, Part D had a different impact in the NH setting compared to that in the community, which highlights the need for further work focusing on how Part D can best serve Medicare enrollees in NHs. It will be especially important to examine whether the impact of the new Medicare program on drug use as described in this study had any effects on the health outcomes of this special population.
Acknowledgments
All individuals listed as authors have contributed significantly to this work to qualify as authors and the corresponding author has obtained written consent from all contributors acknowledged.
Sponsor’s Role. Funding for this study came from The Robert Wood Johnson Foundation. This funding source had no role in the design, methods, data analysis or interpretation or the preparation of this manuscript.
Footnotes
Conflict of Interest. None of the authors of this manuscript have conflicts of interest to declare.
Authors Contributions. Study concept and design: Briesacher, Gurwitz, Soumerai, Field
Acquisition of data: Briesacher
Analysis and interpretation of the data:Briesacher, Gurwitz, Soumerai, Field, Fouayzi
Drafting of the manuscript: Briesacher, Gurwitz, Soumerai, Field
Critical revision of the manuscript: Briesacher, Gurwitz, Soumerai, Field, Fouayzi
Statistical analysis:Briesacher, Soumerai, Field, Fouayzi
Obtained funding: Briesacher
Administrative support: Fouayzi
Study supervision: Briesacher
References
- 1.Kaiser Family Foundation. Medicare---a primer. 2007. [Google Scholar]
- 2.Voyer P, Verreault R, Mengue PN, et al. Prevalence of insomnia and its associated factors in elderly long-term care residents. Arch Gerontol Geriatr. 2006;42:1–20. doi: 10.1016/j.archger.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Medicare & Medicaid Services. Issue Paper. Rockville, MD: 2005. High Quality Access to Long-Term Care Pharmacies. [Google Scholar]
- 4.Doshi JA, Shaffer T, Briesacher BA. National estimates of medication use in nursing homes: findings from the 1997 medicare current beneficiary survey and the 1996 medical expenditure survey. J Am Geriatr Soc. 2005;53:438–443. doi: 10.1111/j.1532-5415.2005.53161.x. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Medicare & Medicaid Services. National Health Expenditures by Type of Service and Source of Funds: Calendar Years 2005-1960. 2005. [Google Scholar]
- 6.Speaker of the House of Representatives. The Medicare Prescription Drug, Improvement, and Modernization Act of 2003. 2003. [Google Scholar]
- 7.Centers for Medicare & Medicaid Services. Long Term Care Guidance. Mar 16, 2005. [Google Scholar]
- 8.Hamilton TE. In: Nursing Homes and Medicare Part D. Directors SSA, editor. Baltimore: Center for Medicaid and State Operations/Survey Certification Group; 2006. [Google Scholar]
- 9.Stuart B, Simoni-Wastila L, Baysac F, et al. Coverage and use ofprescription drugs in nursing homes: implications for the Medicare modernization act. Medical Care. 2006 doi: 10.1097/01.mlr.0000199652.15293.fc. (forthcoming) [DOI] [PubMed] [Google Scholar]
- 10.Stevenson DG, Huskamp HA, Keating NL, et al. Medicare part d and nursing home residents. J Am Geriatr Soc. 2007;55:1115–1125. doi: 10.1111/j.1532-5415.2007.01287.x. [DOI] [PubMed] [Google Scholar]
- 11.Stevenson DG, Huskamp HA, Newhouse JP. Medicare Part D, Nursing Homes, and Long-Term Care Pharmacies. Washington, DC: MedPAC; 2007. [Google Scholar]
- 12.Stefanacci RG. The cost of being excluded: impact of excluded medications under medicare part d on nursing home residents. J Am Med Dir Assoc. 2005;6:415–420. doi: 10.1016/j.jamda.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 13.Clark DO, Von Korff M, Saunders K, et al. A chronic disease score with empirically derived weights. Med Care. 1995;33:783–795. doi: 10.1097/00005650-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Wagner AK, Soumerai SB, Zhang F, et al. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- 15.Greenland S. Model-based estimation of relative risks and other epidemiologic measures in studies of common outcomes and in case-control studies. Am J Epidemiol. 2004;160:301–305. doi: 10.1093/aje/kwh221. [DOI] [PubMed] [Google Scholar]
- 16.Yin W, Basu A, Zhang JX, et al. The Effect of the Medicare Part D Prescription Benefit on Drug Utilization and Expenditures. Ann Intern Med. 2008 doi: 10.7326/0003-4819-148-3-200802050-00200. [DOI] [PubMed] [Google Scholar]
- 17.Neuman P, Strollo MK, Guterman S, et al. Medicare prescription drug benefit progress report: findingsfrom a 2006 national survey of seniors. Health Aff (Millwood) 2007;26:w630–643. doi: 10.1377/hlthaff.26.5.w630. [DOI] [PubMed] [Google Scholar]
- 18.Huskamp HA, Stevenson DG, Keating NL, et al. Rejections of drug claims for nursing home residents under Medicare Part D. Health Aff (Millwood) 2008;27:560–567. doi: 10.1377/hlthaff.27.2.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stevenson DG, Huskamp HA, Newhouse JP. Medicare part D and the nursing home setting. Gerontologist. 2008;48:432–441. doi: 10.1093/geront/48.4.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.American Health Care Association; Health Services Research and Evaluation Group. Nursing Facility Total, Average and Median Number of Patients Per Facility and ADL Dependence. CMS OSCAR Data Current Surveys; Washington, DC: 2006. [Google Scholar]
- 21.Schneeweiss S, Wang PS, Avorn J, et al. Improved comorbidity adjustment for predicting mortality in Medicare populations. Health Serv Res. 2003;38:1103–1120. doi: 10.1111/1475-6773.00165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston: Houghton Mifflin Company; 2002. [Google Scholar]