Abstract
Hematological parameters and the state of liver cells of rats were examined in vivo after the animals received aflatoxin B1 (AfB1) alone and together with modified nanodiamonds (MND) synthesized by detonation. The rats that had received the MND hydrosol had elevated leukocyte levels, mainly due to higher granulocyte counts and somewhat increased monocyte counts compared to control rats. Hematological parameters of the rats that had received AfB1 alone differed from those of the control rats in another way: total white blood cell counts were significantly lower due to the decreased lymphocyte counts. In rats that had consumed AfB1 with the MND hydrosol, changes in hematological parameters were less pronounced than in rats that had consumed either AfB1 or MND. Electron microscopy showed that hepatocytes of the rats that had received the MND hydrosol or AfB1 with the MND hydrosol contained elevated levels of lipid inclusions and lysosomes. Hyperplasia of the smooth endoplasmic reticulum (EPR) was revealed in liver specimens of the rats that had received AfB1. Results of the study suggest the conclusion about mutual mitigation of the effects of nanoparticles and the mycotoxin on rats blood and liver cells after AfB1 has adsorbed on MND.
Keywords: Nanodiamonds, Aflatoxin B1, Detoxification, Adsorbent
Introduction
Aflatoxins are secondary metabolites produced by Aspergillus —a widely occurring genus of mold fungi. Food and feed products infested by mold fungi can be contaminated with aflatoxins. This is a serious hazard to animal and human health, as aflatoxins are mutagenic and carcinogenic. Aflatoxin B1 (AfB1) is the most hazardous mycotoxin in this group, and there is no threshold concentration for its toxic effect. The main target of AfB1 is liver and it undergoes transformations in hepatocytes: biotransformation to active AfB1-8,9-epoxide, which gets bound with DNA; irreversible hydroxylation, forming metabolites M1, P1, and Q1; reversible hydroxylation, forming aflatoxicol [1-5]. Aflatoxins that come into animal and human gastrointestinal systems with contaminated food can be mitigated by various enterosorbents [6-9].
Modified nanodiamonds (MND) synthesized by detonation can be proposed as intestinal adsorbent of mycotoxins. A highly developed MND surface, as well as the presence of various chemically active functional groups, hydrocarbon fragments, and metal microimpurities on the surface of nanoparticles, determines their high affinity for sorption of biomolecules [10-12]. Some physicochemical properties of the nanodiamond surface are presented in the work of Gibson et al. [13]. MND have good colloidal stability in dispersion media and are adapted for biological and medical studies. Thus, MND hydrosols can be used for all kinds of injections and oral administration of nanoparticles to animals in long-duration experiments. We proved in animal experiments that MND are highly biocompatible [14]. Low toxicity of nanodiamonds was reported by A. Schrand et al. [15].
In this study, we examined the effect of AfB1 on hematological parameters and the state of liver cells of rats that orally received AfB1 alone and together with MND.
Experimental Works
Rats
Experiments were conducted on adult Wistar rats, which were kept in a vivarium, under similar conditions. The rats were randomly divided into 4 groups (3 animals per group). Every rat was kept in its own cage. Animals of the control (Group 1) drank water. Animals of the treatment groups drank an MND hydrosol containing 0.4 wt% nanoparticles (Group 2), an aqueous solution of AfB1 (Group 3), an MND hydrosol (0.4 wt%) containing AfB1 (Group 4). Every rat of groups 3 and 4 received the amount of the liquid proportional to its body mass. Thus, the total amounts of AfB1 per 1 g weight orally received by the rats were equal for all animals of these groups. After the rats had consumed the AfB1-containing liquids for 10 days, they received water (Group 3) or MND hydrosol (Group 4) within approximately 25 days. This 25-day period was used for a more complete manifestation of the cumulative effect of the AfB1 in animals. The total duration of the experiment was 35 days.
Aflatoxin B1
AfB1 used in this study was analytical grade and supplied by «Ecolan» (Russia) as the standard for HPLC. One ampoule contained 10 μg mycotoxin dissolved in 1 mL acetonitrile. Aqueous AfB1 solution was prepared by substituting distilled water for acetonitrile.
Preparation of MND and MND with AfB1
MND of 4- to 250-nm grade (Brand RUDDM 0–0.25) produced by detonation in “Real-Dzerzhinsk” Ltd. (Russia) were used in the experiments. The MND hydrosol (0.4 wt%) was prepared by adding distilled water to nanoparticle powder. The AfB1-containing MND hydrosol was prepared by adding a mycotoxin aqueous solution to the nanoparticle hydrosol. The amounts of free AfB1 and AfB1 bound with nanoparticles were determined by spectral analysis. For this purpose, after adding AfB1 aqueous solution to the MND hydrosol samples, they were stirred in a Vortex-Genie 2 g-560E (Scientific Industries, Inc., USA) for 10 s and incubated for 2 min at room temperature, and the particles were then collected by centrifugation (Centrifuge 5415R, Eppendorf, Germany) at 14,100g for 10 min. The ability of nanoparticles to coagulate was used for their more complete removal. For this purpose, the specimens were supplemented with NaCl at a concentration of 80–100 mM before centrifugation. The supernatants obtained were assessed by spectral analysis in the range of 200–500 nm at an UVIKON-943 UV/VIS spectrophotometer (Kontron Instruments, Italy).
Hematological and Electron Microscopic Analyses
After the end of the experiment, we took samples of blood from the animals for hematological analysis. Hematological parameters were evaluated using an ABX MICROS-60 hematology analyzer (France). Then the rats were killed, in compliance with the euthanasia principles, and liver samples were taken for transmission electron microscopic (TEM) examination. Liver tissue samples were fixed in 2.5% glutaraldehyde in 0.1 M cacodylate buffer at pH 7.2; then they were additionally fixed in a 1% OsO4 solution in the same buffer. The samples were dehydrated in graded series of ethanol and in acetone; then they were embedded in Epon 812-Araldite M epoxy resin mixture (“Serva”). Ultrathin sections were cut using a Reichert Um-03 ultramicrotome (Austria) and stained with a 3% of uranil acetate in 30% ethanol solution and 0.2% aqueous solution of lead citrate and examined in the JEM 1400 (JEOL, Japan).
The data were statistically processed by Microsoft Excel 2003 software. The confidence level was α = 0.05.
Results and Discussion
Our earlier in vitro experiments have demonstrated that the addition of MND leads to a rapid AfB1 adsorption by nanoparticles, the incubation time does not exceed 2–3 min. An increase in the incubation time from several minutes to several hours did not elevate the amount of adsorbed mycotoxin [11]. It has been showed (Fig. 1) that the AfB1 sorption capacity of MND depends on the ratio of the mycotoxin to sorbent. For example, the data demonstrate that the adsorption of small AfB1 amounts reaches 60% at 25 mg of MND in the sample (1 mL); however, MND sorption capacity in this case is low. With an increase in the amounts of the mycotoxin, the sorption capacity of nanoparticles elevates by one order of magnitude. Analogously, an increase in the MND amount leads to an increase in the amount of the bound mycotoxin; however, the sorption capacity in this case decreases.
Figure 1.
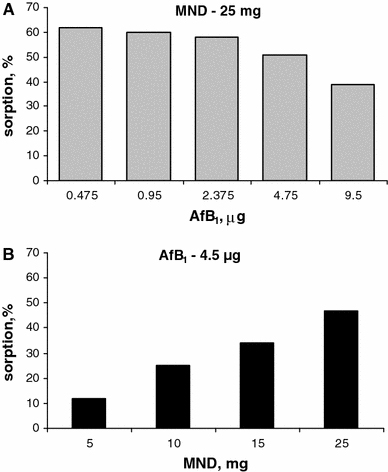
MND sorption characteristics depending on the AfB1 content in specimen at a constant amount of nanoparticles (a) and depending on the content of nanoparticles in specimen at a constant amount of AfB1 (volume 1 mL) (b)
It is well known that animal species exhibit different resistance to the toxic and carcinogenic effect of AfB1. That was the reason why we performed experiments on rats: they are more sensitive to AfB1 than, e.g., mice [16]. Each rat of Group 3 received 0.1 μg AfB1 per gram weight throughout the experiment. The same amount of AfB1 was administered orally with the MND hydrosol to each animal of Group 4. Spectral analysis showed that 81% of the mycotoxin contained in the MND hydrosol was adsorbed on nanoparticles, and 19% was free (Fig. 2).
Figure 2.
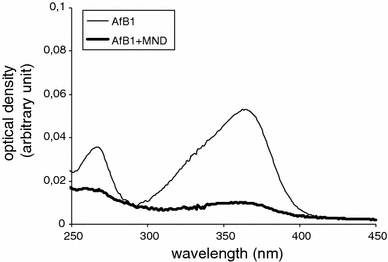
Spectral parameters of the aqueous solution of AfB1 and the supernatant resulting from mixing of the AfB1 aqueous solution and the MND hydrosol and subsequent centrifugation to remove nanoparticles with adsorbed mycotoxin
Analysis of blood samples taken from animals of different groups showed the following differences in hematological parameters (Fig. 3). The blood of rats of Group 2 contained considerably higher leukocyte levels than the blood of control animals (Group 1), probably due to a considerable increase in granulocytes. Previously, we made the assumption that the increase in the total level of white blood cells in mice that orally received MND could be a consequence of the interaction between nanoparticles and gastrointestinal macrophages [17]. The Group 3 rats had lower leukocyte levels, evidently due to a considerable (more than twofold) decrease in lymphocyte counts. This may be indicative of the deterioration of immune status in the rats of this group in response to the toxic effect of AfB1. The literature data suggest that different doses of AfB1 can either stimulate or suppress the immune system of the organism [18-20]. Group 4 animals, which had received AfB1 with the MND hydrosol, exhibited less pronounced dissimilarities in the total leukocyte level, including those in lymphocyte and granulocyte counts, from the respective parameters of Group 1 rats.
Figure 3.
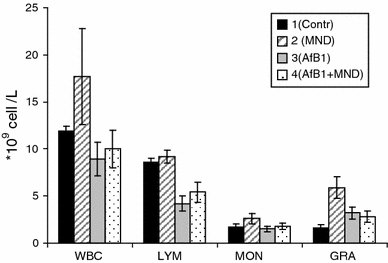
Leukocyte levels in the blood of rats that orally received water (control), the MND hydrosol, the AfB1 aqueous solution, and AfB1 with the MND hydrosol. Note: WBC leukocytes, LYM lymphocytes, MON monocytes, GRA granulocytes. Hematological parameters were determined at the end of experiment
No significant differences were found between erythrocyte counts of any of the treatment rats and the control group (Fig. 4a). Platelet counts were higher in the animals of Group 2 and 3 (Fig. 4b). However, the platelet counts in the blood of the Group 4 rats were similar to those of the Group 1 animals. In our opinion, these results may suggest mutual mitigation of the effects of MND and AfB1 (after the mycotoxin has adsorbed on nanoparticles) on white blood cells. The same explanation can be proposed for the registered differences in platelet counts between the treatment animals and the control group.
Figure 4.
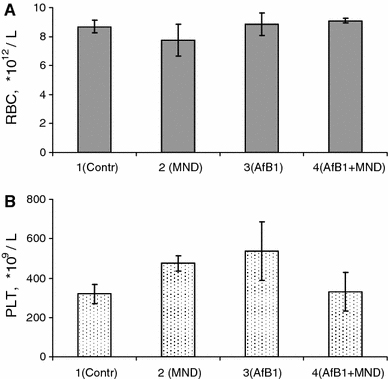
Red blood cells (a) and platelet counts (b) in the rats of the treatment groups and the control animals. Hematological parameters were determined at the end of experiment
The mutagenic and carcinogenic effects of AfB1 are related to the formation of its reactive exo-8,9-epoxide metabolite, which gets firmly bound with DNA. Bioactivation of AfB1 occurs in hepatocytes and are effected by the system of cytochrome P450, localized on membranes of the smooth EPR [1,21,22]. Analysis of ultrathin sections showed differences in the structure of liver cells between the rats of the treatment groups and the control animals (Fig. 5). Hepatocytes of the rats of Group 2 (Fig. 5b) were observed to contain elevated amounts of lysosomes and aggregates of lipid inclusions of low electron density. These changes in the hepatocyte ultrastructure could be a result of the compensatory response of the organism to the oral administration of MND. Electron microscopic analysis of hepatocytes of the Group 3 rats that had consumed AfB1 alone showed hyperplasia of smooth EPR, which could be indicative of its hyperfunction (Fig. 5c). Importantly, no similar changes were observed in the hepatocyte ultrastructure of the rats that had consumed AfB1 with the MND hydrosol (Fig. 5d). The registered lysosome aggregates in hepatocytes and the presence of electron-dense inclusions in bile capillaries can be indicative of active degradation of foreign compounds and their elimination from the cells. Excess accumulation of lipid inclusions in hepatocytes was also reported by author, who used intestinal adsorbents to treat various intoxications [23].
Figure 5.
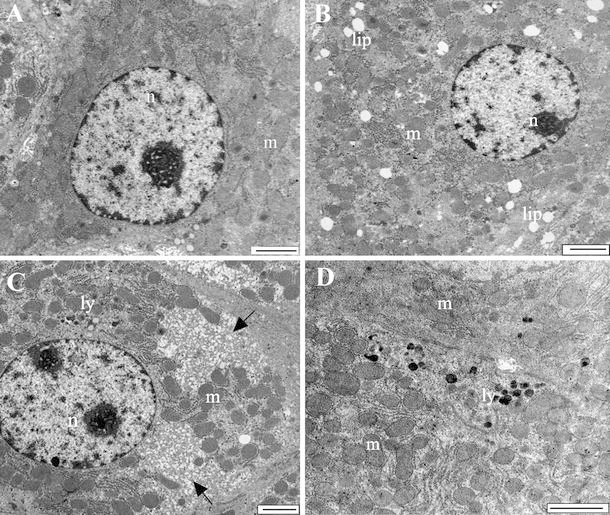
Ultrastructure of hepatocytes of animals: a Group 1 rats that orally received water, b Group 2 rats that orally received the MND hydrosol, c Group 3 rats that orally received the AfB1 aqueous solution, d Group 4 rats that orally received AfB1 with the MND hydrosol. Bar—2 μm. Arrows show hyperplasia of smooth endoplasmic reticulum in hepatocyte image. Note: n nucleus, m mitochondria, lip lipid inclusions, ly lysosomes
Conclusion
Thus, results of the examination of hematological parameters of blood and the state of the rats liver cells can suggest that oral administration of AfB1 together with the MND hydrosol produces a less toxic effect on animals than oral administration of AfB1 alone. After AfB1 has been adsorbed on MND, the effects of the mycotoxin and nanoparticles should be mutually mitigated. Our previous, in vitro, experiments proved that MND can adsorb AfB1 from aqueous solutions with subacid, acid, and alkaline pH, which are characteristic of different sections of the gastrointestinal system [11]. Another advantage of MND as intestinal adsorbent is the high rate of AfB1 adsorption (the process taking not more than 2–3 min) and very good biocompatibility of nanoparticles, proven by in vivo experiments with animals of various species [14]. Hence, MND can be proposed as intestinal adsorbent to bind and neutralize mycotoxins, AfB1 in particular.
Acknowledgments
The study was financially supported by the Russian Foundation for Basic Research (RFBR) (Grant No. 06-04-90234) and the RAS Presidium (Program No. 27, Project No. 64).
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- Gorelick NJ. Risk assessment for aflatoxin: I. Metabolism of aflatoxin B1 by different species. Risk Anal. 1990;10:539. doi: 10.1111/j.1539-6924.1990.tb00538.x. COI number [1:STN:280:DyaK3M7kt1GhtA%3D%3D] [DOI] [PubMed] [Google Scholar]
- Bennett JW, Klich M. Mycotoxins. Clin. 2003;16:497. doi: 10.1128/CMR.16.3.497-516.2003. COI number [1:CAS:528:DC%2BD3sXmsV2qtL4%3D] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy PA, Hendrich S, Landgren C, Bryant CM. Food mycotoxins: an update. J. 2006;71:R51. doi: 10.1111/j.1750-3841.2006.00052.x. COI number [1:CAS:528:DC%2BD28Xms1ajsr0%3D] [DOI] [Google Scholar]
- Richard JL. Some major mycotoxins and their mycotoxicoses—an overview. Int. 2007;119:3. doi: 10.1016/j.ijfoodmicro.2007.07.019. COI number [1:CAS:528:DC%2BD2sXht12gtbnM] [DOI] [PubMed] [Google Scholar]
- Castells M, Marin S, Sanchis V, Ramos AJ. Distribution of fumonisins and aflatoxins in corn fractions during industrial cornflake processing. Int. 2008;123:81. doi: 10.1016/j.ijfoodmicro.2007.12.001. COI number [1:CAS:528:DC%2BD1cXjtVChs7Y%3D] [DOI] [PubMed] [Google Scholar]
- Diaz DE, Hagler WM, Hopkins BA, Whitlow LW. Aflatoxin binders I: in vitro binding assay for aflatoxin B1 by several potential sequestering agents. Mycopathologia. 2002;156:223. doi: 10.1023/A:1023388321713. [DOI] [PubMed] [Google Scholar]
- Aly SE, Abdel-Galil MM, Abdel-Wahhab MA. Application of adsorbent agents technology in the removal of aflatoxin B1 and fumonisin B1 from malt extract. Food Chem. 2004;42:1825. doi: 10.1016/j.fct.2004.06.014. COI number [1:CAS:528:DC%2BD2cXntlGgtLk%3D] [DOI] [PubMed] [Google Scholar]
- Desheng Q, Fan L, Yanhu Y, Niya Z. Adsorption of aflatoxin B1 on montmorillonite. Poult. 2005;84:959. doi: 10.1093/ps/84.6.959. COI number [1:CAS:528:DC%2BD2MXlt1CiurY%3D] [DOI] [PubMed] [Google Scholar]
- Phillips TD, Afriyie-Gyawu E, Williams J, Huebner H, Ankrah NA, Ofori-Adjei D, Jolly P, Johnson N, Taylor J, Marroquin-Cardona A, Xu L, Tang L, Wang J-S. Reducing human exposure to aflatoxin through the use of clay: a review. Food. Addit. Contam. Part A. 2008;25:134. doi: 10.1080/02652030701567467. COI number [1:CAS:528:DC%2BD1cXitFKhs7s%3D] [DOI] [PubMed] [Google Scholar]
- Bondar VS, Puzyr AP. Nanodiamonds for biological investigations. Phys. Solid State. 2004;46:716. doi: 10.1134/1.1711457. COI number [1:CAS:528:DC%2BD2cXjtF2lurc%3D]; Bibcode number [2004PhSS...46..716B] [DOI] [Google Scholar]
- Puzyr AP, Purtov KV, Shenderova OA, Luo M, Brenner DW, Bondar VS. The adsorption of aflatoxin B1 by detonation-synthesis nanodiamonds. Dokl. 2007;417:299. doi: 10.1134/S1607672907060026. COI number [1:CAS:528:DC%2BD1cXlsVWn] [DOI] [PubMed] [Google Scholar]
- Purtov KV, Burakova LP, Puzyr AP, Bondar VS. The interaction of linear and ring forms of DNA molecules with nanodiamonds synthesized by detonation. Nanotechnology. 2008;19:1. doi: 10.1088/0957-4484/19/32/325101. [DOI] [PubMed] [Google Scholar]
- Gibson N, Shenderova O, Luo TJM, Moseenkov S, Bondar V, Puzyr A, Purtov K, Fitzgerald Z, Brenner DW. Colloidal stability of modified nanodiamond particles. Diam. 2009;18:620. doi: 10.1016/j.diamond.2008.10.049. COI number [1:CAS:528:DC%2BD1MXitFKnt7w%3D] [DOI] [Google Scholar]
- Puzyr AP, Baron AV, Purtov KV, Bortnikov EV, Skobelev NN, Mogilnaya OA, Bondar VS. Nanodiamonds with novel properties: a biological study. Diam. 2007;16:2124. doi: 10.1016/j.diamond.2007.07.025. COI number [1:CAS:528:DC%2BD2sXhtlGmt7fL] [DOI] [Google Scholar]
- Schrand AM, Huang H, Carlson C, Schlager JJ, Osawa E, Hussain SM, Dai L. Are diamond nanoparticles cytotoxic? J. Phys. Chem. B. 2007;111:2. doi: 10.1021/jp066387v. COI number [1:CAS:528:DC%2BD28XhtlSrsrrE] [DOI] [PubMed] [Google Scholar]
- Hengstler JG, Van Der Burg B, Steinberg P, Oesch F. Interspecies differences in cancer susceptibility and toxicity. Drug Metab. 1999;31:917. doi: 10.1081/DMR-100101946. COI number [1:CAS:528:DyaK1MXnvFCitrY%3D] [DOI] [PubMed] [Google Scholar]
- Puzyr AP, Bondar VS, Selimkhanova ZYu, Inzhevatkin EV, EV Bortnikov. Results of studies of application of detonation nanodiamonds as enterosorbents. Sib. Med. Rev. 2004;25:2–3. [Google Scholar]
- Reddy RV, Taylor MJ, Sharma RP. Studies of immune function of CD-1 mice exposed to aflatoxin B1. Toxicology. 1987;43:123. doi: 10.1016/0300-483X(87)90002-3. COI number [1:CAS:528:DyaL2sXhslSltb0%3D] [DOI] [PubMed] [Google Scholar]
- Raisuddin S, Singh KP, Zaidi SI, Saxena AK, Ray PK. Effects of aflatoxin on lymphoid cells of weanling rat. J. 1990;10:245. doi: 10.1002/jat.2550100404. COI number [1:CAS:528:DyaK3cXlt1Oru7c%3D] [DOI] [PubMed] [Google Scholar]
- Hinton DM, Myers MJ, Raybourne RA, Francke-Carroll S, Sotomayor RE, Shaddock J, Warbritton A, Chou MW. Immunotoxicity of aflatoxin B1 in rats: effects on lymphocytes and the inflammatory response in a chronic intermittent dosing study. Toxicol. 2003;73:362. doi: 10.1093/toxsci/kfg074. COI number [1:CAS:528:DC%2BD3sXktVCnsr8%3D] [DOI] [PubMed] [Google Scholar]
- Imaoka S, Ikemoto S, Shimada T, Funae Y. Mutagenic activation of aflatoxin B1 by pulmonary, renal, and hepatic cytochrome P450s from rats. Mutat. 1992;269:231. doi: 10.1016/0027-5107(92)90204-f. COI number [1:CAS:528:DyaK3sXit1Kr] [DOI] [PubMed] [Google Scholar]
- Guengerich FP. Cytochrome P450 and chemical toxicology. Chem. 2008;21:70. doi: 10.1021/tx700079z. COI number [1:CAS:528:DC%2BD2sXhtlynurbF] [DOI] [PubMed] [Google Scholar]
- Zhaksilikova AK. Ultrastructural changes of liver after cadmium intoxication and Tagan-sorbent correction. Bull. 2005;115:66. [Google Scholar]


