Abstract
Objective
Dynamic seated postural control is essential for individuals who perform their daily activities from a wheelchair. While seated reach distance is used as a proxy measure for postural control, it is unknown whether this is an accurate and reliable measure of the limits of stability in individuals with motor-incomplete spinal cord injury (MISCI).
Design
To determine whether kinematic measures of excursion are valid measures of postural control in individuals with MISCI, seated reach test (SRT; obtained from a wrist marker) and associated trunk excursion values (obtained from a C7 marker) were compared with center of pressure excursion (COPE). Data were obtained from individuals with MISCI and from non-disabled individuals for each of four directions. To assess the reliability of these measures in subjects with MISCI, these values were collected on two separate days.
Results
The SRT was correlated with the COPE in three directions of reaching (r≥0.71) with the exception being leftward reaching. Trunk excursion was correlated with COPE in all directions (r≥0.93). In ND individuals, both SRT (r≥0.56) and trunk excursion (r≥0.91) were correlated with COPE for all directions. In individuals with MISCI, there was significant intersession agreement for both reach distance (ICC≥0.78) and trunk excursion (ICC≥0.77) measured in all directions.
Conclusions
While both SRT and trunk excursion are reasonable reflections of COPE, measurement of postural control based on trunk excursion has advantages for individuals who may have difficulty maintaining arm position during reaching. Reach distance is highly reliable in individuals with MISCI in all directions of reaching.
Keywords: Functional reach, limits of stability, balance, postural control
Introduction
Dynamic postural control, the ability to maintain balance while moving, is essential for functional mobility.1 The margins of dynamic postural control, or the extremes to which an individual can reach and still maintain balance, defines his/her limits of stability (LOS). For individuals who use a wheelchair as their primary means of mobility, dynamic stability during seated reaching activities defines the workspace available to perform activities without using the arms for balance.
The seated reach test (SRT)2, a test of maximal reach distance, is a clinical measure of seated postural control. In individuals with motor-complete spinal cord injury (SCI), this test is a reliable measure in the forward-reaching direction.3 Maximal forward reach distance is correlated with scores on clinical tests of function in individuals with SCI4 and stroke.5 Despite its clinical usefulness, there are issues that may limit utility of the SRT as a measure of postural control in individuals with motor-incomplete SCI (MISCI).
First, notwithstanding the associations among the SRT and other clinical tests, the value of SRT assumes that it accurately reflects LOS. There may be important differences between postural control measured kinematically by the SRT and more definitive kinetic measures of LOS, such as center of pressure excursion (COPE). While in non-disabled (ND) elderly individuals, seated reaching distance in the forward, leftward, and rightward directions is correlated with COPE,6 these findings may not generalize to those with MISCI. For example, ND individuals use various strategies during standing reach, and the extent to which reach distance reflects dynamic balance varies with the strategy used.7 Many individuals with SCI use atypical movement patterns during reaching to compensate for motor impairment and trunk instability.8, 9 These compensatory strategies may alter the relationship between SRT and COPE.
Second, in addition to altered trunk control, impaired control of the upper extremities is likely to influence reaching distance after SCI. While SRT is typically measured via fingertip excursion, in those with tetraplegia the inability to fully extend the wrist and fingers is problematic, however this difficulty can be overcome by using a wrist marker. More problematic is that even in ND individuals scapular and accessory arm movements influence reaching distance, e.g., reach distance can be increased by shoulder protraction.10 This is an even greater challenge in individuals with impaired motor control. Differences between SCI and ND individuals have been identified in reach-related kinematics of hand and trunk movements.11 Therefore, the SRT may not accurately reflect postural control in those with impaired motor function.
Third, individuals who perform their activities of daily living from a wheelchair need dynamic balance control during reaching in all directions. In SCI individuals, various aspects of forward reaching have been reported, including test-retest reliability,3 muscle activation patterns,12 influence of seating,13 and relationships among reach, time since injury, level of injury, and functional performance measures.4 Forward reaching has also been investigated in individuals with stroke,5, 14 and ND individuals. 6, 15-17 However, for a measure to be a valid representation of postural control, it must accurately reflect COPE in all directions. Different mechanisms for maintaining dynamic postural control may be employed for different directions,18 some of which may result in a mismatch between reach distance and dynamic balance, as has been shown in ND subjects during standing reach tests.7 There is little information related to LOS in the lateral direction, and available information addresses only ND individuals.6, 18 Further, only a single study in ND individuals, has assessed postural control in backward leaning, finding no significant correlation between backward leaning distance and COPE.6
Our objective was to determine whether the SRT is a valid and reliable measure of seated postural control in individuals with MISCI. We operationally defined seated postural control as ability to maintain seated balance while reaching to LOS. As part of validity testing, we compared SCI data to data obtained from ND individuals. While prior studies of SRT have focused on forward reach, it is functionally important to maintain postural stability in all directions; therefore we tested all directions of reach. Recognizing that in individuals with impaired motor function reach may be affected by factors other than postural control, such as inability to maintain appropriate arm position, we compared kinematic LOS as measured from the wrist to that measured from the upper trunk. We compared maximal reach distance to COPE measures, with the latter being the definitive measure of LOS. To assess reliability, we tested whether reach measures were stable over time.
Materials and Methods
Subjects
Subjects with MISCI were recruited from the research subject volunteer database at The Miami Project to Cure Paralysis. Inclusion criteria were SCI of at least one year duration and injury level above T12. Exclusion criteria were current orthopedic problems or history of cardiac condition. The ten ND subjects had no known orthopedic or neurological deficits. The study was approved by the Human Subjects Research Office of the University of Miami Miller School of Medicine, and all subjects gave written consent to participate.
To test the hypothesis that SRT accurately measures LOS in MISCI individuals, reach distance and excursion of the upper trunk were compared to maximal COPE (see Kinetic Analysis and Kinematic Comparisons). Data from ten MISCI individuals (2 women, 8 men; 9 classified as American Spinal Injury Association (ASIA) Impairment Scale (AIS)19 C, 1 classified as AIS D; 6 tetraplegic, 4 paraplegic; ht:1.8±0.1m; age:46.7±5.8yrs; time since injury:4.3±3.4yrs), were compared to that from ten ND subjects (4 women, 6 men; ht:1.7±0.1m; age:41.4±13.6yrs). No attempt was made to match subjects as no evidence suggests that age or anthropometrics influences reliability/validity of reach. However the two groups were similar in terms of age and height.
A reliability study was conducted to confirm that reliable measures of reach distance could be obtained from MISCI individuals in each of four directions. Kinematic data were captured while seated subjects reached forward, leftward, and rightward, and leaned backward (see Kinematic Analysis). Thirty-two individuals (7 women, 25 men) with chronic MISCI (C3-T10; 25 classified as AIS C, 7 classified as AIS D; 23 tetraplegic, 9 paraplegic; ht:1.8 ± .01m; age:44.9 ± 11.2 yrs; time since injury:5.1 ± 6.0 yrs) participated.
Equipment
Kinematic data was acquired via an eight-camera Peak Performance (Centennial, CO) motion analysis system (60Hz capture rate) and video record was obtained with a digital video camera (JVC TK-31680). Kinetic data was obtained from a force platform (Kisler Instrument Corp., Amherst, NY) with a 0.64cm padded cover. The kinematic, video, and kinetic data were synchronized via TTL pulse.
Positioning
Subjects sat with hip, knee, and ankle joints each positioned at 90o, feet flat on the floor, and the popliteal fossa approximately two inches from the surface edge.3 The left arm was designated as the reaching arm for all directions except for the right reach test. Subjects were instructed to hold the reaching arm at shoulder height with the hand aimed in direction of reach, and to rest the opposite hand on their chest. The exception was backward reaching trials wherein subjects raised the arm to the front, and leaned back as far as possible. For right reach tests the hand positions were reversed. Start and end positions for the different reach directions is illustrated in Figure 1. The subjects were oriented such that the forward/backward reach directions were aligned along the y-axis, while left/right reach directions were aligned along the x-axis. Subjects were given the instruction “reach (or lean) as far as possible without losing your balance” following the cue “ready, set, go.” In some individuals, motor impairment limited ability to maintain the reaching arm at shoulder height, but they were encouraged to maintain this position to the extent possible. An assistant stood nearby to guard against falling. If balance was lost or the reaching hand contacted the table or assistant, the trial was repeated until five acceptable reaches were achieved for each direction. Subjects were allowed to rest as needed.
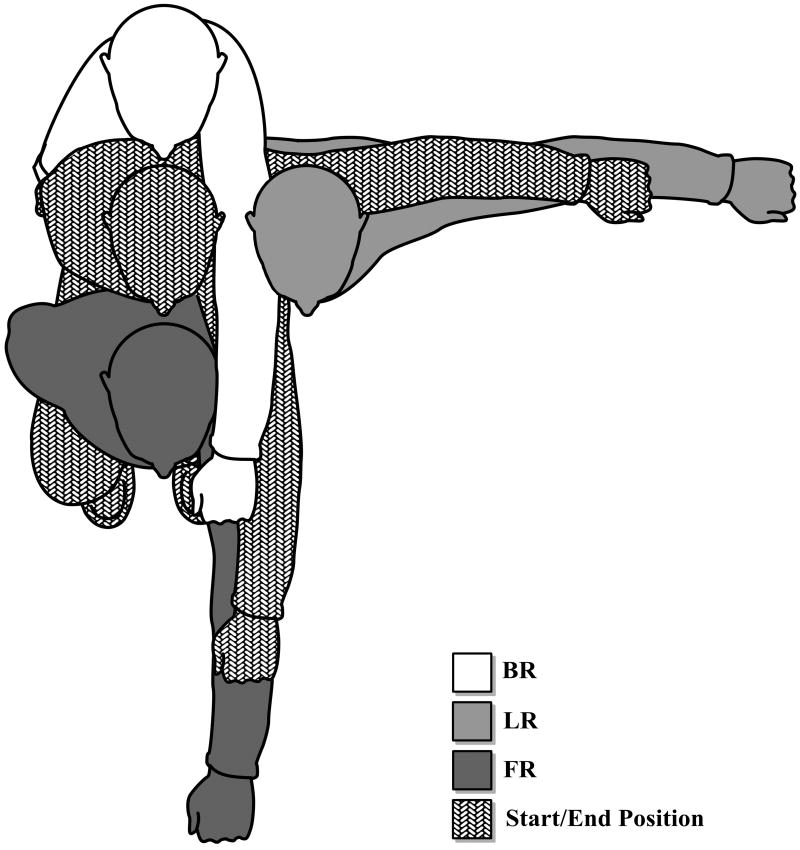
Figure 1.
Reach start and end positions. Illustration of start position (stippled gray figure) and maximum reach in the forward (dark gray), leftward (light gray) and backward (white) directions. Rightward reach was also tested but is not illustrated.
Kinematic Analysis
Markers were affixed at the trochanters, anterior superior iliac spines, sacrum, T10 spinous process, acromia, lateral humeral epicondyles, ulnar styloid process (wrist marker), and C7 spinous process (trunk marker). The SRT was measured from the wrist rather than the fingertips as many subjects with tetraplegia were unable to maintain their fingers in the extended position. Marker coordinates were filtered (Butterworth forth-order, 6Hz low-pass filter; Peak Motus®, Peak Performance, Centennial, CO) and the average of the three longest reach values obtained in five attempts was calculated. For assessment of test-retest reliability, subjects were retested within seven to ten days following initial test.
Kinetic Analysis and Kinematic Comparisons
Subjects sat on a height-adjustable table with an embedded force platform (Kistler Instrument Corp., Amherst, NY) with a 0.64cm padded cover. This standardized testing condition was used because chair configuration influences reaching distance in individuals with SCI.13, 17 Force data was collected at 600Hz and filtered (Butterworth, 4Hz low-pass filter; Peak Motus® software). The COPE (as measured by the excursion of the center of pressure in the direction of reach) was compared to concurrently acquired SRT (as measured by excursion of the wrist marker) and trunk excursion (as measured by excursion of the C7 marker) in the corresponding direction.
Statistical Analyses
To assess reproducibility of kinematic measures, intraclass correlation coefficients (ICC (3, 1); two-way, mixed-effects model) were calculated. The strength of the relationship between the SRT and COPE, and between the excursion of C7 and COPE were quantified with Pearson coefficients. Statistical analyses were performed using SPSS (Chicago, IL) with significance at α ≤0.05.
Results
Test-Retest Reliability of Reaching in MISCI individuals
Test-retest reliability of SRT in MISCI subjects was high for all directions of reach: FF (ICC=0.95; p < 0.001), LR (ICC=0.81; p < 0.001), RF (ICC=0.78; p < 0.001), and BF (ICC=0.83; p < 0.001). Test-retest reliability of trunk excursion in subjects with MISCI was also high for all directions: FF (ICC=0.93; p < 0.001), LF (ICC=0.77; p < 0.001), RF (ICC=0.89; p <0.001), and BF (r=0.81; p < 0.001)
Relationship between wrist and trunk excursion
There was a significant difference between excursion of the wrist marker (for the SRT) and C7 marker (trunk excursion) for the FF and BF directions (p< 0.001 for each), and trends toward differences in the LF and RF directions (p=0.073 and p=0.057, respectively).
Relationship between Kinematic and Kinetic Measures of LOS during Seated Reaching
There was a significant correlation between SRT and COPE in three of four reach directions in MISCI subjects, (FR: r=0.71, p=0.02; RR: r=0.72, p=0.02; BR: r=0.95, p=0.001), the exception being leftward reaching (LR: r=0.61, p=0.061). In comparison, for ND individuals correlation between SRT and COPE was significant in all four directions (FR: r=0.56, p=0.05; LR: r=0.77, p=0.004; RR: r=0.78, p=0.004; BR: r=0.88, p<0.001).
The relationship between trunk excursion and COPE was highly significant in all four directions both in MISCI subjects (FR: r = 0.99, p < 0.001; LR: r=0.93, p <0.001; RR: r = 0.98, p < 0.001; BR: r = 0.97, p <0.001) and ND individuals (FR: r=0.91, p<0.001; LR: r=0.98, p<0.001; RR: r=0.95, p<0.001; BR: r=0.94, p<0.001). Mean SRT, trunk excursion, and COPE are illustrated in Figure 2.
Figure 2.
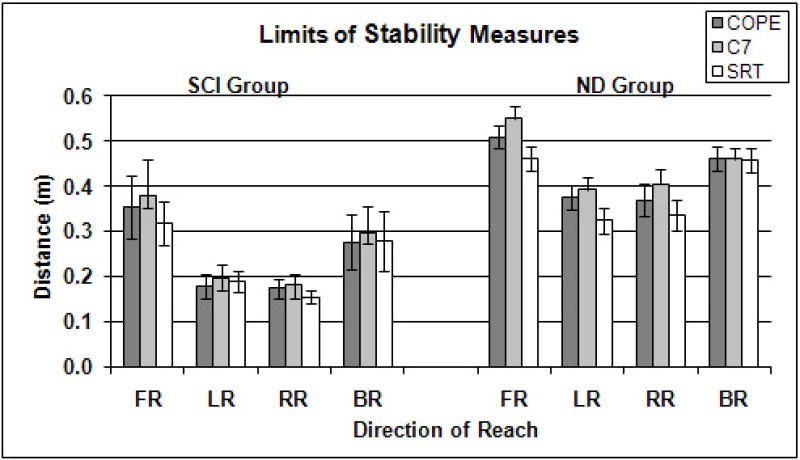
Comparison of limits of stability measures. Mean SRT, trunk excursion, and COPE (±SD) for individuals with SCI (n = 10) and ND individuals (n = 10). FR: forward reaching, LR: left reaching, RR: right reaching, BR: Backward reaching.
Discussion
Postural control during seated tasks is an early predictor of rehabilitation outcomes following stroke,20, 21 and is associated with improved functional task performance both in individuals with SCI4, 9 and stroke.5, 14, 21 The importance of dynamic sitting balance for function in wheelchair users underscores the need for valid and reliable measures of postural control. Our results indicate that the SRT provides a valid and reliable measure of postural control in MISCI individuals in most directions of reaching, with a possible exception being leftward reaching. These results are similar to prior reports for forward reaching in individuals with motor-complete SCI3 and stroke.5 However, kinematic measures of excursion as measured from trunk appear to be more accurate than those measured from the wrist.
In MISCI individuals and ND individuals, kinematic measures obtained from both the wrist (SRT) and the trunk (C7) during reaching are reasonable reflections of the more definitive kinetic measure of LOS, the COPE. A possible exception is the SRT in the leftward direction. In our sample of MISCI individuals, leftward reaching distance had the lowest correlation with the COPE, but the probability value (p=0.061) suggests a reasonable relationship. Most people are right-hand dominant, and it is likely that most MISCI individuals continue to perform the majority of activities with their right hands. Consequently, subjects would be more practiced in manipulating the right-side environment and reaching in rightward, and would therefore demonstrate comparatively less skill reaching leftward. This decreased movement toward the non-dominant side during seated reaching has been observed in ND individuals.6
In the clinical setting where equipment for capture/analysis of movement data is not typically available, our results demonstrate that the SRT represents a reasonable estimate of the LOS. However, there may be advantages to using measures related to trunk (C7) excursion versus the SRT. In both MISCI and ND subjects, levels of agreement between COPE and excursion of the trunk was greater than that between COPE and SRT. This may indicate that ancillary movements, such as difficulty maintaining full elbow extension, influence the SRT making it a less accurate reflection of LOS than measures obtained from the trunk. Therefore, for data acquired via motion capture system, measuring trunk excursion is a superior measure of LOS. Trunk excursion measured from C7 provides a distinctive anatomical landmark and minimizes influences from arm accessory movements that could over- or under-estimate postural control, especially in those with impaired motor control.
Limitations
All testing was completed with feet on the floor. As COPE measures were obtained from an instrumented seating surface and some pressure would have been distributed to the feet during forward reaching, the COPE measured in the forward direction may not represent the actual value of excursion of the COPE. However, this measure of COPE is proportional to the actual value. Our interest was in relationships among SRT, trunk excursion, and COPE, therefore we felt this approach was preferable to raising the seating platform such that the feet did not touch the floor (a condition which subjects found difficult and anxiety-provoking). We also felt that reaching with feet on the floor was a more typical condition, more directly representing reaching tasks performed in daily life.
Conclusions
Our results indicate that the SRT is a reasonably accurate reflection of LOS during reaching in both MISCI individuals and ND individuals. In MISCI individuals, SRT measures are stable over time. When motion capture equipment is available to record/analyze reach-related data, measurement obtained from the trunk may be preferable as these more precisely reflects COPE. However, both axial and upper extremity sites provide acceptable levels of fidelity to COPE, with the possible exception of leftward reaching in MISCI individuals. Further, our results demonstrate that SRT and trunk excursion provide satisfactory measures of postural control in all directions of reaching.
Acknowledgments
We are grateful for support from NIH grant HD41487, the Craig H. Nielsen Foundation, and The Miami Project to Cure Paralysis. We thank Stephen Lindley for technical contributions.
Reference List
- 1.Nichols DS. Balance retraining after stroke using force platform biofeedback. Phys Ther. 1997;77:553–558. doi: 10.1093/ptj/77.5.553. [DOI] [PubMed] [Google Scholar]
- 2.Duncan PW, Weiner DK, Chandler J, Studenski S. Functional Reach - A New Clinical Measure of Balance. Journals of Gerontology. 1990;45:M192–M197. doi: 10.1093/geronj/45.6.m192. [DOI] [PubMed] [Google Scholar]
- 3.Lynch SM, Leahy P, Barker SP. Reliability of measurements obtained with a modified functional reach test in subjects with spinal cord injury. Phys Ther. 1998;78:128–133. doi: 10.1093/ptj/78.2.128. [DOI] [PubMed] [Google Scholar]
- 4.Sprigle S, Maurer C, Holowka M. Development of valid and reliable measures of postural stability. J Spinal Cord Med. 2007;30:40–49. doi: 10.1080/10790268.2007.11753913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tyson SF, DeSouza LH. Reliability and validity of functional balance tests post stroke. Clin Rehabil. 2004;18:916–923. doi: 10.1191/0269215504cr821oa. [DOI] [PubMed] [Google Scholar]
- 6.Kerr HM, Eng JJ. Multidirectional measures of seated postural stability. Clin Biomech (Bristol, Avon) 2002;17:555–557. doi: 10.1016/s0268-0033(02)00068-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liao CF, Lin SI. Effects of different movement strategies on forward reach distance. Gait Posture. 2007 doi: 10.1016/j.gaitpost.2007.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Seelen HA, Potten YJ, Drukker J, Reulen JP, Pons C. Development of new muscle synergies in postural control in spinal cord injured subjects. J Electromyogr Kinesiol. 1998;8:23–34. doi: 10.1016/s1050-6411(97)00002-3. [DOI] [PubMed] [Google Scholar]
- 9.Chen CL, Yeung KT, Bih LI, Wang CH, Chen MI, Chien JC. The relationship between sitting stability and functional performance in patients with paraplegia. Arch Phys Med Rehabil. 2003;84:1276–1281. doi: 10.1016/s0003-9993(03)00200-4. [DOI] [PubMed] [Google Scholar]
- 10.Kaminski TR, Bock C, Gentile AM. The coordination between trunk and arm motion during pointing movements. Exp Brain Res. 1995;106:457–466. doi: 10.1007/BF00231068. [DOI] [PubMed] [Google Scholar]
- 11.Reft J, Hasan Z. Trajectories of target reaching arm movements in individuals with spinal cord injury: effect of external trunk support. Spinal Cord. 2002;40:186–191. doi: 10.1038/sj.sc.3101277. [DOI] [PubMed] [Google Scholar]
- 12.Potten YJ, Seelen HA, Drukker J, Reulen JP, Drost MR. Postural muscle responses in the spinal cord injured persons during forward reaching. Ergonomics. 1999;42:1200–1215. doi: 10.1080/001401399185081. [DOI] [PubMed] [Google Scholar]
- 13.Sprigle S, Wootten M, Sawacha Z, Thielman G. Relationships among cushion type, backrest height, seated posture, and reach of wheelchair users with spinal cord injury. J Spinal Cord Med. 2003;26:236–243. doi: 10.1080/10790268.2003.11753690. [DOI] [PubMed] [Google Scholar]
- 14.Dean CM, Shepherd RB. Task-related training improves performance of seated reaching tasks after stroke. A randomized controlled trial. Stroke. 1997;28:722–728. doi: 10.1161/01.str.28.4.722. [DOI] [PubMed] [Google Scholar]
- 15.Dean C, Shepherd R, Adams R. Sitting balance I: trunk-arm coordination and the contribution of the lower limbs during self-paced reaching in sitting. Gait Posture. 1999;10:135–146. doi: 10.1016/s0966-6362(99)00026-0. [DOI] [PubMed] [Google Scholar]
- 16.Dean CM, Shepherd RB, Adams RD. Sitting balance II: reach direction and thigh support affect the contribution of the lower limbs when reaching beyond arm's length in sitting. Gait Posture. 1999;10:147–153. doi: 10.1016/s0966-6362(99)00027-2. [DOI] [PubMed] [Google Scholar]
- 17.Janssen-Potten YJ, Seelen HA, Drukker J, Reulen JP. Chair configuration and balance control in persons with spinal cord injury. Arch Phys Med Rehabil. 2000;81:401–408. doi: 10.1053/mr.2000.3859. [DOI] [PubMed] [Google Scholar]
- 18.Parkinson MB, Chaffin DB, Reed MP. Center of pressure excursion capability in performance of seated lateral-reaching tasks. Clin Biomech (Bristol, Avon) 2006;21:26–32. doi: 10.1016/j.clinbiomech.2005.08.004. [DOI] [PubMed] [Google Scholar]
- 19.Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE, Haak M, Hudson LM, Priebe MM. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26(1):S50–S56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- 20.Franchignoni FP, Tesio L, Ricupero C, Martino MT. Trunk control test as an early predictor of stroke rehabilitation outcome. Stroke. 1997;28:1382–1385. doi: 10.1161/01.str.28.7.1382. [DOI] [PubMed] [Google Scholar]
- 21.Tyson SF, Hanley M, Chillala J, Selley AB, Tallis RC. The relationship between balance, disability, and recovery after stroke: predictive validity of the Brunel Balance Assessment. Neurorehabil Neural Repair. 2007;21:341–346. doi: 10.1177/1545968306296966. [DOI] [PubMed] [Google Scholar]