Abstract
Objective
America On the Move (AOM) is a national weight gain prevention initiative that promotes small lifestyle changes by increasing walking by 2000 steps/day and reducing energy intake by about 100 kcal/day. The study’s intent was to determine the impact of these small changes recommendations on steps/day and energy intake.
Methods
In this cross-sectional study, food and fluid intake and physical activity in 116 healthy overweight adults (BMI: 25–36 kg/m2; age: 18–60y) was compared between a non-intervention and an intervention week using diet diaries and pedometers. The major outcomes were steps/day, daily caloric intake, macronutrient intake and meal size. Within subject ANOVAs were conducted to compare results between intervention and non-intervention weeks.
Results
Total energy intake was lower during intervention week than non-intervention week (P < .01), including macronutrient contents (all P’s < .01), meal size (P < .01), consumption of sugar (P < .01), sugared sodas (P < .01) and sodium (P < .01). Steps/day were higher during intervention week than non-intervention week (P < .01).
Conclusions
The results support previous research showing that the message to increase steps/day results in an increase in physical activity. The results demonstrate for the first time that the message to reduce intake by 100 kcal/day does actually result in a lower intake in the short term. People seem to be able to make positive changes in diet and physical activity in response to these messages. If these small changes can be sustained, this approach could be effective in preventing further weight gain in the population.
Keywords: small-changes approach, weight gain, daily caloric intake, pedometers, America on the Move
INTRODUCTION
Most Americans today are overweight or obese and the gradual weight gain of the population that created the obesity epidemic continues [1]. It is estimated that 66% of adult Americans are overweight or obese [1], and as such have substantially increased morbidity and mortality from hypertension, stroke, coronary artery disease, dyslipidemia, type 2 diabetes, sleep apnea and a number of other conditions [2–6]. Higher body weight also increases all causes of mortality. Obesity is a chief contributor to preventable deaths in the United States and poses a major public health challenge [7,8].
There is no sign that the increase in obesity is abating. It is predicted that obesity rates will rise over the next few years in the U.S. and also in the rest of the world [9,10]. Immediate efforts are needed to address the gradual weight gain that is occurring globally.
Obesity, once present, is difficult to reverse [11]. This is due both to biological opposition to weight loss in the form of reductions in energy expenditure [12] and increases in appetite but also because the large behavior changes needed to sustain weight loss [13] are difficult for most people to sustain in an environment where food is abundant and where little physical activity is required in daily living [14]. Hill et al (2003) suggested that small behavior changes, which are likely to be more feasible to achieve and sustain, can be sufficient to prevent excess weight gain and stop the gradual population weight gain [10]. Previous research has estimated that affecting energy balance by approximately 100 calories per day through some combination of reductions in energy intake and increases in physical activity could prevent weight gain in most of the population [10]. Others have verified that the degree of positive energy balance that is causing weight gain in other populations is small [15]. Thus, small changes that reduce the small positive energy balance in the population should be more feasible to sustain over time and should be sufficient to prevent further weight gain.
AOM is a national initiative to promote the “small changes” approach. The program inspires people to make small lifestyle changes to prevent weight gain and improve health, starting with walking 2000 more steps/day over current levels and decreasing energy intake by 100 kcal/day. It has previously been shown that this approach can be used to increase physical activity [16] and to prevent weight gain [17,18].
The aim of this study was to evaluate the short-term effectiveness and usefulness of the America on the Move message. The AOM program provides tips for simple ways to decrease food intake by approximately 100 calories per day, many of which involve the substitution of healthier food choices for less healthy ones. Similarly, the AOM program provides tips for increasing walking. This study aimed to determine whether the AOM messages, along with tips for achieving the two small changes, would result in measurable changes in walking and in total energy intake in a group of overweight individuals over the short-term. If successful, the results would support the promotion of the small changes approach.
MATERIALS AND METHODS
Participants
Subjects for this cross-sectional study were 116 healthy overweight (BMI of 25–36 kg/m2) adults between the age of 18 and 60 years. The sample consisted of 15 males and 101 females. Recruitment was via emails send through the University of Colorado at Denver and Health Sciences Center (UCDHSC) server advertising the study as a research project to find ways to improve people’s dietary and physical activity behavior. As in most health and diet related studies, mostly middle-aged women were interested in participating compared to younger women and men. Interested individuals, both UCDHSC and non-UCDHSC employees, were sent a screening questionnaire and more details about the study via email. Interested, eligible, participants were asked to attend an informational meeting to determine further eligibility, sign consent and receive study instructions. The Colorado Institutional Review Board of the University of Colorado at Denver and Health Sciences Center reviewed and approved the research study including consent forms and measurement tools.
Outcome Measures
Upon consent, body weight and height were taken in order to calculate BMI. In addition, participants were asked to complete a questionnaire of demographic information and they were instructed on how to use a pedometer and a diet diary.
Steps/Day
Participants were asked to wear a pedometer (Accusplit AE120, San Jose, CA) for a total of three weeks. Pedometers have been shown to be accurate at capturing the number of steps taken [19] and they are recommended in the AOM program [20]. The average steps/day during the first week (7 days of recording) was considered to be the usual level of physical activity for participants. At least 4 days of step recording had to be available to be used in the data analysis. During the intervention week (2 weeks with the instruction to record steps for the second week) the participants were asked to increase walking by 500 steps per week above the level recorded in the non-intervention week, striving to increase their walking by 1000 steps in two weeks. While this was half the value than recommended in the AOM initiative, the length of this intervention was also only one-third of the original AOM program. The intent was to have a sufficient increase in order to assess the ability of the message to increase steps. Further, we have previously reported increases in walking in response to the AOM message of increasing walking by 2000 steps/day [16].
Energy Intake
A validated 7-day diet diary was used to assess the impact of the dietary message on food intake [21]. Participants were asked to record their food intake as detailed as possible including the type of food preparation (cooked, raw, fried), all ingredients together with condiments, product brands, food weight and volume as well as the eating location and time of consumption for seven days without changing anything in regards to their typical eating behavior. After the first seven day, non-intervention period, participants returned to the Center for Human Nutrition to be informed about the AOM program and to be asked to reduce their usual food intake by approximately 100 calories per day. To support this caloric reduction, participants were given 100 creative ways to reduce food intake by 100 calories with the instructions to use one of the options at least once per day.
The participants were asked again to fill out a 7-day diet diary during the last week of the 2 intervention weeks, and to indicate for which meals throughout the day they had used one of the 100 ways to reduce their daily intake. They were also instructed to indicate which of the provided options they had chosen throughout each day.
Data Analysis
Average daily steps of each participant during the AOM intervention week were compared to average daily steps during the one week non-intervention period with repeated measures ANOVAs. Within subject comparisons were used to compare dietary intake between the non-intervention and AOM intervention week. Differences in overall caloric intake, macronutrient contents and meal size (average calories per eating occasion) were analyzed using F-tests. Meals during the AOM week that indicated the use of one of the “100 ways to reduce caloric intake” option were compared with AOM meals without the “100 ways to reduce caloric intake” option. Frequency analyses were run to determine participants’ preferences of the “100 ways to reduce caloric intake” options.
Individual meals were identified from the diaries and the composition of the individual items composing the meals was determined. The raw diary entries were coded to calculate the nutrient composition of the ingested foods and fluids. Each food and fluid is assigned a code number. A continuously updated computer file which contains over 4000 food and fluid items that was created from the USDA Handbooks, food industry sources and published literature was used to analyze the coded data. Reported intakes containing at least 50 kilocalories (kcal) and separated in time from the preceding and following intake by at least 45 minutes were considered to be individual meals. The meals were described by their total caloric content, and by carbohydrate, fat, and protein content. The average composition of each of the meal characteristics and the mean average energy intakes were then calculated for each participant. Individual means were used to calculate the overall group means. For all analyses a significance level of 0.05 was chosen. For a detailed review of the diet-diary method, and the reliability and validity procedure see de Castro, 1994 and 1999 [21,22].
RESULTS
Of the 116 participants, 105 participants (15 male with mean age = 34.2 ± 10.7 years, 101 female with mean age = 41.2 ± 11.1 years) completed the non-intervention week providing steps/day and 7-day diet diary information. Male participants had a mean BMI of 29.6 ± 2.9 (height = 175.1 ± 7.1 cm and weight = 91.0 ± 11.3 kg for men) and female participants had a mean BMI of 29.5 ± 2.8 (height = 163.6 ± 6.3 cm and weight = 79.1 ± 9.6 for women). Ninety-eight of the participants completed both the non-intervention period and the AOM intervention weeks. However, 26 of the 98 participants were excluded from the diet-diary analyses due to suspected underreporting (with calculated energy intake being <10% above their estimated resting basal metabolic rate for the baseline week) [23–25]. However, the participants’ characteristics and the results did not differ when including the under reporters in the analysis. Table 1 shows participants’ characteristics divided by gender.
Table 1.
Participants’ Characteristics (Standard Deviation)
| Male (N = 15) | Female (N = 101) | |
|---|---|---|
| Age in years (SD) | 34.2 (10.7) | 41.2 (11.1) |
| Height in cm (SD) | 175.1 (7.1) | 163.6 (6.3) |
| Height in inches (SD) | 68.9 (2.8) | 64.4 (2.5) |
| Weight in kg (SD) | 91.0 (11.3) | 79.1 (9.6) |
| Weight in lbs (SD) | 200.6 (24.9) | 174.4 (21.2) |
| BMI (SD) | 29.6 (2.9) | 29.5 (2.8) |
The daily step average during the recorded AOM intervention week was significantly higher than during the non-intervention week (P <.01), with an average increase of 1,454 steps taken per day (Table 2).
Table 2.
Comparison of Daily Intake (Standard Error of the Mean) and Steps/day (Standard Error of the Mean) of Baseline Week and Intervention Week
| Daily Nutrient Intake | Baseline Week | AOM Week | ||
|---|---|---|---|---|
| Mean | SEM | Mean | SEM | |
| Total intake (kcal)* | 2273 | 50 | 1859 | 46 |
| CHO (kcal)* | 996 | 28 | 844 | 24 |
| Fat (kcal)* | 891 | 27 | 675 | 18 |
| Protein (kcal)* | 372 | 8 | 324 | 8 |
| Sugar (g)* | 111 | 5 | 92 | 4 |
| Daily Food Intake | ||||
| Sugared Sodas (g)* | 138 | 25 | 96 | 22 |
| Fruits (g) | 154 | 25 | 126 | 14 |
| Vegetables (g) | 153 | 12 | 133 | 10 |
| Daily Meal Size | ||||
| Average meal size (kcal)* | 589 | 20 | 490 | 13 |
| Meal CHO (kcal)* | 257 | 10 | 222 | 7 |
| Meal Fat (kcal)* | 232 | 9 | 178 | 6 |
| Meal Protein (kcal)* | 96 | 3 | 85 | 2 |
| Daily step average* | 6363 | 269 | 7755 | 284 |
P < .01.
Participants reported eating significantly less during the AOM intervention week in comparison to the non-intervention week (F(1,71) = 76.454; P < .01; see Table 2). Average daily intake of carbohydrates (F(1,71) = 37.193), fat (F(1,71) = 83.717), and protein (F1,71) = 38.842) was significantly lower during the AOM intervention week compared to the non-intervention week (P < .01). Average daily sugar (F(1,71 = 20.762) and sodium intake (F(1,71) = 11.588) was also significantly lower during the AOM intervention week than during the non-intervention week (P < .01). During the non-intervention week, more sugared sodas were consumed (F(1,71) = 8.582; P < .01) in comparison to the AOM intervention week. No differences in average fruit or vegetable intake could be found between weeks.
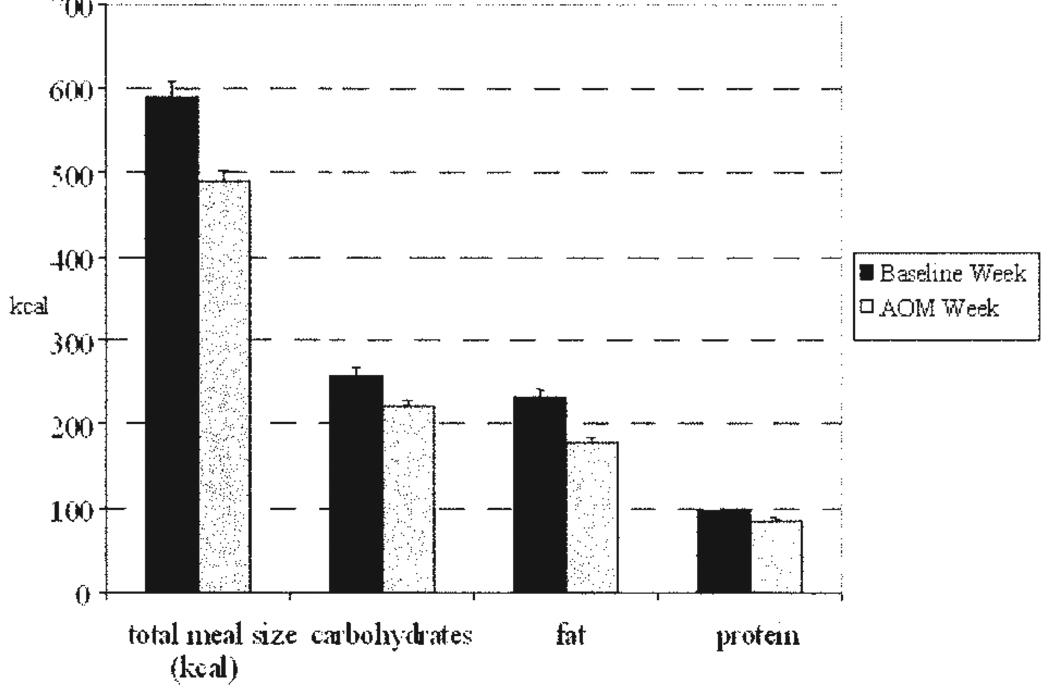
Average meal size was significantly lower during the AOM intervention week as compared to the non-intervention week (F (1,71 = 35.597; P < .01). Also, the macronutrient content in each meal differed significantly (see Fig. 1, all P <.01). In addition, during the AOM intervention week, meal sizes were significantly smaller when the “100 ways to reduce caloric intake” option was used than when it was not used. The average meals size was 489 calories (SEM = 24kcal) for meals indicated as having used the “100 ways to reduce caloric intake” option compared to a mean of 559 calories (SEM = 20kcal) for meals without using any reduction method (F(1, 50) = 5.711; P < .05). Both less fat (174 ± 9 kcal vs. 211 ± 10 kcal; p < .01) and protein (73 ± 3 kcal vs. 100 ± 4 kcal; p < .01) were consumed when having used the “100 ways to reduce caloric intake” option.
Fig. 1.
Average Daily Meal Size (SEM) of Baseline Week and AOM Week.
The most common methods of reducing energy intake were “leaving 3–4 bites on the plate”, “switching to skim milk”, “choosing fruits or vegetables over higher caloric snacks”, and “choosing diet soda over regular soda”.
DISCUSSION
Preventing weight gain in the population will require changing both diet and physical activity patterns. We have argued that this can best be done through small lifestyle changes that are more feasible to achieve and sustain than larger lifestyle changes [10]. We have demonstrated that a small changes message to increase physical activity by 2000 steps/day results in significant increases in daily walking [16].
This is the first demonstration that recommendations to reduce energy intake by about 100 calories per day along with tips and ideas for doing this results in significant reductions in total daily energy intake. Further, energy intake was reduced more at the meals where the tips were used than at meals where the tips were not used. When combined with the message to increase daily steps, this strategy should be effective in preventing weight gain. The daily increase of about 1454 steps equals approximately an additional caloric energy expenditure of about 70 calories per day. The mean daily intake during the intervention week was reduced by about 300 calories per day, suggesting that the small changes recommendations were feasible, easy to understand and to implement.
The participants were encouraged to reduce their caloric intake by about 100kcal/day; interestingly, it appears that the daily intake was reduced by an additional 200 calories. It is possible that the small changes message is more helpful and feasible than rigorous diet restrictions and therefore encourages participants to apply more than just one small-changes tip into their daily lifestyle which results in an even larger reduction of caloric intake than suggested.
During the intervention week, reductions were seen in each macronutrient and in sugar and sodium. Interestingly, less sugared soda was consumed during the intervention week, and this was one of the most popular options for reducing energy intake. Another popular message was just leaving 3–4 bites of food on the plate, perhaps because this option does not require the individual to completely give up favorite foods. It was interesting that although subjects reported often selecting the option of choosing fruits and vegetables over higher caloric snacks, the results indicate no differences in fruit and vegetable consumption between the two weeks. It is not clear if the participants failed to actually increase fruit and vegetable intake or whether the changes were too small to detect with our methods.
From the diet diaries, we can conclude that during the intervention week, participants were eating a diet similar to their usual diet with the exception that meal sizes were smaller. This, in turn, resulted in less total energy intake over the day. Meal frequency did not change in the intervention week, indicating that skipping meals was not used to reduce energy intake.
This study is to our knowledge, the first study that has attempted to measure small changes in total energy intake using diet diaries. Diet diaries have been widely used to investigate the nature of influences on food intake in free-living humans [26–28] and research suggests that three to seven days of recording is sufficient to obtain accurate information of the individuals’ overall daily intakes [29,30]. In the diet-diary method by de Castro [21,22], participants were asked to record in a pocket-sized diary their eating behavior, and the environmental context in which they eat and drink for seven consecutive days. There seems to be a good agreement between diary records and the actual amounts eaten [31–33] and comparisons of self-reports of intake and the actual food ingestion revealed agreements of about 87% between the diary records and the actual amounts eaten [33]. Using observers to write down the participants’ food intake and comparing it to the participants’ record showed truthful and valid records [34]. While underreporting of food intake does occur with the diet diary method, especially in overweight participants [35–41], it is expected to be consistent within groups and thus, analysis within groups comparing baseline with intervention weekly dietary intake seems appropriate [42–44]. In addition, in the present study, participants who reported intake that fulfilled an operational definition of suspected underreporting were eliminated from the analysis.
One limitation of this study is the convenience sample of both university and non-university employees which included mainly women and therefore cannot be generalized. As in most health and diet related studies, mostly middle-aged women were interested in participating compared to younger women and men. In addition, it was not possible to determine whether the participants altered their food intake due to the small changes program or due to other potential factors such as a close food monitoring or more extreme habit changes. A possible placebo effect might have taken place if the program only worked because the participants believed it would work for them. However, the eating behavior of the participants changed as hypothesized and it appears that this type of intervention could be a successful tool to reduce energy intake. Although this study was not sufficiently long to see effects on weight gain, we have shown that the small changes approach can significant reduce weight gain in overweight and at risk for overweight children over a period of 6 months [18]. These results add to the body of research supporting the small changes approach to modifying energy intake, energy expenditure and preventing excessive weight gain [10,16,17].
CONCLUSION
The primary intent of this study was to assess whether the small changes message to reduce energy intake by 100 kcal/day would produce a reduction in total energy intake in a group of overweight subjects in the short-term. One hundred calories is a very small reduction in energy intake and it was not clear that such a message would actually result in an overall reduction in energy intake. The results demonstrated that the small changes message was effective in significantly reducing total energy intake and also in increasing total steps/day. The reduction of total energy intake was even larger than expected. The behavioral changes seen in this study would be more than sufficient to prevent excessive weight gain if these behaviors could be maintained long-term. This suggests that the small changes strategy promoted by AOM could be useful in stopping the gradual weight gain in the population. Other community-based interventions also showed supportive results in terms of small diet- and physical activity related lifestyle changes as significant contributors to the maintenance of healthy body weights [45].
The AOM program promotes small changes to both physical activity and caloric intake. Making small changes to lifestyle behaviors appears to have potential for a healthier lifestyle in the long-term. People seem to be able to understand the simple messages and translate these into the desirable behavior changes. Weight management recommendations for patients might be more effective when the small changes approach is used instead of the suggestion to enroll in intensive temporary exercise and diet programs. Although it is likely to reduce body weight instantly, the small change approach appears to have a better chance to be maintained, especially in regards to the prevention of weight gain. The major challenge with changing diet and physical activity behaviors is to sustain the changes and although this will be a challenge with the small changes approach as well, it seems to be a more feasible approach. Future studies will be directed toward understanding factor that impact the sustainability and long-term effects of the small changes.
ACKNOWLEDGEMENTS
This study was partially funded by NIH Grant DK42549 Merit Award “Diet & Physical Activity Interactions in Obesity”.
REFERENCES
- 1.National Center for Health Statistics, Centers for Disease Control and Prevention. Prevalence of overweight and obesity among adults: United States, 2003–2004. [Accessed October 22, 2007]; Available at: http://www.ede.gov/nchs/products/pubs/pubd/hestats/overweight/overwght_adult_03.htm.
- 2.Eckel RH, Krauss RM AHA Nutrition Committee. American Heart Association call to action: Obesity as a major risk factor for coronary heart disease. Circulation. 1998;97:2099–2100. doi: 10.1161/01.cir.97.21.2099. [DOI] [PubMed] [Google Scholar]
- 3.Terry RB, Wood PD, Haskell WL, Stefanick ML, Krauss RM. Regional adiposity patterns in relation to lipids, lipoprotein cholesterol, and lipoprotein subfraction mass in men. J Clin Endocrinol Metab. 1989;68:191–199. doi: 10.1210/jcem-68-1-191. [DOI] [PubMed] [Google Scholar]
- 4.Overweight, obesity, and health risk. National Task Force on the Prevention and Treatment of Obesity. Arch Intern Med. 2000;160:898–904. doi: 10.1001/archinte.160.7.898. [DOI] [PubMed] [Google Scholar]
- 5.Strohl KP, Strobel RJ, Parisi RA. Obesity and pulmonary function. In: Bray GA, Bouchard C, James WP, editors. Handbook of Obesity. New York, NY: Mercel Dekker; 1998. pp. 725–735. [Google Scholar]
- 6.Hubert HB, Feinleib M, McNamara PM, Castelli WP. Obesity as an independent risk factor for cardiovascular disease: A 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67:968–977. doi: 10.1161/01.cir.67.5.968. [DOI] [PubMed] [Google Scholar]
- 7.O’Flaherty ME, Ford ES, Allendeer S, Scarborough P, Capewell S. Coronary heart disease trends in England and Wales from 1984 to 2004: concealed leveling of mortality rates among young adults. Heart. 2008;94:178–181. doi: 10.1136/hrt.2007.118323. [DOI] [PubMed] [Google Scholar]
- 8.Allison DB, Fontaine KR, Manson JE, Stevens J, Vanltallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–1538. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 9.IOTF, International Obesity Task Force. The Global Epidemic. [Accessed October 22, 2007]; Available at: http://www.iotf.org/globalepidemic.asp. [Google Scholar]
- 10.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: Where do we go from here? Science. 2003;299:853–855. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- 11.Nestle M, Jacobson MF. Halting the obesity epidemic. A public health policy approach. Public Health Rep. 2000;115:12–14. doi: 10.1093/phr/115.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med. 1995;332:621–628. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 13.Wing RR, Hill JO. Successful weight loss maintenance. Annu Rev Nutr. 2001;21:323–341. doi: 10.1146/annurev.nutr.21.1.323. [DOI] [PubMed] [Google Scholar]
- 14.Peters JC, Wyatt HR, Donahoo WT, Hill JO. From instinct to intellect: the challenge of maintaining healthy weight in the modern world. Obes Rev. 2002;3:69–74. doi: 10.1046/j.1467-789x.2002.00059.x. [DOI] [PubMed] [Google Scholar]
- 15.Brown WJ, Williams L, Ford JH, Ball K, Dobson AJ. Identifying the energy gap: magnitude and determinants of 5-year weight gain in midage women. Obes Res. 2005;13:1431–1441. doi: 10.1038/oby.2005.173. [DOI] [PubMed] [Google Scholar]
- 16.Wyatt HR, Peters JC, Reed GW, Grunwald GK, Barry M, Thompson H, Jones J, Hill JO. Using electronic step counters to increase lifestyle physical activity: Colorado on the Move. JPAH. 2004;1:181–191. [Google Scholar]
- 17.Rodearmel SJ, Wyatt HR, Barry MJ, Dong F, Pan D, Israel RG, et al. A family-based approach to preventing excessive weight gain. Obesity. 2006;14:1392–1401. doi: 10.1038/oby.2006.158. [DOI] [PubMed] [Google Scholar]
- 18.Rodearmel SJ, Wyatt HR, Stroebele N, Smith S, Ogden L, Hill JO. Small changes in dietary sugar and physical activity as an approach to preventing excessive weight gain: the America on the Move Family Study. Pediatrics. 2007;120:869–879. doi: 10.1542/peds.2006-2927. [DOI] [PubMed] [Google Scholar]
- 19.Tudor-Locke C, Myers AM. Challenges and opportunities for measuring physical activity in sedentary adults. Sports Med. 2001;31:91–100. doi: 10.2165/00007256-200131020-00002. [DOI] [PubMed] [Google Scholar]
- 20.America on the Move. [Accessed March 29, 2007]; Available from: http://www.americaonthemove.org. [Google Scholar]
- 21.De Castro JM. Measuring real-world eating behavior. Prog Obes Res. 1999;8:215–220. [Google Scholar]
- 22.De Castro JM. Methodology, correlational analysis, and interpretation of diet diary reports of the food and fluid intakes of free-living humans. Appetite. 1994;23:179–192. doi: 10.1006/appe.1994.1045. [DOI] [PubMed] [Google Scholar]
- 23.Schofield WN, Schofield C, James WPT. Basal metabolic rate - review and prediction, together with an annotated bibliography of source material. Hum Nutr Clin Nutr. 1985;39 Suppl 1:1–96. [PubMed] [Google Scholar]
- 24.Black AE, Goldberg GR, Jebb SA, Livingstone MB, Cole TJ, Prentice AM. Critical evaluation of energy intake data using fundamental principles of energy physiology: 2. Evaluating the results of published surveys. Br J Clin Nutr. 1991;45:583–599. [PubMed] [Google Scholar]
- 25.Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA, Prentice AM. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of Cut-off limits to identifying under-recording. Br J Clin Nutr. 1991;45:569–581. [PubMed] [Google Scholar]
- 26.De Castro JM. Socio-cultural determinants of meal size ad frequency. Br J Nutr. 1997;77 Suppl.1:39–55. doi: 10.1079/bjn19970103. [DOI] [PubMed] [Google Scholar]
- 27.De Castro JM. Measuring real-world eating behavior. Prog Obes Res. 1999;8:215–220. [Google Scholar]
- 28.De Castro JM, De Castro ES. Spontaneous meal patterns of humans: influence of the presence of other people. Am J Cl Nutr. 1989;50:237–247. doi: 10.1093/ajcn/50.2.237. [DOI] [PubMed] [Google Scholar]
- 29.Larkin FA, Metzner HL, Guire KE. Comparison of three consecutive- day and three random-day records of dietary intakes. JADA. 1991;91:1538–1542. [PubMed] [Google Scholar]
- 30.Tinker LF, Schneeman BO, Willis NH. Number of weeks of 24hour food records needed to estimate nutrient intake during a community-based clinical nutrition trial. JADA. 1993;93:332–334. doi: 10.1016/0002-8223(93)91564-7. [DOI] [PubMed] [Google Scholar]
- 31.Gersovitz M, Madden JP, Smicikalas-Wright H. Validity of the 24-hour dietary recall and seven-day record for group comparisons. JADA. 1978;73:48–55. [PubMed] [Google Scholar]
- 32.Krantzler NJ, Mullen BJ, Schutz HG, Grivetti LE, Holden CA, Meiselman HL. The validity of telephoned diet recalls and records for assessment of individual food intake. Am J Cl Nutr. 1982;36:1234–1242. doi: 10.1093/ajcn/36.6.1234. [DOI] [PubMed] [Google Scholar]
- 33.De Castro JM. Methodology, correlational analysis, and interpretation of diet diary reports of the food and fluid intakes of free-living humans. Appetite. 1994;23:179–192. doi: 10.1006/appe.1994.1045. [DOI] [PubMed] [Google Scholar]
- 34.Braam LA, Ocke MC, Bueno-de-Mesquita HB, Seidell JC. Determinants of obesity-related underreporting of energy intake. Am J Epidemiol. 1998;147:1081–1086. doi: 10.1093/oxfordjournals.aje.a009402. [DOI] [PubMed] [Google Scholar]
- 35.Heitmann BL, Lissner L. Dietary underreporting by obese individuals--is it specific or non-specific? BMJ. 1995;311:986–989. doi: 10.1136/bmj.311.7011.986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Price GM, Paul AA, Cole TJ, Wadsworth ME. Characteristics of the low-energy reporters in a longitudinal national dietary survey. Br J Nutr. 1997;77:833–851. doi: 10.1079/bjn19970083. [DOI] [PubMed] [Google Scholar]
- 37.Samaras K, Kelly PJ, Campbell LV. Dietary underreporting is prevalent in middle-aged British women and is not related to adiposity (percentage body fat) Int J Obes Relat Metab Disord. 1999;23:881–888. doi: 10.1038/sj.ijo.0800967. [DOI] [PubMed] [Google Scholar]
- 38.Voss S, Kroke A, Klipstein-Grobusch K, Boeing H. Is macronutrient composition of dietary intake data affected by underreporting? Results from the EPIC-Potsdam Study. European Prospective Investigation into Cancer and Nutrition. Eur J Clin Nutr. 1998;52:119–126. doi: 10.1038/sj.ejcn.1600525. [DOI] [PubMed] [Google Scholar]
- 39.Warwick PM, Reid J. Trends in energy and macronutrient intakes, body weight and physical activity in female university students (1988–2003), and effects of excluding under-reporters. Br J Nutr. 2004;92:679–688. doi: 10.1079/bjn20041247. [DOI] [PubMed] [Google Scholar]
- 40.Trabulsi J, Schoeller DA. Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endocrinol Metab. 2001;281:E891–E899. doi: 10.1152/ajpendo.2001.281.5.E891. [DOI] [PubMed] [Google Scholar]
- 41.Merz W, Tsui JC, Judd JT, Reiser S, Hallfrisch J, Morris ER, Steele PD, Lashley E. What are people really eating? The relation between energy intake derived from estimated diet records and intake determined to maintain body weight. Am J Clin Nutr. 1991;54:291–296. doi: 10.1093/ajcn/54.2.291. [DOI] [PubMed] [Google Scholar]
- 42.Lissner L, Habicht J-P, Strupp BJ, Levitsky DA, Haas JD, Roe DA. Body composition and energy intake: do overweight women overeat and underreport? Am J Clin Nutr. 1989;49:320–325. doi: 10.1093/ajcn/49.2.320. [DOI] [PubMed] [Google Scholar]
- 43.de Castro JM. Varying levels of food energy self-reporting are associated with between group but not within subjects differences in food intake. J Nutr. 2006;136:1382–1388. doi: 10.1093/jn/136.5.1382. [DOI] [PubMed] [Google Scholar]
- 44.Liebman M. Promoting healthy weight: Lessons learned from WIN the Rockies and other key studies. J Nutr Educ Behav. 2005;37:S95–S100. doi: 10.1016/s1499-4046(06)60206-6. [DOI] [PubMed] [Google Scholar]
- 45.Hill JO, Thompson H, Wyatt H. Weight Maintenance: What’s missing? J Am Diet Assoc. 2005;105:S63–S66. doi: 10.1016/j.jada.2005.02.016. [DOI] [PubMed] [Google Scholar]