Abstract
Background: Persons with psychotic illnesses have an increased risk for suicide, especially early in the illness. Sufficient knowledge allowing for early recognition is lacking. Objectives: To describe suicide behaviors before and during the 4 years following first psychiatric hospitalization, examine associations of demographic and psychiatric risk factors, and develop a suicide risk index. Method: Data came from the Suffolk County Mental Health Project, a first-admission cohort (n = 529). Cox regression was used to study associations of risk factors to suicide behaviors; a summary suicide behavior risk index was also tested. Results: Prior to first admission, 28.0% (n = 148) of the cohort had attempted suicide. During the 4-year follow-up, 13.6% (n = 72) of the cohort attempted suicide (29.7% of those with previous attempts and 7.3% making their first attempt) and 3 respondents died of suicide. The significant predictors at index admission of subsequent attempts were prior attempts or ideation, severity of depressive symptoms and thought disorder, lifetime substance abuse, and younger age. Suicide ideation was predicted by the same variables with the addition of insight into illness and with the exception of age at admission. A 3-category risk index was created; 61.1% of those who made a suicide attempt were in the highest risk group (n = 44/72). Conclusion: The current study confirms and extends previous research showing that risk factors early in the course of illness are predictive of subsequent ideation and attempts. The risk index may be a useful adjunct in identifying individuals likely to benefit from preventive interventions.
Keywords: early episode, suicide risk index, suicide ideation, suicide attempt
Suicide behaviors are significantly more prevalent among persons with psychosis than in the general population.1–3 The rate of completed suicide ranges from 5%–13% among persons with schizophrenia and other psychoses,4–8 compared with 1.14 per 10 000 in the general population.9 Patients with schizophrenia under age 28 y have an even higher risk than patients with schizophrenia older than age 28 years.4,8,10–12 One hypothesis for the elevated rate in patients younger than 28 years is their higher rate of substance abuse, a known risk factor for suicide.13–16
The prevalence of suicide attempts ranges between 25% and 50% in psychiatric populations,8,17 compared with 2%–5% in the general population.18 The risk factors for suicide attempts among persons with a psychotic illness are being white, having a higher IQ,8,10,15,19 having greater insight into illness,14,20 having a history of previous attempts,15,19,21,22 and being in an early stage of illness.11,23–25 The risk is elevated during the period shortly after first admission.4,11,26–28 In schizophrenia, males are at greater risk for attempts than females.8,19,29 In nonpsychotic samples, in contrast, women are at increased risk of attempt but males have a higher rate of completed suicides,30 particularly men from upper socioeconomic status (SES) households.31,32
Depression is also associated with suicide behaviors. Although it is not the most salient risk factor for suicide in this population,11,15,33–35 the association of mood symptoms is sometimes stronger than the relationships of positive and negative symptoms.17,36
The National Comorbidity Survey18 was the first study to investigate the conditional risk of attempts in persons with suicide ideation in the general population, finding that 57.9% of ideators with a plan and 25.2% without a plan made a subsequent attempt. Although considerable research in nonpsychotic patients has tried to develop suicide prediction models to improve clinical judgments, these studies have been limited by focusing on a restricted set of predictors,13,37 narrowly defined samples (eg, persons with past suicide behaviors), and retrospective reports.38
In a preliminary analysis of suicide behaviors in the first 184 respondents comprising the Suffolk County Mental Health Project (SCMHP),28 we found that 23.0% made a suicide attempt before their first admission and 15% (65% of attempters) made an attempt during the episode for which they were hospitalized. However, none of the demographic or clinical risk factors differentiated attempters from nonattempters. The current study extends the focus by examining the rate of suicide ideation and attempts in the full cohort during the 4-year period following admission and evaluating a more comprehensive set of clinical and demographic risk factors. A second purpose was to develop a clinically useful risk index to predict suicide behavior during the first 4 years after the first psychiatric admission.
Materials and Methods
Sample and Procedures
The SCMHP is described in detail elsewhere.39 Briefly, first-admission patients aged 15–60 years who were residents of Suffolk County, NY (population 1.3 million) and who presented with psychotic symptoms were recruited by the chief nurse, social worker, or project staff from 12 inpatient facilities between September 1989 and December 1995 (baseline response rate = 72%). The procedures for obtaining written informed consent were approved annually by the Committees on Research Involving Human Subjects at Stony Brook University and by Institutional Review Boards of the hospitals where respondents were recruited. Written informed consent to all study procedures was obtained from respondents and from parents of respondents under the age of 18 years.
Signed releases for hospital and clinical records were obtained at each face-to-face follow-up assessment although this was not a requirement for participation. Initial interviews occurred primarily in the hospital. Follow-up interviews took place in participants’ homes at 6-, 24-, and 48-month follow-up. The original cohort included 628 hospitalized respondents interviewed initially from 1989–1995 and found to be diagnostically eligible. Data on suicide behaviors in at least one of the 3 follow-up waves were available for 529 respondents.
Measures
Suicide Behaviors
Lifetime and current suicide ideation and attempts was gleaned from multiple sources, including the depression module of the Schedule for Clinical Diagnosis (SCID) DSM-III-R,40 supplemented by ratings of ideation or attempts. Specifically, respondents who reported suicide ideation were asked whether they ever tried to kill themselves or did anything that could have killed them, and if so whether an attempt was made in the past 12 months. Other sources of information used to classify ideation and attempts included the suicide item in the Hamilton Depression Rating Scale (Ham-D)41 and the reason for admission recorded in the medical record. By combining self-report, rating scale data, and reason for hospitalization, we were able to improve the reliability of our determination of suicide behavior.
Suicide ideation and attempts during the follow-up period were obtained during the 6-, 24-, or 48-month interviews. The data were only available for respondents who had full interviews at these time points. Similar to Borges et al,38 persons with suicide attempts were regarded as having had ideation even if this information was missing.42 Consequently, we were able to examine the probability of having subsequent ideation and attempts in the full analysis sample. Mortality was monitored annually using the National Death Index.
Risk Factors
Demographic and clinical risk factors assessed at baseline included sex, age at admission, and duration of untreated psychosis (DUP). Age at admission and duration between onset of psychosis and initial hospitalization were divided into categories to minimize the effects of extreme values. Categories were collapsed to stabilize associations when odds ratios did not differ meaningfully. As a result, for age at admission, we used a median split to provide 2 equal categories (<28 vs 28+). For the duration of time from onset of psychosis to first hospitalization (DUP), we used 6 months because it is a marker of future chronicity. DUP was determined from SCID information about time of onset of first psychotic symptom.43 Other demographic risk factors included race that was dichotomized into “white” vs “other” (black, Hispanic, Asian, Native American), living status dichotomized into lives “alone” vs “other” (with parents, spouse, other relatives, or friends), social class of household of origin dichotomized into “upper/middle” (5 or better on the Hollingshead Occupational Scale) and “lower” groups based on the parent with the highest household-level occupation.44 Other clinical risk factors included Diagnostic and Statistical Manual of Mental Disorders (Third Edition Revised) lifetime substance abuse/dependence determined by the SCID, hospital admission status (voluntary vs involuntary), duration between onset of psychosis and hospital admission determined from SCID information about time of onset of first psychotic symptom, (see below), insight into psychotic illness, low intellectual functioning, and diagnosis. Low intellectual functioning was defined as full-scale IQ < 85 based on school record information on neuropsychological test results, or if test data were not available, it was estimated based on the presence of 2 of the following: low Quick test score45 at baseline or 6-month follow-up, participating in a special education program, school dropout or graduated from a nonacademic track, unable to add/subtract, or unable to hold a job for reasons other than mental illness.46
Core schizophrenia symptoms were assessed using the Scale for the Assessment of Positive Symptoms (SAPS) and the Scale for the Assessment of Negative Symptoms (SANS) reflecting the 4-week period preceding the interview.47,48 The SAPS items were factor analyzed,49 and 2 factors emerged: psychotic (hallucinations and delusions) and disorganized (bizarre behavior and formal thought disorder) symptom dimensions. The factor analysis of the SANS yielded a single negative dimension, and one symptom score was created (mean of all items). Depressive symptom severity (past month) at baseline was measured with the Ham-D,41 dichotomized into “mild” (0–18) vs “severe” (19–60) depression scores.50 Insight was measured with the insight item of the HAM-D; this item had been modified for the study to refer to level of insight into psychotic illness rather than depression51 and was dichotomized into “acknowledges psychotic illness” vs “denies psychotic illness.”
Diagnosis
A team of psychiatrists formulated the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition) study diagnosis at consensus conferences held after the 6- and 24-month assessment using all available sources of information.45 The 24-month diagnosis was used to define the diagnostic groups; the 6-month diagnosis was used when the 24-month variable was missing. This article focuses on 208 respondents with schizophrenia (n = 171), schizoaffective disorder (n = 30), or schizophreniform disorder (n = 7) and 321 with other psychoses, including bipolar disorder with psychotic features (n = 131), major depression with psychotic features (n = 93), other psychotic illnesses (n = 50), and other (mostly drug-induced) disorders (n = 47). For the analysis, participants were dichotomized into “schizophrenia” (n = 208, 39.3%) and “other psychosis” (n = 321, 60.7%) categories.
Statistical Analysis
Comparison of those with (n = 529) and without (n = 99) follow-up suicide information found that those with information in at least one follow-up time interval were significantly younger (P < .001). No significant differences were found with respect to sex, voluntary vs involuntary admission, SES, living alone vs other, race, diagnosis, intelligence, lifetime substance abuse, severity of depressive symptoms, insight into illness, duration of symptoms, positive or negative symptom severity, or lifetime suicide ideation or attempts, the variables of interest for this report, suggesting that attrition had minimal impact on the results. We note that at 6 months, data were available for 468 respondents; at 24 months, data were available for 421 respondents; and at 48 months, data were available for 357 respondents. For budgetary reasons, many of the 48-month assessments were done by telephone and thus had to be abbreviated.
Two sets of Cox regression analyses were conducted. The first predicted suicide ideation during the 48-month follow-up after baseline, and the second predicted suicide attempts during the same time period. Variables included as risk factors in the Cox regression models were assessed at baseline. Each risk factor was first examined at the univariable level, and the subsequent significant predictors were included in multivariable Cox regression models. A separate analysis of respondents who entered the study with no history of attempts was also conducted.
All analyses were conducted for the entire sample, adjusting for diagnosis (schizophrenia vs other). We also conducted separate analyses for each diagnostic group because in preliminary analysis for this article we found that they differed on several variables included in this article. Specifically, the schizophrenia group had more males (66.3% vs 54.8%, P < .01), low SES households (37.0% vs 27.4%, P < .05), low intellectual capacity (19.2% vs 10.1%; P < .01), and psychosis for more than 6 months before hospitalization (48.3% vs 20.1%, P < .001). Fewer had a lifetime history of substance abuse (45.7% vs 56.4%, P < .05) and insight into their illness (71.0% vs 84.4%, P < .001). More were younger (mean = 27.38 ± SD = 8.23 vs 30.33 ± SD = 9.99, P < .01) and presented with higher scores on both positive (psychotic) symptoms (mean = 13.8 ± SD = 10.67 vs mean = 9.66 ± SD = 8.17, P < .01) and negative symptoms (mean = 23.7 ± SD = 13.75 vs mean = 13.41 ± SD = 11.73, P < .01). Most importantly for this report, respondents with schizophrenia were less likely to report a history of suicide ideation at baseline (43.8% vs 55.8%, P < .01).
To summarize the findings, a risk index, modeled after Borges et al,38 was constructed from the variables that were significant in the Cox regression models. Index building started by identifying the group with the greatest risk (ie, highest probability of future suicide behavior) and terminated by identifying the group with the lowest risk. Because previous suicide behavior is generally the most salient predictor of future suicide behavior, we first examined whether the presence of any additional risk factors alone and then in combination would be associated with an even greater risk among those with previous suicide behavior. The risk index was constructed by computing a series of contingency tables and attendant risk statistics. Moving down the risk scale, a similar procedure was followed among those without previous suicide behavior to first identify what combinations of risk factors were associated with greatest risk. Finally, the probability of suicide behavior among those persons with no other risk factors was computed.
Results
Rates
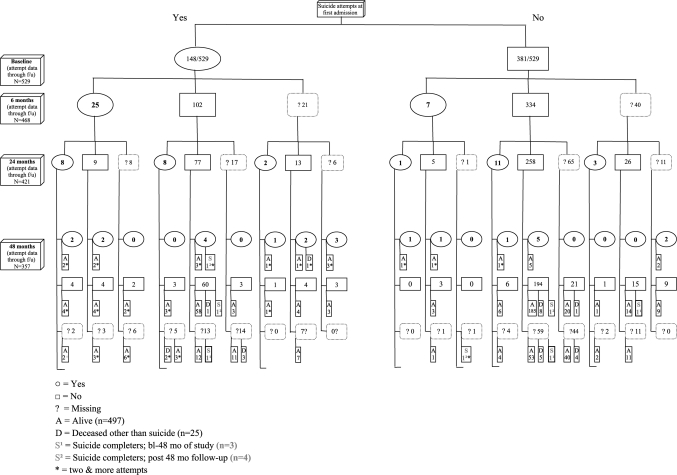
At baseline, the lifetime rate of suicide ideation was 51.0% (n = 270/529), of whom 76.3% (206/270) had ideation at the time of admission (38.9% of the sample) and 27.8% (n = 116/270) had suicide ideation during the 48-month follow-up. Among the 259 respondents with no history of ideation, 12.0% (n = 31/259) had subsequent ideation. The lifetime rate of suicide attempts was 28.0% (n = 148/529), among whom 33.1% (49/148) made an attempt at the time of their admission (9.3% of the sample). As shown in figure 1, among the 148 respondents with a lifetime history of suicide attempts, 29.7% (n = 44/148) made a subsequent attempt that was fatal in 1 case; among the 381 respondents without a lifetime suicide attempt history at baseline, 7.3% (n = 28/381) made a first attempt during the 4-year follow-up period that was fatal in 2 cases. The rate of suicide attempts during the follow-up among baseline respondents without a history of ideation was 3.5% (n = 9/259).
Fig. 1.
Distribution of Suicide Attempts Throughout the Study.
Characteristics of Suicide Deaths
The 3 respondents who committed suicide before the 48-month point were white, male, were diagnosed with schizophrenia, were from upper/middle class households, had IQ within normal limits, did not live alone at admission, and were admitted for reasons other than suicide behavior. One respondent was 24 years old at time of death. He had no history of substance abuse scored in the mild range on the Ham-D Scale at baseline (11), manifested insight into his illness, had signs of thought disorder (SAPS disorganized dimension was 19, putting him above the median value for cohort), and had no previous reports of ideation or attempts. He committed suicide by gunshot to the head.
The second respondent was 28 at time of first hospitalization. At baseline, he had a history of substance abuse, scored in the mild range on the Hamilton Scale (15), had poor insight into his illness, had signs of thought disorder on the SAPS (score of 15 on the disorganized dimension), and had a lifetime history of ideation and attempts. He committed suicide by jumping in front of a train.
The third respondent was 24 at time of first hospitalization. At baseline, he had a history of substance abuse, scored in the mild range on the Hamilton Scale (11), showed poor insight into his illness, had considerable negative symptoms (SANS = 45) and thought disorder, and had no history of attempts or ideation. He committed suicide by gunshot.
Risk Factors for Suicide Ideation
As shown in table 1, the following variables assessed at time of first hospital admission were significant predictors of subsequent suicide ideation (in descending order): history of suicide attempts (hazard ratio [HR] = 3.96, confidence interval [CI] = 2.66–5.89, P < .001), history of suicide ideation (HR = 3.27, CI = 2.36–4.53, P < .001), severity of depression on the Ham-D (HR = 2.18, CI = 1.57–3.04, P < .001), history of substance abuse (HR = 1.49, CI = 1.07–2.08, P < .05), insight into illness (HR = 1.62, CI = 1.03–2.56, P < .05), and greater thought disorder (SAPS, disorganization dimension, HR = 1.03, CI = 1.00–1.06, P < .05). The following variables in descending order were not significant risk factors: duration of time between onset of psychosis and hospitalization, diagnosis, living alone, involuntary admission, younger than age 28 years at admission, high SES, race, SAPS psychoticism dimension, negative symptom severity, intellectual capacity, and sex.
Table 1.
Predictors of Suicide Ideation and Attempts Over the 48-mo Period After First Hospitalization: Cox Regression Analysis
| Suicide Ideation |
Suicide Attempts |
|||||||||||
| Variables at Time of Admission | Univariable Model (n = 529) |
Multivariable Modela (n = 505/529)b |
Univariable Model (n = 529) |
Multivariable Modelc (n = 505/529)d |
||||||||
| HR | 95% CI | P Value | HR | 95% CI | P Value | HR | 95% CI | P Value | HR | 95% CI | P Value | |
| Age at admission < 28 y: younger (n = 286)/older (n = 243) | 1.00 | 0.99–1.02 | .30 | 1.03 | 1.00–1.05 | .03* | 1.03 | 1.00–1.06 | .04* | |||
| Sex: male (n = 314)/female (n = 215) | 1.04 | 0.75–1.45 | .78 | 1.14 | 0.72–1.83 | .55 | 1.34 | 0.82–2.18 | .23 | |||
| Admissione: voluntary (n = 194)/involuntary (n = 277) | 1.19 | 0.85–1.68 | .29 | 1.33 | 0.82–2.14 | .24 | ||||||
| Living status: alone (n = 69)/other (n = 460) | 1.27 | 0.81–1.92 | .28 | 1.04 | 0.53–2.04 | .89 | ||||||
| Socioeconomic statusf: upper-middle (n = 72)/lower (n = 454) | 1.18 | 0.82–1.69 | .36 | 1.21 | 0.72–2.03 | .45 | ||||||
| Race: white (n = 394)/other (n = 135) | 1.19 | 0.81–1.76 | .36 | 1.11 | 0.64–1.91 | .70 | ||||||
| Diagnosis: schizophrenia (n = 208)/other (n = 321) | 1.26 | 0.90–1.77 | .17 | 1.17 | 0.72–1.89 | .52 | ||||||
| IQg: IQ WNL (n = 454)/low IQ (n = 72) | 1.09 | 0.69–1.71 | .70 | 1.08 | 0.56–2.05 | .81 | ||||||
| Lifetime substance abuse: yes (n = 273)/no (n = 256) | 1.49 | 1.07–2.08 | .01* | 1.33 | 0.95–1.85 | .09$ | 1.78 | 1.10–2.90 | .01* | 1.56 | 0.94–2.58 | .08$ |
| Depression (HAM-D > 18)h: severe (n = 157)/mild (n = 348) | 2.18 | 1.57–3.04 | <.00*** | 1.19 | 1.05–1.36 | <.01** | 2.56 | 1.38–4.77 | <.01** | 1.74 | 1.04–2.89 | .03* |
| Insighti: acknowledges (n = 417)/denies (n = 110) | 1.62 | 1.03–2.56 | .03* | 1.18 | 0.73–1.90 | .54 | 1.77 | 0.90–3.46 | .09$ | |||
| Duration of symptomsj: <6 mo (n = 342)/>6 mo (n = 159) | 1.32 | 0.90–1.92 | .14 | 1.03 | 0.61–1.73 | .89 | ||||||
| SANS (negative symptoms) | 1.00 | 0.99–1.02 | .56 | 1.00 | 0.99–1.02 | .36 | ||||||
| SAPS (disorganized dimension) | 1.03 | 1.00–1.06 | .03* | 1.01 | 0.98–1.04 | .31 | 1.05 | 1.01–1.10 | .01* | 1.03 | 0.98–1.08 | .14 |
| SAPS (psychoticism dimension) | 1.00 | 0.99–1.02 | .41 | 1.01 | 0.98–1.04 | .24 | ||||||
| Lifetime suicide ideation: yes (n = 270)/no (n = 259) | 3.27 | 2.36–4.53 | <.00*** | 4.45 | 2.77–7.16 | <.00*** | ||||||
| Lifetime suicide attempts: yes (n = 148)/no (n = 381) | 3.96 | 2.66–5.89 | <.00*** | 2.88 | 2.07–4.02 | <.00*** | 7.05 | 3.50–14.18 | <.00*** | 3.55 | 2.17–5.79 | <.00*** |
Note: HR = hazard ratio, CI = confidence interval, HAM-D = Hamilton Depression Rating Scale, SANS = Scale for the Assessment of Negative Symptoms, SAPS = Scale for the Assessment of Positive Symptoms, *P < .05, **P < .01, ***P < .001, $ = approaching significance.
Omnibus Test of Model Coefficients (likelihood ratio) was significant (−2 log likelihood = 1735.146), overall score: χ2 = 66.70, df = 4, P < .001. All significant variables from previous univariable model were entered into multivariable model. Attempt measured at baseline (lifetime) was included in final model, whereas lifetime ideation was excluded due to high correlations between these 2 variables. Not shown is an alternative multivariable model excluding the variable lifetime attempts, which gave similar results.
n = 24 ideators were excluded due to missing values on the HAM-D.
Omnibus Test of Model Coefficients (likelihood ratio) was significant (−2 log likelihood = 824.766), overall score: χ2 = 58.61, df = 6, P < .00. All significant variables from previous univariable model were entered into multivariable model. Attempt measured at baseline (lifetime) was included into final model, whereas ideation (lifetime) was excluded due to high correlations among these 2 variables. Not shown is an alternative multivariable model excluding the variable lifetime attempts, which gave similar results.
n = 24 attempters were excluded due to missing values on the HAM-D.
n = 471, 58 persons have missing data.
n = 526, 3 persons have missing data.
n = 526, 3 persons have missing data.
n = 505, 24 persons have missing data.
n = 527, 2 persons have missing data.
n = 501, 28 persons have missing data.
The significant predictors were included in a multivariable model (table 1). Results indicated that a history of suicide attempts prior to baseline (HR = 2.88, CI = 2.07–4.02, P < .001) and severity of depression on the Hamilton at baseline (HR = 1.19, CI = 1.05–1.36, P < .01) were the only unique risk factors.
No significant effects were detected in analyses of predictors of ideation among respondents having no baseline attempts. Separate analyses conducted for the 2 broad diagnostic groups found a similar pattern of results as presented for the entire sample with the exception of substance abuse (lifetime), which was significant in the other psychosis group but not in the schizophrenia group (P = .03, tables available from J.R.).
Risk Factors for Suicide Attempts
Table 1 shows that the following variables assessed at time of first hospital admission were significant predictors of subsequent suicide attempt (in descending order): history of suicide attempts (HR = 7.05, CI = 3.50–14.18, P < .001), history of suicide ideation (HR = 4.45, CI = 2.77–7.16, P < .001), severity of depression on the Ham-D (HR = 2.56, CI = 1.38–4.77, P < .01), history of substance abuse (HR = 1.78, CI = 1.10–2.90, P < .05), greater thought disorder (SAPS, disorganization dimension, HR = 1.05, CI = 1.01–1.10, P < .05), and age younger than 28 years (HR = 1.03, CI = 1.00–1.05, P < .05). The following variables in descending order were not significant risk factors: insight into illness, SAPS psychoticism dimension, involuntary admission, negative symptom severity, high SES, diagnosis, sex, race, intellectual capacity, living alone, and duration of time between onset of psychosis and hospitalization.
The significant predictors were included in a multivariable model (table 1). Results indicated that a history of suicide attempts prior to baseline (HR = 3.55, CI = 2.17–5.79, P < .001), baseline Ham-D (HR = 1.74, CI = 1.04–2.89, P < .05), and age less than 28 years (HR = 1.03, CI = 1.00–1.06, P < .05) were unique risk factors.
When the analysis was restricted to respondents without a history of attempts before index hospitalization, the only significant predictor of future attempts was being Caucasian (HR = 4.30, CI = 1.02–18.13, P = .04). Separate analyses by diagnostic group again found a similar pattern of results with the exception of lifetime substance abuse that was significant (P = .03) in the other psychosis group but not in the schizophrenia group (tables available from J.R.). Given the smaller sample size of this analysis that limits power as compared with the entire cohort, we regarded differences of P < .10 as being of interest. The significant results obtained were the same for each diagnostic group as had been obtained for entire cohort with the exception of substance abuse that emerged for the schizophrenia group when predicting ideation (P = .08) and when predicting attempts (P = .09).
Summary Risk Index
The significant risk factors identified in the previous analyses (history of suicide attempts, Ham-D > 18, SAPS disorganized dimension > 5.5, having insight into illness, history of substance abuse, and age < 28 y) were used to construct a 3-point summary risk index (table 2). As seen by the HRs, there was an increase in subsequent ideation and attempts associated with each additional step of the risk index.
Table 2.
Suicide Risk Index Implemented to Predict Suicide Ideation and Attempts During 48 mo
| Probability of Suicide Ideation, 6–48 mo (n = 529)a |
Probability of Suicide Attempt, 6–48 mo (n = 529)b |
|||
| Risk category (variables measured at baseline) | % (n) | OR (95% CI)c | % (n) | OR (95% CI)d |
| Low (n = 169): no history of suicide attempt at baseline and having no more than 2 risk factors (ie, older than 28 years at admission, SAPS [disorganization] below 5.5, no substance abuse history, and depression scores < 18) | 12.4 (21/169) | — | 4.1 (7/169) | — |
| Intermediate (n = 212): no history of suicide attempt at baseline and having 3 or more other risk factors | 23.1 (49/212) | 1.90 (1.14–3.18) | 9.9 (21/212) | 2.42 (1.03–5.70) |
| High (n = 148): history of suicide attempt and 1 or more risk factors | 52.0 (77/148) | 4.91 (3.02–7.96) | 29.7 (44/148) | 7.97 (3.59–17.70) |
Note: OR = odds ratio, CI = confidence interval, SAPS = Scale for the Assessment of Positive Symptoms.
In the subsequent ideation model, the 3 groups were also dichotomized into low and intermediate vs high categories, OR = 4.81, CI = 3.18–7.28. Sensitivity, specificity, and positive predictive values are as follows: 52.3%, 18.5%, and 52.0%, respectively.
In the subsequent attempts model, the 3 groups were also dichotomized into low and intermediate vs high categories, OR = 5.33, CI = 3.16–8.98. Sensitivity, specificity, and positive predictive values are as follows: 61.1%, 22.7%, and 29.7%, respectively.
Cox regression predicting subsequent ideation, with risk index entered as a categorical variable with simple contrast. Omnibus Test of Model Coefficients (likelihood ratio) was significant (−2 log likelihood = 1746.43), overall score: χ2 = 56.19, df = 3, P < .001.
Cox regression predicting subsequent attempts, with risk index entered as a categorical variable with simple contrast. Omnibus Test of Model Coefficients (likelihood ratio) was significant (−2 log likelihood = 834.420), overall score: χ2 = 48.79, df = 3, P < .001.
The “low”-risk group consisted of 169 persons who had no history of previous suicide attempts and no more than 2 other risk factors; 6.5% (n = 11) had no other risk factors, 33.1% (n = 56) had 1, and 60.4% (n = 102) had 2. In this low-risk group, 12.4% (n = 21) had subsequent ideation and 4.1% (n = 7) made a subsequent attempt.
The “intermediate” risk group consisted of 212 persons who had no history of previous suicide attempts but had 3 or more other risk factors. Specifically, 65.1% (n = 138) had 3 other risk factors, 31.6% (n = 67) had 4, and 3.3% (n = 7) had 5. In this intermediate risk group, 23.1% (n = 49) had subsequent ideation and 9.9% (n = 21) made a subsequent attempt.
The “high”-risk group consisted of 148 persons who had a history of previous suicide attempts and at least 1 other risk factor. Most had multiple other risk factors. Specifically, 6.8% (n = 10) had 1 other risk factor, 27.0% (n = 40) had 2, 37.2% (n = 55) had 3, 25.7% (n = 38) had 4, and 3.4% (n = 5) had 5. In this high-risk group, 52.0% (n = 77) had subsequent ideation and 29.7% (n = 44) made a subsequent attempt.
Discussion
The current study traces suicide behaviors in a large first-admission cohort of persons with psychotic illnesses over 48 months since index hospital admission. We found that 28.0% entered the study with previous attempts, and 13.6% made attempts during the follow-up. Future suicide ideation and attempts were associated with a history of suicide attempts, severity of depressive symptoms, insight into illness, substance abuse, thought disorder, and age less than 28 years at the time of index admission.
There was a substantial increase in suicide risk associated with each additional step on the risk index; from low to intermediate, the risk more than doubled (4.1%–9.9%), and from intermediate to high, it more than tripled (9.9%–29.7%). The key risk factor in the high group was having a history of suicide attempts that surpassed all other risk factors in its predictive power. The risk index will need to be validated in additional cohorts, and these replications may also suggest the inclusion of other risk factors. If the index is basically confirmed in other samples, then it may offer clinicians a simple scoring tool to help screen for subsequent ideation and attempts that can be used to supplement clinician judgment. Clearly, an actuarial tool cannot replace clinician judgment and is not sensitive to unique situational variables. We note that all persons with a psychotic illness are at higher risk of suicidality than the general population, even the individuals in our low-risk group. Future prospective studies could employ the index to help detect patients potentially at high risk for future attempts.
The findings relating to a history of suicide as a powerful risk factor for future suicide are consistent with prior research in psychiatric17,36,52,53 and nonpsychiatric samples.18,38,42 Furthermore, a history of lifetime attempts was distinguished from other baseline variables as the strongest predictor of future suicide attempts. The current article identifies risk factors and a risk index that can be applied to help identify persons at risk. The number of suicide deaths was small and was insufficient for statistical analysis. However, the description of the 3 suicide deaths highlights the unique profiles among those who ultimately commit suicide.
Other risk factors associated with suicide in this study were consistent with the literature. Similar, but not as strong as in previous studies,8,17 age younger than 28 years was associated with suicidality. Severity of depressive symptoms was a risk factor,17,36 as was influence of substance abuse.1,54 Similar to recent studies,14,37,55 we found that insight was associated with future suicide albeit only in isolation of other risk factors.
We found that of the positive and negative symptom measures, only thought disorder was significantly associated with suicide. This finding is consistent with several prior studies that found an association between bizarre behavior (ie, paranoid ideation and suspiciousness) and suicide.10,12 In contrast, other studies propose interactive models linking both positive and negative symptoms to subsequent suicide based on diagnosis-specific models.56,57 Still others have found no association between positive or negative symptoms and suicide risk.17,36,58 A possible explanation for these inconsistencies might be the clinical heterogeneity among the samples, differences in sample sizes, and a lack of standardization in defining suicide behaviors.17
Our finding of no association between duration of interval from first psychotic symptom to hospitalization is contrary to previous reports supporting an association between DUP and lifetime suicide attempts.59,60 This finding is possibly the result of the considerable variations in the way this variable was measured and the difficulty in disentangling the effects of suicide attempts as a trigger for hospital admission. A suicide attempt could in some cases shorten DUP while in others be the result of protracted DUP.
While males with schizophrenia and females with other psychotic illnesses are reported to have an increased lifetime risk of suicide compared with their counterparts,61 we did not find sex to be a significant risk factor in this study. As previously reported, the suicide rates did not differ significantly between the schizophrenia and other psychosis respondents.62 This finding supports the notion that suicide behaviors may be related to the presence of any psychotic illness rather than to the specific diagnostic condition. Furthermore, suicide behaviors were not consistently associated with race, living status, intellectual capacity, voluntary vs involuntary admission, and SES. This is consistent with several other reviews reporting inconclusive associations between many risk factors (race, living status, IQ level,8,63 voluntary vs involuntary admission, and SES36) and suicide behaviors.
Previous early episode studies have reported that among young patients, up to 5%15,23,26,60 and as high as 10%4 completed suicide within the first 4–19 years after first hospitalization. We note that our prospective ongoing data collection involved intensive, albeit nontherapeutic, contact by mental health clinicians,62 and it is conceivable that their support had a protective effect on the respondents and hence reduced their suicide risk.
The current study had several limitations. First, the cohort was assembled during a specific time period and geographic location, and although the sample was drawn from all hospitals in a large county, the generalizability is limited. Second, the risk factors were measured at baseline only and treated as predictors, but some of them, such as living status, could have changed during the follow-up study. Future research needs to address time-varying covariates as well as baseline predictors. Third, information was retrospective at follow-up and might have led to underenumerating the number of attempts, thus diminishing the strength of the risk index. Fourth, an examination of presence or absence of a suicide plan and lethality of intent could not be analyzed because of power considerations; future studies with larger samples should consider these factors particularly because they relate to subsequent completed suicide. Fifth, it would be important to compare the risk factors for suicide behaviors among those in the early course of illness with individuals who have been ill for a long time. Sixth, future research is needed to examine the predictors of subsequent suicide behaviors in larger samples of previous nonattempters, with particular attention to race. Lastly, the risk index was developed and tested on the same cohort, and its predictive ability needs to be validated in additional cohorts.
Conclusions
In summary, the current epidemiologically based findings suggest that persons with a first admission for psychosis are a very vulnerable group for suicide behaviors. Early recognition of individuals who are at risk may prove to be key in the prevention of future suicide attempts. To aid clinicians in early identification of persons at increased risk of suicide attempts, a cumulative risk index has been proposed. Collectively, it is suggested that persons with histories of suicide behaviors, insight into illness, substance abuse, thought disorder, depressive symptoms, and age less than 28 years at time of first admission should be carefully monitored for future suicide attempts.
Funding
This work was funded by NIH grant MH44801 (to EJB), the Elie Weisel Chair (J Rabinowitz), and the President's Doctoral Fellowship (S Bakst), both at Bar Ilan University.
Acknowledgments
This work was part of doctoral research conducted at Bar Ilan University. The authors acknowledge the respondents, psychiatrists, and interviewers who participated over many years and Su-wei Chang and Stephen Levine for data management support.
References
- 1.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 2.Allebeck P. Schizophrenia: a life-shortening disease. Schizophr Bull. 1989;15:81–89. doi: 10.1093/schbul/15.1.81. [DOI] [PubMed] [Google Scholar]
- 3.Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry. 1997;171:502–508. doi: 10.1192/bjp.171.6.502. [DOI] [PubMed] [Google Scholar]
- 4.Westermeyer JF, Harrow M, Marengo JT. Risk for suicide in schizophrenia and other psychotic and nonpsychotic disorders. J Nerv Ment Dis. 1991;179:259–266. doi: 10.1097/00005053-199105000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Meltzer HY. Suicide in schizophrenia, clozapine, and adoption of evidence-based medicine. J Clin Psychiatry. 2005;66:530–533. doi: 10.4088/jcp.v66n0417. [DOI] [PubMed] [Google Scholar]
- 6.Inskip HM, Harris EC, Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Br J Psychiatry. 1998;172:35–37. doi: 10.1192/bjp.172.1.35. [DOI] [PubMed] [Google Scholar]
- 7.Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry. 2005;62:247–253. doi: 10.1001/archpsyc.62.3.247. [DOI] [PubMed] [Google Scholar]
- 8.Caldwell CB, Gottesman II. Schizophrenics kill themselves too: a review of risk factors for suicide. Schizophr Bull. 1990;16:571–589. doi: 10.1093/schbul/16.4.571. [DOI] [PubMed] [Google Scholar]
- 9. Division of Vital Statistics, National Vital Statistics Reports, April 24th, 2008. http://www.cdc.gov/nchs/fastats/suicide.htm. [Google Scholar]
- 10.Fenton WS, McGlashan TH, Victor BJ, Blyler CR. Symptoms, subtype, and suicidality in patients with schizophrenia spectrum disorders. Am J Psychiatry. 1997;154:199–204. doi: 10.1176/ajp.154.2.199. [DOI] [PubMed] [Google Scholar]
- 11.Harkavy-Friedman JM, Restifo K, Malaspina D, et al. Suicidal behavior in schizophrenia: characteristics of individuals who had and had not attempted suicide. Am J Psychiatry. 1999;156:1276–1278. doi: 10.1176/ajp.156.8.1276. [DOI] [PubMed] [Google Scholar]
- 12.Pompili M, Mancinelli I, Ruberto A, Kotzalidis GD, Giardi P, Tatarelli R. Where schizophrenic patients commit suicide: a review of suicide among inpatients and former inpatients. Int J Psychiatry Med. 2005;35:171–190. doi: 10.2190/9CA1-EL73-1VXD-9F2V. [DOI] [PubMed] [Google Scholar]
- 13.Meltzer HY, Alphs L, Green AI, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT) Arch Gen Psychiatry. 2003;60:82–91. doi: 10.1001/archpsyc.60.1.82. [DOI] [PubMed] [Google Scholar]
- 14.Kim CH, Jayathilake K, Meltzer HY. Hopelessness, neurocognitive function, and insight in schizophrenia: relationship to suicidal behavior. Schizophr Res. 2003;60:71–80. doi: 10.1016/s0920-9964(02)00310-9. [DOI] [PubMed] [Google Scholar]
- 15.Fenton WS. Depression, suicide, and suicide prevention in schizophrenia. Suicide Life Threat Behav. 2000;30:34–49. [PubMed] [Google Scholar]
- 16.Verdoux H, Liraud F, Gonzales B, Assens F, Abalan F, Van Os J. Predictors and outcome characteristics associated with suicidal behaviour in early psychosis: a two-year follow-up of first-admitted subjects. Acta Psychiatr Scand. 2001;103:347–354. doi: 10.1034/j.1600-0447.2001.00202.x. [DOI] [PubMed] [Google Scholar]
- 17.Pompili M, Amador XF, Girardi P, et al. Suicide risk in schizophrenia: learning from the past to change the future. Ann Gen Psychiatry. 2007;6:10. doi: 10.1186/1744-859X-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617–626. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 19.De Hert M, McKenzie K, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long-term follow-up study. Schizophr Res. 2001;47:127–134. doi: 10.1016/s0920-9964(00)00003-7. [DOI] [PubMed] [Google Scholar]
- 20.Drake RE, Gates C, Cotton PG. Suicide among schizophrenics: a comparison of attempters and completed suicides. Br J Psychiatry. 1986;149:784–787. doi: 10.1192/bjp.149.6.784. [DOI] [PubMed] [Google Scholar]
- 21.Harkavy-Friedman JM, Nelson E. Management of the suicidal patient with schizophrenia. Psychiatr Clin North Am. 1997;20:625–640. doi: 10.1016/s0193-953x(05)70334-8. [DOI] [PubMed] [Google Scholar]
- 22.Nordentoft M, Jeppesen P, Abel M, et al. OPUS study: suicidal behaviour, suicidal ideation and hopelessness among patients with first-episode psychosis. One-year follow-up of a randomised controlled trial. Br J Psychiatry Suppl. 2002;43:s98–s106. doi: 10.1192/bjp.181.43.s98. [DOI] [PubMed] [Google Scholar]
- 23.Jarbin H, Von Knorring AL. Suicide and suicide attempts in adolescent-onset psychotic disorders. Nord J Psychiatry. 2004;58:115–123. doi: 10.1080/08039480410005611. [DOI] [PubMed] [Google Scholar]
- 24.Harkavy-Friedman JM. Can early detection of psychosis prevent suicidal behavior? Am J Psychiatry. 2006;163:768–770. doi: 10.1176/ajp.2006.163.5.768. [DOI] [PubMed] [Google Scholar]
- 25.Addington J, Williams J, Young J, Addington D. Suicidal behaviour in early psychosis. Acta Psychiatr Scand. 2004;109:116–120. doi: 10.1046/j.0001-690x.2003.00232.x. [DOI] [PubMed] [Google Scholar]
- 26.Kuo CJ, Tsai SY, Lo CH, Wang YP, Chen CC. Risk factors for completed suicide in schizophrenia. J Clin Psychiatry. 2005;66:579–585. doi: 10.4088/jcp.v66n0506. [DOI] [PubMed] [Google Scholar]
- 27.Caldwell CB, Gottesman II. Schizophrenia–a high-risk factor for suicide: clues to risk reduction. Suicide Life Threat Behav. 1992;22:479–493. [PubMed] [Google Scholar]
- 28.Cohen S, Lavelle J, Rich CL, Bromet E. Rates and correlates of suicide attempts in first-admission psychotic patients. Acta Psychiatr Scand. 1994;90:167–171. doi: 10.1111/j.1600-0447.1994.tb01573.x. [DOI] [PubMed] [Google Scholar]
- 29.Grossman LS, Harrow M, Rosen C, Faull R. Sex differences in outcome and recovery for schizophrenia and other psychotic and nonpsychotic disorders. Psychiatr Serv. 2006;57:844–850. doi: 10.1176/ps.2006.57.6.844. [DOI] [PubMed] [Google Scholar]
- 30.Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, et al. Sex differences in clinical predictors of suicidal acts after major depression: a prospective study. Am J Psychiatry. 2007;164:134–141. doi: 10.1176/appi.ajp.164.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lewine RR. Social class of origin, lost potential, and hopelessness in schizophrenia. Schizophr Res. 2005;76:329–335. doi: 10.1016/j.schres.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 32.Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15:127–135. doi: 10.1177/026988110101500209. [DOI] [PubMed] [Google Scholar]
- 33.Harkavy-Friedman JM, Nelson EA, Venarde DF, Mann JJ. Suicidal behavior in schizophrenia and schizoaffective disorder: examining the role of depression. Suicide Life Threat Behav. 2004;34:66–76. doi: 10.1521/suli.34.1.66.27770. [DOI] [PubMed] [Google Scholar]
- 34.Gupta S, Black DW, Arndt S, Hubbard WC, Andreasen NC. Factors associated with suicide attempts among patients with schizophrenia. Psychiatr Serv. 1998;49:1353–1355. doi: 10.1176/ps.49.10.1353. [DOI] [PubMed] [Google Scholar]
- 35.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 36.Hawton K, Sutton L, Haw C, Sinclair J, Deeks JJ. Schizophrenia and suicide: systematic review of risk factors. Br J Psychiatry. 2005;187:9–20. doi: 10.1192/bjp.187.1.9. [DOI] [PubMed] [Google Scholar]
- 37.Bourgeois M, Swendsen J, Young F, et al. Awareness of disorder and suicide risk in the treatment of schizophrenia: results of the international suicide prevention trial. Am J Psychiatry. 2004;161:1494–1496. doi: 10.1176/appi.ajp.161.8.1494. [DOI] [PubMed] [Google Scholar]
- 38.Borges G, Angst J, Nock MK, Ruscio AM, Walters EE, Kessler RC. A risk index for 12-month suicide attempts in the National Comorbidity Survey Replication (NCS-R) Psychol Med. 2006;36:1747–1757. doi: 10.1017/S0033291706008786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bromet EJ, Naz B, Fochtmann LJ, Carlson GA, Tanenberg-Karant M. Long-term diagnostic stability and outcome in recent first-episode cohort studies of schizophrenia. Schizophr Bull. 2005;31:639–649. doi: 10.1093/schbul/sbi030. [DOI] [PubMed] [Google Scholar]
- 40.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical Interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 41.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293:2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- 43.Craig TJ, Bromet EJ, Fennig S, Tanenberg-Karant M, Lavelle J, Galambos N. Is there an association between duration of untreated psychosis and 24-month clinical outcome in a first-admission series? Am J Psychiatry. 2000;157:60–66. doi: 10.1176/ajp.157.1.60. [DOI] [PubMed] [Google Scholar]
- 44.Brown AS, Susser ES, Jandorf L, Bromet EJ. Social class of origin and cardinal symptoms of schizophrenic disorders over the early illness course. Soc Psychiatry Psychiatr Epidemiol. 2000;35:53–60. doi: 10.1007/s001270050008. [DOI] [PubMed] [Google Scholar]
- 45.Ammons RB, Ammons CH. The Quick Test: provisional manual. Psychol Rep. 1962:111–161. [Google Scholar]
- 46.Schwartz JE, Fennig S, Tanenberg-Karant M, et al. Congruence of diagnoses 2 years after a first-admission diagnosis of psychosis. Arch Gen Psychiatry. 2000;57:593–600. doi: 10.1001/archpsyc.57.6.593. [DOI] [PubMed] [Google Scholar]
- 47.Andreasen NC, Olsen S. Negative v positive schizophrenia. Definition and validation. Arch Gen Psychiatry. 1982;39:789–794. doi: 10.1001/archpsyc.1982.04290070025006. [DOI] [PubMed] [Google Scholar]
- 48.Andreasen NC. Negative symptoms in schizophrenia. Definition and reliability. Arch Gen Psychiatry. 1982;39:784–788. doi: 10.1001/archpsyc.1982.04290070020005. [DOI] [PubMed] [Google Scholar]
- 49.Kotov R, Guey LT, Bromet EJ, Schwartz JE. Smoking in schizophrenia: diagnostic specificity, symptom correlates, and illness severity. Schizophr Bull. doi: 10.1093/schbul/sbn066. June 17, 2008; doi:10.1093/schbul/sbn066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mcdowell I, Newell C. Measuring Health: A Guide to Rating Scales and Questionnaires. New York, NY: Oxford University Press; 2006. pp. 369–378. [Google Scholar]
- 51.Fennig S, Everett E, Bromet EJ, et al. Insight in first-admission psychotic patients. Schizophr Res. 1996;22:257–263. doi: 10.1016/s0920-9964(96)00077-1. [DOI] [PubMed] [Google Scholar]
- 52.Limosin F, Loze JY, Philippe A, Casadebaig F, Rouillon F. Ten-year prospective follow-up study of the mortality by suicide in schizophrenic patients. Schizophr Res. 2007;94:23–28. doi: 10.1016/j.schres.2007.04.031. [DOI] [PubMed] [Google Scholar]
- 53.Harkavy-Friedman JM, Kimhy D, Nelson EA, Venarde DF, Malaspina D, Mann JJ. Suicide attempts in schizophrenia: the role of command auditory hallucinations for suicide. J Clin Psychiatry. 2003;64:871–874. [PubMed] [Google Scholar]
- 54.Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76(suppl):S11–S19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- 55.Crumlish N, Whitty P, Kamali M, et al. Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatr Scand. 2005;112:449–455. doi: 10.1111/j.1600-0447.2005.00620.x. [DOI] [PubMed] [Google Scholar]
- 56.Kaplan KJ, Harrow M. Positive and negative symptoms as risk factors for later suicidal activity in schizophrenics versus depressives. Suicide Life Threat Behav. 1996;26:105–121. [PubMed] [Google Scholar]
- 57.Kaplan KJ, Harrow M. Psychosis and functioning as risk factors for later suicidal activity among schizophrenia and schizoaffective patients: a disease-based interactive model. Suicide Life Threat Behav. 1999;29:10–24. [PubMed] [Google Scholar]
- 58.Grunebaum MF, Oquendo MA, Harkavy-Friedman JM, et al. Delusions and suicidality. Am J Psychiatry. 2001;158:742–747. doi: 10.1176/appi.ajp.158.5.742. [DOI] [PubMed] [Google Scholar]
- 59.Altamura AC, Bassetti R, Bignotti S, Pioli R, Mundo E. Clinical variables related to suicide attempts in schizophrenic patients: a retrospective study. Schizophr Res. 2003;60:47–55. doi: 10.1016/s0920-9964(02)00164-0. [DOI] [PubMed] [Google Scholar]
- 60.Clarke M, Whitty P, Browne S, et al. Suicidality in first episode psychosis. Schizophr Res. 2006;86:221–225. doi: 10.1016/j.schres.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 61.Thorup A, Petersen L, Jeppesen P, et al. Gender differences in young adults with first-episode schizophrenia spectrum disorders at baseline in the Danish OPUS study. J Nerv Ment Dis. 2007;195:396–405. doi: 10.1097/01.nmd.0000253784.59708.dd. [DOI] [PubMed] [Google Scholar]
- 62.Craig TJ, Ye Q, Bromet EJ. Mortality among first-admission patients with psychosis. Compr Psychiatry. 2006;47:246–251. doi: 10.1016/j.comppsych.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 63.Drake RE, Gates C, Cotton PG, Whitaker A. Suicide among schizophrenics. Who is at risk? J Nerv Ment Dis. 1984;172:613–617. doi: 10.1097/00005053-198410000-00004. [DOI] [PubMed] [Google Scholar]