Abstract
Cilia are microscopic projections that extend from eukaryotic cells. There are two general types of cilia; primary cilia serve as sensory organelles, whereas motile cilia exert mechanical force. The motile cilia emerging from human airway epithelial cells propel harmful inhaled material out of the lung. We found that these cells express sensory bitter taste receptors, which localized on motile cilia. Bitter compounds increased the intracellular Ca2+ concentration and stimulated ciliary beat frequency. Thus, airway epithelia contain a cell-autonomous system in which motile cilia both sense noxious substances entering airways and initiate a defensive mechanical mechanism to eliminate the offending compound. Hence, like primary cilia, classical motile cilia also contain sensors to detect the external environment.
Cilia can be divided into two general types, primary and motile (1–3). Primary cilia are sensory organelles that contain a variety of receptors, including G protein-coupled receptors (GPCRs) (1). Cells typically sprout a single primary cilium with a characteristic 9+0 cytoskeletal structure (axoneme). In contrast, motile cilia can occur in the tens and hundreds on epithelial cells, they have a typical 9+2 axoneme, and they serve a mechanical role (1–3). Although their functions differ, there are exceptions to the primary cilia-motile cilia distinction (3, 4); for example, primary nodal cilia exhibit rotational movement (29, 30). In addition, the two types of cilia share many structural and molecular features (2, 7), they are evolutionarily related (8) and genetic diseases such as Bardet-Biedl Syndrome can affect both (9–11). However, whether classic motile cilia can also function as sensory organelles is not clear.
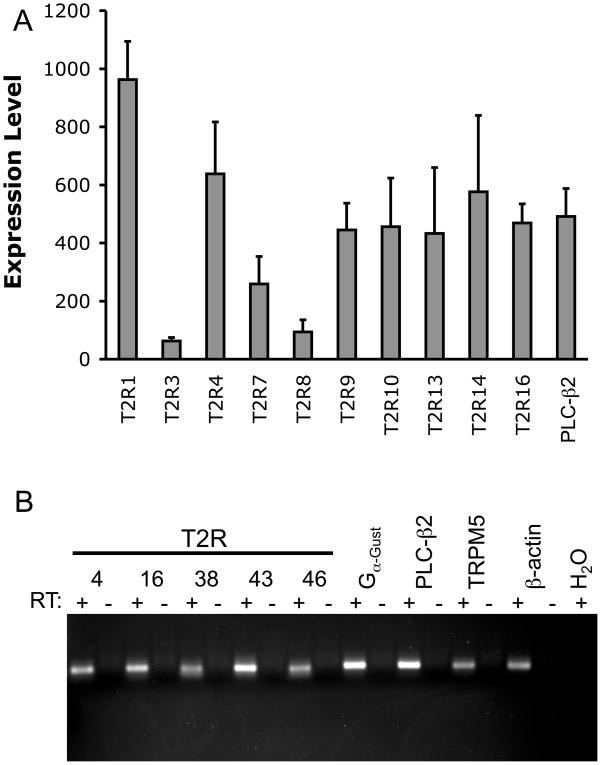
On airway epithelia, motile cilia move mucus out of the lung, and their disruption causes airway disease (12, 13). Because defense of the airway involves detection of danger signals, we hypothesized that motile cilia might sense noxious stimuli. To test this hypothesis, we searched for sensory-related genes in microarray expression data from primary cultures of differentiated human airway epithelia (14). Microarray analysis (15) and reverse transcription-polymerase chain reaction (RT-PCR) revealed that the epithelia expressed several members of the bitter taste receptor (T2R) family (Fig. 1A, 1B). The human genome contains ~25 T2R genes. Several may detect more than one different bitter compound, and individual taste receptor cells express multiple T2Rs (16, 17). Thus, in the tongue, the system is broadly tuned to detect multiple bitter compounds and warn against ingestion of toxic substances.
Figure 1.
Bitter taste receptors are expressed in human airway epithelia. (A) Microarray analysis of mRNA isolated from airway epithelial samples isolated from eight human donors (15). Data are mean±SEM. (B) RT-PCR analysis of mRNA isolated from differentiated cultures of human airway epithelia.
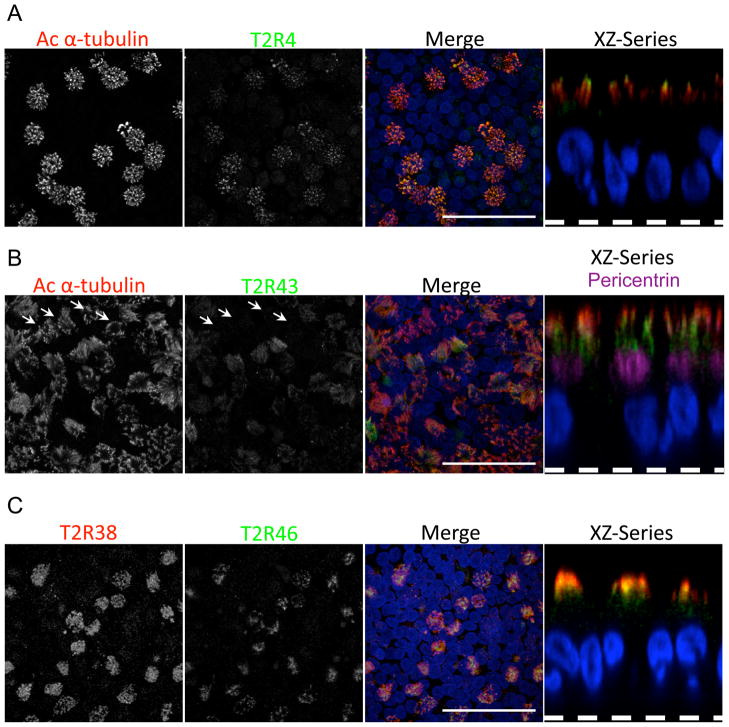
We studied several T2Rs for which antibodies are available and/or for which ligands are known, and w identified T2R4, T2R43, T2R38, and T2R46 in human airway epithelia (Fig. 2A–2C, S1–S6). Only ciliated epithelial cells expressed these receptors, and they specifically localized in cilia, which were identified by acetylated α-tubulin immunostaining. Almost every ciliated cell expressed each of the four T2Rs, although the intensity varied from cell to cell and in some ciliated cells T2R43 was not detected (Fig. 2B). Thus single ciliated epithelial cells express multiple T2Rs, rather like individual taste receptor cells that express multiple T2Rs (18). The receptors appeared to localize preferentially at different places along the cilium. For example, T2R4 seemed to sit nearer the tips of cilia, whereas T2R43 appeared to reside more proximally in cilia (Fig. 2A, 2B, S1, S3, S7), which was more apparent when we immunostained both T2R4 and T2R43 in the same epithelia (Fig. S7). Co-labeling T2R38 and T2R46 revealed a similar relationship, with T2R38 appearing to sit more distally than T2R46 (Fig. 2C, S7).
Figure 2.
T2Rs localize along the motile cilia of airway epithelia. Confocal immunofluorescence microscopy of cultured human airway epithelia with anti-T2R antibodies showed that (A) T2R4 and (B) T2R43 (both green) localize to motile cilia, which were identified by antibody to acetylated α-tubulin (red). Nuclei stained with DAPI are blue. Arrows in panel B indicate location of ciliated cells that were not labeled by anti-T2R43 antibody. (C) T2R38 (red) and T2R46 (green) localize to motile cilia. Data are stacks of confocal z-series images in X-Y plane and a single X-Z plane image (right, dashed line indicates the filter). Panel B (right) also shows anti-pericentrin antibody (purple), which labels the basal body below cilia. Scale bars indicate 20 μM. See also Fig. S1–S7.
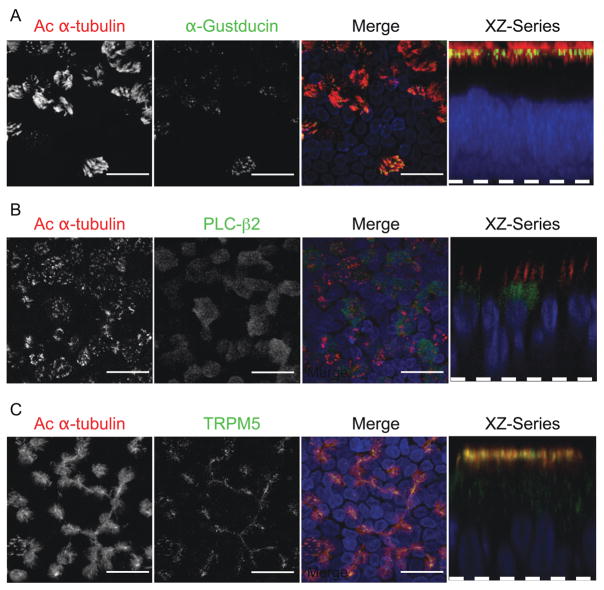
The T2R signal transduction pathway comprises several proteins, including the G-protein α-gustducin, the enzyme phospholipase C-β2, (PLC-β2), and the transient receptor potential channel-M5 (TRPM5) (16, 17). We detected transcripts for all three in airway epithelia (Fig. 1B). Immunostaining revealed these signaling molecules only in ciliated epithelial cells (Fig. 3A–3C, S3). Like the T2Rs, α-gustducin and TRPM5 resided in cilia. In contrast, PLC-β2 appeared to sit below the cilia in the apical portion of the cell. We speculate that the seeming complexity of T2R and signaling protein localization along the ciliary shaft and in the cell might provide a mechanism for coupling to other signaling pathways or influencing cilia function. Distinct localization may also occur with other proteins that are localized proximally in cilia and flagella (19–20).
Figure 3.
Components of the bitter taste transduction pathway localize to ciliated cells and to the cilia. Immunolocalization of (A) α-gustducin, (B) PLC-β2, and (C) TRPM5 are in green and acetylated α-tubulin is in red. Other aspects of Figure are as described in legend of Fig. 2. Scale bars indicate 20 μM. See also Fig. S1–S3.
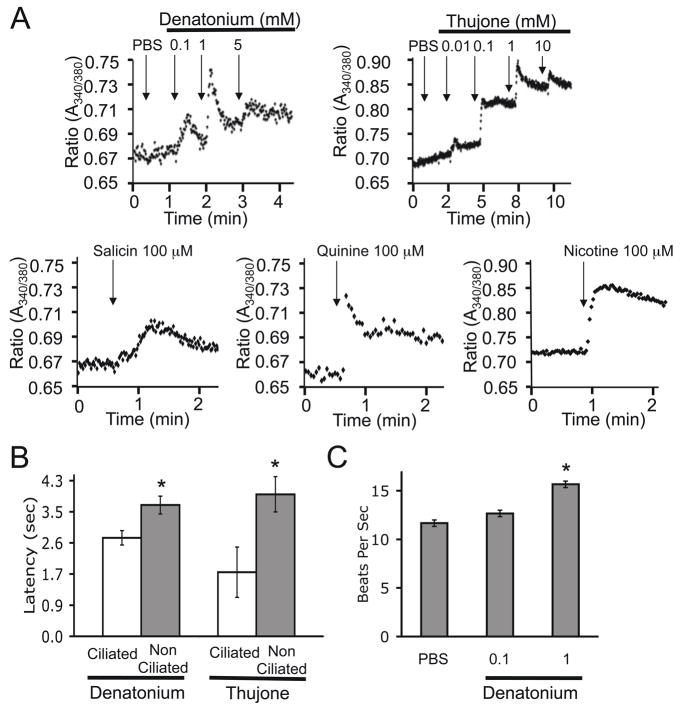
To determine whether the T2R signaling pathway was functional, we applied bitter compounds to differentiated human airway epithelia and measured changes in the T2R-associated second messenger, intracellular Ca2+ concentration [Ca2+]i. Denatonium is a very bitter compound and a ligand for T2R4 (16). Its application induced transient, dose-dependent elevations of [Ca2+]i (Fig. 4A). Several other bitter compounds, including thujone (activates T2R14), salicin (activates T2R16), quinine, and nicotine also elicited [Ca2+]i elevations. The denatonium and thujone concentrations inducing [Ca2+]i elevations were in the same range as those that elicit responses in heterologous cells expressing T2Rs (21).
Figure 4.
Bitter compounds increase [Ca2+]i in ciliated cells. (A) Differentiated airway epithelia were loaded with Fura2-AM and fluorescence imaging was performed to assess changes in [Ca2+]i, indicated as the ratio of 340nm/380nm. Denatonium, thujone, salicin, quinine, or nicotine was added as indicated. “PBS” indicates addition of phosphate buffered saline and arrows indicate the time of addition. Data points are average of 20 cells. (B) Latency to increase in [Ca2+]i following addition of 1 mM denatonium or 1 mM thujone; latency includes the time for the compound to diffuse to the cell following its addition. Asterisks indicate P<0.001, N = 20. See also Fig. S8. (C) Denatonium increases ciliary beat frequency. Data are ciliary beat frequency in differentiated human airway epithelia treated with PBS or denatonium. N = 4. Asterisks indicate P<0.01. See also Fig. S8, S9.
Airway epithelia contain both ciliated and non-ciliated cells, and when [Ca2+]i increases in an individual airway epithelial cell, it can rapidly spread through gap junctions to adjacent cells (22). Thus, the [Ca2+]i increase shown in Fig. 4A could have begun from either cell type. Therefore, we asked if [Ca2+]i first increased in ciliated or non-ciliated cells by applying the bitter compound apically and comparing the latency to a [Ca2+]i elevation in the different cells. After adding denatonium or thujone, [Ca2+]i rose in ciliated cells before increasing in other cells (Fig. 4B), consistent with our finding that only ciliated cells bear receptors for bitter compounds. We also studied cells growing on glass in short-term culture because the [Ca2+]i increase does not spread; in those cells denatonium increased [Ca2+]i only in ciliated cells (Fig. S8).
We assessed the functional consequences of activating T2Rs in airway epithelia by measuring the frequency of cilia beating. Because an elevated [Ca2+]i can stimulate ciliary motility (23), we predicted that a bitter compound would increase frequency. Indeed, applying denatonium increased cilia beat frequency ~25% (Fig. 4C, S9).
Thus some of the same receptors that detect noxious compounds on the tongue to protect animals from ingesting harmful material may also defend human airways. The receptors are positioned on cilia, a location optimal for sampling air and material entering the lung. Moreover, the bitter compound denatonium stimulated ciliary activity, which should hasten elimination of noxious and harmful substances. Substances that activate T2Rs might enter airways through inhalation or aspiration or be generated within the lung by infection. We speculate that this signaling system might also play a role in airway disease. For example, in cystic fibrosis, lungs are commonly infected with Pseudomonas aeruginosa. This bacterium produces quorum-sensing molecules that are lactones, which activate some bitter taste receptors (24, 25). Airway T2Rs might also be activated by cigarette smoke, which contains the bitter tasting compound nicotine (26). In addition, airway cilia are lost in some viral infections and with cigarette smoking (27), which would disrupt this defensive system.
Previous work suggested a general dichotomy for vertebrate cilia – primary cilia are sensory and motile cilia are mechanical. Studies of primary nodal cilia in embryos indicated that the distinction is not absolute; those cilia can exhibit a rotational movement different from the planar beating typical of motile cilia (5, 6). Now our data indicate that classical motile cilia also have a sensory function.
T2Rs on taste receptor cells, which are not known to have primary cilia, detect bitter ligands and transmit that information to nerves to elicit a response (16, 21). In cells outside the tongue where α-gustducin and T2Rs have been identified - nasal and laryngeal solitary chemosensory cells (SCCs) and intestinal tract enteroendocrine cells - signals are transmitted to the associated nerve networks (28–30). In contrast, in airway epithelia, T2Rs enable cell-autonomous detection of a signal followed by a response in the same cell to eliminate harmful substances.
Supplementary Material
Acknowledgments
We thank T. Yin for assistance and discussions and P. Karp, T. Nesselhauf, P. Hughes, and the In Vitro Models and Cell Culture Core (supported in part by the National Heart, Lung, and Blood Institute (HL51670), Cystic Fibrosis Foundation (R458-CR02 and ENGLH9850), and the National Institute of Diabetes and Digestive and Kidney Disease (DK54759)) for excellent assistance. YBS was an Associate and MJW is an Investigator of the HHMI.
References and Notes
- 1.Singla V, Reiter JF. Science. 2006;313:629. doi: 10.1126/science.1124534. [DOI] [PubMed] [Google Scholar]
- 2.Marshall WF, Nonaka S. Curr Biol. 2006;16:R604. doi: 10.1016/j.cub.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 3.Fliegauf M, Benzing T, Omran H. Nat Rev Mol Cell Biol. 2007;8:880. doi: 10.1038/nrm2278. [DOI] [PubMed] [Google Scholar]
- 4.Basu B, Brueckner M. Curr Top Dev Biol. 2008;85:151. doi: 10.1016/S0070-2153(08)00806-5. [DOI] [PubMed] [Google Scholar]
- 5.Hirokawa N, Tanaka Y, Okada Y, Takeda S. Cell. 2006;125:33. doi: 10.1016/j.cell.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 6.McGrath J, Somlo S, Makova S, Tian X, Brueckner M. Cell. 2003;114:61. doi: 10.1016/s0092-8674(03)00511-7. [DOI] [PubMed] [Google Scholar]
- 7.Davenport JR, Yoder BK. Am J Physiol Renal Physiol. 2005;289:F1159. doi: 10.1152/ajprenal.00118.2005. [DOI] [PubMed] [Google Scholar]
- 8.Satir P, Mitchell DR, Jekely G. Curr Top Dev Biol. 2008;85:63. doi: 10.1016/S0070-2153(08)00803-X. [DOI] [PubMed] [Google Scholar]
- 9.Davis RE, et al. Proc Natl Acad Sci USA. 2007;104:19422. [Google Scholar]
- 10.Shah AS, et al. Proc Natl Acad Sci USA. 2008;105:3380. [Google Scholar]
- 11.Nachury MV, et al. Cell. 2007;129:1201. doi: 10.1016/j.cell.2007.03.053. [DOI] [PubMed] [Google Scholar]
- 12.Horvath G, Sorscher EJ. Cell Motil Cytoskeleton. 2008;65:469. doi: 10.1002/cm.20273. [DOI] [PubMed] [Google Scholar]
- 13.Afzelius BA. J Pathol. 2004;204:470. doi: 10.1002/path.1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Karp PH, et al. In: Epithelial Cell Culture Protocols. Wise C, editor. Vol. 188. Humana Press, Inc; Totowa, NJ: 2002. pp. 115–137. [Google Scholar]
- 15.Zabner J, et al. Am J Physiol Lung Cell Mol Physiol. 2005;289:L545. doi: 10.1152/ajplung.00065.2005. [DOI] [PubMed] [Google Scholar]
- 16.Meyerhof W. Rev Physiol Biochem Pharmacol. 2005;154:37. doi: 10.1007/s10254-005-0041-0. [DOI] [PubMed] [Google Scholar]
- 17.Chandrashekar J, Hoon MA, Ryba NJ, Zuker CS. Nature. 2006;444:288. doi: 10.1038/nature05401. [DOI] [PubMed] [Google Scholar]
- 18.Behrens M, Foerster S, Staehler F, Raguse JD, Meyerhof W. J Neurosci. 2007;27:12630. doi: 10.1523/JNEUROSCI.1168-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shiba D, et al. J Cell Sci. 2009;122:44. doi: 10.1242/jcs.037408. [DOI] [PubMed] [Google Scholar]
- 20.Iomini C, Li L, Mo W, Dutcher SK, Piperno G. Curr Biol. 2006;16:1147. doi: 10.1016/j.cub.2006.04.035. [DOI] [PubMed] [Google Scholar]
- 21.Chandrashekar J, et al. Cell. 2000;100:703. doi: 10.1016/s0092-8674(00)80706-0. [DOI] [PubMed] [Google Scholar]
- 22.Boitano S, Sanderson MJ, Dirksen ER. J Cell Sci. 1994;107(Pt 11):3037. doi: 10.1242/jcs.107.11.3037. [DOI] [PubMed] [Google Scholar]
- 23.Braiman A, Priel Z. Respir Physiol Neurobiol. 2008;163:202. doi: 10.1016/j.resp.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 24.Brockhoff A, Behrens M, Massarotti A, Appendino G, Meyerhof W. J Agric Food Chem. 2007;55:6236. doi: 10.1021/jf070503p. [DOI] [PubMed] [Google Scholar]
- 25.Davies DG, et al. Science. 1998;280:295. doi: 10.1126/science.280.5361.295. [DOI] [PubMed] [Google Scholar]
- 26.Oliveira-Maia AJ, et al. Proc Natl Acad Sci U S A. 2009;106:1596. doi: 10.1073/pnas.0810184106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sisson JH, et al. Am J Respir Crit Care Med. 1994;149:205. doi: 10.1164/ajrccm.149.1.8111584. [DOI] [PubMed] [Google Scholar]
- 28.Gulbransen BD, Clapp TR, Finger TE, Kinnamon SC. J Neurophysiol. 2008;99:2929. doi: 10.1152/jn.00066.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Merigo F, Benati D, Tizzano M, Osculati F, Sbarbati A. Cell Tissue Res. 2005;319:211. doi: 10.1007/s00441-004-1007-2. [DOI] [PubMed] [Google Scholar]
- 30.Kaske S, et al. BMC Neurosci. 2007;8:49. doi: 10.1186/1471-2202-8-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.