Abstract
Background
Defibrotide is a novel orally bioavailable polydisperse oligonucleotide with anti-thrombotic and anti-adhesive effects. In SCID/NOD mice, defibrotide showed activity in human myeloma xenografts. This phase I/II study was conducted to identify the most appropriate dose of defibrotide in combination with melphalan, prednisone and thalidomide in patients with relapsed and relapsed/refractory multiple myeloma, and to determine its safety and tolerability as part of this regimen.
Design and Methods
This was a phase I/II, multicenter, dose-escalating, non-comparative, open label study. Oral melphalan was administered at a dose of 0.25 mg/kg on days 1–4, prednisone at a dose of 1.5 mg/kg also on days 1–4 and thalidomide at a dose of 50–100 mg/day continuously. Defibrotide was administered orally at three dose-levels: 2.4, 4.8 or 7.2 g on days 1–4 and 1.6, 3.2, or 4.8 g on days 5–35.
Results
Twenty-four patients with relapsed/refractory multiple myeloma were enrolled. No dose-limiting toxicity was observed. In all patients, the complete response plus very good partial response rate was 9%, and the partial response rate was 43%. The 1-year progression-free survival and 1-year overall survival rates were 34% and 90%, respectively. The most frequent grade 3–4 adverse events included neutropenia, thrombocytopenia, anemia and fatigue. Deep vein thrombosis was reported in only one patient.
Conclusions
This combination of melphalan, prednisone and thalidomide together with defibrotide showed anti-tumor activity with a favorable tolerability. The maximum tolerated dose of defibrotide was identified as 7.2 g p.o. on days 1–4 followed by 4.8 g p.o. on days 5–35. Further trials are needed to confirm the role of this regimen and to evaluate the combination of defibrotide with new drugs (ClinicalTrials.gov Identifier: NCT00406978).
Keywords: melphalan, defibrotide, SCID/NOD mice, multiple myeloma
Introduction
Multiple myeloma causes up to 16,000 deaths per year, and 12,000 in the USA.1 For approximately 50 years, the combination of melphalan with prednisone was the reference therapy for elderly patients with multiple myeloma.2,3 Recently, however, the addition of thalidomide or bortezomib or lenalidomide to the standard melphalan plus prednisone combination has changed the treatment paradigm for elderly patients with multiple myeloma.4–12 In five independent, randomized studies, response rates and progression-free survival were significantly better in patients treated with the combination of melphalan, prednisone and thalidomide than in those given melphalan and prednisone.4–9 In a phase III study, a four-drug combination, bortezomib-melphalan-prednisone-thalidomide, doubled the complete response rate in comparison to that achieved with bortezomib-melphalan-prednisone alone.10 Other agents may potentially enhance the therapeutic index of the melphalan, prednisone and thalidomide combination.
Defibrotide is a polydeoxyribonucleic acid derivative13 which targets endothelial cell damage and is used for the treatment of various vascular disorders.14,15 In vitro data indicate that it may have anti-myeloma activity, especially in combination with other anti-neoplastic drugs; it markedly sensitizes multiple myeloma cells to cytotoxic agents and overcomes resistance to chemotherapy.16,17 Defibrotide potently down-regulates heparanase, which is overexpressed in multiple myeloma plasma cells and is also correlated with progression and metastasis in solid tumors.18 Moreover, defibrotide counteracts the alterations of fibrinolytic factors in microvascular endothelial cells and may protect against thomboembolic events.19 The aim of this phase I/II study was to identify the most appropriate dose of defibrotide in combination with melphalan, prednisone and thalidomide in patients with relapsed or relapsed/refractory multiple myeloma, and to determine its safety and tolerability as part of this regimen.
Design and Methods
Patients
From March through November 2006, 24 patients with multiple myeloma were enrolled. Inclusion criteria were: relapsed or relapsed and refractory disease after at least one or two lines of therapy, measurable disease, platelet count of 90×109/L or greater, absolute neutrophil count of 1×109/L or greater, corrected serum calcium 3.5 mmol/L or less, serum hepatic aminotransferase levels 2.5-fold or less, of upper limit of normal, total bilirubin 1.5-fold or less of the upper limit of normal, and creatinine clearance of 20 mL/min or greater. Patients agreed to use contraception. The institutional review board at each participating center approved the study and all patients provided written informed consent.
Study design and Treatment
This was a phase I/II, multicenter, dose-escalating, non-comparative, open label study. Oral melphalan was administered at the dose of 0.25 mg/kg on days 1 to 4, prednisone at the dose of 1.5 mg/kg on days 1 to 4, and thalidomide at doses ranging from 50 to 100 mg/day continuously on days 1–35. Defibrotide (PROCICLIDE Gentium S.p.A.) was administered either intravenously (i.v.) or orally (p.o.) on days 1 to 4 and orally on days 5 to 35 for six cycles. Three different dose levels of defibrotide were tested. Dose level 1 was 17 mg/Kg i.v. or 2.4 g p.o. on days 1 to 4, followed by 1.6 g p.o. on days 5 to 35. Dose level 2 was 34 mg/Kg i.v. or 4.8 g p.o. on days 1 to 4, followed by 3.2 g p.o. on days 5 to 35. Dose level 3 was 51 mg/Kg i.v. or 7.2 g p.o. on days 1 to 4, followed by 4.8 g p.o. on days 5 to 35. For each dose-level, the first two patients enrolled in the study received defibrotide i.v. on days 1 to 4; all the others then received defibrotide orally. After induction, patients received maintenance therapy including oral defibrotide (1.2 g/day) and thalidomide (50 mg/day) continuously until disease progression, or any unacceptable toxicity. All patients received antibiotic prophylaxis, but no other anti-thrombotic pro-phylaxis was administered.
Occurrence of grade 4 hematologic toxicities (except neutropenia), grade 4 neutropenia for 7 days or more or any non-hematologic toxicities of grade 3 or more were defined dose-limiting toxicity.
Efficacy and safety
Efficacy was assessed after each induction cycle and every 6–8 weeks thereafter utilizing EBMT criteria and International Myeloma Working Group criteria to assess very good partial response.20,21 Toxicities were estimated weekly during the first three cycles of treatment, every 15 days during the last three cycles, and every 6–8 weeks during maintenance.
Progression-free survival was calculated from the time of enrollment to the date of progression, relapse, death or when the patient was last seen in remission. Overall survival was estimated from the date of enrollment to the date of death or the date when the patient was last known to be alive. All adverse events were graded according to the National Cancer Institute Common Toxicity Criteria (version 3.0).22
End-points and statistical analysis
The primary safety end-points were to define dose-limiting toxicities, which included febrile neutropenia, or grade 4 hematologic toxicities with neutropenia for 7 days or more, or any grade 3 non-hematologic toxicity in more than 30% of patients during the first cycle of therapy. The maximum tolerated dose was then defined as the dose level prior to that resulting in dose-limiting toxicity. The primary efficacy end-point was a minimal response rate of 55% or better. Secondary efficacy end-points included progression-free survival and overall survival. All patients meeting eligibility criteria who completed the first cycle of therapy were evaluated for response, toxicity and survival. The time-to-event analysis was conducted using the Kaplan-Meier method,23 with computations performed by STATGRAPHICS, Centurion software, version 15.2.14 (Statpoint Technologies, Inc.).
Results
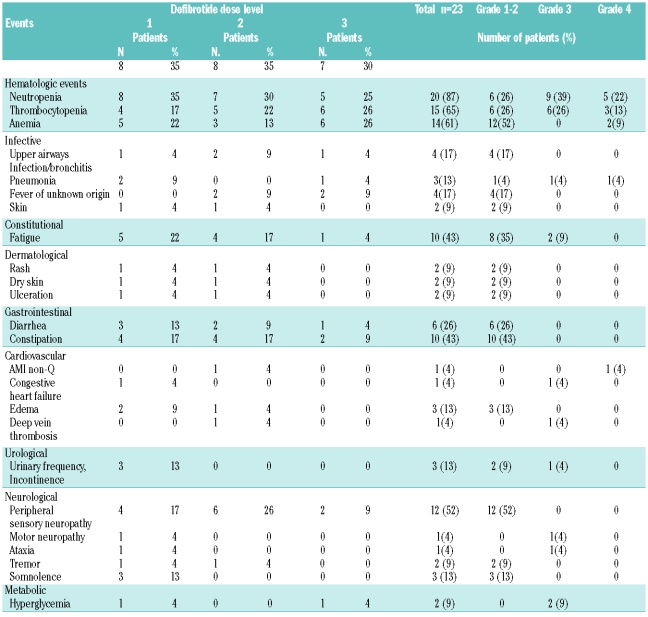
The patients’ characteristics are shown in Table 1. As regards prior therapies, 48% of patients underwent stem cell transplantation, and another 48% were treated with conventional chemotherapy. One patient developed rapidly progressive disease at the time he entered the study, causing his death before the end of the first cycle, and precluding evaluation. The remaining 23 patients were evaluable for safety and efficacy.
Table 1.
Patients’ characteristics.
At dose levels 1, 2 and 3 of defibrotide, no dose-limiting toxicity was observed during the first cycle. At dose level 1, one patient developed grade 3 congestive heart disease (cycle 1), grade 3 fatigue, ataxia and motor neuropathy (cycle 2), and grade 3 interstitial pneumonia (cycle 6), all of which were considered unrelated to defibrotide; one patient experienced grade 4 neutropenia (cycle 1). At dose level 2, three patients experienced grade 4 neutropenia (cycles 1–2), and one had a grade 4 cardiologic adverse event (non-Q acute myocardial infarction) (cycle 1), also considered unrelated to defibrotide. At dose level 3, one patient required a delay in treatment administration because of persistent neutropenia, and one patient developed progressive disease (cycle 1). Dose level 3 of defibrotide was, therefore, defined as the maximum tolerated dose.
At the time of analysis, all patients had completed the assigned treatment period; 12 of the 23 patients did not complete the assigned six cycles because of progressive disease or non-response to treatment (10 patients), an adverse event (1 patient; grade 4 cardiac ischemic episode), or intercurrent illness (1 patient; concomitant anaplastic astrocytoma). Two patients completed the assigned six cycles of treatment, but did not start the maintenance therapy because of progressive disease (1 patient) and the episode of unrelated grade 3 congestive heart disease plus interstitial pneumonia described above (1 patient).
Efficacy
The overall response rate in the whole group of patients was 52%, including partial response and complete plus very good partial response rates of 43% and 9%, respectively. Twenty-two percent of the patients had a minimal response, another 22% had no response and disease progression occurred in the remaining 4%. In 90% of the responding patients, a partial response occurred within the first two cycles (69% after the first cycle and 22% after the second). The median time from diagnosis to study entry was 52 months. The median duration of follow-up from study entry was 30 months (range, 26–34 months). The 1-year progression-free survival was 34%, with a median of 10 months (Figure 1A). From time of enrollment in the study, the 1-year overall survival rate among all patients was 90%, with a median of 29 months (Figure 1B). The median progression-free survival was 17 months in patients who achieved a complete or very good partial response, and 11 months in those who achieved only a partial response.
Figure 1.
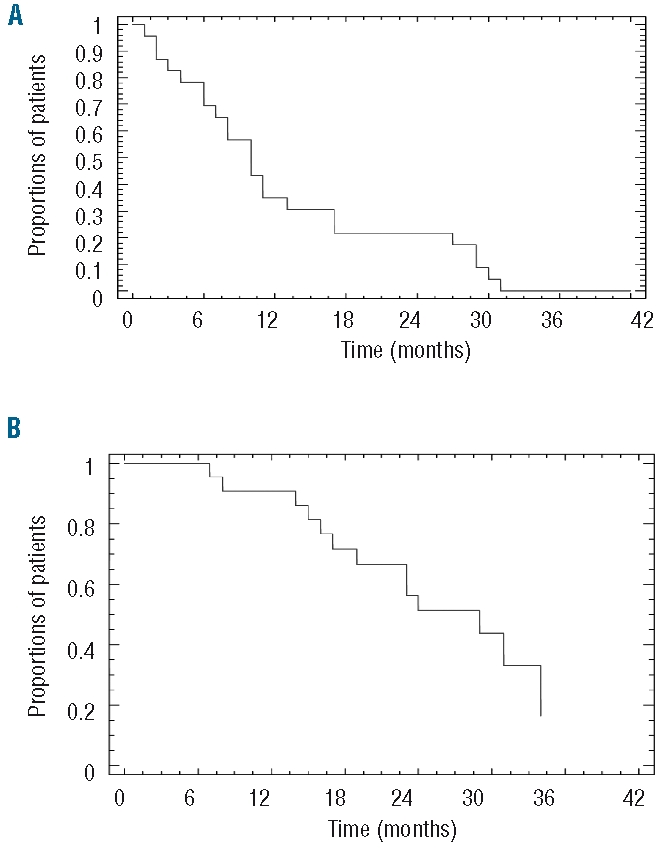
(A) Progression-free survival. (B) Overall survival.
Safety
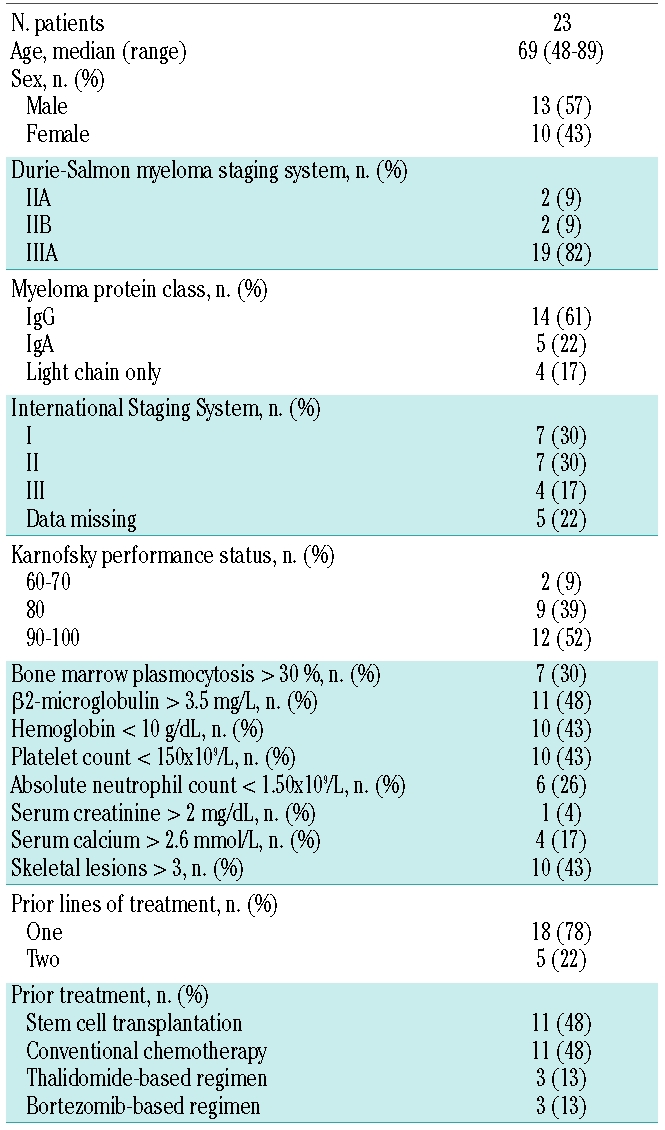
No deaths were reported to have occurred as a consequence of adverse events. The most frequent hematologic grade 3–4 toxicities were neutropenia (61%) and thrombocytopenia (39%). Granulocyte colony-stimulating factor support was required in nine patients, recombinant human erythropoietin support in three patients, concentrated red blood cell transfusion in three patients and platelet transfusion in two patients. The most common non-hematologic grade 3–4 adverse events included fatigue, which occurred in two patients, and hyperglycemia, experienced by another two patients and attributed to glucocorticoids. Gastrointestinal adverse events and peripheral neuropathy were manageable with thalidomide dose modification, and no grade 3 peripheral neuropathy was seen. No thromboembolic prophylaxis was administered in this study, and just one deep vein thrombosis was reported during the fifth cycle (for an overall deep vein thrombosis rate of 4%). No major bleeding occurred, and only one episode of minor bleeding (hematoma of the arm) was reported (Table 2). The dose of melphalan was reduced in two patients (9%) because of grade 3 neutropenia and thrombocytopenia; the dose of thalidomide was halved in five patients (22%) due to constipation, tremor, paresthesia, hypoesthesia, somnolence, confusion, bradycardia, or pneumonia. Ataxia, motor neuropathy, and fatigue led to the discontinuation of thalidomide in one patient. Defibrotide was never discontinued, and the dose was reduced in only one patient because of the grade 2 hematoma described above.
Table 2.
Adverse events.
Discussion
In this phase I/II study, we evaluated dosing, safety and efficacy of the combination of melphalan, prednisone, thalidomide and defibrotide in patients with advanced multiple myeloma. The maximum tolerated dose of defibrotide was defined as 7.2 g p.o. on days 1–4 followed by 4.8 g p.o. on days 5–35.
The combination of melphalan, prednisone and thalidomide was proven to be superior to the combination of melphalan and prednisone in several independent randomized trials.4–9 The melphalan, prednisone and thalidomide combination was also found to be effective in relapsed/refractory patients.25 The addition of bortezomib to the melphalan and prednisone regimen gave clearly better results than the melphalan and prednisone combination alone.12 Furthermore, the four-drug combination bortezomib, melphalan, prednisone and thalidomide produced significantly higher response rates compared to those of the three-drug bortezomib, melphalan and prednisone regimen.10,26 However, toxicity and in particular deep vein thrombosis and peripheral neuropathy are major limitations of these regimens. This provided the clinical rationale for investigating the consolidated melphalan, prednisone and thalidomide regimen in combination with a fourth novel agent such as defibrotide.
In our study, the complete plus very good partial response rate was 9% and 52% of the series achieved a partial response or better. While the very good partial response rate in this study is lower than the 59% very good partial response rate observed with the bortezomib, melphalan, prednisone and thalidomide regimen, the median progression-free survival of our patients was 10 months, with a comparable progression-free survival at 1 year of 61% in patients treated with bortezomib, melphalan, prednisone and thalidomide,26 and a median progression-free survival of 9 months reported in a similar study evaluating a combination of bortezomib, melphalan, dexamethasone and thalidomide.24
The main goals of this study were to determine response rates, define the maximum tolerated dose of defibrotide and reduce toxicity. In this regard, the low rate of deep vein thrombosis, absence of significant peripheral neuropathy and clinical benefit seen with this combination are encouraging. Further phase II studies will now be needed to better define the combination’s efficacy in larger numbers of patients treated at the maximum tolerated dose. Severe myelosuppression was observed in 50% of patients, and infection occurred in 9% of patients. Neutropenia was the most common adverse event, with thrombocytopenia being less common. Severe non-hematologic side effects were rare, except grade 1/2 fatigue and hyperglycemia in 9% of patients. These results compare favorably with those of two other studies of combinations including bortezomib, melphalan, thalidomide, and corticosteroids, in which the incidence of infection was 7% and 15% and significant peripheral neuropathy developed in at least 6% and 10% of patients, respectively.24,26 Of note, Echart et al. suggested a potential role of defibrotide for the prevention of deep vein thrombosis specifically induced by thalidomide.19 In our study, no anti-thrombotic prophylaxis was administered and the incidence of deep vein thrombosis was only 4%. By comparison, deep vein thrombosis occurred in about 10% of patients receiving melphalan, prednisone and thalidomide, despite the use of enoxaparin as anticoagulant prophylaxis.8 These data, therefore, suggest a protective activity of defibrotide against thrombotic events, and support future trials of defibrotide in combination with thalidomide or other immunomodulatory drugs, such as lenalidomide and pomalidomide.
In conclusion, treatment with defibrotide in combination with melphalan, prednisone and thalidomide was associated with a low incidence of severe adverse events. In the light of the ability of defibrotide to modulate endothelial cell injury and thereby enhance sensitivity to chemotherapy, further studies are warranted to assess whether defibrotide can augment the cytotoxicity of melphalan, prednisone and thalidomide in multiple myeloma, while decreasing the risk of thrombosis.
Acknowledgments
we are very grateful to the nurses and medical staff who cared for the patients and to the study coordinators who collected the trial and follow-up data. We are especially grateful to the patients and their families for their participation.
Footnotes
AP has received honoraria from and serves on advisory committees for Celgene and Janssen-Cilag; FG and FC have received honoraria from Celgene; SB has received honoraria from Celgene and Janssen-Cilag; MI serves as scientific director for Gentium; KA was a member of Gentium’s Board of Directors until August 2009; MB has received research support from and serves as a consultant on scientific advisory boards for Celgene and Janssen-Cilag; PR has received honoraria for serving on Gentium’s advisory committees.
Authorship and Disclosures
AP wrote the paper; AP, CM, KA, MB, and PR designed the study, supervised its conduct and data analysis, edited the paper and provided final approval for the manuscript; AL, MG, KK, CR, FG, PF, VM, and FC participated in designing research and the protocol, collected and verified data, and assisted in drafting the manuscript; DR, GB, LM, MI, and GG provided material or patients for the study, and reviewed the manuscript.
All the remaining authors declare they have no competing financial interests relevant to this study.
References
- 1.Ferlay J, Bray F, Pisani P, Parkin DM. GLOBOCAN 2002: cancer incidence, mortality and prelevance worldwide. Lyon. France: GLOBOCAN; 2004. [Google Scholar]
- 2.Cavo M, Benni M, Ronconi S, Fiacchini M, Gozzetti A, Zamagni E, et al. Melphalanprednisone versus alternating combination VAD/MP or VND/MP as primary therapy for multiple myeloma: Final analysis of a randomized clinical study. Haematologica. 2002;87(9):934–42. [PubMed] [Google Scholar]
- 3.Myeloma Trialists’ Collaborative Group. Combination chemotherapy versus melphalan and prednisone as treatment of multiple myeloma: An overview of 6,633 patients from 27 randomized trials. J Clin Oncol. 1998;16(12):3832–42. doi: 10.1200/JCO.1998.16.12.3832. [DOI] [PubMed] [Google Scholar]
- 4.Palumbo A, Bringhen S, Liberati AM, Caravita T, Falcone A, Callea V, et al. Oral melphalan, prednisone, and thalidomide in elderly patients with multiple myeloma: updated results of a randomized controlled trial. Blood. 2008;112(8):3107–14. doi: 10.1182/blood-2008-04-149427. [DOI] [PubMed] [Google Scholar]
- 5.uldbrandsen N, Waage A, Gismin P, Turesson I, Juliusson G, Abildgaard N, et al. A randomised placebo controlled study with melphalan/prednisone vs melphalan/prednisone/thalidomide: quality of life and toxicity [abstract] Haematologica. 2008;93:0209. [Google Scholar]
- 6.Wijermans P, Schaafsma M, van Norden Y, Ammerlaan R, Wittebol S, Sinnige H, et al. Melphalan + prednisone versus melphalan + prednisone + thalidomide in induction therapy for multiple myeloma in elderly patients: final analysis of the Dutch Cooperative Group HOVON 49 study [abstract] Blood. 2008;112:649. [Google Scholar]
- 7.Hulin C, Facon T, Rodon P, Pegourie B, Benboubker L, Doyen C, et al. Efficacy of melphalan and prednisone plus thalidomide in patients older than 75 years with newly diagnosed multiple myeloma: IFM 01/01 trial. J Clin Oncol. 2009;27(22):3664–70. doi: 10.1200/JCO.2008.21.0948. [DOI] [PubMed] [Google Scholar]
- 8.Palumbo A, Bringhen S, Caravita T, Merla E, Capparella V, Callea V, et al. Oral melphalan and prednisone chemotherapy plus thalidomide compared with melphalan and prednisone alone in elderly patients with multiple myeloma. Randomised controlled trial. Lancet. 2006;367(9513):825–831. doi: 10.1016/S0140-6736(06)68338-4. [DOI] [PubMed] [Google Scholar]
- 9.Facon T, Mary JY, Harousseau JL, Benboubker L, Attal M, Pegourie B, et al. Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99–06): a randomised trial. Lancet. 2007;370(9594):1209–18. doi: 10.1016/S0140-6736(07)61537-2. [DOI] [PubMed] [Google Scholar]
- 10.Palumbo A, Bringhen S, Rossi D, Magarotto V, Di Raimondo F, Ria R, et al. A Prospective, randomized phase III study of bortezomib, melphalan, prednisone and thalidomide (VMPT) versus bortezomib, melphalan and prednisone (VMP) in elderly newly diagnosed myeloma patients. Blood. Abstract. 2008;112652 [Google Scholar]
- 11.Palumbo A, Falco P, Corradini P, Falcone A, Di Raimondo F, Giuliani N, et al. Melphalan, prednisone, and lenalidomide treatment for newly diagnosed myeloma: a report from the GIMEMA-Italian Multiple Myeloma Network. J Clin Oncol. 2007;25(28):4459–65. doi: 10.1200/JCO.2007.12.3463. [DOI] [PubMed] [Google Scholar]
- 12.San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M, et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Eng J Med. 2008;359(9):906–17. doi: 10.1056/NEJMoa0801479. [DOI] [PubMed] [Google Scholar]
- 13.Coccheri S, Biagi G. Defibrotide. Cardiovascular Drug Reviews. 1991;9(2):172–96. [Google Scholar]
- 14.Palmer KJ, Goa KL. Defibrotide. A review of its pharmacodynamic and pharmacokinetic properties, and therapeutic use in vascular disorders. Drugs. 1993;45(2):259–94. doi: 10.2165/00003495-199345020-00007. [DOI] [PubMed] [Google Scholar]
- 15.Falanga A, Vignoli A, Marchetti M, Barbul T. Defibrotide reduces procoagulant activity and increases fibrinolytic properties in endothelial cells. Leukemia. 2003;17(8):1636–42. doi: 10.1038/sj.leu.2403004. [DOI] [PubMed] [Google Scholar]
- 16.Koehl GE, Geissler EK, Iacobelli M, Frei C, Burger V, Haffner S, et al. Defibrotide: an endothelium protecting and stabilizing drug, has an angiogenic potential in vitro and in vivo. Cancer Biol Ther. 2007;6(5):686–90. doi: 10.4161/cbt.6.5.3959. [DOI] [PubMed] [Google Scholar]
- 17.Mitsiades CS, Rouleau C, Menon K, Teicher B, Iacobelli M, Anderson KC, et al. Defibrotide targets tumor microenviromental interaction and sensitizes multiple myeloma and solid tumor cells to cytotoxic chemotherapy. Blood. Abstract. 2004;104286 [Google Scholar]
- 18.Echart C, Distaso M, Ferro L, Palumbo A, Mitsiades C, Anderson K, et al. Defibrotide induces downregulation of heparenase expression in multiple myeloma cell lines: a novel mechanism of action. Haematologica. 2007;92 (S2):146. [Google Scholar]
- 19.Echart C, Graziadio B, Repice C, Boccadoro M, Palumbo A, Mitsiades C, et al. Defibrotide counteracts the modifications of anti-thrombotic phenotype of endothelial cells induced by thalidomide. Blood. Abstract. 2007;1102502 [Google Scholar]
- 20.Blade J, Samson D, Reece D, Apperley J, Björkstrand B, Gahrton G, et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haematopoietic stem cell transplantation. Br J Haematol. 1998;102(5):1115–23. doi: 10.1046/j.1365-2141.1998.00930.x. [DOI] [PubMed] [Google Scholar]
- 21.Durie BG, Harousseau JL, Miguel JS, Bladé J, Barlogie B, Anderson K, et al. International uniform criteria for multiple myeloma. Leukemia. 2006;20(9):1467–73. doi: 10.1038/sj.leu.2404284. [DOI] [PubMed] [Google Scholar]
- 22.Cancer Therapy Evaluation Program. Common terminology criteria for adverse events, version 3.0.DCTD, NCI, NIH, DHHS. Mar 31, 2003. http://ctep.cancer.gov.
- 23.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–81. [Google Scholar]
- 24.Terpos E, Kastritis E, Roussou M, Heath D, Christoulas D, Anagnostopoulos N, et al. The combination of bortezomib, melphalan, dexamethasone and intermittent thalidomide is an effective regimen for relapsed/refractory myeloma and is associated with improvement of abnormal bone metabolism and angiogenesis. Leukemia. 2008;22(12):2247–56. doi: 10.1038/leu.2008.235. [DOI] [PubMed] [Google Scholar]
- 25.Palumbo A, Avonto I, Bruno B, Ambrosini MT, Bringhen S, Cavallo F, et al. Intravenous melphalan, thalidomide and prednisone in refractory and relapsed multiple myeloma. Eur J Haematol. 2006;76(4):273–7. doi: 10.1111/j.1600-0609.2005.00610.x. [DOI] [PubMed] [Google Scholar]
- 26.Palumbo A, Ambrosini MT, Benevolo G, Pregno P, Pescosta N, Callea V, et al. Bortezomib, melphalan, prednisone, and thalidomide for relapsed multiple myeloma. Blood. 2007;109(7):2767–72. doi: 10.1182/blood-2006-08-042275. [DOI] [PubMed] [Google Scholar]