Recent investigations in chronic lymphocytic leukemia (CLL) have correlated the mutational status of immunoglobulin heavy-chain variable-region (IgVH) gene to the development of secondary immune thrombocytopenia, the risk being higher for unmutated cases.1,2 A similar association between autoimmune hemolytic anemia (AHA) and IgVH gene status has not yet been defined. Therefore, whereas it is well known that the prevalence of autoimmune hemolytic anemia is highest in the more advanced stages of the disease,3 and may depend on the type of treatment administered,4,5 the impact of this autoimmune complication on the outcome of patients with chronic lymphocytic leukemia remains controversial.4–7
To address this, we searched our database of 473 chronic lymphocytic leukemia patients consecutively referred to our Department from 1st January 2000 to 1st January 2009. We identified 35 chronic lymphocytic leukemia patients (7%) who developed overt autoimmune hemolytic anemia. All patients met the chronic lymphocytic leukemia diagnostic criteria of the National Cancer Institute. Autoimmune hemolytic anemia was defined with standard criteria: a fall in hemoglobin level of at least 2 g/dL, associated with a positive direct antiglobulin test and/or increased reticulocyte count, and a rise in indirect bilirubin with no other causes of anemia identified.
As part of the diagnostic work-up, IgVH DNA sequence analysis was performed on peripheral blood or bone marrow specimens of all the 238 consecutive chronic lymphocytic leukemia patients diagnosed at our Institution since June 2004. Mutational status was obtained retrospectively, using the samples collected at diagnosis, in 12 of the 35 cases of chronic lymphocytic leukemia with autoimmune hemolytic anemia occurring before June 2004. Sequences were aligned to IMGT and V-BASE directories and analyzed using DNAPLOT and IMGT/VQUEST software. Those differing more than 2% from the corresponding germ-line gene were considered mutated.
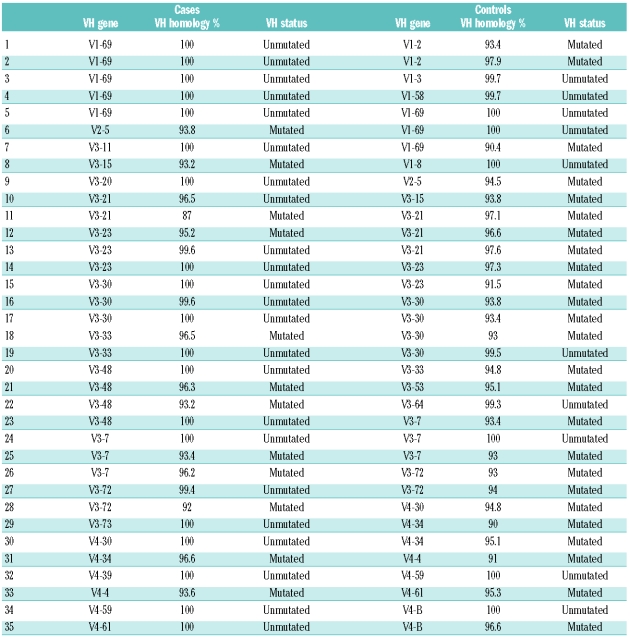
Median follow-up from diagnosis of chronic lymphocytic leukemia was 66 months (range 6–118). All patients with autoimmune hemolytic anemia except 2 presented with RAI stage 0 or 1, and developed autoimmune hemolytic anemia in a median time of 48 months (range 0–102), all requiring specific therapy for the anemia. In order to avoid possible confounding effects due to patient selection in determining the association between occurrence of autoimmune hemolytic anemia and IgVH status, we performed a case-control study comparing the 35 patients with chronic lymphocytic leukemia and autoimmune hemolytic anemia (cases) with 35 chronic lymphocytic leukemia patients without autoimmune hemolytic anemia (controls). Cases and controls were matched for gender, age (± 2 years) and RAI stage at diagnosis, year of diagnosis, and length of follow-up to adjust for the time at risk of developing autoimmune hemolytic anemia. A higher prevalence of un-mutated IgVH was found in patients with autoimmune hemolytic anemia (23 of 35, 66%). In comparison only 10 of 35 (28%) controls showed un-mutated IgVH, as expected in an unselected cohort.8 The odds ratio of developing autoimmune hemolytic anemia in un-mutated chronic lymphocytic leukemia could be estimated as 4.79 (95% CI 1.74–13.18, P=0.001 by Fisher’s exact test). No significant difference was observed in VH family distribution between the two groups, with VH3 family being the most represented among patients with autoimmune hemolytic anemia (66%; Table 1).
Table 1.
IgVH mutational status in cases (CLL with AHA) and controls (CLL without AHA)
Considering all chronic lymphocytic leukemia patients in our series, overall survival (OS) was similar in patients with or without autoimmune hemolytic anemia (5-year OS 70% vs. 80%, respectively, P=0.46) despite the association of autoimmune hemolytic anemia with un-mutated IgVH and the overall adverse impact of un-mutated IgVH on overall survival in our series. Of note, autoimmune hemolytic anemia developed significantly earlier in the course of chronic lymphocytic leukemia in patients with un-mutated IgVH compared to mutated patients (39 vs. 59 months, respectively, P=0.04). Patients developing autoimmune hemolytic anemia within 48 months (early AHA) after chronic lymphocytic leukemia diagnosis (16 patients, 81% un-mutated) had a significantly inferior overall survival compared to patients developing autoimmune hemolytic anemia later in the course of the disease (47% vs. 94%, P=0.0001) or without autoimmune hemolytic anemia (47% vs. 81%, P=0.0008).
In summary, our data show that autoimmune hemolytic anemia is associated with un-mutated status in chronic lymphocytic leukemia patients and that patients with early onset of autoimmune hemolytic anemia have a shorter survival. Similar observations have been reported in patients developing secondary immune thrombocytopenia in the course of chronic lymphocytic leukemia, where time to immune thrombocytopenia development was also associated with overall survival.9 The poorer outcome of patients with autoimmune complications arising early in the course of chronic lymphocytic leukemia might depend on the association with un-mutated status but also on the increased morbidity and mortality due to immunosuppressive treatments required for treating autoimmunity. Larger prospective cohorts are needed in order to verify this observation, and to tell us whether the association is directly causal or whether it reflects an increased tumor bulk at the time of autoimmune hemolytic anemia development.
Footnotes
Funding:this work was supported in part by grants from AViLL/AIL (Associazione Vicentina per le Leucemie, i Linfomi e il Mieloma/Associazione Italiana Leucemie) (Vicenza, Italy); Fondazione Progetto Ematologia (Vicenza, Italy); and by the Regione Veneto, Italy, through the “Ricerca Sanitaria Finalizzata 2006” program.
References
- 1.Visco C, Giaretta I, Ruggeri M, Madeo D, Tosetto A, Rodeghiero F. Un-mutated IgVH in chronic lymphocytic leukemia is associated with a higher risk of immune thrombocytopenia. Leukemia. 2007;21(5):1092–3. doi: 10.1038/sj.leu.2404592. [DOI] [PubMed] [Google Scholar]
- 2.Visco C, Ruggeri M, Laura Evangelista M, Stasi R, Zanotti R, Giaretta I, et al. Impact of immune thrombocytopenia on the clinical course of chronic lymphocytic leukemia. Blood. 2008;111(3):1110–6. doi: 10.1182/blood-2007-09-111492. [DOI] [PubMed] [Google Scholar]
- 3.Hamblin TJ. Autoimmune complications of chronic lymphocytic leukemia. Semin Oncol. 2006;33(2):230–9. doi: 10.1053/j.seminoncol.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 4.Borthakur G, O’Brien S, Wierda WG, Thomas DA, Cortes JE, Giles FJ, et al. Immune anaemias in patients with chronic lymphocytic leukaemia treated with fludarabine, cyclophosphamide and rituximab--incidence and predictors. Br J Haematol. 2007;136(6):800–5. doi: 10.1111/j.1365-2141.2007.06513.x. [DOI] [PubMed] [Google Scholar]
- 5.Dearden C, Wade R, Else M, Richards S, Milligan D, Hamblin T, et al. The prognostic significance of a positive direct antiglobulin test in chronic lymphocytic leukemia: a beneficial effect of the combination of fludarabine and cyclophosphamide on the incidence of hemolytic anemia. Blood. 2008;111(4):1820–6. doi: 10.1182/blood-2007-07-101303. [DOI] [PubMed] [Google Scholar]
- 6.Mauro FR, Foa R, Cerretti R, Giannarelli D, Coluzzi S, Mandelli F, et al. Autoimmune hemolytic anemia in chronic lymphocytic leukemia: clinical, therapeutic, and prognostic features. Blood. 2000;95(9):2786–92. [PubMed] [Google Scholar]
- 7.Barcellini W, Capalbo S, Agostinelli RM, Mauro FR, Ambrosetti A, Calori R, et al. GIMEMA Chronic Lymphocytic Leukemia Group. Relationship between autoimmune phenomena and disease stage and therapy in B-cell chronic lymphocytic leukemia. Haematologica. 2006;91(12):1689–92. [PubMed] [Google Scholar]
- 8.Vasconcelos Y, Davi F, Levy V, Oppezzo P, Magnac C, Michel A, et al. Binet’s staging system and Vh genes are independent but complementary prognostic indicators in chronic lymphocytic leukemia. J Clin Oncol. 2003;21(21):3928–32. doi: 10.1200/JCO.2003.02.134. [DOI] [PubMed] [Google Scholar]
- 9.Visco C, Rodeghiero F. Immune thrombocytopenia in lymphoproliferative disorders. Hematol Oncol Clin North Am. 2009;23(6):1261–74. doi: 10.1016/j.hoc.2009.08.006. [DOI] [PubMed] [Google Scholar]