Abstract
Objective
Vertebral fractures (VFs) are frequently under-recognized, reflecting their lack of diagnostic clinical features. For example, although VFs are associated with back pain, this is also common in the general population. To establish whether back pain can be used to recognize patients with VF, we investigated the site of pain in people with and without VFs using a simple tool.
Methods
A cohort of 504 post-menopausal women was recruited from primary care in South West UK. Back pain was assessed by self-completion of the Margolis pain diagram, and analysis was modified to assess whether pain was mid-line or lateral. VFs were diagnosed by the algorithm-based qualitative method on radiographs. A cross-sectional analysis was carried out to assess the association between back pain and VFs.
Results
Three hundred and twenty-two women (64.1%) reported back pain over the last 12 months. Thirty seven (7.3%) had one or more VFs. In women with back pain, the presence of lateral waist area pain was associated with a 4.5-fold increased risk of VFs [odds ratio (OR) 4.48; 95% CI 2.02, 9.94; P<0.001].
Conclusions
In post-menopausal women with back pain, the presence of lateral waist pain, as shown on the Margolis pain diagram, may identify women at higher risk of prevalent VF.
Keywords: Back pain, Margolis pain diagram, Vertebral fractures
Introduction
Vertebral fractures (VFs) are common in post-menopausal women: data from the European Vertebral Osteoporosis Study (EVOS) suggest the prevalence is 12%, ranging from 6 to 21% according to age [1]. There are significant health-related implications of VF. People with VFs are at a high risk of further fractures if left untreated [2], and this is particularly true for multiple VFs, of whom one in four will experience a further VF over 5 years [3], and 9% will experience a limb fracture including hip fracture over 3 years [4]. Even single VFs are associated with a reduced quality of life [5]: a woman aged 65 years has been suggested to have a quality-adjusted life year of 0.70 [6], but this is reduced to 0.44 after a clinical VF, which is lower than that post-hip fracture (0.55) [7]. Radiographic vertebral deformity is also associated with a modest excess mortality, particularly in women, with a rate ratio of excess mortality of 1.9 after adjustment for age (95% CI 1.0, 3.4) [8].
Despite the importance of VFs, only a minority come to clinical attention. Precise figures are difficult to obtain, but it has been suggested that less than one-third are diagnosed and subsequently managed for osteoporosis [9]. However, if these undiagnosed women are prescribed bisphosphonates or other appropriate drugs, the expected osteoporotic fractures can be reduced by ~50% for repeat VFs [10] and 20–50% for non-VFs [11].
One of the major reasons for this diagnostic failure is that there is currently a lack of clear clinical triggers for referral for diagnostic spinal X-rays in patients with possible VFs. One of the main reasons for this is the high prevalence of back pain in the elderly population: ~30% of adults experience back pain at any one point [12]. Additionally, although it is known that women with multiple VFs have more back pain than those with only one VF [8], population-based work suggests that people with VFs have no more back pain than people without VFs [13]. What is not known fully is whether the quality, intensity or site of back pain in people with VFs is different from those with back pain but no VFs. This is an important question; if easily assessed characteristics such as the site of pain predict the likelihood of VFs, these could be used to differentiate between those with back pain who should go on to have a spinal X-ray and those who should not.
Previous investigators have considered the site of back pain and the relationship with VF: Roux et al. [14] found that thoracic localization of pain is associated with a 62% increased risk of VF [odds ratio (OR) 1.62; 95% CI 1.03, 2.56; P = 0.037]. However, the study population comprised 410 women with known osteoporosis, not the general population, and there would be a much lower threshold for referral for diagnostic spinal X-rays in this osteoporotic population. Back pain was defined quite crudely as either thoracic or lumbar pain on direct questioning of the study participants, and so repeatability and validity of this measure are questionable. More robust methods for collecting data on the site of back pain include the Margolis pain drawing in which the participant shades or marks the painful areas on a mannequin diagram [15] (Fig. 1).
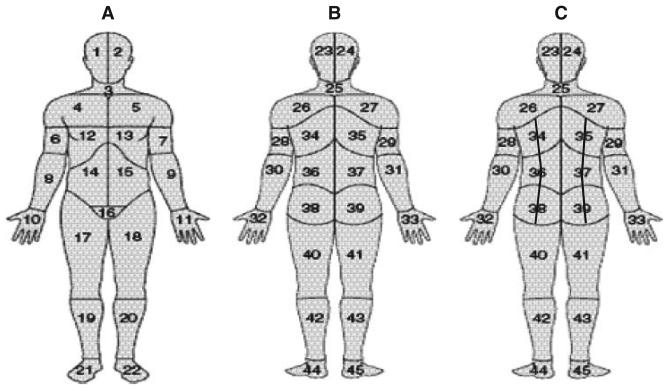
Fig. 1.
Diagrams showing the traditional Margolis pain drawing (A) from the front, (B) from the back and (C) the modified Margolis pain diagram used in this study.
However, the traditional Margolis pain diagram does not distinguish between mid-line and non-mid-line back pain. This may be particularly important for VF, as other investigators have shown that 70% of 288 patients presenting for percutaneous vertebroplasty to manage their back pain from VFs have non-mid-line pain [16]. Therefore, the aim of this study was to assess if more detailed analysis of the Margolis pain diagram, including assessment of site of pain, could be used to identify women with a higher risk of VF.
Materials and methods
We carried out a cross-sectional analysis of the association of back pain with VFs, using a cohort of post-menopausal women recruited from primary care. Patients were recruited by M.D.S., J.C.M., A.K.B. and J.H.T. Participants were assessed by A.P.H. and radiographs read by E.V.M. E.M.C. carried out the statistical analyses. All authors had full access to the data, and were independent of funders.
Study population
The population for this study was recruited during 2004–2005 from four General Practices located in Bristol, Bath, Cardiff and Glamorgan. All women aged 65 to 75 deemed suitable by their General Practitioner (GP) to be contacted (1518 in total), were invited to participate in a study designed to investigate the clinical risk factors that identify post-menopausal women with VFs. There were no exclusion criteria. Five hundred and forty women attended the assessment, and spinal radiographs were obtained in 509. This study population is described in detail elsewhere [17]. Written informed consent was obtained from all participants. Approval for this study was given by the Multi-Centre Research Ethics Committee (Ref. No. MREC/ 03/10/98).
Measurement of back pain
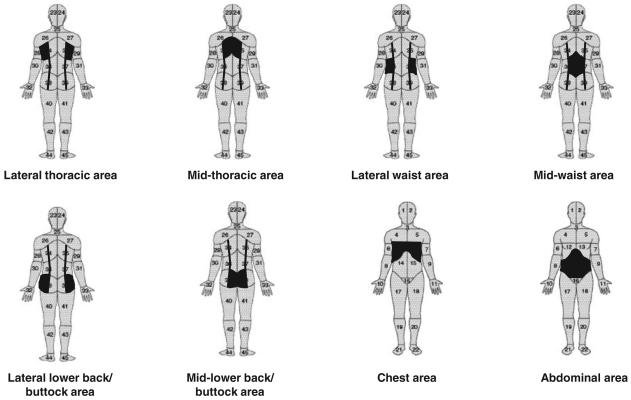
Back pain was assessed by self-completion of the Margolis pain drawing [15] during a face-to-face assessment with a research nurse (A.P.H.) before obtaining spinal radiographs. If a participant admitted to experiencing back pain over the past year, they were asked to shade or mark the sites of most recent back pain. The most recent episode of pain was chosen as it was felt this would be most easily remembered by the participant and, therefore, less likely to be influenced by recall bias. The pain drawings were then scored by a researcher (E.M.C.) who did not know the participant's fracture status. In addition to the traditional regions used on the original Margolis pain drawing (Fig. 1), three back areas (thoracic, waist and lower back/buttock) were sub-divided by a vertical line mid-way through each of these regions so that distinction could be made between lateral- and mid-back pain (Fig. 2). Weighted scores were not used; instead, it was noted for each participant whether or not they had pain in any of the nine areas of interest. These were lateral thoracic (either side), mid-thoracic (either side), lateral waist (either side), mid-waist (either side), lateral lower back/buttock (either side), mid-lower back/buttock (either side), chest (either side), abdomen (either side) and leg radiation (defined as any mark in any part of the 12 leg regions on either the front or back of the body).
Fig. 2.
Diagrams showing the modified Margolis pain with the specific areas of interest used in this study highlighted in black: the lateral thoracic, mid-thoracic, lateral waist, mid-waist, lateral lower back/buttock, mid-lower back/buttock, chest and abdominal areas.
Diagnosis of VF
Each participant attended their local hospital and had a lateral thoracic and lumbar spine radiograph obtained using a standardized protocol [1]. The radiographs were anonymized and sent to the University of Sheffield for reading by a researcher trained in the algorithm-based qualitative (ABQ) method [18]. With this method, evidence of a deformity of the vertebral endplate is taken as the primary indicator of an osteoporotic VF.
Other measures
During the face-to-face assessment carried out by a research nurse (A.P.H.), data comprising date of birth and recalled height at 25 years of age were collected. A clinical examination was performed and included measuring current height (without shoes using a wall-mounted stadiometer), current weight (static calibrated scales without shoes and heavy outdoor clothing), rib-to-pelvis distance (measured in finger-breadths as previously described [19]) and wall–tragus distance.
Statistical analysis
The presence or absence of VFs was the outcome of interest. The main exposure of interest was back pain. The proportion of participants with and without VFs who experienced particular areas of back pain was compared using chi-squared tests. Logistic regression was used to calculate ORs and 95% CIs for risk of VF for each area of back pain. ORs were used as the prevalence of VF in this population was <10%. For clarity and ease of understanding, the Results and Discussion use the word risk, but this reflects the OR. Multivariable logistic regression was used to adjust for potential confounders such as age and weight, and to assess the effect of height loss or reduced rib-to-pelvis distance. All statistics were carried out by E.M.C. using STATA 8.0.
Results
Five hundred and four women had full data and were used in this analysis. Mean age of the whole cohort was 69.6 (3.0) years; 37 women (7.3%) were diagnosed with one or more VFs using the ABQ method, 24 had one VF and 13 had more than one (range 2–13), with the majority of fractures occurring between T7 and L1 inclusive. As published previously [17], compared with women without VFs, women with one or more VFs were more likely to be older (70.7 vs 69.5 years; P = 0.02) and have reported more height loss since 25 years of age (3.5 vs 1.9 cm; P = 0.002) and have a reduced rib–pelvis distance (1.7 vs 1.9 fingers; P = 0.018). For a full description of the demographics of the women with and without VFs, see Table 1 in the original cohort description [17].
Table 1.
Site of back pain in women with and without VFs in the 504 women in this cohort
| No VF (n = 467), n (%) |
Any VF (n = 37), n (%) |
P-value for difference between none or any VF |
One VF (n = 24), n (%) |
More than one VF (n = 13), n (%) |
P-value for difference between one or more than one VF |
|
|---|---|---|---|---|---|---|
| Thoracic back pain (n = 77) | 66 (14.1) | 11 (29.7) | 0.011 | 4 (16.7) | 7 (53.9) | 0.018 |
| Mid-line only (n = 47) | 42 (9.0) | 5 (13.5) | 0.231 | 2 (8.3) | 3 (23.1) | 0.096 |
| Lateral only (n = 7) | 6 (1.3) | 1 (2.7) | 0.373 | 1 (4.2) | 0 | 0.586 |
| Both (n = 23) | 18 (3.9) | 5 (13.5) | 0.213 | 1 (4.2) | 5 (38.5) | 0.490 |
| Waist area back pain (n = 214) | 196 (42.0) | 18 (48.7) | 0.429 | 10 (42.7) | 8 (61.5) | 0.248 |
| Mid-line only (n = 156) | 151 (32.3) | 5 (13.5) | 0.135 | 2 (8.3) | 3 (23.1) | 0.155 |
| Lateral only (n = 13) | 8 (1.7) | 5 (13.5) | <0.001 | 2 (8.3) | 3 (23.1) | 0.155 |
| Both (n = 45) | 37 (7.9) | 8 (21.6) | <0.001 | 6 (25.0) | 2 (15.4) | 0.207 |
| Lower back/buttock back pain (n = 198) | 184 (39.4) | 14 (37.8) | 0.851 | 9 (37.5) | 5 (38.5) | 0.954 |
| Mid-line only (n = 91) | 86 (18.4) | 5 (13.5) | 0.508 | 2 (8.3) | 3 (23.1) | 0.295 |
| Lateral only (n = 28) | 27 (5.8) | 1 (2.7) | 0.439 | 1 (4.2) | 0 | 0.470 |
| Both (n = 79) | 71 (15.2) | 8 (21.6) | 0.257 | 6 (25.0) | 2 (15.4) | 0.207 |
| Anterior chest pain (n = 3) | 2 (0.4) | 1 (2.7) | 0.083 | 0 | 1 (7.7) | 0.168 |
| Abdominal pain (n = 18) | 17 (3.6) | 1 (2.7) | 0.767 | 0 | 1 (7.7) | 0.168 |
| Leg radiation (n = 83) | 77 (16.5) | 6 (16.2) | 0.966 | 3 (12.5) | 3 (23.1) | 0.405 |
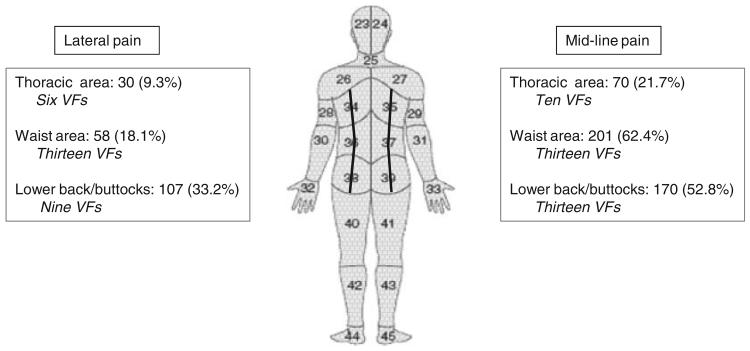
Three hundred and twenty-two women (64.1%) reported back pain over the past 12 months. Women with VFs tended to be more likely to report back pain over the past 12 months than those without VFs (78.4 vs 62.7%; P = 0.057), although 25% of women with one VF and 15.4% of women with more than one VF denied back pain over the previous year. As described in the Materials and methods section, we did not use the traditional Margolis score to describe back pain, instead simply noting whether women described pain in any of the 14 areas shown in Fig. 2. Seventy-seven women (23.9% of those with pain) reported pain in the thoracic area, 214 (66.5%) in the waist area and 198 (61.5%) in the lower back/buttock area; 83 women reported pain radiating down one or both legs, of whom 21 had thoracic pain, 52 waist pain and 63 lower back/buttock pain. Only three women reported anterior chest pain and 18 reported abdominal pain. Mid-line pain was more common than lateral pain (Fig. 3).
Fig. 3.
Distribution and pattern of back pain in the 322 women from this cohort according to whether the pain is lateral or mid-line. The Number of VFs identified in the corresponding areas is shown in italics.
In the whole cohort, those with any thoracic pain, lateral waist pain alone or lateral waist pain in combination with mid-waist area pain were more likely to have a VF than those women with pain elsewhere (Table 1). For the thoracic pain, this appeared to be more strongly associated with multiple VFs rather than single VFs.
Considering only those women who reported back pain (n = 322), the presence of lateral waist area pain on the modified Margolis pain diagram was associated with a 4.5-fold increased risk of VFs (OR 4.48; 95% CI 2.02, 9.94; P < 0.001). This association was not explained by age, weight, reported height loss, a reduced rib–pelvis distance or an increased wall–tragus distance (Table 2).
Table 2.
Association between site of back pain and presence of morphometric VF in 322 women
| No VF (n = 293), n (%) |
VF (n = 29), n (%) |
Crude OR (95% CI), P-value |
Adjusted (A) OR (95% CI), P-value |
Adjusted (B) OR (95% CI), P-value |
Adjusted (C) OR (95% CI), P-value |
Adjusted (D) OR (95% CI), P-value |
Adjusted (E) OR (95% CI), P-value |
|
|---|---|---|---|---|---|---|---|---|
| Presence of thoracic back pain | ||||||||
| No | 227 (77.5) | 18 (62.1) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 66 (22.5) | 11 (37.9) | 2.10 (0.95, 4.67), P = 0.068 | 1.96 (0.88, 4.39), P = 0.102 | 1.81 (0.80, 4.09), P = 0.156 | 1.89 (0.83, 4.28), P = 0.127 | 1.83 (0.81, 4.15), P = 0.419 | 1.88 (0.83, 4.22), P = 0.129 |
| Presence of lateral thoracic back pain | ||||||||
| No | 269 (91.8) | 23 (79.3) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 24 (8.2) | 6 (20.7) | 2.92 (1.09, 7.88), P = 0.034 | 2.65 (0.98, 7.21), P = 0.056 | 2.46 (0.90, 6.75), P = 0.080 | 2.70 (0.98, 7.48), P = 0.056 | 2.58 (0.95, 7.03), P = 0.064 | 2.64 (0.96, 7.26), P = 0.061 |
| Presence of mid-line thoracic back pain | ||||||||
| No | 233 (79.5) | 19 (65.5) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 60 (20.5) | 10 (34.5) | 2.04 (0.90, 4.63), P = 0.086 | 1.95 (0.86, 4.43), P = 0.111 | 1.80 (0.78, 4.15), P = 0.166 | 1.83 (0.79, 4.22), P = 0.157 | 1.81 (0.78, 4.19), P = 0.166 | 1.88 (0.82, 4.30), P = 0.137 |
| Presence of waist area pain | ||||||||
| No | 97 (33.1) | 11 (37.9) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 196 (66.9) | 18 (62.1) | 0.81 (0.37, 1.78), P = 0.600 | 0.86 (0.39, 1.91), P = 0.709 | 0.94 (0.42, 2.11), P = 0.875 | 0.91 (0.41, 2.05), P = 0.823 | 0.87 (0.39, 1.93), P = 0.734 | 0.82 (0.37, 1.83), P = 0.630 |
| Presence of lateral waist area pain | ||||||||
| No | 248 (84.6) | 16 (55.2) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 45 (15.4) | 13 (44.8) |
4.48 (2.02, 9.94), P<0.001 |
4.47 (2.00, 10.00), P<0.001 |
4.03 (1.79, 9.09), P = 0.001 |
5.07 (2.20, 11.69), P<0.001 |
4.40 (1.96, 9.98), P<0.001 |
4.25 (1.89, 9.59), P<0.001 |
| Presence of mid-line waist area pain | ||||||||
| No | 105 (35.8) | 16 (55.2) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 188 (64.2) | 13 (44.8) | 0.45 (0.21, 0.98), P = 0.044 | 0.48 (0.22, 1.03), P = 0.061 | 0.52 (0.24, 1.14), P = 0.103 | 0.50 (0.23, 1.11), P = 0.088 | 0.50 (0.23, 1.08), P = 0.078 | 0.47 (0.22, 1.03), P = 0.059 |
| Presence of lower back/buttock pain | ||||||||
| No | 109 (37.2) | 15 (51.7) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 184 (62.8) | 14 (48.3) | 0.55 (0.26, 1.19), P = 0.129 | 0.54 (0.25, 1.16), P = 0.115 | 0.58 (0.27, 1.27), P = 0.174 | 0.51 (0.24, 1.13), P = 0.097 | 0.54 (0.25, 1.16), P = 0.114 | 0.58 (0.27, 1.26), P = 0.168 |
| Presence of lateral lower back/buttock pain | ||||||||
| No | 195 (66.6) | 20 (69.0) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 98 (33.5) | 9 (31.0) | 0.90 (0.39, 2.04), P = 0.793 | 0.83 (0.36, 1.91), P = 0.666 | 0.85 (0.37, 1.97), P = 0.704 | 0.80 (0.34, 1.85), P = 0.597 | 0.84 (0.36, 1.94), P = 0.683 | 0.84 (0.36, 1.93), P = 0.674 |
| Presence of mid-line lower back/buttock pain | ||||||||
| No | 136 (46.4) | 16 (55.2) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 157 (53.6) | 13 (44.8) | 0.70 (0.33, 1.52), P = 0.369 | 0.70 (0.33, 1.52), P = 0.374 | 0.75 (0.34, 1.64), P = 0.472 | 0.67 (0.31, 1.48), P = 0.323 | 0.70 (0.32, 1.52), P = 0.370 | 0.78 (0.36, 1.71), P = 0.541 |
| Presence of leg radiation | ||||||||
| No | 216 (73.7) | 23 (79.3) | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 77 (26.3) | 6 (20.7) | 0.73 (0.29, 1.87), P = 0.513 | 0.71 (0.28, 1.81), P = 0.474 | 0.74 (0.28, 1.92), P = 0.529 | 0.65 (0.25, 1.69), P = 0.371 | 0.67 (0.26, 1.72), P = 0.403 | 0.70 (0.27, 1.79), P = 0.482 |
Results presented are crude ORs and 95% CIs and adjusted for A: age; B: age and current weight; C: age and reported height loss since 25 years of age; D: age and wall–tragus distance; E: age and rib–pelvis distance. Values in bold indicates statistically significant associations with P<0.05.
This gives the presence of lateral waist pain a sensitivity of 44.8% and a specificity of 84.6%, i.e. if an X-ray were performed in all women with lateral waist area pain, approximately one in four would have a VF identified, but half of all women with a VF would be missed. The presence of lateral thoracic area pain was also associated with an increased risk of VF (OR 2.92; 95% CI 1.09, 7.88; P = 0.034), although this appeared to be explained by age. Conversely, there was a suggestion that the presence of mid-line waist area pain detected women who were less likely to have a VF (OR 0.45; 95% CI 0.21, 0.98; P = 0.044). The point estimate for this association did not change after adjustment (Table 2), although this was no longer statistically significant. No other sites of pain predicted women with a higher or lower risk of VF. Leg radiation did not identify women at a lower risk of VF.
Discussion
This study shows that in post-menopausal women from primary care with back pain, the site of pain as assessed by novel analysis of the Margolis pain diagram may identify women with an increased risk of VF using the ABQ method. This is the first time the Margolis pain diagram has been interpreted in this way.
Our results confirm what is already well known: back pain is a predictor of new VF [20, 21]. However, our work extends this further and suggests that in women presenting with back pain to primary care, the presence of lateral waist pain may identify women at higher risk of VF. This novel analysis suggests that the routine use of this modified Margolis pain diagram, without any additional statistical analysis, may have a role during consultations in primary care for back pain in post-menopausal women—one of the most common reasons for a consultation with a GP in the UK [22]. It is likely that pain in the waist area rather than pain anywhere else, was associated with an increased risk of VFs because the transition from thoracic to lumbar vertebrae is the most common site for VFs [23].
Other risk factors have been used to predict prevalent VFs. The most widely studied is bone density, with many studies suggesting a 2-fold increase in VF incidence in women per S.D. decrease in BMD [24, 25]. VFs are also more common in women than men (relative risk 2.3; 95% CI 1.5, 3.6), although this is because at any given age their spine BMD is lower [26]. Perhaps the strongest independent predictor of a new VF is the presence of one or more previous VFs, which gives a 3- to 7-fold [3, 20, 25, 27] increased risk. Height loss of >2 cm has also been shown to increase the probability of VF 3-fold [20]. This suggests that our results of a 4.5-fold increase in risk of prevalent VF with the presence of lateral waist pain is likely to be clinically useful, as it gives a similar size effect to that seen with height loss or the presence of one or more previous VFs.
In addition, our finding that the association between lateral waist pain and VF is independent of other risk factors such as height loss or weight is consistent with the previous published work on this cohort that showed the conventional Margolis pain score to be independent of these risk factors [17]. This raises the prospect that combining the presence of lateral waist pain with other clinical risk factors for VF such as previous VF or height loss may improve predictive power.
However, further work needs to be done on the use of the modified Margolis pain diagram in clinical settings. We used the ABQ method to identify VFs, and this is not in common use in radiology departments for general reporting purposes—whether or not the presence of lateral waist area pain identified on the modified Margolis pain diagram identifies women with VFs diagnosed by reporting radiologists as part of routine clinical care is unknown. This highlights the current difficulty in identifying what is actually a VF on thoraco-lumbar radiographs. For research purposes, diagnosis of VFs on spinal radiographs initially consisted of quantitative or semi-quantitative methods based on definitions related to the percentage of vertebral height loss [28], but this approach may be over-sensitive in detecting minor vertebral deformities of limited clinical significance. More recent strategies have favoured qualitative definitions involving the detection of vertebral end-plate deformities, such as the ABQ method used in our study [18]. However, reporting radiologists in secondary care tend to use a wide range of experiential terms (e.g. height loss, end-plate abnormalities, wedge deformities, biconcave appearance, etc.), which can cause confusion as to whether a VF is present or not [29]. Until reporting is standardized and unambiguous, it may limit use of the modified Margolis pain diagram in routine back pain consultations.
Our study also highlights the difficulties of back pain as a clinical trigger for referral for diagnostic spinal X-ray: one-quarter of women with a VF did not report any back pain over the past 12 months. In addition, some of the women with VFs did not have lateral waist area pain. This agrees with the body of literature showing the complex relationship between back pain and VF. For example, one study has shown that 80% of the people with thoracic VFs localize their pain to the lumbar region only [30], and it is also well recognized that some VFs are not associated with any back pain [31]. An additional complicating feature is that the most common reason for back pain in the elderly is degenerative back disease, and many women with VFs will also have evidence of degeneration on X-ray. Teasing out which causes the back pain is currently not possible, and there is some evidence that spine degeneration causing disc space narrowing and osteophytes may be associated with a decreased VF prevalence [32].
Our work also suggests that the presence of mid-line waist area pain reduces the risk of VF, and that radiation of pain down the legs should not be used as a clue to the presence or absence of VF. This perhaps disagrees with current wisdom that suggests that pain radiating down the leg is likely to be associated with a reduced risk of VF: a description of pain published in 1991 of acute vertebral osteoporotic fractures in people presenting to secondary care that showed leg radiation was uncommon [33]. Limitations of our study may explain this discrepancy, although most VFs do not present acutely, and our study may be more representative of the actual burden of VFs in the community. Mid-line pain may identify women with degenerative spinal disease, and this is increasingly felt to be associated with a reduced risk of VF [32].
Potential limitations of our study include a small number of VFs, although this may be offset by the advantage of our population being recruited from primary care and therefore being somewhat representative of post-menopausal women consulting a GP for their back pain. The main reason for the small number of VFs is our use of the ABQ method of VF identification. This is advantageous, as ABQ is a much more specific method for VF identification than other methods more commonly employed, such as quantitative morphometry. As such, our results will be less likely to be biased by false positive VFs. In common with all observational studies, ours may suffer from bias and uncontrolled confounding, although we have attempted to minimize this by making sure the outcome (VF) was assessed by a trained researcher blinded to any participant details, and we adjusted for age in the regression analyses. The Margolis pain diagram was completed before radiographs were obtained, and the novel analysis was carried out by a researcher blinded to the participants' fracture status. The association found between the lateral waist area pain and risk of VF may have occurred by chance, and this finding requires repeating in other populations.
Thus in conclusion, we have shown that in post-menopausal women with back pain, the presence of lateral waist pain as shown on the modified Margolis diagram may identify women at higher risk of VF. The presence of lateral waist pain could be used to differentiate which women should be referred for diagnostic spinal X-ray, although the current non-standardized and often ambiguous reporting of VFs in secondary care may limit application of our results at present.
Rheumatology key message.
• Lateral waist pain may identify post-menopausal women at higher risk of prevalent vertebral fracture.
Acknowledgements
Funding: This work was supported by an unrestricted research grant from Procter and Gamble. This grant covered running expenses and salary costs for Alison Hutchinson during data collection and original analyses. Emma Clark is a Clinician Scientist Fellow funded by the Arthritis Research Campaign (ARC).
Footnotes
Disclosure statement: J.C.M. has received honoraria from Roche, Eli Lilly, Servier and Amgen. All other authors have declared no conflicts of interest.
References
- 1.O'Neill TW, Felsenberg D, Varlow J, et al. The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res. 1996;11:1010–8. doi: 10.1002/jbmr.5650110719. [DOI] [PubMed] [Google Scholar]
- 2.Klotzbuecher CM, Ross PD, Landsman PB, et al. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res. 2000;15:721–39. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 3.Kaptoge S, Armbrecht G, Felsenberg D, et al. When should the doctor order a spine X-ray? Identifying vertebral fractures for osteoporosis care: results from the European Prospective Osteoporosis Study (EPOS) J Bone Miner Res. 2004;19:1982–93. doi: 10.1359/JBMR.040901. [DOI] [PubMed] [Google Scholar]
- 4.Ismail AA, Cockerill W, Cooper C, et al. Prevalent vertebral deformity predicts incident hip though not distal forearm fracture: results from the European Prospective Osteoporosis Study. Osteoporos Int. 2001;12:85–90. doi: 10.1007/s001980170138. [DOI] [PubMed] [Google Scholar]
- 5.Oleksik A, Lips P, Dawson A, et al. Health-related quality of life in postmenopausal women with low BMD with or without prevalent vertebral fractures. J Bone Miner Res. 2000;15:1384–92. doi: 10.1359/jbmr.2000.15.7.1384. [DOI] [PubMed] [Google Scholar]
- 6.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997;35:1095–108. doi: 10.1097/00005650-199711000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Kanis JA, Johnell O, Oden A, et al. The risk and burden of vertebral fractures in Sweden. Osteoporos Int. 2004;15:20–6. doi: 10.1007/s00198-003-1463-7. [DOI] [PubMed] [Google Scholar]
- 8.Ismail AA, O'Neill TW, Cooper C, et al. Mortality associated with vertebral deformity in men and women: results from the European Prospective Osteoporosis Study (EPOS) Osteoporos Int. 1998;8:291–7. doi: 10.1007/s001980050067. [DOI] [PubMed] [Google Scholar]
- 9.Fink HA, Milavetz DL, Palermo L, et al. What proportion of incident radiographic vertebral deformities is clinically diagnosed and vice versa? J Bone Miner Res. 2005;20:1216–22. doi: 10.1359/JBMR.050314. [DOI] [PubMed] [Google Scholar]
- 10.Watts NB, Josse RG, Hamdy RC, et al. Risedronate prevents new vertebral fractures in postmenopausal women at high risk. J Clin Endocrinol Metab. 2003;88:542–9. doi: 10.1210/jc.2002-020400. [DOI] [PubMed] [Google Scholar]
- 11.Boonen S, Laan R, Barton I, et al. Effect of osteoporosis treatments on risk of non-vertebral fractures: review and meta-analysis of intention-to-treat studies. Osteoporos Int. 2005;16:1291–8. doi: 10.1007/s00198-005-1945-x. [DOI] [PubMed] [Google Scholar]
- 12.Webb R, Brammah T, Lunt M, et al. Prevalence and predictors of intense, chronic and disabling neck and back pain in the UK general population. Spine. 2003;28:1195–202. doi: 10.1097/01.BRS.0000067430.49169.01. [DOI] [PubMed] [Google Scholar]
- 13.O'Neill TW, Cockerill W, Matthis C, et al. Back pain, disability, and radiographic vertebral fracture in European women: a prospective study. Osteoporos Int. 2004;15:760–5. doi: 10.1007/s00198-004-1615-4. [DOI] [PubMed] [Google Scholar]
- 14.Roux C, Priol G, Fechtenbaum J, et al. A clinical tool to determine the necessity of spine radiography in postmenopausal women with osteoporosis presenting with back pain. Ann Rheum Dis. 2007;66:81–5. doi: 10.1136/ard.2006.051474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Margolis RB, Tait RC, Krause SJ. A rating system for use with patient pain drawings. Pain. 1986;24:57–65. doi: 10.1016/0304-3959(86)90026-6. [DOI] [PubMed] [Google Scholar]
- 16.Gibson JE, Pilgram TK, Gilula LA. Response of nonmidline pain to percutaneous vertebroplasty. Am J Roentgenol. 2006;87:869–72. doi: 10.2214/AJR.05.0084. [DOI] [PubMed] [Google Scholar]
- 17.Tobias JH, Hutchinson AP, Hunt LP, et al. Use of clinical risk factors to identify postmenopausal women with vertebral fractures. Osteoporos Int. 2007;18:35–43. doi: 10.1007/s00198-006-0209-8. [DOI] [PubMed] [Google Scholar]
- 18.Jiang G, Eastell R, Barrington N, et al. Comparison of methods for the visual identification of prevalent vertebral fractures in osteoporosis. Osteoporos Int. 2004;15:887–96. doi: 10.1007/s00198-004-1626-1. [DOI] [PubMed] [Google Scholar]
- 19.Siminoski K, Warshawski RS, Jen H, et al. Accuracy of physical examination using the rib–pelvis distance for detection of lumbar vertebral fractures. Am J Med. 2003;115:233–6. doi: 10.1016/s0002-9343(03)00299-7. [DOI] [PubMed] [Google Scholar]
- 20.Krege J, Siminoski K, Adachi J, et al. A simple method for determining the probability a new vertebral fracture is present in postmenopausal women with osteoporosis. Osteoporos Int. 2006;17:379–86. doi: 10.1007/s00198-005-2005-2. [DOI] [PubMed] [Google Scholar]
- 21.Nevitt MC, Ettinger B, Black DM, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med. 1998;128:793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 22.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2000;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 23.Melton JL, Kan SH, Frye MA, et al. Epidemiology of vertebral fractures in women. Am J Epidemiol. 1989;129:1000–11. doi: 10.1093/oxfordjournals.aje.a115204. [DOI] [PubMed] [Google Scholar]
- 24.Marshall D, Johnell O, Wedel H. Meta-analysis of how well measures of BMD predict occurrence of osteoporotic fractures. Br Med J. 1996;312:1254–9. doi: 10.1136/bmj.312.7041.1254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.van der Klift M, de Laet CEDH, McCloskey EV, et al. Risk factors for incident vertebral fractures in men and women: the Rotterdam study. J Bone Miner Res. 2004;19:1172–80. doi: 10.1359/JBMR.040215. [DOI] [PubMed] [Google Scholar]
- 26.EPOS Group The relationship between bone density and incident vertebral fracture in men and women. J Bone Miner Res. 2002;17:2214–21. doi: 10.1359/jbmr.2002.17.12.2214. 2002. [DOI] [PubMed] [Google Scholar]
- 27.Samelson EJ, Hannan MT, Zhang Y, et al. Incidence and risk factors for vertebral fracture in women and men: 25-year follow-up results from the population-based Framingham study. J Bone Miner Res. 2006;21:1207–14. doi: 10.1359/jbmr.060513. [DOI] [PubMed] [Google Scholar]
- 28.Genant HK, Wu CY, van Kuijk C, et al. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res. 1993;8:1137–48. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 29.Lenchik L, Rogers LF, Delmas PD, et al. Diagnosis of osteoporotic vertebral fractures: importance of recognition and description by radiologists. Am J Roentgenol. 2004;183:949–58. doi: 10.2214/ajr.183.4.1830949. [DOI] [PubMed] [Google Scholar]
- 30.Friedrich M, Gittler G, Pieler-Bruha E. Misleading history of pain location in 51 patients with osteoporotic vertebral fractures. Eur Spine J. 2006;15:1797–1800. doi: 10.1007/s00586-006-0065-4. [DOI] [PubMed] [Google Scholar]
- 31.Huntoon E, Sinaki M. Thoracic osteoporotic fracture without upper back pain. Am J Phys Med Rehabil. 2004;83:729. doi: 10.1097/00002060-200409000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Roux C, Fechtenbaum J, Briot K, et al. Inverse relationship between vertebral fractures and spine osteoarthritis in postmenopausal women with osteoporosis. Ann Rheum Dis. 2008;67:224–8. doi: 10.1136/ard.2007.069369. [DOI] [PubMed] [Google Scholar]
- 33.Patel U, Skingle S, Campbell GA, et al. Clinical profile of acute vertebral compression fractures in osteoporosis. Rheumatology. 1991;30:418–21. doi: 10.1093/rheumatology/30.6.418. [DOI] [PubMed] [Google Scholar]