Abstract
Adverse neurological outcome is a major cause of long-term morbidity in ex-preterm children. To investigate the effect of parturition and inflammation on the fetal brain, we utilized two in vivo mouse models of preterm birth. To mimic the most common human scenario of preterm birth, we used a mouse model of intrauterine inflammation by intrauterine infusion of lipopolysaccharide (LPS). To investigate the effect of parturition on the immature fetal brain, in the absence of inflammation, we used a non-infectious model of preterm birth by administering RU486. Pro-inflammatory cytokines (IL-10, IL-1β, IL-6 and TNF-α) in amniotic fluid and inflammatory biomarkers in maternal serum and amniotic fluid were compared between the two models using ELISA. Pro-inflammatory cytokine expression was evaluated in the whole fetal brains from the two models. Primary neuronal cultures from the fetal cortex were established from the different models and controls in order to compare the neuronal morphology. Only the intrauterine inflammation model resulted in an elevation of inflammatory biomarkers in the maternal serum and amniotic fluid. Exposure to inflammation-induced preterm birth, but not non-infectious preterm birth, also resulted in an increase in cytokine mRNA in whole fetal brain and in disrupted fetal neuronal morphology. In particular, Microtubule-associated protein 2 (MAP2) staining was decreased and the number of dendrites was reduced (P < 0.001, ANOVA between groups). These results suggest that inflammation-induced preterm birth and not the process of preterm birth may result in neuroinflammation and alter fetal neuronal morphology.
Keywords: mouse model of preterm birth, neuroinflammation, neuronal injury
In the United States, approximately 12% of all live births are delivered preterm (Green et al., 2005). Preterm birth (PTB) is the leading cause of neonatal mortality and morbidity in the United States. Specifically, PTB is a risk factor for adverse neurological outcome for ex-preterm children (Anderson and Doyle, 2003; Hack et al., 2005).
It has long been believed that cerebral palsy is the primary neurological outcome of clinical interest. However, it is now known that ex-preterm children also are at a significant risk for a spectrum of cognitive and neurobehavioral disorders (Marlow et al., 2005; Wood et al., 2005; Costeloe, 2006; Limperopoulos et al., 2007; Lindstrom et al., 2009) including autism spectrum disorders (Brimacombe et al., 2007; Limperopoulos et al., 2008; Schendel and Bhasin, 2008). Current understanding of the pathogenesis of fetal brain injury in a PTB focuses mainly on specific structural findings of white matter damage (WMD) (Cai et al., 2000; Paintlia et al., 2004; Rousset et al., 2006). This current paradigm may be insufficient to explain the increasing prevalence of adverse cognitive and neurobehavioral outcomes in ex-preterm infants.
While adverse neurological outcomes are increasingly prevalent in ex-preterm children, it remains unknown whether the process of parturition alone at an early gestational age or inflammatory pathways associated with preterm birth are mechanistically responsible for evoking injury in the fetal brain. Reports that maternal fever and/or inflammation of the placenta at the time of a PTB dramatically increase the risk for adverse neurological outcome in these infants (Dammann and Leviton, 1998; Dammann et al., 2002; Roze et al., 2008) strongly argue that activation of inflammatory pathways may mediate fetal brain injury in a preterm birth. Furthermore, increased levels of pro-inflammatory cytokines (tumor necrosis factor (TNF)-α, interleukin (IL)-1β, and IL-6) in the amniotic fluid or cord blood are associated with future development of cerebral palsy in these preterm offspring (Duggan and Edwards, 2001; Yoon et al., 2003). Although the effect of preterm birth on the fetal brain has been investigated utilizing various animal models of inflammation (Bell and Hallenbeck, 2002; Debillon et al., 2003; Elovitz and Mrinalini, 2004; Wang et al., 2006, 2007), the outcomes of interest (e.g. WMD) was never compared to a non-infectious/inflammatory model of preterm birth. Furthermore, while the presence of WMD was investigated in these models, these previous studies did not address whether preterm birth evokes neuronal injury.
For the current study, we hypothesize that exposure to inflammation in preterm parturition and not just the process of parturition causes a specific neuronal injury in the fetal brain that may result in long-term neuronal dysfunction that leads to cognitive, behavioral and motor abnormalities in ex-preterm children. These studies sought to assess whether preterm parturition promotes neuronal injury and to determine if these untoward effects were mediated by the process of parturition on a premature brain or whether activation of inflammatory cascade was required for the neuronal injury.
METHODS
Models of Preterm Birth
Two mouse models of pre-term birth (CD-1 out-bred, timed pregnant mice; Charles River Laboratories, Wilmington, MA) were utilized: 1) a model of intrauterine inflammation and 2) a non-infectious model of preterm birth. All of the experiments were conducted in accordance with international standards on animal welfare as well as in compliance with local and national regulations. Adequate measures were taken to minimize pain or discomfort of animals. Specifically, isoflurane anesthesia was utilized during mini-laparotomy and animals were euthanized with carbon dioxide (CO2).
Mouse Model of Intrauterine Inflammation
We utilized an established mouse model of localized intrauterine inflammation (Bell and Hallenbeck, 2002; Elovitz and Mrinalini, 2004; Wang et al., 2007) by an intrauterine injection of lipopolysacharide (LPS); an endotoxin and a component of the cell wall of gram-negative bacteria. For these studies, survival surgery and intrauterine injection of LPS are performed on day 15 (E15) of gestation (term is 19 days), and result in preterm birth 95% of the time and no maternal mortality as previously reported (Elovitz et al., 2003, 2006; Elovitz and Mrinalini, 2004, 2005; Elovitz and Gonzalez, 2008). Under isofluorane anesthesia, a mini-laparotomy was performed and dams received an intrauterine infusion of LPS (L2880, Sigma-Aldrich, St Louis, MO) at a dose of 250 µg in 100 µl of sterile saline solution per dam between the 2 most caudal gestational sacs (n = 9–12). Control dams for these experiments received the same volume of intrauterine injection of vehicle (normal saline; n = 9–12), or no anesthesia or intrauterine injection (control; n = 9). This model involves intrauterine infusion of LPS or saline with care not to inject it into the gestational sac/amniotic cavity. The mini-laparotomy was closed with staples and dams were humanely euthanized 6 hr after the procedure for tissue harvesting and generation of primary neuronal cultures as described below. As many cases of preterm birth are associated with inflammation of the fetal membranes and/or placenta (demonstrating local inflammation), this model aptly mimics the most common human scenario by which a fetus is exposed to inflammation. Use of such rodent models to serve as models to investigate the effect of intrauterine inflammation on fetal development is well established in the literature (Bell and Hallenbeck, 2002; Elovitz et al., 2003; Wang et al., 2007; Salminen et al., 2008; Burd et al., 2009).
Mouse Model of Non-infectious Preterm Birth
RU486, a progesterone receptor antagonist, was utilized for the mouse model of non-infectious preterm birth (Dudley et al., 1996; Gonzalez et al., 2009). Progesterone withdrawal has been proposed as the mechanism leading to parturition in normal term pregnancies, without inflammatory or infectious causes (Mesiano et al., 2002; Madsen et al., 2004; Mitchell and Taggart, 2009). Therefore, this model serves to mirror the process of parturition in the absence of an inflammatory stimulus. RU486 induced delivery at most gestational ages in the mouse; we used this agent at the same time gestational day as our inflammatory model to determine if the process of parturition on an immature (fetal) brain could cause any evidence of brain injury (cytokine elevation and neuronal injury). We have previously confirmed prior work that demonstrated the 150 micrograms induces labor in the same time interval as our inflammatory model (Dudley et al., 1996; Gonzalez et al., 2009). On E15, dams were injected in the neck region subcutaneously with RU486 (diluted in DMSO) (Sigma-Aldrich) at a dose of 150 µg/dam (n = 9–12). Control dams for these experiments received the same volume of vehicle (DMSO) subcutaneously (n = 6).
Treatment Groups
At the same time point in gestation (E15), the following treatment groups were utilized for these studies: 1) controls (gestationally matched dams receiving no intervention) 2) intrauterine saline (“sham”, receiving anesthesia, surgery, and intrauterine infusion of saline); 3) intrauterine LPS (inflammation-induced preterm birth); and 4) RU486 (non-infectious model of preterm birth).
Harvesting of Tissues
Maternal serum, amniotic fluid and whole fetal brains were harvested consistent with our prior reports, 6 hr after the treatment (LPS or RU486) or vehicle injection (Elovitz and Mrinalini, 2005; Elovitz et al., 2006; Elovitz and Gonzalez, 2008). Nine dams were utilized per each condition. Dams were humanely euthanized with CO2 and tissues were immediately extracted. Maternal serum was collected by aortic puncture with a 19-gauge needle. Amniotic fluid was collected using a 19-gauge needle inserted through the uterine wall into each gestational sac. Amniotic fluid from 3–4 gestational sacs per dam was pooled as one sample and placed immediately on ice. Specimens were spun at 3,000g for 5 min to remove any cellular debris and then immediately placed in −80°C. After the removal of amniotic fluid, 2–3 fetuses were removed from these gestational sacs and the fetal brains dissected from the cranium. All tissues were immediately placed into liquid nitrogen and placed into −80°C freezer for further evaluation.
Markers and Mediators of Inflammation in Maternal Serum and Amniotic Fluid
Cytokines, the traditional markers of an inflammatory state, were assessed in the maternal serum and amniotic fluid. Prior work from our laboratory has demonstrated that cytokine response is quite variable in maternal serum (Gonzalez et al., 2009). Therefore, we sought to assess earlier markers of an inflammatory response-endothelial and leukocyte activation. All cytokines (IL-10, IL-1β, IL-6 and TNF-α) and other biomarkers of inflammation were measured by commercially available ELISA kits (R&D Systems, Minneapolis, MN). Specifically, markers of early leukocyte activation and soluble cellular adhesion molecules (soluble intercellular adhesion molecule-1 (sICAM), sE-Selectin, sL-Selectin) or innate immunity (pentraxin) were assessed.
Levels of sICAM, sE-Selectin, sL-Selectin, and pentraxin were investigated in maternal serum from all four treatment groups (n = 9 per treatment group). For amniotic fluid, levels of these 4 biomarkers were evaluated first in the amniotic fluid from LPS-exposed and saline-exposed dams (n = 9 per treatment group). If a significant difference was observed then follow-up ELISAs comparing levels in amniotic fluid from RU486-exposed and control dams were performed (n = 9 per treatment group).
Cytokine Expression in the Fetal Brain
As we have previously demonstrated that cytokines are increased in fetal brains after exposure to LPS-induced preterm birth (Elovitz et al., 2006), we sought to compare if cytokine message expression was altered in non-infectious preterm birth compared to LPS-induced preterm birth. To assess cytokine mRNA expression of IL-10, IL-1 β, TNF-α and IL-6 in the fetal brain, total RNA was extracted from whole fetal brains with Trizol (Invitrogen, Carlsbad, CA) and purified with the Qiagen RNeasy midi kit (Qiagen, Valencia, CA), and cDNA was generated with high capacity cDNA reverse transcription kit (Applied Biosystems, Foster City, CA). Primer sets, conjugated to Taqman MGB probes, were used for Quantititative Polymerase Chain Reaction QPCR (Applied Biosystems). QPCR reactions were carried out with equivalent dilutions of each cDNA sample on the Applied Biosystems Model 7900 sequence detector PCR machine, as previously reported from our laboratory (Elovitz and Mrinalini, 2005; Elovitz et al., 2006; Elovitz and Gonzalez, 2008). The relative abundance of the target of interest was divided by the relative abundance of 18S in each sample to generate a normalized abundance for the target of interest. All samples were analyzed in triplicate.
Cerebral Cortex Primary Neuronal Cultures
Primary neuronal cultures were created using previously described technique which results in neuronal cultures which consist of 95% of neurons (Monnerie et al., 2003; Burd et al., 2009). Three to four fetal brains were harvested per dam (n = 9 dams per condition) and placed into Petri dishes containing cold (4°C) Ca++/Mg++-free Hanks Balanced Salt Solution (HBSS; Invitrogen), pH 7.4. Meninges and olfactory bulbs were removed. Each cortex was separated from the brain, minced, placed in 4 milliliters (ml) of Neurobasal medium (NBM; Invitrogen) containing 0.03% trypsin (Invitrogen) and incubated for 15 min at 37°C and 5% CO2. Brain tissue was removed and placed in 4.5 ml NBM containing 10% fetal bovine serum (FBS) and aspirated to inactivate trypsin. The medium was decanted and replaced with NBM supplemented with B-27 (Invitrogen) and 0.5mM L-glutamine. Cells were dissociated by trituration. Cell concentration was determined using 1:10 dilution. Cells were plated at low density (4 × 104 cells/ml) on poly-L-lysine (1 mg/ml; Sigma-Aldrich) coated glass coverslips, using 6- and 12-well culture plates. Groups (control, saline-exposed, RU486-exposed and LPS-exposed) were plated to equal density for each experiment. Because of the time involved in preparing cultures and to be consistent with harvesting 6 hr after the LPS or RU486 challenge, experiments were done for two treatment groups at a time (i.e. control and LPS, control and saline, saline and LPS, control and RU486). For each experiment, 3 dams per treatment group were utilized; 3–4 fetal brains were collected per dam and constituted one culture. All experiments were performed in triplicate, i.e. 9 dams were utilized per each treatment group.
Immunocytochemistry
Primary neuronal cultures grown on cover slips were fixed at days in vitro (DIV) 1, 2, 3, 7, 10, 14 and 21 to assess morphologic changes between the treatment groups, using double immunofluorescence. Cells were fixed with 4% paraformaldehyde and permeabilized with 0.5% Triton X-100 (DiaSys Europe Ltd, Wokingham, UK). A mouse monoclonal antibody to Microtubule-associated protein 2 (MAP2; Sigma-Aldrich) was used to identify dendrites and cell bodies at dilution of 1:100. A rabbit polyclonal antibody to 200 kDa Neurofilament protein (NF-200, Sigma-Aldrich) was used to label the entire cell and axon at dilution of 1:400. MAP2 and NF-200 were incubated in 1% of FBS in PBS at 37°C for 2 hr. Secondary antibodies, Alexa Fluor goat anti-mouse 488 (Invitrogen) and Alexa Fluor goat anti-rabbit 568 (Invitrogen) were used for immunofluorescence at 1:500 dilution, with incubations at 37°C for 1 hr. Coverslips were mounted on slides with Fluoromount (Southern Biotechnology, Birmingham, AL). Confocal microscopy (Leica SP2 Confocal) was utilized for the examination of neuronal morphology. Images were evaluated at a final image magnification of 400× with immersion oil.
Quantitative Analysis of Dendritic Processes from Primary Neuronal Cultures
Dendrite growth was analyzed at days in vitro (DIV) 3 using previously described techniques (Monnerie et al., 2003). Briefly, cells were selected at random using at least 3 coverslips for each condition. One coverslip represented 3 fetal brains from 1 dam and three different dams were used for each condition. At least 3 experiments were performed for the condition. To quantify processes emanating from each cell body, 30 neurons from each treatment group were evaluated at a final image magnification of 400×. Individual neurons were selected if they were clearly defined and not overlapping with other neurons. Fluorescent images were recorded and analyzed using a Dell Latitude D620, using an image processing program (Image J 1.37v). Primary dendrite length was measured according to an established technique (Monnerie et al., 2003) by tracing the total length of each dendrite emanating from the cell body.
Quantification of Neuronal Viability
Quantification of cell viability was determined in cortical cultures on DIV 2, 7 and 10 between treatment groups using the 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) Cell Proliferation Assay (Sigma-Aldrich) to measure mitochondrial activity. Briefly, using sterile technique, 10% reconstituted MTT solution was added to each well and incubated at 37°C for 3 hr. Then, 1 ml MTT Solubilization solution was added to each well and mixed by aspiration. The samples were placed into cuvettes and absorbance of samples was assessed at two different wavelengths (570 nm and 690nm). The difference between measurements was calculated to obtain normalized absorbance. Each well represented a primary neuronal culture. All experiments were performed in triplicate. Nine dams were utilized per each treatment group.
Statistical Analysis
Statistical analysis was performed using SigmaStat 3.5 (Aspire Software International, Asburn, VA). Data are expressed as the mean standard deviation of the mean (SD) or as the median where the data is not normally distributed. Statistical significance was defined as a two-sided P < 0.05. To evaluate biomarkers in maternal serum and amniotic fluid and to examine the number of dendritic processes, One-way ANOVA (or ANOVA on ranks for non-parametric data) was used to compare values between the treatment groups. If significance was reached, pair-wise comparison was then performed using Student-Newman-Keuls (SNK) method. For statistical analysis of inflammatory biomarkers in the amniotic fluid, Student t-test (for parametric data) or Mann-Whitney Rank Sum (for non-parametric data) was used. To analyze cytokine mRNA expression in the fetal brains, mRNA expression was 1) compared between LPS-and saline-exposed fetal brain and 2) compared between RU486 and controls using Student t-test or Mann-Whitney Rank sum. For the MTT assay, repeated measures of ANOVA were employed.
RESULTS
Mouse Models of Preterm Birth
Mouse model of intrauterine inflammation resulted in > 95% preterm delivery 8–20 hr after LPS injection while there is no preterm delivery in saline-exposed dams (Elovitz et al., 2003, 2006; Elovitz and Mrinalini, 2004, 2005; Elovitz and Gonzalez, 2008). The RU486 model (non-infectious) resulted in preterm delivery in the same time period as the inflammatory model (8–22 hr following an injection). None of the DMSO-treated dams had preterm delivery (data not shown).
Markers and Mediators of Inflammation in Maternal Serum and Amniotic Serum
Using both mouse models of preterm birth, we sought to assess whether an inflammatory response was present in the maternal serum (maternal compartment). Levels of sICAM, se-Selectin, and pentraxin were significantly different in maternal serum in the different treatment groups (Fig. 1). sICAM was increased 3.8-fold in the maternal serum of LPS treated dams compared to saline (P < 0.001, SNK); sE-Selectin was increased 3-fold compared to saline (P = 0.005, SNK), and pentraxin showed a 5-fold increase in the LPS group compared to saline (P < 0.001, SNK). In contrast, none of these mediators were significantly elevated in maternal serum of RU486 treated dams when compared to saline or control (Fig. 1). Levels of sL-Selectin were not significantly different in maternal serum of the treatment groups (P > 0.05; data not shown).
Fig. 1.
Biomarkers of inflammation in maternal serum in inflammation-induced and non-infectious preterm birth models. Means and standard deviations are presented for biomarker levels in maternal serum (n = 9 for control, n = 9 for saline, n = 9 for LPS and n = 9 for RU486). SICAM levels were significantly different between the groups (P ≤ 0.001, One-Way ANOVA). SICAM demonstrated a 3.8 increase in LPS-exposed dams compared to saline-exposed (P ≤ 0.001, SNK) and was significantly increased compared to control and RU486 (P ≤ 0.001, SNK for both). SICAM levels were similar in controls and RU486. SE-Selectin levels were significantly different between the groups (P ≤ 0.001, One-Way ANOVA). Se-Selectin levels were increased in LPS-exposed dams compared to controls, saline and RU486 (P ≤ 0.001, SNK for all comparisons). Se-Selectin levels were not significantly different between controls, saline-exposed or RU486. Pentraxin levels were significantly different between the groups (P ≤ 0.001, One-Way ANOVA). Pentraxin levels in LPS-exposed dams were increased 7-fold compared to controls, 4.2-fold compared to saline-exposed, and 5-fold compared to RU486 exposed (P ≤ 0.001 for all pair-wise comparisons, SNK). Pentraxin levels were not significantly different between saline, control or RU486. * - indicates statistical significance with P < 0.05.
Amniotic fluid (fetal compartment) levels of cytokines IL-10, IL-1 β, TNF-α and IL-6 were significantly elevated between LPS and saline groups (P < 0.001, Student t-test) but not between RU486 and control groups (Table I).
TABLE I.
Cytokine Fold Change in Amniotic Fluid
P = 0.001 (n = 8 for control, n = 8 for saline, n = 8 for LPS and n = 8 for RU486).
sE-Selectin and pentraxin were not significantly different between LPS and saline-exposed dams. SICAM levels were increased 2.3-fold in the amniotic fluid from LPS-exposed dams compared to saline-exposed (P = 0.002, Mann Whitney). Levels of sL-Selectin were increased 65-fold (P = 0.008, Student t-test) in LPS-exposed compared to saline-exposed dams. However, none of the biomarkers were significantly elevated in the amniotic fluid from RU486-exposed dams compared to controls (data not shown). Taken together, these findings show that the intrauterine inflammation model but not the non-infectious model resulted in an elevation of inflammatory biomarkers in the maternal serum and amniotic fluid.
Cytokine Expression in the Fetal Brain from Inflammation-mediated and Non-infectious Preterm Birth Models
Since the difference between the two models was noted in respect to the expression of cytokines and inflammatory markers in the fetal compartment (amniotic fluid), we investigated the expression of IL-10, IL-1 β, TNF-α and IL-6 in the fetal brain. Message expression of IL-10, IL-1 β, TNF-α and IL-6 was significantly elevated in LPS-exposed fetal brains as compared to saline-exposed. Specifically, IL-10 was increased 2.5 fold (P = 0.005, Student t-test), IL-1β was increased 52.4 fold (P = 0.02, Student t-test), TNF-α was increased 4.1 fold (P = 0.017, Student t-test), and IL-6 was increased 6.2 fold (P = 0.03, Student t-test). In contrast, fetal brains from the non-infectious model of preterm birth did not demonstrate any change in cytokine mRNA expression compared to controls (Table II). These results demonstrate that while both the LPS and RU486 model can trigger preterm birth only the LPS model increases cytokine expression in the fetal brain.
TABLE II.
Cytokine Fold Change in Whole Fetal Brains
P = 0.05 for IL-10, 0.002 for IL-1β, 0.017 for TNF-α and 0.03 for IL-6 (n = 9 for control, n = 9 for saline, n = 9 for LPS and n = 9 for RU486).
Neuronal Morphology and Growth are Altered by Exposure to Intrauterine Inflammation
Since cytokines have been demonstrated to be neurotoxic (Yamasaki et al., 1995; Barone et al., 1997; Nawashiro et al., 1997; Allan et al., 2000; Viviani et al., 2003, 2006) and this time of fetal development is important for cortical neuronal synapse development (Leviton and Gressens, 2007), neuronal morphology and neuronal survival were evaluated.
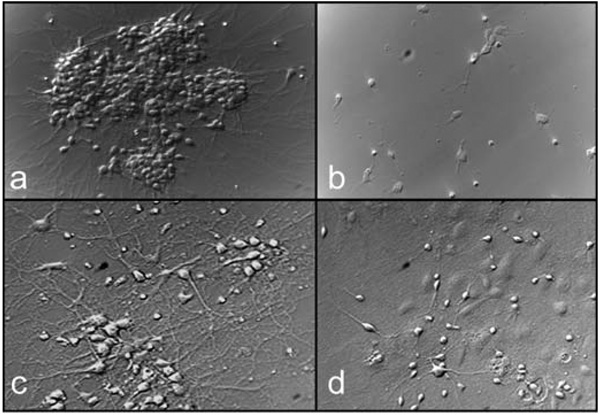
At DIV 3, LPS-exposed cells had abnormal cell body morphology as evaluated by phase (Fig. 2) and confocal microscopy (Figs. 3, 4). By DIV 10, the LPS-exposed cells continued to demonstrate a lack of processes and abnormal morphology. On qualitative assessment, confocal images of neurons exposed to LPS, but not exposed to saline or RU486, demonstrated decreased growth, abnormal morphology and an overall decrease in MAP2 staining.
Fig. 2.
Phase-contrast pictures of neuronal cells DIV 3 and 14. Control cells demonstrate aggregation of neuronal cells and numerous processes from each cell body (panels A and C- Div 3 and 14, respectively), LPS-exposed neurons demonstrate lack of aggregation, altered morphology (dysmorphic cell bodies) and decreased processes emanating from the cell bodies (panels B and D- Div 3 and 14, respectively). Magnification 400×.
Fig. 3.
Confocal overlay (MAP2 and NF200) images of neurons at DIV 10. MAP-2 staining is seen in green and NF200 staining in red. Panel a represents neuronal morphology in control group at DIV 10. Panel b shows neuronal morphology in RU486-treated neurons at DIV 10. Panels C and D show neuronal morphology in LPS-treated group at DIV 10. The control and RU486 cells demonstrated numerous processes present with discrete cellular morphology. The LPS-exposed neurons demonstrated decreased growth, abnormal morphology and decreased MAP2 staining. In the addition, the MAP2 staining in LPS treated neurons has a discontinuous dotted pattern. Magnification 400×.
Fig. 4.
Confocal images of neurons at DIV 14. A: Overlay of NF200 and MAP2. B: NF-200. C: MAP2. The control and RU486 cells demonstrated numerous processes present with discrete cellular morphology. The LPS-exposed neurons demonstrated decreased growth, abnormal morphology and overall decreased NF and MAP2 staining. Magnification 400×.
Quantitative Analysis of Dendritic Processes from Primary Neuronal Cultures
The number of dendritic processes was recorded from cultured neurons at DIV 3. The use of the number of dendritic processes on cultured neurons is an objective method to examine potential neuronal injury among surviving neurons and is well established in the literature (Coronas et al., 2002; Monnerie et al., 2003; Monnerie and Le Roux, 2007). Compared to control or saline-exposed, the LPS-exposed neurons had a significantly decreased number of dendrites (Fig. 5). In addition, RU486 exposed neurons, harvested from fetuses in the non-infectious PTB model, demonstrated no change in the number of dendritic processed as compared to saline or control cells. The length of the dendritic processes at DIV 3 was not significantly different between any of the treatment groups (P > 0.05, ANOVA).
Fig. 5.
Number of dendritic processes of cultured neurons at DIV 3. Means and standard errors are represented for each group (n = 9 for control, n = 9 for saline, n = 9 for LPS and n = 9 for RU486). There were significantly less processes present on LPS-exposed cells at DIV 3 than for saline-exposed, RU486-exposed or control groups (*P< 0.001, ANOVA between groups).
Quantification of Neuronal Viability
Neuronal cell viability in the cortical cultures was assessed at DIV 2, 7, and 10 (n = 6 per each treatment group). Statistical analysis demonstrated no significant difference in multiple comparisons over time between control and the LPS-exposed cells (P = 0.92, 0.29, and 0.63 respectively for days 2, 7 and 10, repeated measures ANOVA).
DISCUSSION
About 1 in 10 live births is a preterm birth. This is an enormous public health issue since many of these preterm infants survive with neurocognitive, behavioral and motor disability (Wood et al., 2005; Marlow et al., 2005; Costeloe, 2006; Limperopoulos et al., 2007; Lindstrom et al., 2009). The precise mechanisms behind neuronal injury and dysfunction after preterm birth have not been investigated. In this study, using mouse models, we examined whether preterm parturition in the presence or absence of intrauterine inflammation influences neuronal morphology. Our novel data demonstrate that inflammation-mediated preterm birth results in altered neuronal morphology in the fetus. In particular, we observed not only subjective findings of altered neuronal morphology but also the objective finding of a decrease in the number of dendrites. This may be a clinically important finding since dendrite morphology and plasticity likely represent the cellular response to learning and memory. Importantly, our results indicate that this neuronal injury is not from the process of parturition on an immature brain but rather from activation of inflammatory pathways.
A number of animal models have been developed to elucidate the mechanisms by which preterm birth promotes fetal brain injury (Bell and Hallenbeck, 2002; Debillon et al., 2003; Elovitz and Mrinalini, 2004; Wang et al., 2006, 2007). However, all of these models of preterm birth employ an inflammatory stimulus for labor induction. From these studies, it remains unclear whether inflammation in a preterm birth was an epiphenomena or truly necessary for the observed brain injury. By comparing a model of inflammation-induced preterm birth to a non-infectious preterm birth model, we were able to demonstrate that intrauterine inflammation is a critical and necessary for fetal brain injury and altered neuronal morphology in preterm birth. While these studies cannot determine if the inflammatory biomarkers or cytokines assessed are mechanistically involved, our results do indicate that inflammatory pathways are activated in the mother, fetus and fetal brain when neuronal injury is present. Whether activation of inflammatory pathways in any or all of these compartments is necessary and/or sufficient for fetal brain injury requires further investigation.
The use of an animal model has notable limitations for the study of any disease state. Yet, this line of research is neither practical nor feasible in human pregnancy. As prenatal inflammation confers a documented risk for adverse neurobehavioral disorders, animal models of this condition are tantamount to hopes of successful interventions. Mouse models to study parturition and inflammation-induced preterm parturition are well-established in the literature; the models used herein provide acceptable models for the study of the effects of inflammation and parturition on the fetal brain. Furthermore, the use of the rodent models to investigate neuronal injury in other neuroinflammatory disorders that afflict humans is well established (Nguyen et al., 2004; Walter et al., 2006; Piazza and Lynch, 2009; Cunningham et al., 2009). While the effect of inflammation-induced preterm birth on a immature brain has been studied by others (Bell and Hallenbeck, 2002; Debillon et al., 2003; Elovitz and Mrinalini, 2004; Wang et al., 2006, 2007), the focus for most of this work has been on unraveling the pathogenesis of white matter injury from prenatal inflammation. Until now, these models have not been utilized to explore the effect of prenatal inflammation on neuronal injury and morphology.
Recent studies demonstrate that ex-preterm infants have significant behavioral, social and learning disabilities throughout childhood and adolescence (Marlow et al., 2005; Wood et al., 2005; Costeloe, 2006; Limperopoulos et al., 2007; Lindstrom et al., 2009). Yet, most of these infants do not have overt evidence of structural injury by radiological imaging (Rademaker et al., 2005). These findings suggest that while overt injury (e.g. cystic periventricular leukomalacia) or even WMD may be sufficient for long-term adverse outcomes, neuronal injury may play a crucial role for observed adverse neurological outcomes in ex-preterm children. While our study does not rule out WMD as an etiology for these adverse outcomes, it does provide compelling evidence that neuronal injury may be responsible for the abnormal neuronal function and communication that is observed as these ex-preterm children mature. Furthermore, recent clinical evidence, using quantitative MRI, demonstrated volume loss in the cerebral cortex, thalamus and hippocampus in children surviving preterm birth (Inder et al., 1999, 2005). This may suggest a more subtle cortical injury, such as neuronal loss or lack of dendritic arborization (King et al., 2006). These clinical findings of neuronal rather than just glial involvement are consistent with our laboratory data and represent a novel way of conceptualizing brain damage associated with preterm birth.
In our experiments, we used three different control groups (control, saline and RU486). None of these controls demonstrated neuronal abnormalities which strengthens our findings that inflammation in preterm birth plays an essential role in neuronal injury. In particular we found that the number of dendritic processes was reduced in neurons harvested from LPS induced preterm birth. Since dendritic morphology has been demonstrated to be vital to normal neuronal information processing and allows the neuron to receive messages and permits cortical connectivity (Whitford et al., 2002), our findings suggest that this damage may lead to long-term adverse neurological outcomes by modulating communication between neurons and other neurons, or neurons and glia. Furthermore, we observed a decrease in MAP2 staining in LPS-exposed cultures. Previous reports demonstrate decreased MAP2 staining in cultured neurons that are fragile or exposed to excitotoxicity (Bigot et al., 1991; King et al., 2006).
One notable limitation in our work that primary neuronal cultures were 95% pure with the other 5% consisting of glia (Coronas et al., 2002; Monnerie et al., 2003; Monnerie and Le Roux, 2007). While it is possible that microglia and astrocytes played an important role in the initiation of neuronal injury and this injury was communicated by glia within the 6 hr of exposure in vivo, the use of the NBM which is selective for neurons and does not contain fetal bovine serum is less likely to support glial growth at DIV 14 (when the neuronal injury is continued to be seen). Studies were undertaken to investigate neuronal morphology in co-cultures (neurons plus glia) as well as the expression of the marker of neuronal differentiation (MAP2) in the whole fetal brains (Burd et al., 2009). In those studies, LPS-exposed neurons showed an abnormal morphology in co-culture with glia, demonstrating a decrease in MAP2 staining (Burd et al., 2009). Furthermore, MAP2 mRNA expression was similarly decreased in the whole fetal brains (Burd et al., 2009). Therefore, these studies, along with the current ones, demonstrated that glia may be involved in initiation of neuronal injury but may not be necessary for continued neuronal injury (as observed with these in vitro studies) nor did the presence of glia appear to provide a sufficient neuroprotective role.
Importantly, while LPS-exposed neurons appear dysmorphic and have a decreased number of processes, they continue to grow in culture with no significant increase in cell death. This finding is consistent with our prior work, indicating that there is no overt necrosis or apoptosis in the developing brains as well as no significant involvement of caspases (Elovitz et al., 2006; Burd et al., 2009). If this finding is true in vivo, in human preterm birth, then the possibility of continued survival, growth and interaction of abnormal neurons could result in significant and continued brain injury through altered neuron-neuron and neuron-glia communication leading to adverse neurobehavioral outcomes. Since at this time of gestation (E15), greater than 95 % of fetuses deliver within 24 hr (by E16–17), it was not possible to investigate the effect of longer LPS exposure on the fetal brains. Further studies are necessary to evaluate whether the exposure to lower doses of intrauterine LPS, while not resulting in preterm birth, will lead to changes in neuronal morphology and neurobehavioral outcomes.
Cytokines, specifically IL-1β and TNF-α, have been demonstrated to be neurotoxic (Yamasaki et al., 1995; Barone et al., 1997; Nawashiro et al., 1997; Allan et al., 2000; Viviani et al., 2003, 2006). The increase in cytokines in the amniotic fluid may be more reflective of the fetal inflammatory response and as such, may not indicate the immune response in the fetal brain. However, the elevation of the message expression of these cytokines in the fetal brain in our inflammation-induced PTB model but not the non-infectious model, suggests that these cytokines may be a critical mechanism in the observed neuronal injury. The demonstration that IL-1β, IL-6 and TNF-α mRNA are up-regulated in LPS-exposed brains is consistent with prior work from our laboratory and other animal models (Cai et al., 2000; Bell and Hallenbeck, 2002; Elovitz et al., 2006; Kumral et al., 2007). IL-1β has been demonstrated to mediate neuronal injury, potentiate excitotoxicity and to be an essential player in neuron-glia cross talk (Ma et al., 2002). As with IL-1β, IL-6 is reported to alter NMDA receptor-mediated response and to enhance neurotoxicity (Qiu et al., 1998). Targeting IL-1β and/or IL-6 may hold promise in preventing neuronal injury in a preterm birth. However, we acknowledge that these cytokines may represent secondary mediators and may not be essential for neuronal injury in a preterm birth. Further work is required to dissect the precise mechanisms responsible for fetal and neonatal brain injury in inflammation-induced preterm birth.
In conclusion, neuronal injury may be a critical mechanism by which inflammation-induced preterm birth leads to adverse neurological outcome. By targeting the primary mediators and precise mechanisms involved in inflammation-induced neuronal damage, new avenues for novel therapeutic options to reduce adverse neonatal outcome in ex-preterm infants can begin.
Acknowledgments
Contract grant sponsor: Institute for Translational Medicine and Therapeutics of the University of Pennsylvania; Contract grant sponsor: National Institutes of Health; Contract grant number: 5-RO1-HD046544-0 (to M.E.); Contract grant sponsor: National Center for Research Resources Grant; Contract grant number: UL1RR024134.
REFERENCES
- Allan SM, Parker LC, Collins B, Davies R, Luheshi GN, Rothwell NJ. Cortical cell death induced by IL-1 is mediated via actions in the hypothalamus of the rat. Proc Natl Acad Sci USA. 2000;97:5580–5585. doi: 10.1073/pnas.090464197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson P, Doyle LW. Neurobehavioral outcomes of school-age children born extremely low birth weight or very preterm in the 1990s. JAMA. 2003;289:3264–3272. doi: 10.1001/jama.289.24.3264. [DOI] [PubMed] [Google Scholar]
- Barone FC, Arvin B, White RF, Miller A, Webb CL, Willette RN, Lysko PG, Feuerstein GZ. Tumor necrosis factor-alpha. A mediator of focal ischemic brain injury. Stroke. 1997;28:1233–1244. doi: 10.1161/01.str.28.6.1233. [DOI] [PubMed] [Google Scholar]
- Bell MJ, Hallenbeck JM. Effects of intrauterine inflammation on developing rat brain. J Neurosci Res. 2002;70:570–579. doi: 10.1002/jnr.10423. [DOI] [PubMed] [Google Scholar]
- Bigot D, Matus A, Hunt SP. Reorganization of the cytoskeleton in rat neurons following stimulation with excitatory amino acids in vitro. Eur J Neurosci. 1991;3:551–558. doi: 10.1111/j.1460-9568.1991.tb00842.x. [DOI] [PubMed] [Google Scholar]
- Brimacombe M, Ming X, Lamendola M. Prenatal and birth complications in autism. Matern Child Health J. 2007;11:73–79. doi: 10.1007/s10995-006-0142-7. [DOI] [PubMed] [Google Scholar]
- Burd I, Chai J, Gonzalez J, Ofori E, Monnerie H, Le Roux PD, Elovitz MA. Beyond white matter damage: fetal neuronal injury in a mouse model of preterm birth. Am J Obstet Gynecol. 2009;201:e271–e278. doi: 10.1016/j.ajog.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Z, Pan ZL, Pang Y, Evans OB, Rhodes PG. Cytokine induction in fetal rat brains and brain injury in neonatal rats after maternal lipopolysaccharide administration. Pediatr Res. 2000;47:64–72. doi: 10.1203/00006450-200001000-00013. [DOI] [PubMed] [Google Scholar]
- Coronas V, Arnault P, Roger M. Cortical diffusible factors increase MAP-2 immunoreactive neuronal population in thalamic cultures. Neurosci Res. 2002;43:57–67. doi: 10.1016/s0168-0102(02)00020-2. [DOI] [PubMed] [Google Scholar]
- Costeloe K. EPICure: facts and figures: why preterm labour should be treated. BJOG. 2006;113:10–12. doi: 10.1111/j.1471-0528.2006.01118.x. [DOI] [PubMed] [Google Scholar]
- Cunningham C, Campion S, Lunnon K, Murray CL, Woods JF, Deacon RM, Rawlins JN, Perry VH. Systemic inflammation induces acute behavioral and cognitive changes and accelerates neurodegenerative disease. Biol Psychiatry. 2009;65:304–312. doi: 10.1016/j.biopsych.2008.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dammann O, Leviton A. Maternal intrauterine infection, cytokines, and brain damage in the preterm newborn. Pediatr Res. 1997;42:1–8. doi: 10.1203/00006450-199707000-00001. [DOI] [PubMed] [Google Scholar]
- Dammann O, Leviton A. Infection remote from the brain, neonatal white matter damage, and cerebral palsy in the preterm infant. Semin Pediatr Neurol. 1998;5:190–201. doi: 10.1016/s1071-9091(98)80034-x. [DOI] [PubMed] [Google Scholar]
- Dammann O, Kuban KC, Leviton A. Perinatal infection, fetal inflammatory response, white matter damage, and cognitive limitations in children born preterm. Ment Retard Dev Disabil Res Rev. 2002;8:46–50. doi: 10.1002/mrdd.10005. [DOI] [PubMed] [Google Scholar]
- Debillon T, Gras-Leguen C, Leroy S, Caillon J, Roze JC, Gressens P. Patterns of cerebral inflammatory response in a rabbit model of intrauterine infection-mediated brain lesion. Brain Res Dev Brain Res. 2003;145:39–48. doi: 10.1016/s0165-3806(03)00193-7. [DOI] [PubMed] [Google Scholar]
- Dudley DJ, Branch DW, Edwin SS, Mitchell MD. Induction of preterm birth in mice by RU486. Biol Reprod. 1996;55:992–995. doi: 10.1095/biolreprod55.5.992. [DOI] [PubMed] [Google Scholar]
- Duggan PJ, Edwards AD. Placental inflammation and brain injury in preterm infants. Dev Med Child Neurol Suppl. 2001;86:16–17. doi: 10.1111/j.1469-8749.2001.tb04140.x. [DOI] [PubMed] [Google Scholar]
- Elovitz MA, Mrinalini C. Animal models of preterm birth. Trends Endocrinol Metab. 2004;15:479–487. doi: 10.1016/j.tem.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Elovitz MA, Mrinalini C. Can medroxyprogesterone acetate alter Toll-like receptor expression in a mouse model of intrauterine inflammation? Am J Obstet Gynecol. 2005;193:1149–1155. doi: 10.1016/j.ajog.2005.05.043. [DOI] [PubMed] [Google Scholar]
- Elovitz MA, Gonzalez J. Medroxyprogesterone acetate modulates the immune response in the uterus, cervix and placenta in a mouse model of preterm birth. J Matern Fetal Neonatal Med. 2008;21:223–230. doi: 10.1080/14767050801923680. [DOI] [PubMed] [Google Scholar]
- Elovitz MA, Wang Z, Chien EK, Rychlik DF, Phillippe M. A new model for inflammation-induced preterm birth: the role of platelet-activating factor and Toll-like receptor-4. Am J Pathol. 2003;163:2103–2111. doi: 10.1016/S0002-9440(10)63567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elovitz MA, Mrinalini C, Sammel MD. Elucidating the early signal transduction pathways leading to fetal brain injury in preterm birth. Pediatr Res. 2006;59:50–55. doi: 10.1203/01.pdr.0000191141.21932.b6. [DOI] [PubMed] [Google Scholar]
- Gonzalez JM, Ofori E, Burd I, Chai J, Scholler N, Elovitz MA. Maternal mortality from systemic illness: unraveling the contribution of the immune response. Am J Obstet Gynecol. 2009;200:430–438. doi: 10.1016/j.ajog.2009.01.049. [DOI] [PubMed] [Google Scholar]
- Gonzalez JM, Xu H, Chai J, Ofori E, Elovitz MA. Preterm and term cervical ripening in CD1 mice (Mus musculus): similar or divergent molecular mechanisms? Biol Reprod. 2009 doi: 10.1095/biolreprod.108.075309. (In Press) [DOI] [PubMed] [Google Scholar]
- Green NS, Damus K, Simpson JL, Iams J, Reece EA, Hobel CJ, Merkatz IR, Greene MF, Schwarz RH. Research agenda for preterm birth: recommendations from the March of Dimes. Am J Obstet Gynecol. 2005;193:626–635. doi: 10.1016/j.ajog.2005.02.106. [DOI] [PubMed] [Google Scholar]
- Hack M, Taylor HG, Drotar D, Schluchter M, Cartar L, Andreias L, Wilson-Costello D, Klein N. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA. 2005;294:318–325. doi: 10.1001/jama.294.3.318. [DOI] [PubMed] [Google Scholar]
- Inder TE, Huppi PS, Warfield S, Kikinis R, Zientara GP, Barnes PD, Jolesz F, Volpe JJ. Periventricular white matter injury in the premature infant is followed by reduced cerebral cortical gray matter volume at term. Ann Neurol. 1999;46:755–760. doi: 10.1002/1531-8249(199911)46:5<755::aid-ana11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Inder TE, Warfield SK, Wang H, Huppi PS, Volpe JJ. Abnormal cerebral structure is present at term in premature infants. Pediatrics. 2005;115:286–294. doi: 10.1542/peds.2004-0326. [DOI] [PubMed] [Google Scholar]
- King AE, Chung RS, Vickers JC, Dickson TC. Localization of glutamate receptors in developing cortical neurons in culture and relationship to susceptibility to excitotoxicity. J Comp Neurol. 2006;498:277–294. doi: 10.1002/cne.21053. [DOI] [PubMed] [Google Scholar]
- Kumral A, Baskin H, Yesilirmak DC, Ergur BU, Aykan S, Genc S, Genc K, Yilmaz O, Tugyan K, Giray O, Duman N, Ozkan H. Erythropoietin attenuates lipopolysaccharide-induced white matter injury in the neonatal rat brain. Neonatology. 2007;92:269–278. doi: 10.1159/000105493. [DOI] [PubMed] [Google Scholar]
- Leviton A, Gressens P. Neuronal damage accompanies perinatal white-matter damage. Trends Neurosci. 2007;30:473–478. doi: 10.1016/j.tins.2007.05.009. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Bassan H, Gauvreau K, Robertson RL, Jr, Sullivan NR, Benson CB, Avery L, Stewart J, Soul JS, Ringer SA, Volpe JJ, duPlessis AJ. Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors? Pediatrics. 2007;120:584–593. doi: 10.1542/peds.2007-1041. [DOI] [PubMed] [Google Scholar]
- Limperopoulos C, Bassan H, Sullivan NR, Soul JS, Robertson RL, Jr, Moore M, Ringer SA, Volpe JJ, du Plessis AJ. Positive screening for autism in ex-preterm infants: prevalence and risk factors. Pediatrics. 2008;121:758–765. doi: 10.1542/peds.2007-2158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom K, Lindblad F, Hjern A. Psychiatric morbidity in adolescents and young adults born preterm: a Swedish national cohort study. Pediatrics. 2009;123:e47–e53. doi: 10.1542/peds.2008-1654. [DOI] [PubMed] [Google Scholar]
- Ma XC, Gottschall PE, Chen LT, Wiranowska M, Phelps CP. Role and mechanisms of interleukin-1 in the modulation of neurotoxicity. Neuroimmunomodulation. 2002;10:199–207. doi: 10.1159/000068322. [DOI] [PubMed] [Google Scholar]
- Madsen G, Zakar T, Ku CY, Sanborn BM, Smith R, Mesiano S. Prostaglandins differentially modulate progesterone receptor-A and -B expression in human myometrial cells: evidence for prostaglandin-induced functional progesterone withdrawal. J Clin Endocrinol Metab. 2004;89:1010–1013. doi: 10.1210/jc.2003-031037. [DOI] [PubMed] [Google Scholar]
- Marlow N, Wolke D, Bracewell MA, Samara M. Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med. 2005;352:9–19. doi: 10.1056/NEJMoa041367. [DOI] [PubMed] [Google Scholar]
- Mesiano S, Chan EC, Fitter JT, Kwek K, Yeo G, Smith R. Progesterone withdrawal and estrogen activation in human parturition are coordinated by progesterone receptor A expression in the myometrium. J Clin Endocrinol Metab. 2002;87:2924–2930. doi: 10.1210/jcem.87.6.8609. [DOI] [PubMed] [Google Scholar]
- Mitchell BF, Taggart MJ. Are animal models relevant to key aspects of human parturition? Am J Physiol Regul Integr Comp Physiol. 2009;297:R525–R545. doi: 10.1152/ajpregu.00153.2009. [DOI] [PubMed] [Google Scholar]
- Monnerie H, Le Roux PD. Reduced dendrite growth and altered glutamic acid decarboxylase (GAD) 65- and 67-kDa isoform protein expression from mouse cortical GABAergic neurons following excitotoxic injury in vitro. Exp Neurol. 2007;205:367–382. doi: 10.1016/j.expneurol.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Monnerie H, Shashidhara S, Le Roux PD. Effect of excess extracellular glutamate on dendrite growth from cerebral cortical neurons at 3 days in vitro: involvement of NMDA receptors. J Neurosci Res. 2003;74:688–700. doi: 10.1002/jnr.10797. [DOI] [PubMed] [Google Scholar]
- Nawashiro H, Martin D, Hallenbeck JM. Inhibition of tumor necrosis factor and amelioration of brain infarction in mice. J Cereb Blood Flow Metab. 1997;17:229–232. doi: 10.1097/00004647-199702000-00013. [DOI] [PubMed] [Google Scholar]
- Nguyen MD, D’Aigle T, Gowing G, Julien JP, Rivest S. Exacerbation of motor neuron disease by chronic stimulation of innate immunity in a mouse model of amyotrophic lateral sclerosis. J Neurosci. 2004;24:1340–1349. doi: 10.1523/JNEUROSCI.4786-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paintlia MK, Paintlia AS, Barbosa E, Singh I, Singh AK. N-acetylcysteine prevents endotoxin-induced degeneration of oligodendrocyte progenitors and hypomyelination in developing rat brain. J Neurosci Res. 2004;78:347–361. doi: 10.1002/jnr.20261. [DOI] [PubMed] [Google Scholar]
- Piazza A, Lynch MA. Neuroinflammatory changes increase the impact of stressors on neuronal function. Biochem Soc Trans. 2009;37:303–307. doi: 10.1042/BST0370303. [DOI] [PubMed] [Google Scholar]
- Qiu Z, Sweeney DD, Netzeband JG, Gruol DL. Chronic interleukin-6 alters NMDA receptor-mediated membrane responses and enhances neurotoxicity in developing CNS neurons. J Neurosci. 1998;18:10445–10456. doi: 10.1523/JNEUROSCI.18-24-10445.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rademaker KJ, Uiterwaal CS, Beek FJ, van Haastert IC, Lieftink AF, Groenendaal F, Grobbee DE, de Vries LS. Neonatal cranial ultrasound versus MRI and neurodevelopmental outcome at school age in children born preterm. Arch Dis Child Fetal Neonatal Ed. 2005;90:F489–F493. doi: 10.1136/adc.2005.073908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rousset CI, Chalon S, Cantagrel S, Bodard S, Andres C, Gressens P, Saliba E. Maternal exposure to LPS induces hypomyelination in the internal capsule and programmed cell death in the deep gray matter in newborn rats. Pediatr Res. 2006;59:428–433. doi: 10.1203/01.pdr.0000199905.08848.55. [DOI] [PubMed] [Google Scholar]
- Roze E, Kerstjens JM, Maathuis CG, ter Horst HJ, Bos AF. Risk factors for adverse outcome in preterm infants with periventricular hemorrhagic infarction. Pediatrics. 2008;122:e46–e52. doi: 10.1542/peds.2007-3305. [DOI] [PubMed] [Google Scholar]
- Salminen A, Paananen R, Vuolteenaho R, Metsola J, Ojaniemi M, Autio-Harmainen H, Hallman M. Maternal endotoxin-induced preterm birth in mice: fetal responses in toll-like receptors, collectins, and cytokines. Pediatr Res. 2008;63:280–286. doi: 10.1203/PDR.0b013e318163a8b2. [DOI] [PubMed] [Google Scholar]
- Schendel D, Bhasin TK. Birth weight and gestational age characteristics of children with autism, including a comparison with other developmental disabilities. Pediatrics. 2008;121:1155–1164. doi: 10.1542/peds.2007-1049. [DOI] [PubMed] [Google Scholar]
- Viviani B, Bartesaghi S, Gardoni F, Vezzani A, Behrens MM, Bartfai T, Binaglia M, Corsini E, Di Luca M, Galli CL, Marinovich M. Interleukin-1beta enhances NMDA receptor-mediated intracellular calcium increase through activation of the Src family of kinases. J Neurosci. 2003;23:8692–8700. doi: 10.1523/JNEUROSCI.23-25-08692.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viviani B, Gardoni F, Bartesaghi S, Corsini E, Facchi A, Galli CL, Di Luca M, Marinovich M. Interleukin-1 beta released by gp120 drives neural death through tyrosine phosphorylation and trafficking of NMDA receptors. J Biol Chem. 2006;281:30212–30222. doi: 10.1074/jbc.M602156200. [DOI] [PubMed] [Google Scholar]
- Walter S, Doering A, Letiembre M, Liu Y, Hao W, Diem R, Bernreuther C, Glatzel M, Engelhardt B, Fassbender K. The LPS receptor, CD14, in experimental autoimmune encephalomyelitis and multiple sclerosis. Cell Physiol Biochem. 2006;17:167–172. doi: 10.1159/000092078. [DOI] [PubMed] [Google Scholar]
- Wang X, Rousset CI, Hagberg H, Mallard C. Lipopolysaccharide-induced inflammation and perinatal brain injury. Semin Fetal Neonatal Med. 2006;11:343–353. doi: 10.1016/j.siny.2006.04.002. [DOI] [PubMed] [Google Scholar]
- Wang X, Hagberg H, Zhu C, Jacobsson B, Mallard C. Effects of intrauterine inflammation on the developing mouse brain. Brain Res. 2007;1144:180–185. doi: 10.1016/j.brainres.2007.01.083. [DOI] [PubMed] [Google Scholar]
- Whitford KL, Dijkhuizen P, Polleux F, Ghosh A. Molecular control of cortical dendrite development. Annu Rev Neurosci. 2002;25:127–149. doi: 10.1146/annurev.neuro.25.112701.142932. [DOI] [PubMed] [Google Scholar]
- Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Wilkinson AR. The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch Dis Child Fetal Neonatal Ed. 2005;90:F134–F140. doi: 10.1136/adc.2004.052407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamasaki Y, Matsuura N, Shozuhara H, Onodera H, Itoyama Y, Kogure K. Interleukin-1 as a pathogenetic mediator of ischemic brain damage in rats. Stroke. 1995;26:676–680. doi: 10.1161/01.str.26.4.676. [DOI] [PubMed] [Google Scholar]
- Yoon BH, Park CW, Chaiworapongsa T. Intrauterine infection and the development of cerebral palsy. BJOG. 2003;110 Suppl 20:124–127. doi: 10.1016/s1470-0328(03)00063-6. [DOI] [PubMed] [Google Scholar]