Abstract
Oxidized phospholipids accumulate in atherosclerotic lesions, on lipoproteins, in other states of chronic inflammation, on apoptotic cells, necrotic cells and cells exposed to oxidative stress. These lipids regulate the transcription of over 1000 gene, regulating many endothelial functions, by activating several different cell surface receptors and multiple signaling pathways. These lipids also have important effects not involving transcription that regulate cell junctions and leukocyte binding. Thus these lipids are potent regulators of endothelial cell function with broad effects comparable in extent but differing from those of cytokines.
Keywords: Oxidized phospholipids, Ox-PAPC, Kodia PC, POVPC, PEIPC, signaling
Background
In the early 1990s, the first reports were published detailing the effect of phospholipid oxidation products on endothelial cell function. These studies grew out of the observation that minimally oxidized LDL (MM-LDL) could activate endothelial inflammatory functions.1 When MM-LDL was fractionated, oxidized phospholipids were found to be the major source of activity. Because there was very little oxidation of linoleic acid in MM-LDL, the studies with oxidized phospholipids focused on phospholipids containing oxidation products of arachidonic acid that were esterified into glycerol-phosphocholine. Studies showing effects of phospholipid oxidation products on specific endothelial inflammatory and pro-coagulant functions soon followed.2–4 Effects of ether containing phospholipid oxidation products were also reported.5 Though many oxidized phospholipids were shown to be present in MM-LDL and in 1-palmitoyl-2-arachidonyl-sn-glycero-3-phosphorylcholine (PAPC) exposed to air oxidation, three oxidized PAPC (Ox-PAPC) products were extensively studied with respect to cell signaling.6 Two of these contained fragmentation products of arachidonic acid: a 5-carbon aldehyde (POVPC) and a 5-carbon acid (PGPC). The third, an especially active oxidized phospholipid, was shown to be a product of the addition of oxygen to arachidonic acid to form an epoxyisoprostane (PEIPC). The effects of other arachidonate and linoleate fragmentation products on endothelial cell inflammatory function have been more recently reported, including alpha beta unsaturated acids (e.g. Kodia PC)7 and aldehydes (e.g. HOOHA-PC).8 Thus, a large number of phospholipid oxidation products have been shown to effect endothelial inflammatory function.
Initially, bioactive phospholipid oxidation products were shown to be formed in lipoproteins oxidized in the test tubes with UV light and enzymes. It was then shown that cultured cells could cause the formation of active phospholipid oxidation products in LDL.5 Phospholipid oxidation products are increased in atherosclerotic lesions in rabbits, mice and humans. In addition, phospholipid oxidation products were shown to accumulate in cells exposed to oxidative stress, including necrotic cells, apoptotic cells and cells treated with IL-1 beta.9, 10 Within the last several years, phospholipid oxidation products have been demonstrated to accumulate in lipoproteins of individuals at risk for coronary events, especially in Lp (a) containing particles, where they may serve as prognostic indicators.11 These studies suggest the importance of phospholipid oxidation products in atherosclerosis. These oxidation products may also play a role in other chronic inflammatory diseases where they have been shown to accumulate.
Introduction
This review will focus on signaling by phospholipids containing esterified oxidized fatty acids at the sn-2 position. We will also make reference to studies with ether containing phospholipid oxidation products and with lyso PC. We have chosen to focus this review on endothelial cell signaling because of the large amount of detailed work in this cell type. Separate reviews have and are being written to examine effects on other cells. In published studies, our group has demonstrated that Ox-PAPC regulates the transcription of over 1000 genes in endothelial cells.12 Of these, approximately 600 are upregulated and 400 are downregulated after a 4-hour treatment. The regulated genes include genes effecting inflammation, procoagulant activity, redox reaction, sterol metabolism, cell cycle, the unfolded protein response (UPR), and angiogenesis. More targeted in vivo analyses of aortas coated with Ox-PAPC have also demonstrated regulation of transcription of a number of the same genes.13 In addition to transcriptional regulation, several groups have demonstrated effects on signaling, as opposed to transcription, related to changes in cell shape and leukocyte binding to the endothelial cells.4, 14 Thus, the published studies demonstrate important effects of Ox-PAPC on all major aspects of endothelial cell function. The array and cell biology studies have highlighted several transcription factors important in Ox-PAPC action, such as STAT3, SREBP, Nrf2, erg-1, NFAT and transcription factors of the UPR system.15, 16 In this review, we will address the roles of these transcription factors as well as other signaling molecules in Ox-PAPC signaling. Since Ox-PAPC contains a mixture of oxidized phospholipids, studies with the individual phospholipids have also been reported and will be discussed in this review. Several other excellent reviews have covered other aspects of Ox-PAPC signaling. 15, 17
Regulation of Inflammatory Pathways by Oxidized Phospholipids
Oxidized phospholipids have been demonstrated to induce an inflammatory response in endothelial cells. This inflammatory response is characterized by an increase in the deposition of leukocyte binding molecules on the endothelial surface to bind monocytes, and by an increase in the production of chemotactic factors.
Monocyte Binding
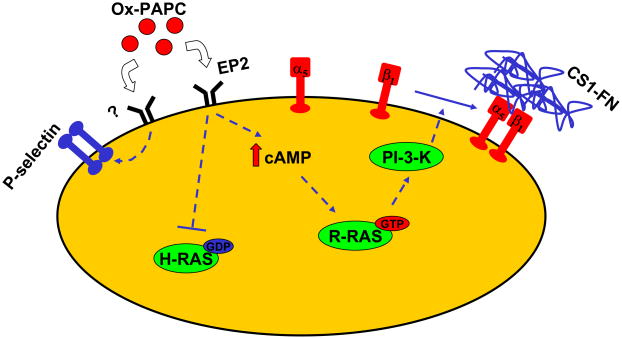
In human aortic EC (HAEC), Ox-PAPC has been demonstrated to promote surface deposition of the CS-1-containing variant of fibronectin (CS1), serving as a ligand for the α4β1 (VLA-4) integrin expressed on the surface of monocytes 4. The deposition of fibronectin is mediated through increasing cAMP levels, leading to the activation of R-Ras and inactivation of H-Ras. R-Ras was shown to activate PI3K, which then results in the activation of α5β1 integrin on the apical surface; this activated integrin binds the fibronectin 18. In fact, it has been shown that inactivation of VLA-4 using a synthetic peptide mimetic of CS1 (4), decreased leukocyte entry and fatty streak formation in mice fed an atherogenic diet (19, 20). Recent findings have also demonstrated a role for the prostaglandin receptor E2 (EP2), a G-protein coupled receptor (GPCR), in this pathway (Figure 1) 21. Agonists of this receptor increased activation of beta 1 integrin. Several groups have obtained evidence that P-Selectin protein expression is increased by oxidized phospholipid, resulting in enhanced release of P-Selectin onto the cell surface by histamine or Ox-LDL 13, 22. Targeted deletion of P-selectin slowed the progression of atherosclerosis in LDL receptor-null mice 23. There is also evidence for an additional pathway regulating monocyte adhesion involving lipoxygenase.24 Treatment of endothelial cells with MM-LDL was shown to cause the release of arachidonic acid; furthermore, monocytes binding induced by MM-LDL and POVPC was reduced by inhibition of the lipoxygenase pathway 25. Furthermore, 12-S-Hete mimicked the effect on monocyte binding and there was evidence for a role of CS-1 fibronectin. The sequence of events in this pathway is not yet determined. Interestingly, the mechanism of leukocyte binding induced by oxidized phospholipids in human EC is different from that of lipopolysaccharide (LPS), tumor necrosis factor α (TNFα), or interleukin 1 (IL-1) which induce both monocyte and neutrophil binding. Ox-PAPC does not upregulate expression of ICAM-1, VCAM-1 and E-selectin and induces only monocyte binding. These properties of Ox-PAPC may indeed explain the selective accumulation of monocytes, rather than neutrophils, in early atherosclerotic lesions.
Figure 1.
Mechanism of Ox-PAPC induced monocyte binding.
Ox-PAPC interacting with EP2 and additional receptors induces an increase in P-Select and a cascade of signaling resulting in activation of alpha 5beta 1 integrin, on the apical surface, which binds fibronectin containing the CS-domain. Monocyte alpha4 beta 1 integrin then binds to the fibronectin.
Chemokine Expression
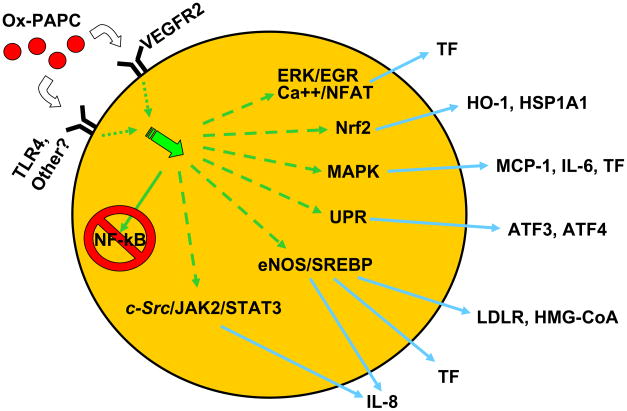
Array data and other studies indicate that Ox-PAPC increases the mRNA levels of a number of chemokines including MCP-1, MIP-1α, MIP-1β, CXCL3, IL-6, IL-8, and GROα 12. These cytokines play important roles in mediating enhanced monocyte/EC adhesion as well as monocyte migration. One interesting feature of Ox-PAPC signaling is the prolonged transcriptional regulation of the chemokines, such as IL-8 and MCP-1, by Ox-PAPC in comparison to traditional cytokines. Ox-PAPC-induced IL-8 transcription, for example, is sustained for at least 18 hours following treatment, with its peak mRNA induction observed at approximately 6 hours following Ox-PAPC treatment.26 This is in comparison to TNF-induced IL-8 transcription, which reaches its peak at 1 hour following treatment and returns to baseline levels at 4 hours. There are multiple signaling pathways controlling this prolonged transcriptional activity (Figure 2). The pathways most extensively studied have been in human aortic endothelial cells (HAEC). Furthermore, most of the pathways discussed below are also activated by PEIPC, the most active pro-inflammatory phospholipid in Ox-PAPC. The rapid activation of IL-8 transcription was demonstrated to be activated by a c-Src/JAK2/STAT3 pathway 27, which is turned on within seconds following Ox-PAPC treatment and returns to baseline levels within 4–6 hours. This pathway directly regulates IL-8 transcription through binding to a novel gamma-interferon activation sequence (GAS) element in the IL-8 promoter. The sustained regulation of IL-8 transcription was found to be mediated by cholesterol depletion and the activation of the uncoupled eNOS/SREBP pathway 28, 29, which is sustained for up to 16 hours after Ox-PAPC treatment in HAEC. Increased binding of SREBP to an SRE element in the IL-8 promoter was also demonstrated. The exact steps causing cholesterol depletion have not yet been determined. However, there is clear involvement of eNOS in SREBP activation. Ox-PAPC treatment was demonstrated to stimulate the activity of eNOS but also promote eNOS uncoupling and the generation of reactive oxygen species (ROS). L-NAME, an inhibitor of eNOS activity, was able to partially inhibit SREBP activation and the expression of known SREBP target genes, such as the LDL receptor (28), by Ox-PAPC. Furthermore, recent findings have also demonstrated a role for VEGFR2 in these pathways 30. In these studies, siRNA against VEGFR2 decreased the transcription of IL-8 and LDL receptor in response to Ox-PAPC, as well as decreasing the activation of SREBP (30). Furthermore, Ox-PAPC-induced VEGFR2 activation was c-Src dependent 30, suggesting potential cross talk between the c-Src/JAK2/STAT3 pathway and the uncoupled eNOS/SREBP pathway. While a role for VEGFR2 in Ox-PAPC induced eNOS activation and uncoupling was not reported, other studies have reported interaction between VEGFR2 and eNOS 31.
Figure 2.
Signaling pathways regulating increased transcription of multiple genes by Ox-PAPC.
Ox-PAPC binding to VEGFR2 and other unknown receptors activates multiple signaling pathways resulting in gene transcription. Ox-PAPC does not activate NfKB and inhibits its activation by a number of TLR ligands.
In addition, ER stress and activation of the unfolded protein response (UPR) pathway have also recently been shown to regulate IL-8 expression in HAEC 32. siRNA-mediated knockdown of transcription factors ATF4 and XBP1, key effectors of the UPR, downregulated both the basal and the Ox-PAPC simulated expression of IL-8 in HAEC. In these studies, a role for the UPR in both the basal and the Ox-PAPC induced expression of IL-6, CXCL3 and MCP-1 in HAEC was also shown.
Several other molecules and receptors have been implicated in the regulation of IL-8 and MCP-1/JE induced by Ox-PAPC. Ox-PAPC, POVPC and PEIPC were demonstrated to activate PPAR alpha and PPAR gamma.33 Using murine aortic EC obtained from PPARα-null mice, a role for PPARα has been demonstrated in the induction of MCP-1 by Ox-PAPC. The role of PPARα in the regulation of chemokine expression by Ox-PAPC in human EC, however, remains controversial. In HeLa cells, a role for TLR4 in activation of IL-8 transcription has also been demonstrated.34 However, effects in HAEC were inconsistent. Interestingly, TLR4 was shown to regulate cell shape changes and MIP-2 synthesis in response to MM-LDL in macrophages.35 These studies suggest differential regulation of chemokine expression by MM-LDL and oxidized lipids across different cell types.
Interestingly, the signaling events activated in EC by Ox-PAPC that regulate chemokine expression are different from those induced by mediators of acute inflammation such as LPS, TNFα and IL-1. The latter agonists induce expression of inflammatory genes rapidly and acutely (with transcriptional activation returning to baseline by 4 hours), and largely act through the activation of the transcription factor, nuclear factor-kappa beta (NFκB). In contrast, Ox-PAPC induces transcriptional regulation of chemokines in a prolonged manner, and through the activation of a different set of transcription factors: STAT3, SREBP, PPAR alpha and UPR. These properties may in part explain the selective chronic inflammatory picture, characterized by monocyte accumulation, observed in atherosclerotic lesions.
Interaction of Oxidized Phospholipids with Other Regulators of Inflammation
Interestingly treatment of cells with Ox-PAPC or its constituent lipids inhibits the effect of LPS, TLR2 ligand and TLR9 ligand on inflammation both in vitro and in vivo.15 The most active Ox-PAPC lipids regulating this inhibition have been identified as alpha beta unsaturated lipids, such as KoDiA PC.7 Several mechanisms have been demonstrated to contribute to this inhibition. Ox-PAPC can form complexes in vitro with CD14 and LBP, thus blocking the binding of LPS.36 In addition, Ox-PAPC effects formation of the TLR4 complex with CD14 by altering caveolar membranes.7 This latter effect appears to be due to activation of neutral sphingomyelinase, which has been demonstrated to alter caveolar function.37 While Ox-PAPC inhibits LPS effects on inflammation, it is actually synergistic with effects of fine diesel exhaust particles found as air-pollutants38 and with TNF alpha.37 The mechanisms regulating these synergisms are not yet known.
Procoagulant activity
Effects of MM-LDL and Ox-PAPC on the synthesis of proteins regulating pro-coagulant activity have been reported in both capillary and aortic endothelial cells. Regulation of this activity can be mediated by changes in molecules that initiate coagulation (tissue factor, TF) or those that regulate the breakdown of small thrombi (plasminogen activator, TPA; plasminogen activator inhibitor PAI; thrombomodulin TM). MM-LDL was shown to regulate all of these activities to promote a procoagulant state.2, 28, 39–42 The signal transduction pathway regulating the induction of TF mRNA levels by Ox-PAPC in HUVEC was shown to be mediated through both a PKC/Erk/EGR-1 pathway and a Ca++/calcineurin/NFAT pathway.39 Both transcription factors, EGR-1 and NFAT, act together in regulating the TF promoter. In a separate study, VEGFR2 was demonstrated to regulate ERK activation and TF expression.30 Thus, VEGFR2 appears to be an important receptor in the regulation of inflammation and coagulation. The mechanism mediating the reduction in TM mRNA levels by Ox-PAPC has also been examined. This inhibition was shown to be due decreased activation of transcription factors RXR, SP1 and RARbeta, known regulators of TM transcription. These studies demonstrate differential regulation of TF and TM transcription by Ox-PAPC, mediated through activation of distinct and separate signaling pathways. In addition, Ox-PAPC was also show to reduce the activity of tissue factor pathway inhibitor (TFPI), a protease inhibitor that inhibits the initial reactions of blood coagulation 42. In these studies, it was concluded that TFPI activity was inhibited through direct interaction of oxidized lipids with the C-terminal basic region of TFPI. In summary, the pro-coagulant activity of oxidized phospholipids is mediated through the activation of several molecular mechanisms.
Angiogenesis
There have been two studies reporting regulation of angiogenesis by phospholipid oxidation products. In the first report, based on hydrolysis by PAF-AH, the authors concluded that oxidized phospholipids in OxLDL for 4 hours inhibited the synthesis of basic FGF by HUVEC and thus were likely to inhibit angiogenesis.40 Their studies, like a number of others, demonstrated that a PAF receptor antagonist could block this effect. However, PAF itself did not have the same effects as OxPAPC. In a more recent report, Bochkov et al. demonstrated both in vivo and in vitro that Ox-PAPC treatment of endothelial cells for 2 days stimulated angiogenesis by increasing level of IL-8, VEGF and COX-2.39 Two specific Ox-PAPC components, POVPC and PGPC, were demonstrated to have this activity when tested at 50ug/ml. They also reported that ERK-1 and NFAT, previously shown to be activated by Ox-PAPC, might play a role in propagating the angiogenic response.
Junctions
Many of the studies discussed above have involved transcriptional regulation. However, other important non-transcriptional effects of oxidized phospholipids have also been described. A large amount of work demonstrates that oxidized phospholipids activate junction formation in pulmonary artery endothelial cells.43 These studies have demonstrated that, both in vitro and in vivo, Ox-PAPC and specifically the epoxycylopentenone-containing phospholipids, increase transendothelial resistance.14 They have shown that the increase in junction formation is due to an increase in Rac activation mediated by activation of PKA, PKC and tyrosine kinases. Furthermore, GTP exchange factors TIAM1 and beta PIX have been identified as the regulators of Rac activation.44 Downstream of Rac, as seen in other systems, Ox-PAPC treatment induces the phosphorylation FAK and Paxillin, which are involved in focal adhesion formation. These studies suggest that oxidized phospholipids protect barrier function in lung endothelial cells.
Regulation of Oxidative Stress
Several studies have demonstrated that treatment of endothelial cells with Ox-PAPC induces oxidative stress. Rouhanizadeh et al. demonstrated that glutathione was depleted in response to Ox-PAPC treatment in bovine aortic endothelial cells and that NADPH oxidase was the source superoxide induction by Ox-PAPC, which led to glutathione depletion.45 Therond et al. observed a decrease in glutathione levels in response to short chain polar lipid derivatives in endothelial cells.46 Gharavi et al. demonstrated that superoxide produced by uncoupled e-NOS also is a source of ROS.28 Increased mitochondrial metabolism may also play a role as has been seen for fatty acid oxidation products 47. Whatever the source of ROS, Ox-PAPC clearly induces transcription of anti-oxidant enzymes including HO-1, glutathione synthase, thioredoxin reductase and glutathione reductase. A newly recognized anti-oxidant gene, OKL 38, is also induced by Ox-PAPC. Regulation of HO-1 transcription has been examined by two groups, who have identified two different pathways involved in this regulation: Kronke et al. identified a MAP kinase/CREB pathway of activation in HUVEC48, while Li et al. identified a pathway involving the activation of Nrf216 in HAEC. Induction of these antioxidant enzymes is likely to protect the cell from cell death, which is negligible in response to Ox-PAPC.
Covalent Binding of Ox-PAPC
Other reviews have covered this subject. However, it is important to recognize that covalent binding of oxidized phospholipids to proteins has been demonstrated and that this binding has been shown to effect protein function (49, 50).
Conclusion
We are beginning to understand the multiple signaling mechanisms by which oxidized phospholipids interact with endothelial cells to activate some processes and inhibit others. Ox-PAPC and individual phospholipids from Ox-PAPC were shown to activate multiple cell signaling pathways and transcription factors. The fact that oxidized phospholipids are present at many sites of chronic inflammation and in blood suggests that they play a prominent role in the regulation of endothelial function. Because these lipids are more difficult to prepare and test, we are at an early stage in our understanding of lipid signaling, that is, in comparison to our understanding of cytokine signaling. However, similar to cytokine signaling, it is clear that multiple pathways are involved in lipid signaling that effect all of the major functions of endothelial cells.
Acknowledgments
Grant Support: PO1 HL30568 and RO1 HL 064731 (JB), AHA Western States Fellowship (NG)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Watson AD, Leitinger N, Navab M, Faull KF, Horkko S, Witztum JL, Palinski W, Schwenke D, Salomon RG, Sha W, Subbanagounder G, Fogelman AM, Berliner JA. Structural identification by mass spectrometry of oxidized phospholipids in minimally oxidized low density lipoprotein that induce monocyte/endothelial interactions and evidence for their presence in vivo. J Biol Chem. 1997;272:13597–13607. doi: 10.1074/jbc.272.21.13597. [DOI] [PubMed] [Google Scholar]
- 2.Drake TA, Hannani K, Fei HH, Lavi S, Berliner JA. Minimally oxidized low-density lipoprotein induces tissue factor expression in cultured human endothelial cells. Am J Pathol. 1991;138:601–607. [PMC free article] [PubMed] [Google Scholar]
- 3.Leitinger N, Tyner TR, Oslund L, Rizza C, Subbanagounder G, Lee H, Shih PT, Mackman N, Tigyi G, Territo MC, Berliner JA, Vora DK. Structurally similar oxidized phospholipids differentially regulate endothelial binding of monocytes and neutrophils. Proc Natl Acad Sci U S A. 1999;96:12010–12015. doi: 10.1073/pnas.96.21.12010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shih PT, Elices MJ, Fang ZT, Ugarova TP, Strahl D, Territo MC, Frank JS, Kovach NL, Cabanas C, Berliner JA, Vora DK. Minimally modified low-density lipoprotein induces monocyte adhesion to endothelial connecting segment-1 by activating beta1 integrin. J Clin Invest. 1999;103:613–625. doi: 10.1172/JCI5710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marathe GK, Prescott SM, Zimmerman GA, McIntyre TM. Oxidized LDL contains inflammatory PAF-like phospholipids. Trends Cardiovasc Med. 2001;11:139–142. doi: 10.1016/s1050-1738(01)00100-1. [DOI] [PubMed] [Google Scholar]
- 6.Berliner JA, Subbanagounder G, Leitinger N, Watson AD, Vora D. Evidence for a role of phospholipid oxidation products in atherogenesis. Trends Cardiovasc Med. 2001;11:142–147. doi: 10.1016/s1050-1738(01)00098-6. [DOI] [PubMed] [Google Scholar]
- 7.Walton KA, Cole AL, Yeh M, Subbanagounder G, Krutzik SR, Modlin RL, Lucas RM, Nakai J, Smart EJ, Vora DK, Berliner JA. Specific phospholipid oxidation products inhibit ligand activation of toll-like receptors 4 and 2. Arterioscler Thromb Vasc Biol. 2003;23:1197–1203. doi: 10.1161/01.ATV.0000079340.80744.B8. [DOI] [PubMed] [Google Scholar]
- 8.Subbanagounder G, Deng Y, Borromeo C, Dooley AN, Berliner JA, Salomon RG. Hydroxy alkenal phospholipids regulate inflammatory functions of endothelial cells. Vascul Pharmacol. 2002;38:201–209. doi: 10.1016/s1537-1891(02)00170-2. [DOI] [PubMed] [Google Scholar]
- 9.Huber J, Vales A, Mitulovic G, Blumer M, Schmid R, Witztum JL, Binder BR, Leitinger N. Oxidized membrane vesicles and blebs from apoptotic cells contain biologically active oxidized phospholipids that induce monocyte-endothelial interactions. Arterioscler Thromb Vasc Biol. 2002;22:101–107. doi: 10.1161/hq0102.101525. [DOI] [PubMed] [Google Scholar]
- 10.Subbanagounder G, Wong JW, Lee H, Faull KF, Miller E, Witztum JL, Berliner JA. Epoxyisoprostane and epoxycyclopentenone phospholipids regulate monocyte chemotactic protein-1 and interleukin-8 synthesis. Formation of these oxidized phospholipids in response to interleukin-1beta. J Biol Chem. 2002;277:7271–7281. doi: 10.1074/jbc.M107602200. [DOI] [PubMed] [Google Scholar]
- 11.Kiechl S, Willeit J, Mayr M, Viehweider B, Oberhollenzer M, Kronenberg F, Wiedermann CJ, Oberthaler S, Xu Q, Witztum JL, Tsimikas S. Oxidized phospholipids, lipoprotein(a), lipoprotein-associated phospholipase A2 activity, and 10-year cardiovascular outcomes: prospective results from the Bruneck study. Arterioscler Thromb Vasc Biol. 2007;27:1788–1795. doi: 10.1161/ATVBAHA.107.145805. [DOI] [PubMed] [Google Scholar]
- 12.Gargalovic PS, Imura M, Zhang B, Gharavi NM, Clark MJ, Pagnon J, Yang WP, He A, Truong A, Patel S, Nelson SF, Horvath S, Berliner JA, Kirchgessner TG, Lusis AJ. Identification of inflammatory gene modules based on variations of human endothelial cell responses to oxidized lipids. Proc Natl Acad Sci U S A. 2006;103:12741–12746. doi: 10.1073/pnas.0605457103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Furnkranz A, Schober A, Bochkov VN, Bashtrykov P, Kronke G, Kadl A, Binder BR, Weber C, Leitinger N. Oxidized phospholipids trigger atherogenic inflammation in murine arteries. Arterioscler Thromb Vasc Biol. 2005;25:633–638. doi: 10.1161/01.ATV.0000153106.03644.a0. [DOI] [PubMed] [Google Scholar]
- 14.Birukov KG, Bochkov VN, Birukova AA, Kawkitinarong K, Rios A, Leitner A, Verin AD, Bokoch GM, Leitinger N, Garcia JG. Epoxycyclopentenone-containing oxidized phospholipids restore endothelial barrier function via Cdc42 and Rac. Circ Res. 2004;95:892–901. doi: 10.1161/01.RES.0000147310.18962.06. [DOI] [PubMed] [Google Scholar]
- 15.Bochkov VN. Inflammatory profile of oxidized phospholipids. Thromb Haemost. 2007;97:348–354. [PubMed] [Google Scholar]
- 16.Li R, Chen W, Yanes R, Lee S, Berliner JA. OKL38 is an oxidative stress response gene stimulated by oxidized phospholipids. J Lipid Res. 2007;48:709–715. doi: 10.1194/jlr.M600501-JLR200. [DOI] [PubMed] [Google Scholar]
- 17.Gleissner CA, Leitinger N, Ley K. Effects of native and modified low-density lipoproteins on monocyte recruitment in atherosclerosis. Hypertension. 2007;50:276–283. doi: 10.1161/HYPERTENSIONAHA.107.089854. [DOI] [PubMed] [Google Scholar]
- 18.Cole AL, Subbanagounder G, Mukhopadhyay S, Berliner JA, Vora DK. Oxidized phospholipid-induced endothelial cell/monocyte interaction is mediated by a cAMP-dependent R-Ras/PI3-kinase pathway. Arterioscler Thromb Vasc Biol. 2003;23:1384–1390. doi: 10.1161/01.ATV.0000081215.45714.71. [DOI] [PubMed] [Google Scholar]
- 19.Huo Y, Hafezi-Moghadam A, Ley K. Role of vascular cell adhesion molecule-1 and fibronectin connecting segment-1 in monocyte rolling and adhesion on early atherosclerotic lesions. Circ Res. 2000;87:153–159. doi: 10.1161/01.res.87.2.153. [DOI] [PubMed] [Google Scholar]
- 20.Shih PT, Brennan ML, Vora DK, Territo MC, Strahl D, Elices MJ, Lusis AJ, Berliner JA. Blocking very late antigen-4 integrin decreases leukocyte entry and fatty streak formation in mice fed an atherogenic diet. Circ Res. 1999;84:345–351. doi: 10.1161/01.res.84.3.345. [DOI] [PubMed] [Google Scholar]
- 21.Li R, Mouillesseaux KP, Montoya D, Cruz D, Gharavi N, Dun M, Koroniak L, Berliner JA. Identification of prostaglandin E2 receptor subtype 2 as a receptor activated by OxPAPC. Circ Res. 2006;98:642–650. doi: 10.1161/01.RES.0000207394.39249.fc. [DOI] [PubMed] [Google Scholar]
- 22.Vora DK, Fang ZT, Liva SM, Tyner TR, Parhami F, Watson AD, Drake TA, Territo MC, Berliner JA. Induction of P-selectin by oxidized lipoproteins. Separate effects on synthesis and surface expression. Circ Res. 1997;80:810–818. doi: 10.1161/01.res.80.6.810. [DOI] [PubMed] [Google Scholar]
- 23.Dong ZM, Chapman SM, Brown AA, Frenette PS, Hynes RO, Wagner DD. The combined role of P- and E-selectins in atherosclerosis. J Clin Invest. 1998;102:145–152. doi: 10.1172/JCI3001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Honda HM, Leitinger N, Frankel M, Goldhaber JI, Natarajan R, Nadler JL, Weiss JN, Berliner JA. Induction of monocyte binding to endothelial cells by MM-LDL: role of lipoxygenase metabolites. Arterioscler Thromb Vasc Biol. 1999;19:680–686. doi: 10.1161/01.atv.19.3.680. [DOI] [PubMed] [Google Scholar]
- 25.Patricia MK, Kim JA, Harper CM, Shih PT, Berliner JA, Natarajan R, Nadler JL, Hedrick CC. Lipoxygenase products increase monocyte adhesion to human aortic endothelial cells. Arterioscler Thromb Vasc Biol. 1999;19:2615–2622. doi: 10.1161/01.atv.19.11.2615. [DOI] [PubMed] [Google Scholar]
- 26.Yeh M, Leitinger N, de Martin R, Onai N, Matsushima K, Vora DK, Berliner JA, Reddy ST. Increased transcription of IL-8 in endothelial cells is differentially regulated by TNF-alpha and oxidized phospholipids. Arterioscler Thromb Vasc Biol. 2001;21:1585–1591. doi: 10.1161/hq1001.097027. [DOI] [PubMed] [Google Scholar]
- 27.Gharavi NM, Alva JA, Mouillesseaux KP, Lai C, Yeh M, Yeung W, Johnson J, Szeto WL, Hong L, Fishbein M, Wei L, Pfeffer LM, Berliner JA. Role of the Jak/STAT pathway in the regulation of interleukin-8 transcription by oxidized phospholipids in vitro and in atherosclerosis in vivo. J Biol Chem. 2007;282:31460–31468. doi: 10.1074/jbc.M704267200. [DOI] [PubMed] [Google Scholar]
- 28.Gharavi NM, Baker NA, Mouillesseaux KP, Yeung W, Honda HM, Hsieh X, Yeh M, Smart EJ, Berliner JA. Role of endothelial nitric oxide synthase in the regulation of SREBP activation by oxidized phospholipids. Circ Res. 2006;98:768–776. doi: 10.1161/01.RES.0000215343.89308.93. [DOI] [PubMed] [Google Scholar]
- 29.Yeh M, Cole AL, Choi J, Liu Y, Tulchinsky D, Qiao JH, Fishbein MC, Dooley AN, Hovnanian T, Mouilleseaux K, Vora DK, Yang WP, Gargalovic P, Kirchgessner T, Shyy JY, Berliner JA. Role for sterol regulatory element-binding protein in activation of endothelial cells by phospholipid oxidation products. Circ Res. 2004;95:780–788. doi: 10.1161/01.RES.0000146030.53089.18. [DOI] [PubMed] [Google Scholar]
- 30.Zimman A, Mouillesseaux KP, Le T, Gharavi NM, Ryvkin A, Graeber TG, Chen TT, Watson AD, Berliner JA. Vascular endothelial growth factor receptor 2 plays a role in the activation of aortic endothelial cells by oxidized phospholipids. Arterioscler Thromb Vasc Biol. 2007;27:332–338. doi: 10.1161/01.ATV.0000252842.57585.df. [DOI] [PubMed] [Google Scholar]
- 31.Jin ZG, Ueba H, Tanimoto T, Lungu AO, Frame MD, Berk BC. Ligand-independent activation of vascular endothelial growth factor receptor 2 by fluid shear stress regulates activation of endothelial nitric oxide synthase. Circ Res. 2003;93:354–363. doi: 10.1161/01.RES.0000089257.94002.96. [DOI] [PubMed] [Google Scholar]
- 32.Gargalovic PS, Gharavi NM, Clark MJ, Pagnon J, Yang WP, He A, Truong A, Baruch-Oren T, Berliner JA, Kirchgessner TG, Lusis AJ. The unfolded protein response is an important regulator of inflammatory genes in endothelial cells. Arterioscler Thromb Vasc Biol. 2006;26:2490–2496. doi: 10.1161/01.ATV.0000242903.41158.a1. [DOI] [PubMed] [Google Scholar]
- 33.Lee H, Shi W, Tontonoz P, Wang S, Subbanagounder G, Hedrick CC, Hama S, Borromeo C, Evans RM, Berliner JA, Nagy L. Role for peroxisome proliferator-activated receptor alpha in oxidized phospholipid-induced synthesis of monocyte chemotactic protein-1 and interleukin-8 by endothelial cells. Circ Res. 2000;87:516–521. doi: 10.1161/01.res.87.6.516. [DOI] [PubMed] [Google Scholar]
- 34.Walton KA, Hsieh X, Gharavi N, Wang S, Wang G, Yeh M, Cole AL, Berliner JA. Receptors involved in the oxidized 1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphorylcholine-mediated synthesis of interleukin-8. A role for Toll-like receptor 4 and a glycosylphosphatidylinositol-anchored protein. J Biol Chem. 2003;278:29661–29666. doi: 10.1074/jbc.M300738200. [DOI] [PubMed] [Google Scholar]
- 35.Miller YI, Viriyakosol S, Worrall DS, Boullier A, Butler S, Witztum JL. Toll-like receptor 4-dependent and -independent cytokine secretion induced by minimally oxidized low-density lipoprotein in macrophages. Arterioscler Thromb Vasc Biol. 2005;25:1213–1219. doi: 10.1161/01.ATV.0000159891.73193.31. [DOI] [PubMed] [Google Scholar]
- 36.Bochkov VN, Kadl A, Huber J, Gruber F, Binder BR, Leitinger N. Protective role of phospholipid oxidation products in endotoxin-induced tissue damage. Nature. 2002;419:77–81. doi: 10.1038/nature01023. [DOI] [PubMed] [Google Scholar]
- 37.Walton KA, Gugiu BG, Thomas M, Basseri RJ, Eliav DR, Salomon RG, Berliner JA. A role for neutral sphingomyelinase activation in the inhibition of LPS action by phospholipid oxidation products. J Lipid Res. 2006;47:1967–1974. doi: 10.1194/jlr.M600060-JLR200. [DOI] [PubMed] [Google Scholar]
- 38.Gong KW, Zhao W, Li N, Barajas B, Kleinman M, Sioutas C, Horvath S, Lusis AJ, Nel A, Araujo JA. Air-pollutant chemicals and oxidized lipids exhibit genome-wide synergistic effects on endothelial cells. Genome Biol. 2007;8:R149. doi: 10.1186/gb-2007-8-7-r149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bochkov VN, Mechtcheriakova D, Lucerna M, Huber J, Malli R, Graier WF, Hofer E, Binder BR, Leitinger N. Oxidized phospholipids stimulate tissue factor expression in human endothelial cells via activation of ERK/EGR-1 and Ca(++)/NFAT. Blood. 2002;99:199–206. doi: 10.1182/blood.v99.1.199. [DOI] [PubMed] [Google Scholar]
- 40.Chang PY, Luo S, Jiang T, Lee YT, Lu SC, Henry PD, Chen CH. Oxidized low-density lipoprotein downregulates endothelial basic fibroblast growth factor through a pertussis toxin-sensitive G-protein pathway: mediator role of platelet-activating factor-like phospholipids. Circulation. 2001;104:588–593. doi: 10.1161/hc3101.092213. [DOI] [PubMed] [Google Scholar]
- 41.Ishii H, Tezuka T, Ishikawa H, Takada K, Oida K, Horie S. Oxidized phospholipids in oxidized low-density lipoprotein down-regulate thrombomodulin transcription in vascular endothelial cells through a decrease in the binding of RARbeta-RXRalpha heterodimers and Sp1 and Sp3 to their binding sequences in the TM promoter. Blood. 2003;101:4765–4774. doi: 10.1182/blood-2002-08-2428. [DOI] [PubMed] [Google Scholar]
- 42.Ohkura N, Hiraishi S, Itabe H, Hamuro T, Kamikubo Y, Takano T, Matsuda J, Horie S. Oxidized phospholipids in oxidized low-density lipoprotein reduce the activity of tissue factor pathway inhibitor through association with its carboxy-terminal region. Antioxid Redox Signal. 2004;6:705–712. doi: 10.1089/1523086041361686. [DOI] [PubMed] [Google Scholar]
- 43.Birukova AA, Chatchavalvanich S, Oskolkova O, Bochkov VN, Birukov KG. Signaling pathways involved in OxPAPC-induced pulmonary endothelial barrier protection. Microvasc Res. 2007;73:173–181. doi: 10.1016/j.mvr.2006.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Birukova AA, Malyukova I, Mikaelyan A, Fu P, Birukov KG. Tiam1 and betaPIX mediate Rac-dependent endothelial barrier protective response to oxidized phospholipids. J Cell Physiol. 2007;211:608–617. doi: 10.1002/jcp.20966. [DOI] [PubMed] [Google Scholar]
- 45.Rouhanizadeh M, Hwang J, Clempus RE, Marcu L, Lassegue B, Sevanian A, Hsiai TK. Oxidized-1-palmitoyl-2-arachidonoyl-sn-glycero-3-phosphorylcholine induces vascular endothelial superoxide production: implication of NADPH oxidase. Free Radic Biol Med. 2005;39:1512–1522. doi: 10.1016/j.freeradbiomed.2005.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Therond P, Abella A, Laurent D, Couturier M, Chalas J, Legrand A, Lindenbaum A. In vitro study of the cytotoxicity of isolated oxidized lipid low-density lipoproteins fractions in human endothelial cells: relationship with the glutathione status and cell morphology. Free Radic Biol Med. 2000;28:585–596. doi: 10.1016/s0891-5849(99)00265-8. [DOI] [PubMed] [Google Scholar]
- 47.Landar A, Zmijewski JW, Dickinson DA, Le Goffe C, Johnson MS, Milne GL, Zanoni G, Vidari G, Morrow JD, Darley-Usmar VM. Interaction of electrophilic lipid oxidation products with mitochondria in endothelial cells and formation of reactive oxygen species. Am J Physiol Heart Circ Physiol. 2006;290:H1777–1787. doi: 10.1152/ajpheart.01087.2005. [DOI] [PubMed] [Google Scholar]
- 48.Kronke G, Bochkov VN, Huber J, Gruber F, Bluml S, Furnkranz A, Kadl A, Binder BR, Leitinger N. Oxidized phospholipids induce expression of human heme oxygenase-1 involving activation of cAMP-responsive element-binding protein. J Biol Chem. 2003;278:51006–51014. doi: 10.1074/jbc.M304103200. [DOI] [PubMed] [Google Scholar]
- 49.Gugiu BG, Mouillesseaux K, Duong V, Herzog T, Hekimian A, Koroniak L, Vondriska TM, Watson AD. Protein targets of oxidized phospholipids in endothelial cells. J Lipid Res. 2008;49:510–520. doi: 10.1194/jlr.M700264-JLR200. [DOI] [PubMed] [Google Scholar]
- 50.Salomon RG. Isolevuglandins, oxidatively truncated phospholipids, and atherosclerosis. Ann N Y Acad Sci. 2005;1043:327–342. doi: 10.1196/annals.1333.040. [DOI] [PubMed] [Google Scholar]