Abstract
Purpose
To compare the effectiveness of the Lea Symbols and the HOTV distance visual acuity (VA) tests, presented monocularly in linear, crowded formats at 3 m, as vision screening tests to identify three- to five-year-old children in need of eye care.
Methods
Subjects were 1,142 three- to five-year-old Head Start children who completed a comprehensive eye examination, used to determine if the child had one or more targeted conditions: amblyopia, strabismus, significant refractive error, or unexplained reduced VA. Each child was tested on both tests by masked examiners, with test order determined randomly. The optotype sizes administered were age-based according to the child’s age at school entry on September 1. Children age three were tested with 10/100, 10/32, 10/25, and 10/20 optotypes while those who were four were tested with 10/100, 10/25, 10/20, and 10/16 optotypes.
Results
Most children (>95%) completed both tests, with no statistically significant differences. Pass/fail cut-offs were set to yield specificities as close as possible to 90%. The largest sensitivity differences observed were in the three-year-old group (mean age 45.3 months), where the sensitivity for detection of ≥1 targeted conditions was 61% for the Lea Symbols and was 46% for the HOTV letters (difference 15%, 95% confidence interval {−0.01, 0.30}) and the sensitivity for detection of Group 1 conditions was 83% for the Lea Symbols and 57% for the HOTV letters (difference 26%, 95% confidence interval {−0.01, 0.49}). However, neither these differences nor any of the other age group sensitivity differences were statistically significant. For the three-year-olds, the pass/fail criterion was one line larger for the HOTV letters than for the Lea Symbols.
Conclusions
Most children completed both tests. While the three-year-olds achieved better acuity scores with the Lea Symbols test, there were no statistically significant differences in sensitivity between tests for any age group.
Keywords: visual acuity, HOTV letter optotypes, Lea Symbols, preschool vision screening, children’s vision
Essential components for effective use of screening recognition visual acuity (VA) tests for detection of vision disorders in preschool-aged children are the ability of the child to perform the task (testability) and the ability of the test to accurately differentiate those children who have an ocular disorder from those children who do not (sensitivity and specificity). In 2000, a task force on Vision Screening in the Preschool Child1 recommended two sets of optotypes, Lea Symbols (house, heart, circle, square) and letters (H, O, T, V), to measure VA in preschool children three to five years of age. However, little age-specific information was available concerning the effectiveness of these tests in screening children within this age range.
Hered et al.2 compared testability of Lea Symbols and HOTV letters during vision screening in a group of 777 preschool children (ages three to five) and found that testability rates improved significantly with age for both Lea Symbols and HOTV. The testability difference between the two charts was statistically significant only for three-year-olds, more of whom were testable with Lea Symbols (92%) than with the HOTV test (85%).
Phase I of The Vision In Preschoolers (VIP) Study compared the effectiveness of eleven different vision screening tests in identifying preschool children in need of an eye examination and possible treatment for amblyopia, strabismus, significant refractive error, or unexplained reduced visual acuity.3 Phase I screening tests included both the Lea Symbols distance VA and the HOTV distance VA tests. As previously reported,4 99% of children were able to complete the binocular pretest for both tests and more than 95% of both three-year-olds and four- to five-year-olds were able to complete monocular testing with each test. There was no significant difference between tests in the proportion of children who were testable as a function of the age of the child, although the percentage of children able to complete the pretest increased slightly as the children got older. The data did, however, provide an indication that for three-year-old children, the Lea Symbols test might be easier than the HOTV test. Specifically, in the 41% of instances when a three-year-old child showed better acuity on one of the two tests, it was more often on the Lea Symbols test (26% of children) than on the HOTV test (15% of children). In contrast, four- and five-year-old children were equally likely to perform better on either the Lea Symbols test or on the HOTV test when there was a difference in their performance on the two tests. A preschoolers’ ability to perform a screening test is a prerequisite for successful screening; however, a screening test’s accuracy in separating children with normal vision and children in need of further vision care requires knowing the test’s sensitivity and specificity for detecting targeted vision disorders.
While the prior VIP Phase I reports3, 4 and the Hered et al. report2 provided age-specific information concerning testability for VA tests constructed of Lea Symbols versus HOTV optotypes, neither report provided age-specific data on the sensitivity and specificity of each optotype set (i.e. the effectiveness of each as a screening tool for detecting preschool children with vision disorders). The purpose of the present paper is to compare the effectiveness of the Lea Symbols test and the HOTV test as vision screening tests to identify preschool children in need of further eye care. Effectiveness will be examined with respect to the age of the child at the time of testing and the vision disorders detected.
METHODS
Subjects
In Year 1 of Phase I of the VIP Study, three- to five-year-old children (n=1,195) who were enrolled in Head Start participated in a vision screening and received a comprehensive eye examination conducted by licensed eyecare practitioners (optometrists and ophthalmologists experienced in the care of young children) through one of the five VIP Clinical Centers (Berkeley, CA, Boston, MA, Columbus, OH, Philadelphia, PA, Tahlequah, OK) during the 2001-2002 academic year. Created in 1965, Head Start is a federal government national school readiness program that provides comprehensive education, health, nutrition, and parent involvement services to low-income three- and four-year-old children and their families.
All screenings and examinations took place on specially equipped vision vans that were parked at the child’s school.5 The data in this report come from the 1,142 children with complete eye examination data. Subjects were not a random sample of the Head Start population. Instead, an effort was made to obtain a sample with a high proportion of vision problems, and therefore a wide range of visual acuities. This was accomplished by recruiting all children who had failed the local annual Head Start vision screening, along with a random sample of those who had not failed.3 The local annual Head Start vision screening is provided by each Head Start agency and differs among Head Start classrooms. The national Head Start organization mandates that children receive a vision screening but does not specify what screening tests must be used.
This research was approved by the appropriate Institutional Review Boards associated with each clinical center. Each child’s parent/guardian provided written informed consent prior to testing.
Visual Acuity (VA) Screening Tests
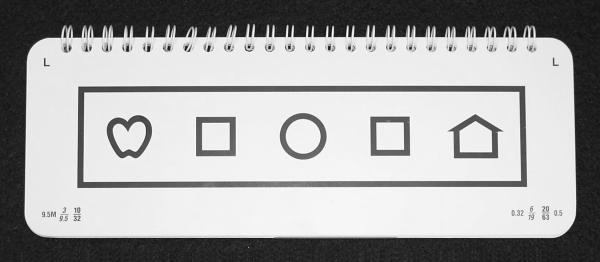
Each child’s VA was screened at a 3 m (10 ft) test distance using the linear, crowded Lea Symbols6 distance VA test and the linear, crowded HOTV distance VA test. The commercially available tests were constructed (Precision Vision, LaSalle, IL) as cards each containing a single line of optotypes for one VA level,7 surrounded on all four sides by a bar (crowding rectangle), as shown in Figure 1. For both charts and for each optotype size, the average distance between optotypes was approximately one optotype width, and the average distance between the optotypes and the crowding rectangle was approximately 0.5 optotype width (see Appendix A).
Figure 1.
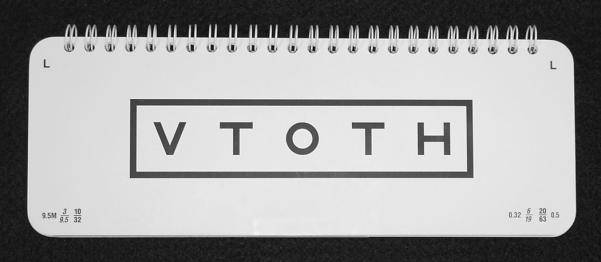
Photograph of 10/32 line from one page of one flip book from the Lea Symbols test (A) and the HOTV test (B). Reprinted from The Vision in Preschoolers Study Group. Preschool visual acuity screening with HOTV and Lea Symbols: Testability and between-test agreement. Optom Vis Sci 2004;81:678-83.
The optotype size and stroke width for the Lea Symbols were based on the test developer’s empirical determination of overall optotype size and stroke width necessary to produce equal VA thresholds in response to blur.6 The size of the Lea Symbols has been further adjusted by the developer (Dr. Hyvärinen) since the VIP Study investigation reported here; therefore some currently available commercial tests may contain optotype sizes different from those used in this study. See Appendix A for a description of the Lea Symbols optotype sizes used in the VIP Study.
Each of the HOTV letters conformed to the standard definitions for VA, in which letters each subtend 5 minutes of arc in height and 1 minute of arc in stroke width and critical details at the specified test distance.8 The HOTV optotypes also subtended a visual angle of 5 minutes of arc in width, which is similar to the format of optotypes in the ETDRS letter charts used in standard clinical trial assessment of VA in adults.9
Visual Acuity Screening Procedure
Details of the procedure have been published previously.3, 4 Each of the two visual acuity screening tests was administered to the child by a different optometrist or ophthalmologist who was trained and certified in the VIP Study screening protocols. Each child had monocular VA screened with both the Lea Symbols test and the HOTV test, with the order of testing randomly assigned. Testers were masked to the child’s local agency Head Start screening results, to the results of the other VA test, and to whether the child wore spectacles. When a child came to the screening wearing spectacles, the Project Coordinator removed them before the examiner saw the child.
For both the Lea Symbols and HOTV tests, the test sequence consisted of (1) binocular pretesting at approximately 1 m with crowded, single, large (approximately 7 cm square including the crowding bars) optotypes; (2) monocular testing of the right eye at 3 m; and (3) monocular testing of the left eye at 3 m. The child named or matched optotypes using a lap card. Pretesting was performed to determine if the child understood and could perform the (matching or naming) task required. The pretest was presented at 1 m to allow the tester to more easily capture the child’s attention before moving back to the 3 m distance. The pretesting letters were large enough to be seen clearly and comfortably by most children. Children who could not complete the binocular pretest were classified as “unable” and were included in the analysis as screening failures. Children who are “unable” on a visual acuity screening test have been shown to be more than twice as likely to have an ocular condition as children who completed the pretest.10
For all children, monocular testing began with the 3/30 (10/100) line. at 3 m followed by testing with age-specific optotype sizes. Children who were three years of age on September 1, 2001, were tested with isolated, crowded lines of optotypes equivalent to acuity levels of 3/30 (10/100), 3/9.6 (10/32), 3/7.5 (10/25), and 3/6 (10/20). Children who were four years of age on September 1, 2001 were tested with isolated crowded lines of optotypes equivalent to acuity levels of 3/30 (10/100), 3/7.5 (10/25), 3/6 (10/20), and 3/4.8 (10/16). Different optotype orders were used for testing right and left eyes. Testing continued until the child failed to name or match three out of three or three out of four optotypes on a line, or until the child identified three out of three or three out of four optotypes on the smallest age-specific optotype size. The screening VA was recorded as the smallest optotype size for which the child was able to identify three out of three or three out of four optotypes.
Eye Examination Procedures
As described previously,3 each child underwent a standardized comprehensive eye examination conducted in the VIP mobile vision van by a study-certified optometrist or ophthalmologist experienced in working with children who was masked to the results of all screening tests. Testing included measurement of monocular threshold VA using the Electronic Visual Acuity (EVA) tester,11-13 a distance and near cover test, and cycloplegic retinoscopy. Results of the eye examination were used to determine whether a child had one or more of the four VIP Study targeted conditions: amblyopia, strabismus, significant refractive error, or unexplained reduced VA. Children who had one or more VIP Study targeted conditions at the most severe levels were identified as having Group 1 conditions, very important to detect and treat early. Definitions of each targeted condition and Group 1 conditions have been published previously3 and are reproduced in Tables 1 and 2.
Table 1.
Definitions of Targeted Disorders in the VIP Studya
| Targeted Disorder |
Definitions (Definitions are applied sequentially for Amblyopia and Reduced VA) |
|---|---|
| Amblyopia | |
| •Presumed Unilateral |
3 line or greater interocular difference in VA AND a unilateral amblyogenic factor* |
| •Suspected Unilateral | 2 line interocular difference in VA AND a unilateral amblyogenic factor* |
| •Suspected Bilateral | |
| ○ 3-year olds | Worse than 20/50 in 1 eye, worse than 20/40 in the contralateral eye, AND a bilateral amblyogenic factor† |
| ○ 4, 5-year olds | Worse than 20/40 in 1 eye, worse than 20/30 in the contralateral eye, AND a bilateral amblyogenic factor† |
|
| |
| Reduced VA ** | |
| •Bilateral | |
| ○ 3-year olds | Worse than 20/50 in 1 eye, worse than 20/40 in the contralateral eye; no bilateral amblyogenic factor† |
| ○ 4, 5-year olds | Worse than 20/40 in 1 eye, worse than 20/30 in the contralateral eye; no bilateral amblyogenic factor† |
| • Unilateral | |
| ○ 3-year olds | Worse than 20/50 in only 1 eye OR 2 line or greater difference between the eyes (except 20/16, 20/25); no unilateral amblyogenic factor* |
| ○ 4, 5-year olds | Worse than 20/40 in only 1 eye OR 2 line or greater difference between the eyes (except 20/16, 20/25); no unilateral amblyogenic factor* |
| Strabismus | Any heterotropia in primary gaze |
|---|---|
|
Significant Refractive
Error |
(cycloplegic refraction) |
| •Astigmatism | > 1.50 D between principal meridians |
| •Hyperopia | > 3.25 D in any meridian |
| •Myopia | > 2.00 D in any meridian > 1.00 D interocular difference in hyperopia; > 3.00 D interocular difference in myopia; |
| •Anisometropia | > 1.50 D interocular difference in astigmatism; Antimetropic*** difference >1.00 D and one eye > 1.00 D hyperopia; Antimetropic*** difference >3.00 D and 1 eye >2.00 D myopia |
Strabismus, anisometropia (as defined in Table 1), or a difference in spherical equivalent of ≥0.50 D when at least one eye had >3.50 D of hyperopia were considered unilateral amblyogenic factors.
Astigmatism > 2.50 D, or hyperopia > 5.00 D, or myopia > 8.00 D in each eye were considered bilateral amblyogenic factors.
Reduced VA not due to amblyopia or refractive error
Antimetropia equals 1 eye hyperopic, 1 eye myopic
Reprinted from Ophthalmology;111(4), The Vision in Preschoolers Study Group. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision in Preschoolers Study. Table 2, p 641
Table 2.
Definitions of Group 1 (Very Important to Detect and Treat Early) Conditions in the VIP Study3
| Amblyopia |
| Presumed Unilateral: ≥ 3 line interocular difference, a unilateral amblyogenic factor*, and worse eye VA ≤ 20/64 |
| Suspected Bilateral: a bilateral amblyogenic factor, worse eye VA < 20/50 for 3-year- olds or < 20/40 for 4-year-olds, contralateral eye VA worse than 20/40 for 3-year- olds or 20/30 for 4-year-olds |
|
|
|
Strabismus: Constant in primary gaze |
| Refractive Error |
| Hyperopia ≥ 5.0 D |
| Astigmatism ≥ 2.5 D |
| Myopia ≥ 6.0 D |
Strabismus, anisometropia (as defined in Table 1), or a difference in spherical equivalent of ≥0.50 D when at least one eye had >3.50 D of hyperopia were considered unilateral amblyogenic factors.
Data Analysis
Analysis of screening results was conducted based on the age of the child at the time of testing. However, the set of optotypes used for screening was based on the child’s age on September 1, 2001. Therefore, the data include “young” four-year-olds who were four years of age when tested, but three years of age on September 1 and tested with the age-specific optotypes for three-year-olds; and “old” four-year-olds who were four years of age both on September 1 and at the time of testing and were tested with the age-specific optotypes for four-year-olds. The five-year-olds were four years of age on September 1 and were tested with the age-specific optotypes for four-year-olds.
The sensitivity when the failure criterion was selected to provide specificity as close as possible to 90% was compared between the two VA tests using the exact McNemar’s test for paired proportions. The sensitivity/specificity calculation and receiver operating characteristic (ROC) analysis are child-specific versus eye-specific, and a child was defined as a screening failure if one or both eyes met the failure criterion on a screening test. Children who were unable to perform the pretest for a specific test were considered a screening failure on that test. Confidence intervals for differences in correlated proportions were calculated using Confidence Interval Analysis (CIA) 2.1.1 software (Trevor Bryant, University of Southampton, Great Britain); all other calculations were performed using SAS/STAT 8.0 software (SAS Institute, Inc., 100 SAS Campus Dr., Cary, NC, 27513-2414). The performance of the tests was further characterized by constructing receiver operating characteristic (ROC) curves for each test.
An ROC curve plots sensitivity against the false positive rate (i.e., 1-specificity), in which each point reflects values obtained at a different cutpoint value from a continuous or ordinal measure. ROC analysis provides several advantages over sensitivity and specificity determination for a single cutpoint. (1) Sensitivity and specificity are characteristics of a diagnostic test at a particular cutoff value, while the ROC curve provides an overall picture of the characteristics of the test itself. (2) The trade-off between sensitivity and specificity can be visualized on an ROC plot as the cutpoint value is shifted. However, the commonly applied statistical tests for comparing the area under two ROC curves cannot be applied because the calculation of specificity for VIP data involves a weighted average to adjust the estimate for the sampling proportions used in the study.3 As described above, VIP Study children were not selected randomly. Children who had previously failed the usual and customary annual Head Start agency vision screening were differentially recruited, in comparison to those who passed the screening. It is therefore not possible to calculate positive and negative predictive values from the VIP Study data. For any population where prevalence is known, positive and negative predictive values can be calculated by using the VIP Study sensitivity and specificity data.
RESULTS
Study Population
The age distribution of the 1,142 Head Start children in the study population is provided in Table 3. Because Head Start places children in classrooms based on the child’s age on September 1 of the school year, there is overlap in the age ranges of the younger four-year-old group (who were age three at the beginning of the school year and were tested with screening cards for three-year-olds) and the older four-year-old group (who were age four at the beginning of the school year and were tested with screening cards for four-year-olds). All children were tested with the Lea Symbols screening test, and all but one were tested with the HOTV screening test.
Table 3.
Age distribution of children at testing (N = 1,142).
| Age in Months |
|||
|---|---|---|---|
| Age (Years) | N | Mean (SD) | Range |
| 3 | 215 | 45.3 (1.80) | 41.0 – 47.9 |
| 4 Young§ | 311 | 51.5 (2.05) | 48.0 – 57.0 |
| 4 Old | 297 | 57.0 (1.90) | 52.0 – 59.9 |
| 5* | 319 | 63.1 (2.14) | 60.0 – 68.0 |
4 years old at screening, but tested with screening cards for 3-year-olds.
5 years old at screening, but tested with screening cards for 4-year-olds.
Testability
Testability for all children (n = 1,253) who completed the screening has been reported previously.4 Testability was high for both VA tests and all age groups (>95%). There was no statistically significant difference in testability between the two VA tests for any age group. Six (0.53%) children who were unable to complete the pretest of the Lea Symbols, and nine (0.79%) children who were unable to complete the pretest of the HOTV test were counted as screening failures in the data analysis.
Sensitivity and Specificity
Table 4 shows the sensitivity, when specificity was set as close as possible to 90%, of the Lea Symbols test and the HOTV test for detecting children with ≥1 VIP Study targeted conditions and Group 1 conditions by age group. The largest difference observed was in the three-year-old group where the sensitivity was 61% for the Lea Symbols test and 46% for the HOTV test for detecting ≥1 VIP Study targeted condition; and was 83% for Lea Symbols and 57% for the HOTV test for detecting Group 1 conditions. However, none of the differences between the two tests is statistically significant.
Table 4.
Sensitivity of LEA Symbols VA and HOTV VA for Detecting a Child with ≥1 VIP Study Targeted Condition(s) and Group 1 Conditions with 90% Specificity by Age of Child (N=1,142)§
| Age (Years) |
N (Child with ≥1 Targeted Condition, child with Group 1 Condition) |
VA test | Failure criterion (Inability to pass) |
Sensitivity to detect ≥1 condition (n = 346) |
Sensitivity to detect Group 1 condition (n =139) |
Specificity (n = 796) |
|---|---|---|---|---|---|---|
| 3 | 215 (59, 23) | Lea | 10/25 | 0.61 | 0.83 | 0.90 |
| HOTV | 10/32 | 0.46 | 0.57 | 0.88 | ||
| Difference Lea – HOTV (95% CI) |
0.15 (−0.01, 0.30) |
0.26 (−0.01, 0.49) |
||||
|
| ||||||
| 4 Young | 311 (93, 37) | Lea | 10/25 | 0.57 | 0.73 | 0.91 |
| HOTV | 10/25 | 0.57 | 0.65 | 0.91 | ||
| Difference Lea – HOTV (95% CI) |
0.00 (−0.11, 0.11) |
0.08 (−0.10, 0.26) |
||||
|
| ||||||
| 4 Old | 297 (83, 30) | Lea | 10/20 | 0.65 | 0.83 | 0.90 |
| HOTV | 10/20 | 0.57 | 0.80 | 0.87 | ||
| Difference Lea – HOTV (95% CI) |
0.08 (−0.03, 0.19) |
0.03 (−0.16, 0.22) |
||||
|
| ||||||
| 5 | 319 (111, 49) | Lea | 10/20 | 0.60 | 0.78 | 0.92 |
| HOTV | 10/20 | 0.56 | 0.82 | 0.92 | ||
| Difference Lea – HOTV (95% CI) |
0.04 (−0.04, 0.13) |
−0.04 (−0.16, 0.07) |
||||
When 90% specificity is not achievable, the specificity closest to 90% was chosen.
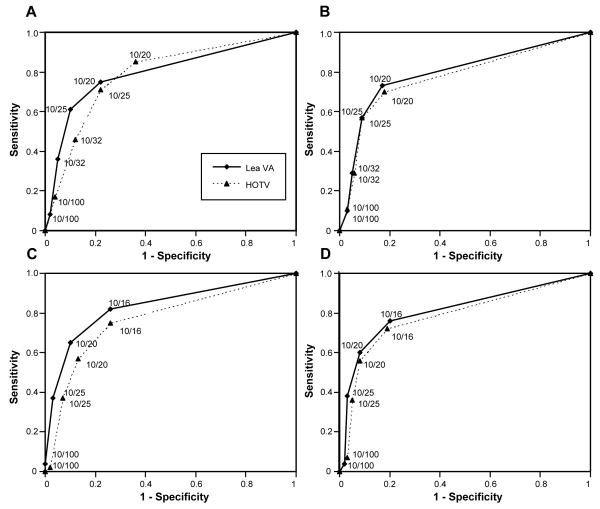
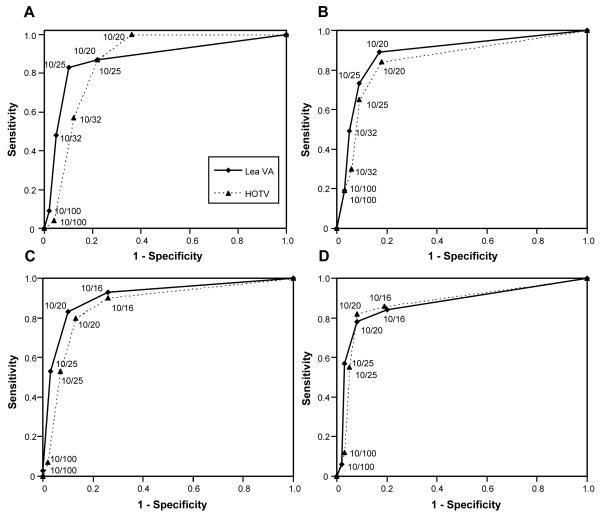
Figures 2A-D show the ROC curves for the two tests for detecting ≥1 VIP Study targeted condition for each of the four age groups. Figures 3A-D show the ROC curves for the two tests for detecting children with Group 1 conditions. For three-year-olds, as shown in Table 4 and Figure 2A and 3A, different failure criteria for the two VA tests allowed comparison as close to 90% specificity as possible. When the test performance among the three-year-old children was compared at the same failure criterion (10/32, 10/25, or 10/20), the sensitivity was higher and the specificity was lower for the HOTV test than for the Lea Symbols test. That is, fewer children could read the HOTV optotype of any given size than the Lea Symbol optotype of the same size regardless of whether the children had a targeted condition or not.
Figure 2.
The ROC curves for the Lea Symbols and HOTV Test for all VIP Study targeted conditions for each of the four age-specific groups of children. (A) Age 3; (B) Age 4 younger; (C) Age 4 older; and (D) Age 5
Figure 3.
The ROC curves for the Lea Symbols and HOTV Test for VIP Group 1 conditions for each of the four age-specific groups of children. (A) Age 3; (B) Age 4 younger; (C) Age 4 older; and (D) Age 5
For the younger four-year-old (Figure 2B and 3B) and five-year old (Figure 2D and 3D) children, the combinations of sensitivity and specificity yielded by each possible failure criterion were similar for the two tests and the curves are very similar to one another. For the older four-year-old children (Figure 2C and 3C), the Lea Symbols test either had slightly higher sensitivity and/or slightly higher specificity for each possible failure criterion than the HOTV test so that the ROC curve for the Lea Symbols test is slightly above the curve for the HOTV test.
DISCUSSION
The Lea Symbols and HOTV optotypes each have characteristics that might make them more or less effective for children of different ages. The Lea Symbols optotypes are symmetrical, closed symbols with size determined by using an “equal blur-out” criterion.6 Comparison in adults between acuities measured with the Bailey-Lovie Chart and the Lea Symbols14 indicates that Lea Symbols result in measured acuities better by an average of one logMAR line than those measured with the Bailey-Lovie Chart. Although the acuity difference between the two tests was reported to become larger as the level of acuity decreased,14 similar measurements of differences between the two eyes, which is critical to the assessment of amblyopia, were reported for the Lea Symbols and Bailey-Lovie Chart. A recent comparison of Lea Symbols acuity and acuity measured with the Early Treatment Diabetic Retinopathy Study (ETDRS) charts in three- to seven-year-old children showed Lea Symbols acuity values that were, on average, one-half line better than ETDRS acuity values.15 Within the limited range of acuity values obtained in this study (20/100 or better), there was no relation between acuity score and the difference between Lea Symbols and ETDRS values obtained.
The HOTV test is constructed of letter optotypes that, like the Lea Symbols, demonstrate left-right symmetry. This letter set was originally developed by Sheridan16 for use with preschool children. H, O, and V are Sloan letters and are judged equivalent in difficulty to each other and to the Landolt ring.8 The letter size is determined by the overall angular subtense and the angular subtense of the letter detail.8 Therefore, for a given visual acuity designation, the Lea Symbols and HOTV optotypes are not the same physical size, as shown in Figure 1.
Children in the youngest group (mean age 45.3 months, range 41 to 47.9 months) found VA testing with the Lea Symbols easier than the HOTV test, whether or not they had a targeted vision condition. As shown in the ROC curve for three-year-olds in Figure 2A and 3A, the HOTV test yielded higher sensitivity and lower specificity than Lea Symbols for each acuity line tested. Furthermore, comparison of the performance on the two tests at the specificity level closest to 90% for each test for three-year-olds required that the failure criterion be adjusted to be one line smaller for the Lea Symbols than for the HOTV test. The Lea Symbols, however, did not perform statistically significantly better than the HOTV test for detecting one or more VIP Study targeted conditions or Group 1 conditions. Of the 215 three-year-olds screened and examined in the VIP Study, 59 children were found to have ≥1 VIP Study targeted condition, and 23 children had Group 1 conditions; therefore, we had limited statistical power to detect a statistically significant difference in sensitivity. As indicated above, the three-year-old children in this study had a mean age of three years nine months. It would be valuable and interesting to know the sensitivity and specificity results for younger three-year-olds.
For the other age groups, the ROC curves are quite similar for the two tests, and the failure criterion yielding closest to 0.90 specificity is the same acuity line for both VA tests. Inspection of the ROC curves illustrates that the sensitivity of either VA test for any age group may be increased by changing the failure criterion to a finer acuity level, resulting in the detection of more of the children with targeted condition(s). As illustrated in the ROC curves in Figure 2A-D and 3A-D, changing the failure criterion to increase sensitivity also has the effect of lowering the specificity level for the screening, which allows more children without a targeted condition to fail the screening and be referred for a full examination, thus increasing the number of over-referrals. For example, in the three-year-old age group, if the 10/20 line is used as the failure criterion for the HOTV test, test sensitivity will be over 80% for any VIP Study targeted condition; but specificity will fall to approximately 60%, meaning that 40% of children without a targeted condition will be referred for an eye examination. Policy makers, in consultation with experts in the field using available data and considering the manpower/resources available, must make decisions that determine which combination of over-referrals and missed cases is acceptable for a particular screening.
A variety of factors may contribute to the observed ROC curves for visual acuity screening. (1) Visual acuity is a cognitively demanding task for preschoolers. Allowing the child to respond by matching rather than naming helps make the task easier, but it remains a difficult task for some children in this age group. (2) Although testing at 3 m (rather than the 6 m adult test distance) and pretesting at 1 m were performed to help overcome environmental distractions, it is difficult for the screener to maintain the child’s attention on the task in a screening environment offering considerable distractions. (3) The VIP Study screening was administered once and not repeated, so any child not feeling well at the time of testing might have failed the screening for reasons unrelated to vision. (4) Not all targeted vision conditions listed in Table 1 would be expected to cause a child to fail a vision screening based on the results of a test of visual acuity. Children who have amblyopia with mildly decreased visual acuity may pass the cut-off vision screening acuity level. Similarly, children with moderate hyperopia or intermittent strabismus might also pass the screening cut-off acuity line.
Although procedural differences exist between the studies, these findings support those of Kvarnstrom and Jakobsson who reported that Lea Symbols and the HOTV test were equivalent when used for vision screening testing in three-and-four-year-old Swedish children seen at the child health care centers for routine care.17
The central question addressed is whether vision screening of three- and four-year-old children is more effective with the youngest children in this age range if Lea Symbols rather than the HOTV letters are used as the screening optotypes. For the youngest children, it was necessary to make the Lea Symbols pass/fail criterion one line smaller than the HOTV test pass/fail criterion in order to compare the tests at 90% specificity. For the older age groups, the pass/fail criterion line closest to 90% specificity was the same for both screening tests. When the cutoff was appropriately adjusted for the three-year-olds, there was no statistically significant difference in any of the four age groups in the effectiveness of the two optotypes in identifying children in need of being referred for further care. Further research is needed on a younger group of three-year-olds to determine whether the differences found in this study become significant in young three-year-olds.
ACKNOWLEDGMENTS
Funded by the institution of each VIP Study Group Executive Committee member and by grants from the National Eye Institute, National Institutes of Health, Department of Health and Human Services: EY12644 (PS); EY12545 (EC); EY12550 (LC); EY12534 (BM); EY12647 (DOB); EY12648 (PS, MTK); and EY12547 (MM). GSY received support from R21EY018908. Further support was provided by an unrestricted gift to the University of Pennsylvania from Research to Prevent Blindness and a gift from the Paul and Evanina Bell Mackall Foundation Trust to MM; and the Morris Funds at the Ohio State University College of Optometry to PS (525044).
Appendix A. Lea Symbols optotype sizes used in the VIP Study
The average size of the Lea Symbols was 1.32 times larger than Sloan letters or 6.6 minutes of arc instead of 5 minutes of arc at the designated test distance. Individually the symbols were: house 1.35; apple 1.31; circle 1.42; and square 1.20 times larger than Sloan letters. The width and height of the house optotype was used as the master symbol to determine the thickness of the stroke width for all symbols and also to determine the distance from the inside of the crowding rectangle to the symbols.
The stroke width for all symbols was 13.9% of the overall size of the house optotype. If a house was 100 mm high or wide, the stroke width was 13.9 mm. The other three symbols for that same acuity level, regardless of their size, also had the same 13.9 mm stroke width. The space between the symbols was the average of the four symbols. This comes out to be 97.8 % of the house. This spacing was recommended by Dr. Merton Flom (pers. comm. Ed Kopidlansky, Precision Vision, LaSalle, IL.). The lines forming the crowding rectangle were the same thickness as the stroke width of the symbols for that acuity level. The distance from the inside of the crowding rectangle to the symbols was 50% of the width of the house on that same acuity level regardless of which symbols were on the ends of the line. The inside height of the rectangle was always constant relative to the size of the symbols because it was based on the house at that acuity level. The inside width of the rectangle could vary depending on which symbol was repeated to make up the five-symbol line.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Hartmann EE, Dobson V, Hainline L, Marsh-Tootle W, Quinn GE, Ruttum MS, Schmidt PP, Simons K. Preschool vision screening: summary of a Task Force report. Behalf of the Maternal and Child Health Bureau and the National Eye Institute Task Force on Vision Screening in the Preschool Child. Pediatrics. 2000;106:1105–16. doi: 10.1542/peds.106.5.1105. [DOI] [PubMed] [Google Scholar]
- 2.Hered RW, Murphy S, Clancy M. Comparison of the HOTV and Lea Symbols charts for preschool vision screening. J Ophthalmic Nurs Technol. 1997;16:68–73. [PubMed] [Google Scholar]
- 3.Schmidt P, Maguire M, Dobson V, Quinn G, Ciner E, Cyert L, Kulp MT, Moore B, Orel-Bixler D, Redford M, Ying GS, the Vision in Preschoolers Study Group Comparison of preschool vision screening tests as administered by licensed eye care professionals in the Vision In Preschoolers Study. Ophthalmology. 2004;111:637–50. doi: 10.1016/j.ophtha.2004.01.022. [DOI] [PubMed] [Google Scholar]
- 4.The Vision in Preschoolers Study Group Preschool visual acuity screening with HOTV and Lea symbols: testability and between-test agreement. Optom Vis Sci. 2004;81:678–83. doi: 10.1097/01.opx.0000144746.80718.67. [DOI] [PubMed] [Google Scholar]
- 5.The Vision in Preschoolers (VIP) Study Group Development and implementation of a preschool vision screening program in a mobile setting. NHSA Dialog. 2005;8:16–24. [Google Scholar]
- 6.Hyvärinen L, Näsänen R, Laurinen P. New visual acuity test for pre-school children. Acta Ophthalmol (Copenh) 1980;58:507–11. doi: 10.1111/j.1755-3768.1980.tb08291.x. [DOI] [PubMed] [Google Scholar]
- 7.Moore B, Weissberg E, Mayer DL. Testability of the Massachusetts Visual Acuity test, a screening version of the LEA visual acuity test. Optom Vis Sci. 1997;74(Suppl.):174. [Google Scholar]
- 8.Committee on Vision Recommended stardard procedures for the clinical measurement and specification of visual acuity. Report of working group 39. Committee on vision. Assembly of Behavioral and Social Sciences, National Research Council, National Academy of Sciences, Washington, D.C. Adv Ophthalmol. 1980;41:103–48. [PubMed] [Google Scholar]
- 9.Ferris FLr, Kassoff A, Bresnick GH, Bailey I. New visual acuity charts for clinical research. Am J Ophthalmol. 1982;94:91–6. [PubMed] [Google Scholar]
- 10.Maguire MG, the Vision In Preschoolers (VIP) Study Group Children unable to perform screening tests in vision in preschoolers study: proportion with ocular conditions and impact on measures of test accuracy. Invest Ophthalmol Vis Sci. 2007;48:83–7. doi: 10.1167/iovs.06-0384. [DOI] [PubMed] [Google Scholar]
- 11.Holmes JM, Beck RW, Repka MX, Leske DA, Kraker RT, Blair RC, Moke PS, Birch EE, Saunders RA, Hertle RW, Quinn GE, Simons KA, Miller JM. The amblyopia treatment study visual acuity testing protocol. Arch Ophthalmol. 2001;119:1345–53. doi: 10.1001/archopht.119.9.1345. [DOI] [PubMed] [Google Scholar]
- 12.Moke PS, Turpin AH, Beck RW, Holmes JM, Repka MX, Birch EE, Hertle RW, Kraker RT, Miller JM, Johnson CA. Computerized method of visual acuity testing: adaptation of the amblyopia treatment study visual acuity testing protocol. Am J Ophthalmol. 2001;132:903–9. doi: 10.1016/s0002-9394(01)01256-9. [DOI] [PubMed] [Google Scholar]
- 13.Kulp MT, Dobson V, Peskin E, Quinn G, Schmidt P, the Vision in Preschoolers (VIP) Study Group The electronic visual acuity tester: testability in preschool children. Optom Vis Sci. 2004;81:238–44. doi: 10.1097/00006324-200404000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Dobson V, Maguire M, Orel-Bixler D, Quinn G, Ying GS, the Vision in Preschoolers (VIP) Study Group Visual acuity results in school-aged children and adults: Lea Symbols chart versus Bailey-Lovie chart. Optom Vis Sci. 2003;80:650–4. doi: 10.1097/00006324-200309000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Dobson V, Clifford-Donaldson CE, Miller JM, Garvey KA, Harvey EM. A comparison of Lea Symbol vs ETDRS letter distance visual acuity in a population of young children with a high prevalence of astigmatism. J AAPOS. 2009;13:253–7. doi: 10.1016/j.jaapos.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sheridan MD. Vision screening of very young or handicapped children. BMJ. 1960;2:453–6. doi: 10.1136/bmj.2.5196.453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kvarnström G, Jakobsson P. Is vision screening in 3-year-old children feasible? Comparison between the Lea Symbol chart and the HVOT (LM) chart. Acta Ophthalmol Scand. 2005;83:76–80. doi: 10.1111/j.1600-0420.2005.00367.x. [DOI] [PubMed] [Google Scholar]