Abstract
Many Korean American persons have hypertension, but competing life priorities often prevent them from attending health‐promotion educational activities. Using principles of community‐based participatory research, the authors conducted a prospective clinical trial to determine the effectiveness of a mailed vs an in‐class culturally tailored education intervention. A total of 380 hypertensive Korean American persons from the Baltimore/Washington area were assigned to a more intense in‐class education group or a less intensive mail education group. Evaluation of postintervention blood pressure (BP) outcomes revealed that significant reductions in systolic BP (13.3 mm Hg and 16.1 mm Hg, respectively) and diastolic BP (9.5 mm Hg and 10.9 mm Hg) and increases in BP control rates (42.3% and 54.3%) were achieved in both groups. No significant differences in BP outcomes between groups, however, were found. In conclusion, education by mail was an effective strategy for improving BP control and may be a viable approach for other immigrant groups if the education materials address their cultural needs.
Managing chronic illnesses such as high blood pressure (BP) is a difficult task for many Americans, 1 , 2 but it is even more challenging for new immigrants. Korean Americans, one of the most rapidly growing ethnic minority populations in the United States, have a high prevalence of high BP and its complications. 3 Studies of BP in immigrant populations indicate that, in general, the prevalence of high BP increases when a group of immigrants migrates to a more developed country 4 because the stress related to acculturation and changes in diet and lifestyle may adversely affect BP levels. 5 , 6 , 7 , 8
Previous reports have indicated that despite the high prevalence of high BP among Korean American persons, individual, cultural, and systemic barriers stand in the way of adequate BP control in this population. 9 , 10 Korean American persons experience not only uncontrolled high BP and its complications but also social isolation and a loss of self‐confidence. 11 To address this health issue in Korean Americans, a community‐based and culturally tailored behavioral intervention program, the Self‐Help Intervention Program for High Blood Pressure Care (SHIP‐HBP), has been constructed and is currently being implemented. The SHIP‐HBP includes a comprehensive intervention trial that combines psychobehavioral education with self‐monitoring of BP and bilingual nurse telephone counseling. Our primary goal in designing this program was to adapt and translate evidence‐based treatment guidelines and behavioral recommendations 12 into more culturally relevant education materials for first‐generation Korean American persons who still subscribe to a traditional Korean culture. An equally important goal was to find the most effective and feasible mode of care delivery for this target population. The focus of this paper is on the differential effects of 2 different modes of health education delivery of the first component of this comprehensive intervention program, psychobehavioral education, on BP and psychosocial outcomes in a hard‐to‐reach middle‐aged population of Korean Americans. The relevance of this approach to other ethnic groups should be evaluated.
While varying degrees of efficacy have been reported for structured educational interventions, 13 , 14 , 15 , 16 the harsh reality is that competing life priorities and limited resources often prevent first‐generation immigrants from attending health‐promotion classes, such as BP management classes. For example, for many middle‐aged Korean American persons, time constraints are one of the critical barriers to seeking medical help or health education programs. 17 In light of our understanding of these contextual factors and in an attempt to find the most useful ways to deliver an effective education program, we tested the effectiveness of a culturally tailored psychobehavioral education intervention, comparing 2 delivery modes: in‐class instruction and a self‐paced mail intervention.
CONCEPTUAL AND OPERATIONAL FRAMEWORK UNDERLYING THE INTERVENTION
The Learned Resourcefulness Model, 18 , 19 , 20 , 21 in conjunction with a community‐based participatory research (CBPR) framework, 22 , 23 , 24 , 25 guided the planning, implementation, and evaluation of this translational study. This model incorporates critical constructs from adult learning, social support, and behavior modification theories. 26 , 27 , 28 It describes how self‐help and quality of life can be affected by chronic illness, and it recognizes individual factors and demands that affect self‐care behaviors (eg, education, income, immigration status, employment status, living arrangements, and daily needs). Its theoretic premise is that if coping skills are maintained or increased through learning a self‐help response to adversity, the skills subsequently provide a stronger base for dealing with adverse situations, such as managing chronic illness. 29 , 30
We also employed CBPR as the operational framework of this research. In particular, following participatory action research principles, 23 , 30 we solicited active community involvement in all processes that shaped the development of our research and intervention strategies, as well as in the implementation and evaluation. We have successfully used CBPR methodologies in our previous research projects involving the Korean American community, including health needs assessment, 9 , 10 , 31 , 32 , 33 intervention development, and health service planning and development. 34 , 35 , 36
METHODS
Design and Sample
The SHIP‐HBP study is a community‐based, prospective trial involving middle‐aged Korean American persons in the Baltimore‐Washington metropolitan area. The trial's primary objective is to determine whether the SHIP‐HBP is effective in controlling high BP at 3, 9, and 15 months from the start of the intervention. This multifaceted intervention has 3 main components: (1) a structured psychobehavioral education that focuses on fostering self‐help skills in controlling high BP, (2) home BP monitoring with a telephone transmission system, and (3) telephone counseling by a bilingual nurse who facilitates problem solving in managing BP. The education component was offered for 6 weeks, followed by a 6‐week test period for home BP monitoring. Home monitoring of BP and telephone counseling began 3 months after the start of the education intervention and lasted for 12 months. For the purposes of this paper, we used outcomes collected at 3 months, including behavioral indicators and BP outcomes measured before we started telephone counseling.
We used a stratified sampling scheme based on the participant's age and sex to create comparable groups of middle‐aged Korean American persons with high BP who were representative of Korean American persons who reside in the Baltimore‐Washington metropolitan area. Approximately 100,000 Korean American persons live in this region, 37 of whom 23,000 are estimated to be in the target age group (40–65 years), and 41.7% are assumed to have high BP. 38 , 39 The eligibility criteria were (1) self‐identified as a first‐generation Korean American, (2) 40 to 64 years of age, and (3) systolic BP (SBP) ≥140 and/or diastolic BP (DBP) ≥90 mm Hg or taking BP medication. At baseline, 445 Korean American persons were recruited primarily from ethnic Korean churches, grocery stores, and ethnic newspaper advertisements. 37 Of those completing the baseline assessment, 65 dropped out either before the education sessions ended or before completing follow‐up data collection at 3 months or did not measure and transmit their BP at home. The reasons for dropping out included lost contact, travel, moving, schedule conflict, personal problem, physical condition, normal BP, belief that their BP was not high enough to require rigorous management, and overwhelmed with assigned BP measurement. There were no significant differences in sociodemographic characteristics between patients who remained in the study and those who dropped out.
Procedure
On institutional review board approval, eligible Korean Americans with high BP who agreed to participate in this study were assessed for baseline characteristics. Trained research staff measured BP, body weight, and height, and questionnaires were completed by self‐report. Participants needed 20 to 40 minutes to complete the baseline questionnaire. They were then assigned to either the in‐class education group (n=184) or the mail education group (n=261), considering such factors as place of residence (ie, proximity to our in‐class locations), schedule compatibility (with our 21 classes in several locations at different times), and participant preference. We were particularly careful to monitor the assignment to obtain compatible groups as well as to minimize potential crossover effect within a relatively small social network (eg, attending the same church) between intervention groups. For example, when a group of participants were identified at a church, one mode of education was offered to the church members. At baseline, the in‐class intervention and mail intervention groups did not significantly differ in terms of sociodemographic or medical characteristics. Altogether, 380 participants (in‐class group, 168; mailing group, 212) completed the 3‐month follow‐up assessments and BP measurements, and they were included in the analysis.
The mailing intervention group received weekly 2‐hour in‐class education sessions over 6 weeks. The group intervention classes were held in a community center located in Korean American‐populated neighborhoods. The self‐paced mailing intervention group received the same educational materials each week for 6 weeks via regular mail. Of those in the in‐class intervention group (n=168), 86 (51.2%) attended all 6 class sessions, while the remainder attended 1 to 5 sessions (mean number of sessions attended, 5.08±1.25). During the 6‐week education for the in‐class intervention group and on completion of the 6‐week education for the mailing intervention group, study participants were given a home‐based BP measurement device (A&D UA‐767; A&D Company, Ltd, Tokyo, Japan) equipped with a telephone transmission system (HBPMT) and instructions. During the following 6‐week testing period, participants were instructed to measure their BP at home using the device and start transmitting BP data once a week via their home telephone; this process generally took <2 minutes per transmission. The purpose of this test period was to increase the participants' level of confidence in measuring their BP and transmitting the data and to prepare them for the next 12‐month telephone counseling phase, which would build on the patient's progress in BP control through tailored messages from a bilingual registered nurse.
Psychobehavioral Education Intervention
Our psychobehavioral education intervention in this ongoing study has 2 main components: the first, an educational and behavioral intervention, is aimed at enhancing clients' knowledge of high BP and its treatment, reducing risk factors, and providing resources to Korean American persons; it also focuses on improving Korean Americans' coping/enabling skills in problem solving, cognitive reframing, and belief in self. The second component, the psychological intervention, is aimed at assisting them in reframing life adversity in a different and positive perspective. The activities of the psychosocial intervention are centered around (1) introducing and enhancing strategies for managing life adversities that are inherent in the experience of having high BP and being a middle‐aged immigrant, (2) providing necessary knowledge or/and information, and (3) promoting self‐care behaviors related to high BP control.
Measurements
All study variables were measured twice (at baseline and 3 months), except for the ongoing monitoring of BP. Research questionnaires used in this study were developed in English and translated into Korean, then back‐translated into English. In this study, participants exclusively used the Korean version because they were all born in Korea and preferred using their mother tongue.
Baseline BP was measured by averaging the second and third BP readings, recorded in mm Hg. Measurements of DBP and SBP were obtained by trained research assistants using the A&D UA‐767, a fully automatic device based on the oscillometric method. We chose not to use mercury sphygmomanometers because of the major measurement issue of interobserver and intraobserver variability, as highlighted in 2 recently published articles. 40 , 41 Instead, we chose the A&D UA‐767 device, which had been previously validated against a mercury sphygmomanometer. 42 The same device, with an additional t n function, was used for HBPMT.
Follow‐up BP measurements were collected by HBPMT, measured at home with the same A&D UA device. During this intervention trial, participants were asked to measure their BP at least 3 times in the morning and 3 times in the evening each week. For the HBPMT test period (6 weeks following the 6‐week education intervention), self‐monitoring of BP was validated by automated BP reports from HBPMT, which showed the time and frequency of BP measurements and BP readings. We used the weekly average of those transmitted data as postintervention data.
High BP belief was measured by the high BP belief scale. 43 High BP beliefs were assessed by a 12‐item questionnaire, which asked participants to indicate whether they believed certain behavioral factors could help lower BP and to select the most important factor to control BP. Higher scores represent higher levels of high BP belief. This scale has been translated into Korean and was used in our previous study of Korean American persons with high BP, 37 with an α coefficient of .897 in the present study.
Self‐efficacy for high BP control was measured by a high BP management self‐efficacy scale, adapted from the high BP belief scale. 43 The modified scale consists of 4‐point Likert‐type items asking how confident the individual is in managing high BP in 11 areas, including reducing salt intake, taking prescribed BP medicines, and eating fewer fatty foods. Higher scores represent higher levels of self‐efficacy in managing high BP. The Korean version yielded an a coefficient of .93 for the present sample.
High BP knowledge was evaluated using 12 items developed by the National High Blood Pressure Education Program of the National Heart, Lung, and Blood Institute (1994), with the addition of 18 items generated by the current investigative team on the basis of a literature review. This modified instrument has been used in our work with Korean American persons. 9 High BP knowledge scores were calculated by counting the number of items with correct responses to statements such as “Young adults don't get high BP” and “High BP is life‐threatening.” Scores ranged from 0 to 30.
Medication adherence was measured by the medication subscale from the Hill‐Bone Compliance Scale. 44 The scale consists of nine 4‐point Likert‐type items (1 = none of the time, 2 = some of the time, 3 = most of the time, 4 = all the time) that measure the reported degree of adherence to medication. Higher scores indicate lower adherence. This scale has demonstrated adequate reliability (α = .74–.84), construct validity, and predictive validity in African American and non‐Hispanic white patients. 44 Cronbach α was .74 for the medication subscale in this sample.
Statistical Analysis
Analysis was performed on 380 Korean American persons who completed both the baseline and 3‐month follow‐up assessments (Figure). The primary outcomes of this study were changes in SBP and DBP from baseline to 3‐month follow‐up. The change in the number of participants in whom control of BP was achieved in each group (BP <140/90 mm Hg) was also assessed. Multiple data points derived from home BP monitoring were averaged at 3 months as 3‐month follow‐up data. Secondary outcomes included the level of high BP knowledge, high BP belief, self‐efficacy, and the level of adherence to medication regimens. We used paired t tests to assess the differences in the proposed outcome variables between the in‐class intervention and mailing intervention groups. Statistical significance was determined at α=.05.
Figure.
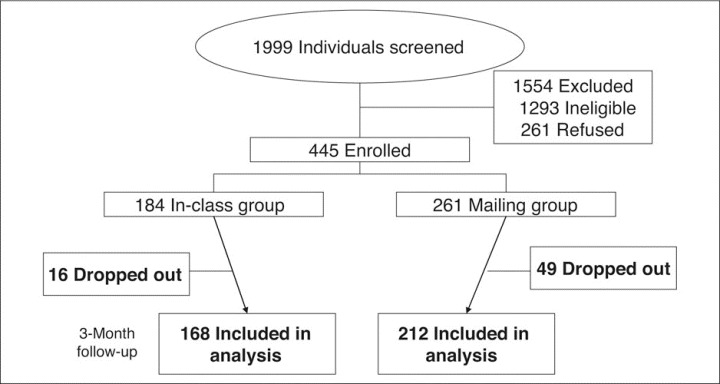
Participant tracking.
RESULTS
Sample Characteristics
Baseline characteristics were similar for the 380 participants, and no statistically significant difference was observed in any of the main variables between the in‐class and mail education groups (Table I). The mean age of the group was 52.0 years (range, 40–64 years), and close‐to‐equal representation of sex was attained (48.9% men, 51.1% women). Most participants were married (94.0%) and had more than a high school education (88.4%); on average, they had resided in the United States for 16.2 years (Table I).
Table I.
Demographics of Enrolled Participants at Baseline
| Variables | In‐Class (n=168) | Mailing (n=212) | Total (N=380) | χ2/t (P Value) |
|---|---|---|---|---|
| Age, y | ||||
| 40–49 | 59 (35.1) | 78 (36.8) | 137 (36.1) | 5.250 (.073) |
| 50–59 | 93 (55.4) | 126 (59.4) | 219 (57.6) | |
| 60–64 | 16 (9.5) | 8 (3.8) | 24 (6.3) | |
| Mean (SD) | 52.3 (5.8) | 51.7 (5.6) | 52.0 (5.7) | 1.027 (.311) |
| Sex | ||||
| Male | 86 (51.2) | 100 (47.2) | 186 (48.9) | 0.606 (.436) |
| Female | 82 (48.8) | 112 (52.8) | 194 (51.1) | |
| Marital status | ||||
| Married | 155 (92.3) | 202 (95.3) | 357 (94.0) | 1.504 (.220) |
| Other | 13 (7.7) | 10 (4.7) | 23 (6.1) | |
| Education | ||||
| Less than high school | 20 (11.9) | 24 (11.3) | 44 (11.6) | 0.077 (.962) |
| High school graduate | 56 (33.3) | 69 (32.6) | 125 (32.9) | |
| ≥Some college | 92 (54.8) | 119 (56.1) | 211 (55.5) | |
| Work status | ||||
| Full‐time | 116 (69.1) | 153 (72.5) | 270 (71.1) | 2.810 (.422) |
| Part‐time | 24 (14.3) | 19 (9.0) | 43 (11.4) | |
| No job | 18 (10.7) | 27 (12.8) | 45 (11.9) | |
| Other | 10 (5.9) | 12 (5.7) | 22 (5.8) | |
| Income level | ||||
| Very comfortable/comfortable | 56 (33.5) | 74 (35.4) | 130 (34.6) | 1.171 (.557) |
| “Okay” | 62 (37.1) | 84 (40.2) | 146 (38.8) | |
| Difficult/very difficult to manage | 49 (29.3) | 51 (24.4) | 100 (26.6) | |
| Years of residence in the United States, mean (SD) | 17.2 (8.9) | 15.3 (9.0) | 16.2 (9.0) | 1.911 (.057) |
| Body mass index, kg/m2 | ||||
| <25 (normal) | 78 (46.4) | 115 (54.3) | 194 (50.8) | 2.330 (.312) |
| 25–30 (overweight) | 78 (46.4) | 85 (40.1) | 163 (42.9) | |
| ≥30 (obese) | 12 (7.1) | 12 (5.7) | 24 (6.3) | |
| Taking BP medication | ||||
| Yes | 97 (58.3) | 117 (55.2) | 215 (56.6) | 0.377 (.539) |
| No | 70 (41.7) | 95 (44.8) | 165 (43.4) | |
| Relevant disease | ||||
| Heart failure | 5 (3.0) | 2 (0.9) | 7 (1.8) | 2.142 (.143) |
| Myocardial infarction | 5 (3.0) | 3 (1.4) | 8 (2.1) | 1.127 (.288) |
| Stroke | 11 (6.6) | 5 (2.4) | 16 (4.2) | 5.264 (.072) |
| Kidney disease | 19 (11.4) | 31 (14.5) | 50 (13.1) | 4.796 (.091) |
| Diabetes | 24 (14.4) | 19 (9.0) | 43 (11.4) | 3.532 (.171) |
| Family history of high BP | ||||
| Yes | 122 (72.6) | 156 (73.9) | 278 (73.5) | 1.554 (.460) |
| Years of high BP, mean (SD) | 4.1 (5.8) | 4.4 (6.5) | 4.3 (6.2) | −0.585 (.559) |
| Values are expressed as No. (%) unless otherwise indicated. Abbreviation: BP, blood pressure. | ||||
The mean duration of high BP was 4.3 years, and 73.5% of the participants reported a family history of high BP. At the time of enrollment, only 56.6% were taking BP medication. One noteworthy characteristic of this sample was the relatively high proportion of Korean American persons who had comorbidities such as kidney disease (13.1%), diabetes (11.4%), stroke (4.2%), and heart failure (1.8%). The baseline mean (SD) SBP and DBP values for the in‐class education group were 141.5 (17.7) and 90.0 (11.1) mm Hg; those for the mail education group were 143.9 (17.0) and 91.8 (10.8) mm Hg.
BP Outcomes
Participants transmitted an average of 35.3 (17.3) BP readings (range, 1–93 readings) during the HBPMT test period (6 weeks following the 6‐week education intervention). Multiple data points derived from HBPMT were averaged as 3‐month outcome data. Three months after the beginning of the intervention, the average BP measurements for both groups showed dramatic improvement (Table II). From baseline to 3 months, the mean (SD) reductions in SBP were 13.3 (16.5) mm Hg in the in‐class group and 16.1 (16.0) mm Hg for the mailing intervention group. The corresponding DBP reductions were 9.5 (10.2) mm Hg and 10.9 (10.0)mm Hg for the in‐class intervention and mailing intervention groups, respectively. During this period, the fraction of the total participants who had controlled BP (<140/90 mm Hg) more than doubled in both groups (Table III). At baseline, only 35.7% of the in‐class education group and 25.9% of the mail education group had controlled BP. At 3 months of follow‐up, the control rate was 78.0% for the in‐class education group and 80.2%for the mailing group (Table III).
Table II.
Blood Pressure Before and After Education Intervention
| Baseline | Postintervention | Change | T Value | P Value | |
|---|---|---|---|---|---|
| Systolic blood pressure, mm Hg | |||||
| In‐class (n=168) | 141.5 (17.7) | 128.2 (12.9) | −13.3 (16.5) | −10.49 | .000 |
| Mailing (n=212) | 143.9 (17.0) | 127.8 (12.8) | −16.1 (16.0) | −14.64 | .000 |
| Total (N=380) | 142.9 (17.3) | 128.0 (12.8) | −14.9 (16.2) | −17.84 | .000 |
| Diastolic blood pressure, mm Hg | |||||
| In‐class (n=168) | 90.0 (11.1) | 81.4 (8.5) | −9.5 (10.2) | −12.07 | .000 |
| Mailing (n=212) | 91.8 (10.8) | 80.9 (9.0) | −10.9 (10.0) | −16.03 | .000 |
| Total (N=380) | 91.4 (11.0) | 81.1 (8.8) | −10.3 (10.1) | −19.95 | .000 |
| Values are mean (SD). | |||||
Table III.
Blood Pressure Control Rates Before and After Educational Intervention
| Baseline | Postintervention | χ2 (P Value) | |
|---|---|---|---|
| Class (n=168) | 60 (35.7) | 131 (78.0) | 7.857 (.005) |
| Mailing (n=212) | 55 (25.9) | 170 (80.2) | |
| Total (N=380) | 115 (30.3) | 301 (79.2) | |
| Blood pressure control defined as <140/90 mm Hg. Values are expressed as No. (%). | |||
Behavioral Outcomes
In general, the psychological and behavioral outcomes improved to a similar degree in the two groups. Data at 3‐month follow‐up, including those regarding feelings of self‐efficacy and high BP knowledge, health belief, and medication adherence were significantly improved when compared with baseline measurements for both groups (Table IV).
Table IV.
Psychosocial Correlates of Blood Pressure Control at Baseline and After Educational Intervention (N=380)
| Baseline | Postintervention | Change | T Value | P Value | |
|---|---|---|---|---|---|
| Self‐efficacy (1.0 to ≈4.0), mean (SD) | |||||
| In‐class (n=168) | 3.07 (0.43) | 3.24 (0.36) | 0.17 (0.38) | 5.58 | .000 |
| Mailing (n=210) | 3.05 (0.38) | 3.20 (0.37) | 0.15 (0.34) | 6.50 | .000 |
| Knowledge of high blood pressure (0.0 to ≈26.0), mean (SD) | |||||
| In‐class (n=168) | 18.80 (3.85) | 22.91 (2.48) | 4.11 (4.01) | 13.26 | .000 |
| Mailing (n=212) | 18.93 (4.30) | 21.58 (3.28) | 2.64 (3.71) | 10.36 | .000 |
| Health beliefs (1.0 to ≈5.0), mean (SD) | |||||
| In‐class (n=165) | 4.72 (0.41) | 4.83 (0.29) | 0.11 (0.38) | 3.83 | .000 |
| Mailing (n=212) | 4.67 (0.46) | 4.75 (0.29) | 0.09 (0.42) | 3.11 | .002 |
| Medication adherence (1.0 to ≈4.0), mean (SD)a | |||||
| In‐class (n=98) | 3.41 (0.33) | 3.49 (0.28) | 0.08 (0.27) | 2.76 | .007 |
| Mailing (n=117) | 3.37 (0.37) | 3.46 (0.28) | 0.09 (0.35) | 2.91 | .004 |
| aAnalyzed for 215 participants who were taking antihypertensive medication. | |||||
DISCUSSION
The results from the 3‐month assessment in this ongoing study have indicated that culturally tailored interventions can greatly improve BP control in middle‐aged Korean American persons. In particular, our findings suggest that applying a community‐partnered approach to developing culturally sensitive intervention materials and executing the trial in a traditionally understudied minority community may be an important and effective operational strategy for complex behavioral intervention involving immigrants with high BP.
In particular, the CBPR approach was useful in crafting intervention messages that directly address beliefs, attitudes, and knowledge that are closely embedded in Korean American persons' cultural upbringing. For example, through our formative intervention phase, our community‐partnered intervention team found that one of the major barriers to taking high BP medication among Korean Americans with high BP was the myth that BP medication can be toxic or even addictive. Many expressed concerns such as “I heard that once you got on medication, you have to be on it for the rest of your life,” or “One needs to postpone taking medication as long as one can in order to prevent organ damage.” To address these prevalent myths, the education materials focused on the fact that the harmful effects on target organs of delaying BP treatment far outweigh any possible adverse effects of high BP medication. In addition, our team chose several intervention messages that addressed myths rooted in cultural beliefs and repeatedly incorporated these messages into written education materials as well as the telephone counseling protocol. Throughout the process, cultural knowledge of and insights into the target ethnic community that were provided by the community members of our research team were essential in crafting and delivering culturally and contextually relevant intervention materials. Such a CBPR approach has been adopted by increasing numbers of researchers in designing effective interventions aimed at complex behavioral changes, such as managing chronic illness. 45 , 46
Our results also suggest that for the delivery of an initial education intervention, a self‐pacing mail intervention was as effective as in‐class education in terms of achieving an optimal BP level. The changes in secondary outcomes in the mail intervention group, however, such as the level of high BP knowledge and adherence to BP medication, were not as great as those in the in‐class education group. It is not yet certain whether the revealed group difference is a clinically meaningful one. While these differences do not suggest that there are significant barriers to achieving and maintaining optimal BP after in‐class or in‐mail education, the long‐term maintenance of the obtained intervention effects will be evaluated as this study progresses.
Several potential limitations should be borne in mind when interpreting our findings. First, our study is not designed to distinguish the precise intervention effects of each component (ie, education, monitoring). While both groups received the same amount of education and were advised to self‐monitor their BP, it is possible that the differential effect of the intervention delivery methods (mail vs in‐class education) might be replicable only with implementation of other intervention components. Second, we were unable to use traditional random sampling because of the potential crossover effect that can occur in a close‐knit ethnic community. Although there were no significant differences in the major characteristics of each group that would be expected to prevent us from successfully creating comparable conditions in the group assignments, it is possible that some as yet unidentified influence could have affected the study outcome. Third, our study may suffer from some of the inherent validity limitations associated with the main data gathering method, self‐report, or some key demographic variable such as income level. The method of a self‐report was chosen to accommodate the need for confidentiality among the Korean American persons who were not exposed to many research projects. Finally, we did not have specific medication data at 3 months; it is possible that some patients had medication changes during this time period that might have changed the results.
In addition, it is difficult to compare findings regarding the effects of the mail intervention in the present study with those in the existing literature because of a lack of published reports regarding the use of self‐pacing mail interventions in chronic illness management in a community setting. Mail intervention has predominantly been used either to deliver a simple health message, such as how to detect the signs of heart attack or stroke, 47 , 48 or to urge people to act, such as to making an appointment or to remembering to get a follow‐up checkup. 49 , 50 The present study is the first structured trial to evaluate the effectiveness and practical utility of a self‐paced mail education intervention related to the rather complex subject of managing high BP. If these findings can be replicated in other studies, they may have significant clinical implications. A lack of time is one of the most critical barriers for implementing intense educational interventions in middle‐aged patients, regardless of ethnic background, and a self‐paced mail education intervention offers an alternative strategy that can reach many patients who are in need of proper education in managing their chronic illness.
CONCLUSIONS
We have shown that a community‐based intervention, culturally tailored to address the cultural upbringing and contextual factors in the lifestyle of the target population, can have a positive impact on improving the health and quality of life of many individuals. As the findings of a recent national hypertension management survey highlighted, misconceptions about the nature and management of hypertension persist in all levels of society, including ethnic minority populations. 51 The method used in this study may potentially be translatable and usable by clinicians and researchers who are working to improve the health and quality of life of underserved and vulnerable populations.
Disclosure:
This research is supported by the Agency for Health Care Research and Quality (HS013160) and in part by the Center for Collaborative Intervention Research at the Johns Hopkins University (P30 NR008995).
References
- 1. Dennison CR, Post WS, Kim MT, et al. Underserved urban African American men: hypertension trial outcomes and mortality during 5 years. Am J Hypertens. 2007;20(2):164–171. [DOI] [PubMed] [Google Scholar]
- 2. Ong KL, Cheung BM, Man YB, et al. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75. [DOI] [PubMed] [Google Scholar]
- 3. US Department of Health and Human Services. Asian American and Pacific Islanders: Executive Overview. The office of Minority Health Resource Center; 1998. [Google Scholar]
- 4. He J, Klag M, Whelton P, et al. Migration, blood pressure pattern, and hypertension: the Yi Migrant Study. Am J Epidemiol. 1991;134(10):1085–1101. [DOI] [PubMed] [Google Scholar]
- 5. Pollard TM, Carlin LE, Bhopal R, et al. Social networks and coronary heart disease risk factors in South Asians and Europeans in the UK. Ethn Health. 2003;8(3):263–275. [DOI] [PubMed] [Google Scholar]
- 6. Singh LP, Kaur B. Impact of migration, environment and socioeconomic conditions on blood pressure of Sikhs. J Biosoc Sci. 1998;30(2):155–164. [DOI] [PubMed] [Google Scholar]
- 7. Trowell HC. From normotension to hypertension in Kenyans and Ugandans 1928–1978. East Afr Med J. 1980;57(3):167–173. [PubMed] [Google Scholar]
- 8. Mustacchi P. Stress and hypertension. West J Med. 1990;153(2):180–185. [PMC free article] [PubMed] [Google Scholar]
- 9. Kim MT, Juon HS, Hill MN, et al. Cardiovascular disease risk factors in Korean American elderly. West J Nurs Res. 2001;23(3):269–282. [DOI] [PubMed] [Google Scholar]
- 10. Kim M, Han HR, Kim KB, et al. The use of traditional and Western medicine among Korean American elderly. J Community Health. 2002;27(2):109–120. [DOI] [PubMed] [Google Scholar]
- 11. Hurh WM, Kim KC. Correlates of Korean immigrants' mental health. J Nerv Ment Dis. 1990;178(11):703–711. [DOI] [PubMed] [Google Scholar]
- 12. National Heart, Lung, and Blood Institute . The Seventh Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Washington DC: NIH Publications; 2003. [PubMed] [Google Scholar]
- 13. Hess PL, Reingold JS, Jones J, et al. Barbershops as Hypertension Detection, Referral, and Follow‐Up Centers for Black Men. Hypertension. 2007;49(5):1040–1046. [DOI] [PubMed] [Google Scholar]
- 14. Scisney‐Matlock M, Glazewki L, McClerking C, et al. Development and evaluation of DASH diet tailored messages for hypertension treatment. Appl Nurs Res. 2006;19(2):78–87. [DOI] [PubMed] [Google Scholar]
- 15. Bosworth HB, Olsen MK, Gentry P, et al. Nurse administered telephone intervention for blood pressure control: a patient‐tailored multifactorial intervention. Patient Educ Couns. 2005;57(1):5–14. [DOI] [PubMed] [Google Scholar]
- 16. Szirmai LA, Arnold C, Farsang C. Improving control of hypertension by an integrated approach‐results of the “Manage it well!” programme. J Hypertens. 2005;23(1):203–211. [DOI] [PubMed] [Google Scholar]
- 17. Han H, Kang J, Ko M, et al. Barriers to and strategies of recruiting Korean Americans for community‐partnered health promotion projects. J Immigr Minor Health. 2007;9(2):137–146. [DOI] [PubMed] [Google Scholar]
- 18. Braden CJ. Learned self‐help response to chronic illness experience: a test of three alternative learning theories. Sch Inq Nurs Pract. 1990;4(1):23,41; discussion 43–45. [PubMed] [Google Scholar]
- 19. Braden CJ. National Institute of Nursing (NINR) Final report: Learned self‐help response to chronic illness experience. 1993; Final report for 1 R29 NR01696–01–05.
- 20. Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self‐management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1):5–14. [DOI] [PubMed] [Google Scholar]
- 21. Lorig KR, Ritter P, Stewart AL, et al. Chronic disease self‐management program: 2‐year health status and health care utilization outcomes. Med Care. 2001;39(11):1217–1223. [DOI] [PubMed] [Google Scholar]
- 22. Israel BA, Schulz AJ, Parker EA, et al. Review of community‐based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. [DOI] [PubMed] [Google Scholar]
- 23. Chrisman NJ, Senturia K, Tang G, et al. Qualitative process evaluation of urban community work: a preliminary view. Health Educ Behav. 2002;29(2):232–248. [DOI] [PubMed] [Google Scholar]
- 24. Lantz PM, Viruell‐Fuentes E, Israel BA, et al. Can communities and academia work together on public health research? Evaluation results from a community‐based participatory research partnerships in Detroit. J Urban Health. 2001;78(3):495–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Henderson DJ. Consciousness raising in participatory research: method and methodology for emancipatory nursing inquiry. ANS Adv Nurs Sci. 1995;17(3):58–69. [DOI] [PubMed] [Google Scholar]
- 26. Pearlin LI, Schooler C. The structure of coping. J Health Soc Behav. 1978;19(1):2–21. [PubMed] [Google Scholar]
- 27. Barrera M. A method for the assessment of social support networks in community survey research. Connections. 1980;3(3):8–13. [Google Scholar]
- 28. Rosenbaum M. Learned resourcefulness as a behavioral repertoire for the self‐regulation of internal events: issues and speculations. In: Rosenbaum EA, ed. Perspectives on Behavior Therapy in the Eighties. New York, NY: Springer Publishing Co; 1990. [Google Scholar]
- 29. Grimes DE, Cole FL. Self‐help and life quality in persons with HIV disease. AIDS Care. 1996;8(6):691–699. [DOI] [PubMed] [Google Scholar]
- 30. LeFort SM, Gray‐Donald K, Rowat KM, et al. Randomized controlled trial of a community‐based psychoeducation program for the self‐management of chronic pain. Pain. 1998;74(2–3):297–306. [DOI] [PubMed] [Google Scholar]
- 31. Kim MT, Kim KB, Juon HS, et al. Prevalence and factors associated with high blood pressure in Korean Americans. Ethn Dis. 2000;10(3):364–374. [PubMed] [Google Scholar]
- 32. Shin H, Kim MT, Juon HS, et al. Patterns and Factors Associated with Health Care Utilization among Korean American Elderly. Asian Am Pac Isl J Health. 2000;8(2):116–129. [PubMed] [Google Scholar]
- 33. Kang JH, Han HR, Kim KB, et al. Barriers to care and control of high blood pressure in Korean‐American elderly. Ethn Dis. 2006;16(1):145–151. [PubMed] [Google Scholar]
- 34. Kim MT, Han HR, Park HJ, et al. Constructing and testing a self‐help intervention program for high blood pressure control in Korean American seniors‐a pilot study. J Cardiovasc Nurs. 2006;21(2):77–84. [DOI] [PubMed] [Google Scholar]
- 35. Han H, Kim K, Pistulka G, et al. Evaluating process outcomes of a self‐help Intervention for Korean American Elderly with Hypertension. In: Addressing Issues in health care disparities through research and practice. 17th Annual Pacific Nursing Research Conference; March 1920, 2004; Honolulu, HI. [Google Scholar]
- 36. Kim K, Han W, Kim M, et al. A community‐based smoking cessation program for Korean Americans in Maryland. In: National Conference on Tobacco or Health; December 1012, 2003; Boston, MA. [Google Scholar]
- 37. Han H, Kim K, Kang J, et al. Knowledge, beliefs, and behaviors about hypertension control among middle‐aged Korean Americans with hypertension. J Community Health. 2007;32(5):324–342. [DOI] [PubMed] [Google Scholar]
- 38. Maryland Department of Health and Mental Hygiene. Maryland Annual Vital Statistics Reports; 2005. [Google Scholar]
- 39. National Heart, Lung and Blood Institute. 2004 NHLBI Morbidity and Mortality Chartbook;2004. [Google Scholar]
- 40. Bobrie G, Chatellier G, Genes N, et al. Cardiovascular prognosis of “masked hypertension” detected by blood pressure self‐measurement in elderly treated hypertensive patients. JAMA. 2004;291(11):1342–1349. [DOI] [PubMed] [Google Scholar]
- 41. Staessen JA, Byttebier G, Buntinx F, et al. Antihypertensive treatment based on conventional or ambulatory blood pressure measurement. A randomized controlled trial. Ambulatory Blood Pressure Monitoring and Treatment of Hypertension Investigators . JAMA. 1997;278(13):1065–1072. [PubMed] [Google Scholar]
- 42. Rogoza AN, Pavlova TS, Sergeeva MV. Validation of A&D UA‐767 device for the self‐measurement of blood pressure. Blood Press Monit. 2000;5(4):227–231. [DOI] [PubMed] [Google Scholar]
- 43. Bloomfield R, Young LD, Graves J. Racial differences in perceptions concerning hypertension and its consequences. South Med J. 1993;86(7):767–770. [DOI] [PubMed] [Google Scholar]
- 44. Kim MT, Hill MN, Bone LR, et al. Development and testing of the Hill‐Bone Compliance to High Blood Pressure Therapy Scale. Prog Cardiovasc Nurs. 2000;15(3):90–96. [DOI] [PubMed] [Google Scholar]
- 45. Ard JD, Rosati R, Oddone EZ. Culturally‐sensitive weight loss program produces significant reduction in weight, blood pressure, and cholesterol in eight weeks. J Natl Med Assoc. 2000;92(11):515–523. [PMC free article] [PubMed] [Google Scholar]
- 46. Poston WS, Reeves RS, Haddock CK, et al. Weight loss in obese Mexican Americans treated for 1‐year with orlistat and lifestyle modification. Int J Obes Relat Metab Disord. 2003;27(12):1486–1493. [DOI] [PubMed] [Google Scholar]
- 47. Pierce LL, Steiner V, Govoni AL, et al. Internet‐based support for rural caregivers of persons with stroke shows promise. Rehabil Nurs. 2004;29(3):95, 99, 103. [DOI] [PubMed] [Google Scholar]
- 48. Fogle CC, Oser CS, Blades LL, et al. Increasing employee awareness of the signs and symptoms of heart attack and the need to use 911 in a State Health Department. Prev Chronic Dis. 2004;1(3):A07. [PMC free article] [PubMed] [Google Scholar]
- 49. Snow WM, Connett JE, Sharma S, et al. Predictors of attendance and dropout at the Lung Health Study 11‐year follow‐up. Contemp Clin Trials. 2007;28(1):25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. McFarland LV, Reiber GE, Norman JE. Recruitment of Medicaid and dual‐enrolled Medicare beneficiaries with diabetes mellitus into a randomized controlled trial. Am J Manag Care. 2005;11(7):443–448. [PubMed] [Google Scholar]
- 51. Moser M, Franklin SS. Hypertension management: results of a new national survey for the hypertension education foundation: Harris interactive. J Clin Hypertens (Greenwich). 2007;9:316–323. [DOI] [PMC free article] [PubMed] [Google Scholar]


