Introduction
The term health gradient is widely used to describe the ways in which mortality and morbidity are related to social position; the higher the social status the better the health, and conversely, the lower the social status the worse the health. This population level pattern has been noted since modern records began.1 This paper considers some of the theoretical, conceptual and methodological issues which are attached to the health gradient and the implications of these for the methods of evidence accumulation and synthesis and evidence-based medicine more generally.
The gradient
The gradient describes a pattern which is formed by comparing measures of mortality and morbidity with some measure of social position. Originally, the social measure was occupation or occupation of head of household.2 Occupation has tended to be readily available in official statistics and has been a good proxy for a range of other aspects of life chances including education, income, housing tenure and social class.
Data collected by Banks and colleagues3 nicely illustrate the gradient. Comparing the UK and USA, they found similar patterns of graded health differences for, among other things, self-assessed health, diabetes, heart disease and lung disease. The same gradient can be seen in the Black Report of the 1980s,4 the Acheson Report of the 1990s,5 and most recently and comprehensively in the Status reports of the Department of Health6 and the Marmot Review of 2010.7 There are many texts and papers which describe the phenomenon. And of course it is not restricted to Britain and scholars have demonstrated that this kind of gradient is common in all developed societies.8–11 The steepness of the gradient and the differences between the top and bottom do vary between societies.12 However, there is a degree of commonality in developed societies in that the nature of the gradient tends to be smooth showing a gradual rise in mortality and morbidity as social position declines. In less developed and middle-income countries the shape of the gradient tends to be less smooth, reflecting different patterns of income distribution and levels of poverty as data collected by Victora and colleagues show.13
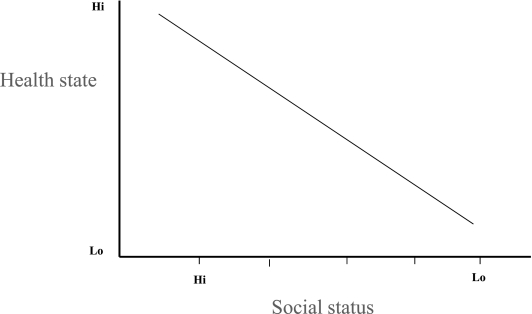
The measures used to describe health or disease at any point on the gradient represents a value. This could be a measure of mortality, the number of cases of cardiovascular disease or responses to a questionnaire describing self-rated health (Figure 1). These measures are helpful in observing changes over time for particular groups because mortality rates may change, the number of cases may rise or fall and people's feelings about their health may change. Such measures are helpful in observing the overall health improvement or overall health decline over time for particular groups.
Figure 1.
The schematic health gradient
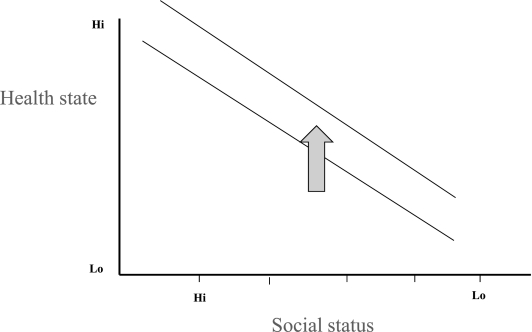
Thinking about the measures relatively though is at the heart of the idea of the gradient. This is because it allows the comparison to be made between groups and how these comparisons may change relative to each other over time. So it is possible to think of a particular gradient made up of absolute measures of health at a particular point in time. If we imagine a population level public health intervention which would affect the whole population similarly then we would anticipate that the gradient as a whole would shift upwards uniformly and by the same amount ( Figure 2). Under such circumstances the absolute health of everybody would be seen to have improved by the same amount. This might be judged to be a good thing. However, if the gradient simply shifts up at the same rate for all groups, the relative differences between the groups remain unchanged, and in that sense health inequity has not changed.
Figure 2.
The health gradient showing uniform improvement
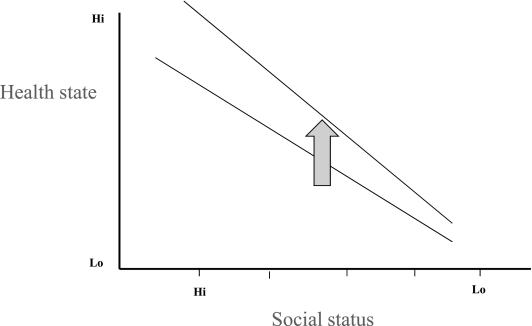
But it is still more difficult because the effect of some public health interventions is to improve the health of the already advantaged more quickly than the less advantaged, or sometimes earlier in the lifecycle of an intervention.14 This means that although the absolute health of all groups is improving, the rate at which it is improving is faster in absolute terms for those already in the best health. In this case the relative differences are getting greater or worse and the pattern of health inequity is getting worse across society as a whole (Figure 3).
Figure 3.
The health gradient showing relative health inequalities getting worse
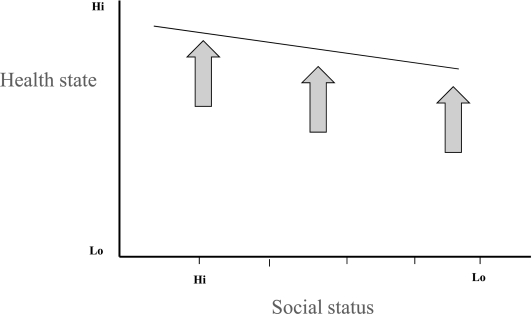
In schematic terms, if the goal of a policy or an intervention is to change the overall pattern of health inequity, a more targeted approach is required which would result in the rate of improvement being faster for those groups whose starting point is worse to begin with, and so shifting the gradient in such a way that it becomes less steep (Figure 4).
Figure 4.
Shifting the health gradient through universal and targeted action
The approach to trying to achieve this goal is sometimes referred to as targeted universalism or progressive universalism. The goal is overall health improvement for all via the delivery of universal reach to the whole population. But those groups with special or greatest need are targeted in order to get the maximum impact.
The axes of social differentiation
However, there are a number of problems in achieving this goal. The measures of socioeconomic grouping, occupation or social class, while useful in describing the overall gradient, are too coarse to capture the finer grained detail of the fabric of social life in a contemporary developed society like modern Britain. We need to be able to describe as accurately as possible the different axes of social differentiation in modern society.
The χ axis in Figures 1–4 represents social variation in the population. Social variation can be measured in a number of ways, and in a complex multicultural society is made up of many elements and facets. These include the obvious and traditional one of occupation, but extend to ethnicity, geography, sexual orientation, lifestyle, social status, and many other micro dimensions of social, economic and political life in modern Britain.15 These different elements interact with each other, they overlap, they are mutually reinforcing and dynamic and changing.
This means that trying to capture the complexity in a single measure like occupation, socioeconomic grouping or income is always going to be both static and blunt. It also provides little by way of direction as to how to do the targeting of the different parts of the population in order to accelerate the absolute changes in the health status of the most disadvantaged. Further, it leaves unanswered the question of which elements are the most important to act upon first in order to achieve the outcomes which are sought.
These different elements of social differentiation affect health and disease, but we have little information, empirically or theoretically about in what proportion and to what degree. So, for example, when thinking about the health state of a Bangladeshi woman living in Tower Hamlets, one of London's poorest boroughs, we can predict that that woman's state of health is likely to be poor and worse than a white middle-class woman of the same age living a few miles away in the richer and healthier borough of Richmond upon Thames. But for this Bangladeshi woman, what are the noxious factors at work creating greater vulnerability and exposure and for that matter what produces the resilience and the resistance in the middle-class woman in Richmond? Is it class position linked to income and access to resources? Is it the racism inherent in the provision of services to the Bangladeshi community? Is it gender relations in the Bangladeshi community itself? Is it that the woman in Tower Hamlets lives in a cold damp house? Is it that she works in the informal labour market and does not enjoy the protection of occupational health legislation? If, as it probably is, a mixture of all these things, is there an additive effect between these different elements? Is it synergistic or what? In short, the answer to this is not clear because we do not have the empirical data or the evidence to answer the question. Therefore, the nature of the way to engage with the most important elements in a targeted way is not to hand in a practical sense.
Individual and relational factors
What are required are very detailed and accurate descriptions of the social worlds of the inhabitants of modern Britain. This needs to move beyond static descriptions to dynamic and relational understandings of the changing, overlapping and coalescing groups and the ways these influence vulnerability, exposure, risk and health.16 This kind of description is strikingly absent in the literature where static descriptors of occupation, income or ethnicity are used and treated as if they were individual characteristics not properties of dynamic group relations.
Occupation, or social class or socioeconomic grouping can be treated as a characteristic of an individual to all intents and purposes similar to an individual biological characteristic like diastolic blood pressure; self-reported health state, or the absence, presence or degree of pathology. But social class or socioeconomic grouping and ethnicity and gender are relational variables. That is they describe the nature of relationships between groups of people and at the heart of those relationships are fundamental conflicts over power, access to resources and life chances more generally. They are, therefore, among the distal factors which explain both individual disease states and population level patterns of disease. Although individual disease states have immediate and proximal biological causes, the vulnerability to disease, and indeed the mechanisms leading to exposure are frequently not biological, but originate in the social circumstances in which people live and work and the relationships between groups and individuals. This is not in some background contextual way but in a direct causal way.
Consequences for the evidence-based approach
This is very important from an evidence accumulation point of view because it means that de facto there is a big hole in our data and understanding and developing an evidence base which would allow the targeted public health actions remains an aspiration.17,18 It is interesting to speculate as to why, while we are very familiar with the idea of biological variation in the population down to the cellular, molecular and genetic levels and engage in exciting research to link these biological variables to disease susceptibility, risk and responses to pharmaceutical interventions, the importance of social variation and its impact on risk, susceptibility, outcome, remains highly undeveloped. The evidence of social variation is ubiquitous, yet its importance remains scientifically under-elaborated.
The evidence-based approach19 has been one of most significant scientific paradigm shifts of the last 40 years or so. The idea of the cumulation and synthesis of the best available evidence as a means of eliminating bias has been fundamental. Its efforts in the fields of clinical medicine have been enormously important. However, the evidence-based approach in public health has been far slower to develop. There are a variety of reasons for this but what is undoubtedly the case is that the moment an attempt is made to apply the evidence-based orthodoxy to relational factors problems will arise. This is because relational factors do not fit well into a system designed to capture individual level phenomenon and require a social not an individual level of explanation.20
The patterning of health inequity arises because of the relationships between classes, genders and ethnic groupings and the locations of these in broader systems of economic and political organization as dynamic processes. The evidence-based orthodoxy can capture static and individual level variables; it fares much less well in trying to capture the dynamic and social level. Of course things like class, gender and ethnicity are captured by in epidemiological data and in syntheses of these data. But this is usually done by reducing the relational variables to the status of individual level variables and treating social class and ethnicity as if they were only an individual characteristic. Of course they can be treated this way, but only at the expense of losing the dynamic and relational quality of the variables involved.
One of the consequences of this is that the hierarchy of evidence which has been developed to assist in the assessment of the probability of bias has to be used with some caution with relational variables. This is because the types of study which capture the nature of power relationships, gender relationships and relations between different ethnic groups are not amenable to data manipulation at the level of meta-analyses, or of randomized controlled trials. At best we may be able to find observational studies. But what is much more likely is that the studies are likely to consist of descriptive studies with associated modelling and theory. These do not fit anywhere very much on the evidence hierarchy except near the bottom. So an altogether different kind of approach to thinking about the quality of evidence has to be adopted involving assessing the value of and parsimony and even the aesthetics and logic of the models, the theories and the descriptions. This is not underdeveloped, and philosophers, logicians, methodologists in the social sciences as well as social theorists and psychologists have finely-honed tools to use in the assessment of this kind of material, and have had for many years. There are even ways to try to extricate the theories and models from any underlying ideological presuppositions they may contain. It is not that such approaches do not exist; it is rather that they have not migrated to the world of evidence-based medicine and are mostly unfamiliar to its practitioners (see, for example, Blalock;21 and Lazarsfeld22 for an introduction to the highly sophisticated approaches developed in the behavioural and social sciences, which pre-date evidence-based medicine by at least a decade).
The problem of cause: individual and social
One of the enduring problems in public health has been the way in which individual and social level explanations are sometimes conflated. It is relatively straightforward to understand the causal pathway at the level of the individual. Pathology occurs in the human body, in an individual's cells and systems. The individual feels pain and suffers and the consequences of such morbidity are familiar to everyone. Medicine provides detailed explanations of the origins of such biological events in the individual. And also in many cases provides an ameliorative or curative therapy based on an understanding of the causal pathway. The origins of the pathology may be proximal, such as chance exposure to a virus or bacteria. Sometimes the originating cause is more distal in some aspect of environmental or occupational exposure to hazards like radiation or asbestos. But even in these cases of distal origins, the explanatory pathway is clear and operates at the level of the individual.
However, there is another equally important pathway that operates at the level of the social or population.16 There are clear patterns of population health. Epidemiologists have successfully described these over many years. These patterns take a variety of forms. The ones which are most familiar are those relating to differences in mortality and morbidity linked to social position or its proxies – income and education. The gradient described above is quintessential in this respect. One way of thinking about the patterns is to assume that they represent the aggregation of individual events. So the differences in mortality and morbidity at population level are the summation of lots of different individual disease episodes. And of course so it is. But the patterns can also be conceptualized as a social reality of their own. The fact is that the patterns themselves repeat themselves and reproduce generation after generation. The pattern has a quality of systemness or structure which exists above and beyond the individual events.
Two ideas illustrate this point. First, in the mid-19th century the principal causes of death were infectious disease. In the early 21st century the principal causes are diseases associated with smoking, diet, alcohol misuse and lack of exercise. Although the biological mechanism involved in the pathology then and now are quite different, the associated diseases still kill more of the relatively disadvantaged prematurely than those from more privileged backgrounds, just as was the case in the 19th century. In other words, quite different biological processes produce startlingly similar patterns. Second, at geographical level the data also have quite remarkable permanent patterning. In 1862, William Gairdner, the first medical officer of health in Glasgow, in his treatise on air, water and cholera, drew up tables to show where the highest rates of infant and premature mortality were to be found. His list shows an eerily familiar overlap with contemporary albeit more finely-grained data. There is not an exact match but somewhere like Tower Hamlets in the East End of London was an unhealthy place in 1862 and it is today. The population has changed considerably in that time by national and ethnic origin, but the pattern of health inequality is reproduced. So an explanation is needed both of the individual disease outcomes and the patterns. The two causal pathways overlap, certainly, and the factors involved interact with each other, but there are two different things to be explained.
The 19th-century pioneers in public health understood this at least intuitively. One can certainly draw the impression reading Gairdner's work1 or that of Duncan, the first medical officer of health in Liverpool,23 that they tried to understand social level causes as they described the social conditions of their cities. Bearing in mind that the biological agents which caused some of the infections that Gairdner and Duncan observed had yet to be identified and that theories of contagion were disbelieved by large sectors of society, they trod a path which in the end led them to work within a conventional individualistic biomedical paradigm. Indeed, it was not until 1897 that Durkheim fully articulated empirically the idea of the social level having social causes separate from the individual.24 But when Gairdner and Duncan were practising this idea, in modern scientific terms, was still some way off, and has never really gained an intellectual foothold in public health or medicine. Of course the idea that there was a social level with its own reality and its own power to impact on humans was not new – even when Durkheim described it empirically and may be found in the writings of enlightenment philosophers like Hobbes, Locke, Hume, and Kant.25–27
However, in practical if not theoretical sense the 19th-century pioneers did get it, and the great sanitation schemes of Bazelgette in London and similar efforts in continental Europe attest to an understanding of the possibility of intervening at population level and influencing the social level very effectively. Indeed, to some extent the major advances in the health of the public of the early period of public health were mostly attributable to the impact of these population level inputs. It was the eventual discovery of the individual microbiological agent that led to the shift in emphasis and the dominance of the individual approach and consequently less attention spent on the population level explanations per se.
Of course a fully-rounded approach to public health requires both the individual and social levels of explanation both for the sake of an all-embracing approach and in order to capture the significant interactions between the individual and the social level phenomena. These interactions are important because they not only articulate the causal pathways to the individual disease outcomes, but they demonstrate the various linkages between different phenomena. This potentially allows for the possibility of much more precise approaches to defining interventions and where and how such interventions should be targeted. They are also important in reading off and interpreting the patterns described in the gradient.
Conclusion
The conclusions to be drawn from these observations are as follows. First, the evidence-based approach is a most fundamental and important development and its benefits to medicine have been immense. The power of cumulative findings assessed for their freedom from bias, evaluated using well-defined and agreed criteria as the basis for clinical decision-making has been a great advance methodologically. Second, the approach works well when applied to variables which in one form or another are located in biological individuals. Third, public health with its abiding interest in inequities in health whether conceived of in terms of class, gender and ethnicity, has developed the idea of the health gradient to describe patterning of health and disease. Fourth, these patterns use familiar individually-based variables like mortality and morbidity to describe the differences and these can be represented using the health gradient. It is important to distinguish between absolute and relative differences when interpreting the gradient and changes in it. Fifth, the gradient not only shows that there are important individual differences in mortality and morbidity but also that these differences are patterned at population level. Sixth, that patterning requires an explanation at the level of the social, because the patterning not only arises because of individual biological events in the human body but also because of social, economic and wider determinants of health which are themselves the products of the nature of social, economic and political relationships between groups of people. The relational factors which are involved in the wider determinants are not well-suited to being captured by the evidence-based orthodoxy, because the importance of the dynamic relationships between groups can be obscured. Further, the types of studies necessary to capture the dynamic nature of the relationships do not fit at all well with the precepts of the hierarchy of evidence and, therefore, a methodological pluralism is needed which is capable of acknowledging the strengths and the weaknesses in studies which are descriptive, uncontrolled and use theory and models as the way of constructing their explanations.
In the final analysis in order to develop better understandings and explanations of the things which affect health in a directly causal way such as class, ethnicity and gender relations, a pluralistic approach to methods, data and evidence synthesis is needed. The possibilities are considerable, and the gains from taking a pluralistic approach very important. What is needed is an acknowledgement that there are different ways of knowing things, an observation made millennia ago by Plato.28 We ignore that basic precept of our own intellectual heritage at our peril.
Footnotes
DECLARATIONS —
Competing interests The author works for the NHS at the National Institute for Health and Clinical Excellence (NICE). The ideas in this paper have been generated in the course of his leading the Public Health Programme at NICE. The ideas and opinions are those of the author and not those of NICE or the Department of Health which funds NICE
Funding None
Ethical approval Not applicable
Guarantor MPK
Contributorship MPK is the sole contributor
Acknowledgements
None
References
- 1.Gairdner WT. Public Health in Relation to Air and Water. Edinburgh: Edmonston & Douglas; 1862 [Google Scholar]
- 2.Graham H, Kelly MP. Health inequalities: concepts, frameworks and policy. London: Health Development Agency; 2004. See http://www.nice.org.uk/page.aspx?o=502453 [Google Scholar]
- 3.Banks J, Marmot M, Oldfield Z, Smith JP. The SES Health Gradient on Both Sides of the Atlantic. Cambridge, MA: National Bureau of Economic Research; 2006 [Google Scholar]
- 4.Townsend P, Davidson N, eds. Inequalities in Health: The Black Report. London: Penguin; 1982 [Google Scholar]
- 5.Acheson D. Independent Inquiry into Inequalities in Health: Report. London: The Stationery Office; 1998 [Google Scholar]
- 6.Department of Health Health Inequalities Unit Tackling Health Inequalities: 10 Years On – A Review of Developments in Tackling Health Inequalities in England Over the Last 10 Years. London: Department of Health; 2009 [Google Scholar]
- 7.Marmot M. Fair Society, Healthy Lives: Strategic Review of Health Inequalities in England post 2010. London: University College London; 2010. See http://www.ucl.ac.uk/gheg/marmotreview/Documents/finalreport [Google Scholar]
- 8.Mackenbach J. Health Inequalities: Europe in Profile. London: COI for the UK Presidency of the EU; 2005 [Google Scholar]
- 9.Siegrist J, Marmot M. Social Inequalities in Health: New Evidence and Policy Implications. Oxford: Oxford University Press; 2006 [Google Scholar]
- 10.CSDH Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Geneva: WHO; 2008 [DOI] [PubMed] [Google Scholar]
- 11.Wilkinson R, Pickett K. The Spirit Level. London: Allen Lane; 2009 [Google Scholar]
- 12.Bonnefoy J, Morgan A, Kelly MP, et al. Constructing the evidence base on the social determinants of health: A guide. London: National Institute for Health and Clinical Excellence; 2007. See http://www.who.int/social_determinants/knowledge_networks/add_documents/mekn_final_guide_112007.pdf [Google Scholar]
- 13.Victora CG, Fenn B, Bryce J, Kirkwood BR. Co-coverage of preventive interventions and implications for child-survival strategies: evidence from national surveys. Lancet 2005;366:1460–6 [DOI] [PubMed] [Google Scholar]
- 14.Victora CG, Vaughan JP, Barros FC, Silva AC, Tomasi E. Explaining trends in inequalities: evidence from Brazilian child health studies. Lancet 2000;356:1093–8 [DOI] [PubMed] [Google Scholar]
- 15.Kelly MP. Mapping the life world: a future research priority for public health. In: Killoran A, Swann C, Kelly MP, eds. Public Health Evidence: Tackling Health Inequalities. Oxford: Oxford University Press; 2006. pp. 553–74 [Google Scholar]
- 16.Kelly MP. A theoretical model of assets: the link between biology and the social structure. In: Morgan A, Ziglio E, Davies M, eds. Health Assets in a Global Context. New York, NY: Springer; 2010. (in press) [Google Scholar]
- 17.Kelly MP. The development of an evidence-based approach to tackling health inequalities in England. In: Killoran A, Swann C, Kelly MP, eds. Public Health Evidence: Tackling Health Inequalities. Oxford: Oxford University Press; 2006. pp. 41–62 [Google Scholar]
- 18.Killoran A, Kelly MP, eds. Evidence Based Public Health: Effectiveness and Efficiency. Oxford: Oxford University Press; 2009 [Google Scholar]
- 19.Egger M, Davey Smith G, Altman BG. Systematic Reviews in Health Care: Meta-analysis in Context. London: BMJ Books; 2001 [Google Scholar]
- 20.Kelly MP. The individual and the social level in public health. In: Killoran A, Kelly MP, eds. Evidence-Based Public Health: Effectiveness and Efficiency. Oxford: Oxford University Press; 2009. pp. 425–351 [Google Scholar]
- 21.Blalock HM. Evaluating the relative importance of variables: In: Lazarsfeld PF, Pansanella AK, Rosenberg M, eds. Continuities in the Language of Social Research. New York, NY: Free Press; 1972 [Google Scholar]
- 22.Lazarsfeld PF. Concept formation and measurement in the behavioural sciences: some historical observations. In: Di Renzo G, ed. Concepts, Theory and Explanation in the Behavioral Sciences. New York, NY: Random House; 1966. pp. 144–205 [Google Scholar]
- 23.Frazer WM. Duncan of Liverpool: Being an Account of the Work of Dr WH Duncan Medical Officer of Health of Liverpool 1847–63. London: Hamish Hamilton; 1947 [Google Scholar]
- 24.Durkheim E. Suicide: A Study in Sociology. London: Routledge & Kegan Paul; 1952 [Google Scholar]
- 25.Woolhouse RS. The Empiricists: A History of Western Philosophy: 5. Oxford: Oxford University Press; 1988 [Google Scholar]
- 26.Hume D. An Enquiry Concerning Human Understanding. Oxford: Oxford University Press; 2007 [Google Scholar]
- 27.Kant I. Critique of Pure Reason. Basingstoke: Palgrave Macmillan; 2003 [Google Scholar]
- 28.Plato The Republic. 2nd edn Harmondsworth: Penguin; 1974 [Google Scholar]