Abstract
Vascular endothelial growth factors (VEGFs) are key regulators of permeability. The principal evidence behind how they increase vascular permeability in vivo and in vitro and the consequences of that increase are addressed here. Detailed analysis of the published literature has shown that in vivo and in vitro VEGF-mediated permeability differs in its time course, but has common involvement of many specific signalling pathways, in particular VEGF receptor-2 activation, calcium influx through transient receptor potential channels, activation of phospholipase C gamma and downstream activation of nitric oxide synthase. Pathways downstream of endothelial nitric oxide synthase appear to involve the guanylyl cyclase-mediated activation of the Rho–Rac pathway and subsequent involvement of junctional signalling proteins such as vascular endothelial cadherin and the tight junctional proteins zona occludens and occludin linked to the actin cytoskeleton. The signalling appears to be co-ordinated through spatial organization of the cascade into a signalplex, and arguments for why this may be important are considered. Many proteins have been identified to be involved in the regulation of vascular permeability by VEGF, but still the mechanisms through which these are thought to interact to control permeability are dependent on the experimental system, and a synthesis of existing data reveals that in intact vessels the co-ordination of the pathways is still not understood.
Keywords: VEGF, Vascular permeability, Calcium, Capillary, Endothelium
1. Importance of vascular endothelial growth factor-mediated permeability in health and disease
The discovery of vascular endothelial growth factor (VEGF) in the 1980s reflects to some degree the continuing revision of our understanding of what this critical molecule does in humans, its mechanisms of action, and its cellular targets. For, while VEGF was originally purified as a tumour-secreted factor, it was done so using an assay designed not for vessel growth but increased extravasation of dye. Thus, it was termed vascular permeability factor by Dvorak and Senger when they partially purified it,1 although neither investigator measured its effect on vascular permeability per se.2 It was subsequently also identified in 19893 to be the long sought after tumour angiogenesis factor4 separately by two endocrinologists who had recently worked in the same laboratory (Ferrara and the late Plouet, who both worked with Denis Gospadorowicz at UCSF in 1988), and was termed vasculotropin by Plouet et al.5 and VEGF by Ferrara and co-workers.6,7 However, VEGF acts on many cell types, including epithelial,8 nerve,9 and tumour cells10 and can act as either a stimulator6 or inhibitor of endothelial cell growth.11 Our understanding has therefore undergone such a radical revision since 1989 that the term VEGF now applies to a molecule that may or may not be either vascular, endothelial, or growth specific.
Subsequent investigations on how VEGF acts to increase vascular permeability are also complex, confusing, and in many cases contradictory. This review will attempt to pull together much of the work on how VEGF acts to increase vascular permeability, and what its role is in health and disease.
1.1. What is VEGF?
The VEGF family of proteins consists in humans of five separate gene products, termed VEGF-A (or VEGF), VEGF-B,12 VEGF-C,13 VEGF-D,14 and placental growth factor (PlGF).15 They are members of the superfamily of platelet derived growth factors cysteine knot proteins that are characterized by eight cysteines that form stable dimeric bonds resulting in dimers in a head to tail conformation.16 VEGF-A can be generated by almost all cells under hypoxic17 or other stress conditions,18 including endothelial cells,19 and are highly expressed in tissues undergoing growth or remodelling including cancers,20 atherosclerosis,21 and during remodelling of the female reproductive cycle.22 All five human VEGFs are generally alternatively spliced to form multiple isoforms with widely varying properties.
1.2. How do VEGFs work?
VEGFs act through ligand binding to their cognate VEGF receptors, in particular VEGFR1 (flt-1),23 VEGFR2 (flk1 in the mouse, KDR in the human),24 and VEGFR3 (flt4).25 All three receptors can be used by various isoforms of the various genes to signal to increase vascular permeability, angiogenesis, and other actions of VEGFs. All the receptors act by homo- and heterodimerization and activation of an intracellular tyrosine kinase activity, recruitment of SH2 domain binding proteins, and subsequent downstream signalling through multiple common signalling pathways.26 The link between these signalling pathways and vascular permeability regulation is, however, not so clear.
1.3. What is their effect?
The effects of VEGF on endothelial cells are profound, complex, and not simple to interpret. It is clearly a potent, though not very powerful, endothelial growth factor. It is a potent and powerful vascular permeabilizing agent,27 and a potent vasodilator.28 It increases migration of endothelial cells, new vessel formation,29 and has effects on the pericytes that surround endothelial cells,30 and on the matrix metalloproteinases secreted by endothelial cells.31 The net result of treatment with VEGF is hypotension when given centrally,32 leakage of fluid and protein from the vasculature to the tissue when secreted locally,33 and chaotically increased vascular growth if given alone.34 However, to understand the published evidence on how VEGF acts to increase vascular permeability it is necessary to define what we mean by vascular permeability.
2. What is permeability?
2.1. Permeability coefficients
The permeability of the vasculature is a property of the capillary wall to impede movement of fluid or solutes driven by a physical force. It is a primary contributor to the regulation of exchange of nutrients and water between tissues and blood. The other primary contributors, which are not dependent on the barrier, include size of the physical forces (pressure for convective flux of fluid and concentration gradient for diffusion of solutes) and surface area of the available barrier. Thus it is critical to identify whether parameters being measured during experiments to identify mechanisms through which VEGF acts are ones that affect properties of the barrier wall or are independent of it. This includes the hydrostatic pressure of capillaries and the interstitium, plasma and interstitial colloid osmotic pressure, concentration gradient of solutes acting across the vessel wall, and the number of capillaries being perfused. All these can be altered by changing blood flow to a tissue independently of changes in the barrier wall and VEGF being a potent vasodilator indicates that separation of a haemodynamic from barrier characteristics is critical for appropriate interpretation of these experiments.
There are three principal permeability coefficients of the capillary wall that can be used to indicate the quality of the barrier to impede flow of fluid or solutes.
2.1.1. Lp—hydraulic conductivity
The fluid flow per unit pressure gradient driving fluid across the barrier is the hydraulic conductivity. This parameter can be measured relatively straightforwardly in vitro and in vivo by determining the flow rate at specific hydrostatic or osmotic pressures across the vascular wall. In continuous capillaries, the pathway is thought to reside in the intercellular clefts of the vascular wall,35 although a significant proportion (up to 20%) may be across the plasma membrane and through the cell.36 In fenestrated capillaries (glomerulus, synovium, salivary gland), the pathway will be dominated by the fenestra which have a high hydraulic conductivity and surface area relative to the intercellular clefts.37 In endothelial cells in culture, the hydraulic conductivity will depend on confluence, and the basement membrane may come into play when measurements are made at higher pressures as the cells compress the basement membrane a ‘sealing’ effect may be seen.38
2.1.2. Ps—solute permeability
Solute permeability is the solute flux by diffusion per unit concentration gradient per unit area.39 The caveat ‘by diffusion’ is critical here, as solutes may also be carried across the vessel wall by convection, and therefore if the convective flux is not accounted for the permeability calculated is overestimated (apparent permeability).40 Ps can be measured in vivo and in vitro, often by extrapolating measurements of apparent permeability back to the point at which flow would cease.41
2.1.3. Oncotic reflection coefficient (σ)
A mixture of large and small molecular weight molecules will exert an osmotic pressure across a semi-permeable membrane proportional to the size of the channels through which molecules may cross.42 Thus if the membrane is permeable to water but not solutes, then the solution will exert its full osmotic pressure (and hence σ = 1). If the membrane is freely permeable to all solutes, then no osmotic pressure can be exerted and σ = 0. The inverse of σ is the sieving coefficient.
2.2. Measurement of the effect of VEGF on permeability
The effect of VEGF on permeability has been investigated using both in vitro and in vivo models.
2.2.1. In vitro
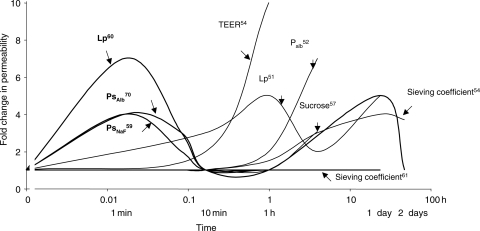
The permeability of endothelial monolayers has been extensively studied, but using three principal methodologies—measurement of hydraulic conductivity (Lp),43,44 transendothelial electrical resistance (TEER),45,46 and albumin transport (Palb).44,47 Lp is measured as described above (fluid flow per unit pressure per unit area of membrane). TEER is the current per unit voltage applied and is inversely proportional to the permeability to the principal charged ions (Na and Cl). Palb is usually measured by adding labelled albumin (often fluorescent) to one side of a monolayer and measuring the amount on the well on the other side of the layer. Using these three assays, the effect of VEGF has been shown to increase permeability in all three models, and there are a number of biochemical studies that have been carried out to investigate the mechanisms (described below). In most, but not all,44 studies of cultured endothelial cells, treatment with VEGF results in increased Lp48 or Ps (to either Na or albumin)44 that develops over a period of 1 h, peaks, and then a second wave occurs between 1 and 4 h (Figure 1).44,46,49 This has been shown for venous arterial and capillary endothelial cells, for cells from the brain,50 glomerulus,45 aorta, retina,44 skin,48 umbilical cord,44 and many other endothelial cell types. One caveat, however, is that in almost all in vitro models permeability is usually significantly higher than in in vivo equivalents. This needs to be borne in mind when interpreting data from monolayers in culture.51
Figure 1.
Time course of VEGF-induced permeability. Alterations in hydraulic conductivity (Lp), solute permeability to albumin (Palb), or small solutes such as Na fluorescein (PNaF), ions (TEER) or sucrose, or sieving coefficient are shown in vivo (bold) or in vitro.
2.2.2. In vivo
In vivo measurement of the effects of VEGF on barrier function per se have been done by the measurement of solute permeability to albumin,52 by hydraulic conductivity,53 and by oncotic reflection coefficient.54 However, the vast majority of studies that have attempted to investigate the effect of VEGF on permeability have used indirect measures, and in particular the accumulation of albumin associated dyes, or labelled albumin into the tissue.55 These latter studies cannot be ignored, but must be interpreted with caution. The most widely used assay was that originally used by Senger and Dvorak to identify VEGF,55 which is to inject Evans' blue incubated with albumin into an animal, and then treat the animal, usually by subcutaneous injection, with VEGF or inhibitors. The tissue is then photographed, and often excised and the amount of Evans blue measured after extraction. There are a number of assumptions that need to be borne in mind when considering these studies.
The delivery of a labelled solute to a tissue depends on the surface area, concentration difference, and driving forces for flux across the vessel wall, as well as the permeability. Thus as VEGF is a vasodilator,28 it results in perfusion of more capillaries and therefore the mechanisms through which it acts may be due to its action as a vasodilator rather than its barrier effects.
The flux of a large molecular weight molecule is primarily convective under low-permeability conditions, and therefore increased hydrostatic pressure will increase solute flux, and as again VEGF is a vasodilator it will increase hydrostatic pressure. In addition, any agent investigated that acts to increase venous pressure will increase post-capillary resistance and therefore increase solute flux.
Evans blue forms an equilibrium binding with albumin. It can be >99% bound to albumin but its free dye concentration is highly dependent on preparation and both dye and albumin concentration. For instance, at 17 mM Evans blue, there is 34% free dye in 6% albumin.56–58 As Evans blue is 50× smaller than albumin, it would be expected to have a permeability of at least 50× that of albumin.59 Moreover, while it is in equilibrium in the plasma and predominantly bound, as soon as it crosses the vessel wall it will again bind albumin and therefore the concentration gradient of Evans blue will remain high as the interstitial concentration is effectively zero. However, if plasma flows slowly through a capillary, as it reaches the end of the capillary the plasma concentration will fall as molecules have diffused into the tissue. If flow rate is increased this concentration will not fall so quickly, so maintaining a higher concentration difference across the vessel wall and so delivering more Evans blue (this is of course how increasing blood flow increases oxygen delivery). This flow limited solute flux60 can explain a large proportion of Evans blue extravasation. Moreover, as permeability increases, albumin flux now also becomes flow limited, so combining increased flow with increased permeability will amplify the solute flux.
Use of a single label such as Evans blue does not distinguish between extravasated dye and dye bound to the surface layer of the endothelium, or still in the blood, and hence increased blood flow will again contribute.
3. How does VEGF increase permeability?
3.1. Time course
Whereas in vitro VEGF results in a slow increase in permeability that peaks at 1 h and then a second continuing peak occurs that lasts for between 1 and 3 days, in vivo there is a great discrepancy in published data. Application of a single bolus of VEGF-A or VEGF-C and measurement of hydraulic conductivity,53,61 and solute permeability52,62–66 to albumin in single capillaries/post-capillary venules results in a very rapid and transient permeability increase that resolves within 2–3 min. This is then followed by a longer and more sustained increase that occurs at some point after 1 h and lasts for up to a few days.27,53,54,67 In contrast, application of VEGF and measurement of solute flux by Evans blue or labelled albumin extravasation results in a slow accumulation over the first hour, similar to that seen in vitro.68,69 There is thus a biphasic response to VEGF—an initial transient increase lasting just a few minutes, and a sustained increase that lasts many hours. The problem is deciphering the contribution of the vasodilatory effects of VEGF towards this sustained effect (the acute effect is measured in vessels where flow and driving forces are controlled, and there are very few studies measuring the chronic response in the same way). The following is therefore an account of the signalling pathways where acute and chronic response, and in vitro vs. in vivo data are compared.
3.2. Signalling pathways
3.2.1. VEGFR activation
VEGF-A has been shown to bind to VEGFR1 and VEGFR2, and VEGF-C binds to VEGFR2 and VEGFR3. The splice variants of VEGF-A that are pro-angiogenic (e.g. VEGF165) act to increase Lp in vivo (acutely),70 Lp in vitro,71 and albumin extravasation through VEGFR2 activation. PlGF, which only binds VEGFR1 appears not to increase Lp acutely.61 VEGF-C increases Lp acutely in vivo by acting on VEGFR2.61 It therefore appears that VEGFR2 is the principal signalling pathway for VEGF-A- and VEGF-C-mediated increased permeability. However, the anti-angiogenic isoforms of VEGF, such as VEGF165b, can also increase Lp acutely and appear to do so through the activation of VEGFR1, not VEGFR2.27 In endothelial cells in culture and in vivo, VEGFR2 is phosphorylated inside 2 min after the addition of VEGF-A,72,73 and this phosphorylation is required for the acute and chronic phases of the increase in permeability.70 VEGFR2 phosphorylation results in initiation of a series of signalling pathways including increased intracellular calcium,74,75 src activation,72,76 and stimulation of the p42/p4MAPK pathway77 and the PI3 kinase pathway.78
3.2.2. Increased intracellular Ca2+
A series of detailed experiments examining how calcium was involved in the VEGF response have indicated that VEGFR2 activation by VEGF-A stimulates phospholipase C activation and production of DAG and IP3.79 However, it appears to be the DAG production that is responsible for the acutely increased calcium and Lp, and this acts independently of calcium store release,80 but through activation of the store-independent TRPC3/6 channels.81 This has now been shown to be the case in vitro for human microvascular endothelial cells (HMVEC),82 a microvascular endothelial cell type, but the calcium response is much slower than in vivo, and there is evidence that in HUVECs, the response to VEGF is dependent on calcium store-mediated TRPC1 channels,83 indicating that there is a significant difference between endothelial cell types. It has now been shown that in HMVECs inhibition of TRPC6 by a dominant negative over-expression inhibits the calcium response, but also endothelial cell migration and tube formation induced by VEGF.84,85
3.2.3. Src activation
VEGF also activates src kinase in endothelial cells in culture,72 and inhibition of src kinase inhibits Evans blue extravasation induced by VEGF,76 suggesting that src may also be required for the increase in permeability. However, there is no clear separation yet between src-dependent VEGF-mediated extravasation and VEGF-mediated permeability and this remains to be seen.
3.2.4. Subcellular localization
VEGFR can be localized to caveolae in endothelial cells, and this appears to form part of a signalling complex, or signalplex, that regulates the downstream signalling. There is a close association between the structural protein caveolin and the C-terminal of VEGFR2,86 including PLCγ87 and hence DAG, eNOS,88 and the TRPC6,89 and downstream signalling pathways such as protein kinase Cα, Raf-1, MAPK kinase 1/2, and ERK2/1.90 Moreover, it has recently been shown that the lipid raft associated proteins such as the store-operated calcium channel Orai, and the scaffolding protein Stim can also interact with receptor-operated calcium channels such as TRPC6 to couple both receptor-operated and store-operated calcium entry in microdomains within the cell,91 thus providing a molecular mechanism through which VEGF signalling could depend upon the components of the signalplex for its mechanisms of cation entry. Thus if VEGFRs are activated outside the caveolae, then the associated TRPC6/Orai activation would lead to a Stim-dependent recruitment to the lipid raft/caveolar domain to initiate a signalling pathway that may be different from that when TRPC6 is dissociated from the caveolae. The concept that a co-ordinated regulation of caveolar signalling is central to the mechanisms and subsequent downstream signalling regulating permeability is becoming clearer, but their link to increased vascular permeability has still not shown. The rapidity of the activation of increased permeability in vivo, particularly compared with in vitro signalling, suggests that the components involved must be very closely associated, and it is perhaps no coincidence that the density of caveolae in microvessels in vivo is substantially higher than in cultured endothelial cells.
3.3. Ultrastructural changes
VEGF activation of endothelial cells in vivo and in vitro results in marked ultrastructural changes that follow the appropriate time course for the permeability responses.
3.3.1. Vesicular vacuolar organelles to gaps
One of the first ultrastructural changes to be described for VEGF was the formation of clusters of linked vesicles through endothelial cells thought to link the luminal and abluminal surfaces.92 These vesicular vacuolar organelles (VVOs) occur very rapidly after activation with VEGF (within a few seconds) in vivo.93 The VVO formation is seen by electron microscopy and has been shown to consist of fenestrated linked caveolar vesicles. Perfusion of electron dense molecules (e.g. ferritin) has shown that VVOs can contain macromolecules, and thus they are thought to form pathways for fluid and solute movement across the vessel wall during VEGF-mediated permeability increase.94 Perfusion of single vessels in frogs and rats with VEGF has also shown the presence of transcellular gaps running close to but not at the endothelial cell junction, as well as intercellular gaps at the cell junction themselves.95 It is not known whether these processes are part of the same mechanism and that VVOs are pre-cursors of transcellular gaps, or whether the processes are entirely separate,96 but what is clear is that large holes can appear in endothelial cell barrier in response to VEGF and that this can occur within a few seconds after administration of VEGF.
3.3.2. Junctional changes
As discussed above, addition of VEGF in endothelial cells in vitro results in differing responses from endothelial cells in vitro, and this also applies to the effect on endothelial junctions. In vitro within 60 min a reduction in staining of junctional proteins such as ZO1,97 occludin,47 VE-cadherin47,98 at the endothelial junctions, coincident with the onset of increased vascular permeability, and prevention of endothelial junctional changes inhibit the VEGF permeability response. These changes are not apparent at 5 min after the activation of VEGF,97 but VE-cadherin is phosphorylated at 5 min after the addition of VEGF to endothelial cells in culture98 (earlier time points have not been investigated). However, in vivo changes in immunofluorescence staining of junctional proteins have been less well described, making it difficult to associate the time-dependent changes in vivo with those in vitro. Ultrastructural studies show that there is a loss of junctional integrity with VEGF activation very rapidly, and there is loss of tight and adherens junctions,95 widening of the cleft, and in many cases micron-sized gaps and VVOs through endothelial cells,99 and mathematical modelling of the VEGF response predicts an opening of the tight junctional strands.52
3.3.3. Fenestrae
VEGF in vivo and in vitro induces the formation of fenestrations,100 again many minutes after the initial transient increase in permeability, but consistent with the development of a chronic increase. This is also seen in endothelial cells in culture, where fenestrations have been described in response to VEGF treatment over 1–24 h.101,102
3.4. The link from the signalplex to the structural changes
3.4.1. eNOS
One of the earliest demonstrated downstream signal targets of VEGF activation was endothelial nitric oxide synthase.28,103 eNOS has been shown to be required for VEGF-mediated increased solute permeability.63 In isolated perfused rat coronary venules, eNOS inhibition resulted in a significant decrease in the transient increase in solute permeability to albumin induced by VEGF, confirming its role as a downstream target involved in the permeability pathways. Subsequent work has identified soluble guanylyl cyclase as the NO-activated target involved in this transient increase in solute permeability63 and extravasation of dye.104 The sGC activation results in the conversion of GTP to cGMP, which activates protein kinase G (PKG) which also appears to be required for the permeability increase.63 The downstream targets for protein kinase G (PKG) have not yet been identified.
3.4.2. Rho/Rac/Cdc42
Members of the Ras superfamily of small GTPases have been implicated in the regulation of permeability by many agents. These are prime candidates for the connection between VEGFR signalling and the ultrastructural changes that occur in response to VEGF. VEGFR, as part of its caveolin complex is associated with ARF6, which also regulates Rac1 activity in membrane ruffling and actin cytoskeleton dynamics.105 The Rho kinase, ROCK is also activated by VEGF, and appears to be required for the transient solute permeability response.106 Activation of ROCK results in phosphorylation of RhoGTPases including Rho, Rac, and Cdc42. These have been clearly identified as regulators of cytoskeletal element within the cell, and classically Rac is required for lamellipodia protrusion, Rho promoting assembly of actin stress fibres, and Cdc42 contributing to filopodia and membrane ruffles. In endothelial cells in culture, the different members of the family have different functions, with Rho resulting in stress fibre formation, Rac and CDC42 forming actin bundles and lamellipodia.107 It is not yet clear how any of these processes may be involved in the regulation of permeability, but it has been suggested from in vitro endothelial experiments that the polymerization of actin can result in cell retraction which could lead to an increase in tension on the intercellular junctions,108 and hence a force for disassociation of the adherens junctions as described below or for generation of actin-dependent contraction of areas of endothelial cells to form transcellular gaps. Rac in particular appears to be linked to VEGF-induced fenestration formation.109 While these associations have been made there is as yet no clear evidence for how cell cytoskeletal changes are linked to barrier changes in endothelial cells in vivo, or how these link to VEGF.
3.4.3. VE-cadherin
VEGF activation of endothelial cells results in phosphorylation and disassembly of VE-cadherin, one of the principal signalling and structural proteins associated with the adherens junction that forms part of the intercellular cleft.110 VE-cadherin phosphorylation is initiated within 5 min, but peaks at 30 min after activation by VEGF in endothelial cells in culture. It is thus able to be responsible at least in part for the chronic increase in permeability, but is too slow to account for the acute increase seen in response to VEGF. The contribution of VE-cadherin to vascular permeability in vivo is not as clearly established as in the in vitro models. There is considerable evidence that the adherens junction itself is regulated by VEGF during alterations in vascular permeability,111 but whether it structurally forms a barrier to fluid or protein flux, is a component of the extracellular matrix, or whether it is primarily a signalling function is still not clearly demonstrated in vivo. For instance, it has recently been shown that the tight junction can be regulated by VE-cadherin signalling.112 Additional data show that VEGF mediates a dephosphorylation of VE-cadherin, which disassociates from src and Csk a negative regulator of src, thus enabling src to be activated. This would fit with a dual mechanism of VEGF-induced permeability—a transient initial calcium dependence, followed by the activation of src, FAK, and VE-cadherin, followed by a cadherin-dependent signalling pathway through the tight junction that involves src activation for the chronic effect.113
3.4.4. Zona occludens-1 and occludin
The tight junction barrier has been closely linked with contributing to maintenance of permeability through a number of studies linking tight junctional barrier presence to baseline permeability in different organs.114 However, recent work indicates that the role of the tight junction may be to provide a narrowing of the fluid exit pathway, regulating junctional fluid velocity, and hence providing a restriction to both protein and fluid flux by maintaining an oncotic reflection coefficient as well as its role as a regulator of fluid and solute flux.115 There is good evidence that in vitro VEGF activation stimulates phosphorylation of the tight junctional regulator Zona occludens-1 (ZO-1),97 and it has been suggested that this mediates the VEGF-mediated permeability increase in vitro.50 Again, however, the phosphorylation of the ZO-1 takes 15–30 min in vitro, too long to account for the acute increase in permeability. There are no data on the time course of VEGF-mediated phosphorylation of ZO-1 in vivo.
3.4.5. PV1
VEGF induces fenestration in endothelial cells in vitro within ∼30 min of activation,101 and in fenestrated tissues, the inhibition of VEGF165-mediated activation of VEGFR2 either by overexpression of the anti-angiogenic isoform VEGF165b116 or by administration of VEGFR tyrosine kinase inhibitors117 or VEGF blocking antibodies118 results in a reduction in the fenestral density and reduction in the hydraulic conductivity and dye extravasation. Fenestrae in many vascular beds are spanned by a diaphragm formed from the protein PV1.119 PV1 has been shown to be both induced and repressed by VEGF, indicating that this may also contribute to the chronic increase in permeability brought about by VEGF. Again this is too slow to account for the acute increase, but may be responsible for the high hydraulic conductivity maintained in many fenestrated vascular beds in which VEGF is constitutively produced (e.g. salivary gland, adrenal gland, ovary, pituitary, etc.).
There is therefore a dichotomy between in vivo and in vitro experiments, and a biphasic response to VEGF. However, VEGF expression can occur either as a sudden onset of VEGF or as a gradual response as the VEGF concentration increases or decreases in response to physiological or pathophysiological stimuli. Interestingly, there is yet to be a clear and concise assessment of how such effects of VEGF on permeability, investigated through multiple arbitrary systems—from bolus administration of VEGF to isolated microvessels in vivo, injection into skin, or application to endothelial cells in culture—apply to the VEGF seen by blood vessels during pathological and physiological states.
4. Consequences of the effects of VEGF on permeability
4.1. Physiological effects
4.1.1. Reproduction
VEGF is highly expressed during the menstrual cycle in a manner that facilitates follicle maturation from primary to secondary antral follicles and during corpus luteal development following ovulation.120 Moreover, the growing endometrium induces a strong VEGF driven vascularization in readiness for implantation of the fertilized embryo. As the mammary glands remodel the mammary alveolar epithelium, massive angiogenesis occurs, which provides sufficient vasculature to generate milk.121 The permeability of the capillaries is extremely variable. Endometrial and corpus luteal vessels are relatively tight with permeabilities approaching normal continuous vessels, ovarian theca interna vessels are highly fenestrated and are thought to contribute to follicular fluid formation. The mammary gland vasculature is variable with alveolar epithelium fenestrated, but ductal epithelium tight, despite both vascular beds seeing continuous high concentrations of VEGF.122
4.1.2. Wound healing
VEGF is also highly expressed during wound healing and the permeability of vessels growing into the wound is raised compared with normal, is fenestrated, and contains large transcellular gaps,123 but recent studies on patients undergoing treatment with anti-VEGF antibodies do not report wound healing side effects.124
4.1.3. Glomerular function
In the glomerulus on the other hand, there is a high vascular permeability, in particular the hydraulic conductivity of the endothelium, in response to substantial VEGF secretion and production by the peri-endothelial podocytes. VEGF inhibition can lead to breakdown of glomerular function, and this may be due to the effects of VEGF on endothelial fenestrations combined with its survival effects on podocytes themselves.125 A similar story can be painted for other tissues with high-VEGF expression including salivary gland adrenal cortex and pituitary gland—high secretion rates but no angiogenesis. It therefore appears that in the physiological system the two pathways are kept separate.
4.2. In disease
In contrast to VEGF-driven physiological angiogenesis where excess fluid formation is rarely seen or VEGF-induced physiologically increased permeability where angiogenesis is rarely seen, in disease states VEGF overexpression often leads to excess of both actions.
4.2.1. Cancer: ascites, cerebral oedema, and so on
VEGF expression driven by hypoxia is considered to be a principal inducer of increased vascular supply to tumours. VEGF expression in tumours is as high or higher than seen in most normal states where VEGF expression is substantial (e.g. renal glomerulus or corpus luteum). The VEGF produced drives not only angiogenesis but also increased vascular permeability and resulting oedema. Inhibition of VEGF in brain tumours,126 ovarian carcinoma,127 as well as in benign conditions such as vestibular Schwannomas, reduces the fluid efflux around the tumours, reducing morbidity, and in the case of hearing loss associated with vestibular Schwannomas, restoring normal function.128 In fact the contribution of reduced vascular permeability to the effect of anti-VEGF agents has not yet been clearly discriminated from their anti-angiogenic actions, and as will be seen below may actually be a more important effect.
4.2.2. Blindness: diabetic macular edema (DME), wet age-related macular degeneration
VEGF is also over-expressed in two key causes of blindness in the western world, neovascular (or wet) age-related macular degeneration (wAMD) and diabetic retinopathy. These two conditions have very different fundamental causes. wAMD results from a build-up of lipid deposits in the retinal pigmented epithelial cells of the retina, and progressive breakdown of the underlying Bruch's membrane. Increased VEGF expression results in a neovascularization from the underlying choroidal vasculature into the retina.129 Whereas retinal blood vessels are part of the blood brain barrier and have extremely low hydraulic conductivity,130 the choroidal vasculature has a very high permeability partly due to the presence of fenestrations in the endothelial cells130 (which may be maintained by constitutive VEGF expression from the basolateral part of the retinal pigmented epithelial cells). When these choroidal vessels invade into the retina, the increased vascular permeability results in sub-retinal oedema, which results in a rapid loss of sight (over a few weeks to months). Intraocular injection with either bevacizumab or the variable fragment of a similar VEGF antibody, termed ranibizumab, can initially reverse the vision loss and then maintain vision.131 This is associated with a resolution of the sub-retinal oedema, indicating that it is the anti-permeability properties of VEGF therapy that is effective at least initially in this disease.
The second leading cause of blindness in the developed world is diabetic retinopathy. This has quite a different aetiology from AMD but is also VEGF dependent. The endothelial dysfunction associated with diabetes occurs systemically, resulting in loss of endothelial cells from the retina and localized areas of ischaemia.132 This results in hypoxic upregulation of VEGF, which acts on the vasculature that is still perfused in the periphery of the ischaemic area to produce a proliferation and increased leakage of vessels resulting in haemorrhage, oedema, and neovascularization intraretinally causing disrupted vision.133 Anti-VEGF therapies are being tried in diabetic retinopathy, and particularly in the form of retinopathy that results in demonstrable fluid formation in the retina—diabetic macular oedema and phase II trials have been promising for ranibizumab. Proliferative diabetic retinopathy is a more complicated initial target because VEGF inhibition results in endothelial cell regression and vascular loss in animal models, which is a potential hazard for diabetic patients where endothelial loss is an underlying cause of the disease.
4.2.3. Other conditions
VEGF-mediated permeability has also been implicated in renal failure, arthritis, psoriasis, and coronary disease, but their consideration is beyond the scope of this review.
5. Conclusion
5.1. Importance of VEGF antagonists in clinical situations
The increasingly widespread use of VEGF antagonists in clinical conditions, in particular, in cancer and eye disease, has focused attention on how these antagonists exert their effects. It has been presumed that as VEGF is a potent angiogenic agent, the effects are mediated through this mechanism. However, it is increasingly becoming the case that anti-VEGF agents are acting on the symptoms of the disease by blocking the VEGF-mediated increase in permeability rather than any direct effect on angiogenesis. In AMD, DME, gliomas, ovarian carcinoma, and lung cancer, this is probably the principal mechanism of action, and it is still unknown even in the most widely known cancer—colorectal cancer—how much is due to anti-angiogenesis and how much is due to increased permeability. The recent interest in mechanisms of escape of tumours from ‘anti-angiogenic’ therapy are built on the premise that the inhibition of tumour growth was due to anti-angiogenesis, whereas if it was due initially to reduced vascular permeability, then the effect is not so much ‘escape from anti-angiogenic therapy’ but unaffected angiogenesis now overcoming the effects of reduced permeability.
5.2. Synthesis of current knowledge to summarize best case
VEGF-mediated permeability experimentally appears to occur in a biphasic manner both in vitro and in vivo, although these two time courses do not compare. The molecular mechanisms underlying this increase in permeability are still not clear, not least due to the difficulty in reconciling different methodologies of permeability measurement, with the respective changes in molecular interactions. We still do not know if src activation, for instance, in vivo occurs within a time frame of the acute increase in permeability or is only required for the chronic response. We do not know whether the ultrastructural features seen initially in vivo (VVOs, gaps) are consistent with altered junctional properties measured in the long term. It therefore appears to be critical for the effect of VEGF on permeability to be examined with care to the timing of the response when investigating the molecular mechanisms, and not to over-interpret in vitro results to the in vivo situation. Equally there is a danger in assuming that abrupt VEGF application to a tissue represents a physiological or even pathological state and that VEGF expression in vivo occurs in a more diffuse and gradual time scale, which needs to be reproduced experimentally to investigate the mechanisms underlying the permeability changes that are clearly important clinically.
5.3. Future directions
The synthesis of existing molecular changes is becoming more and more difficult to reconcile with the generation of results that are not comparable across systems. Endothelial cells from different vascular beds are not the same, and cells in identical vascular beds can respond differently according to their environment—oxygen tension, shear stress, circulating leucocyte interactions, etc. Finally, the transport of molecules across the endothelial wall is dependent on multiple factors in addition to the barrier properties of that wall. It will therefore be critical in the future to be able to build a molecular picture of VEGF-mediated permeability that is specific for vascular beds, that is dependent on the application process (i.e. how quickly VEGF levels rise), and that actually reflects changes in the barrier function of the endothelium, the VEGF type, the vascular wall history, and the response time. Until that is clearly laid out for each new finding, building up a picture of how VEGF increases permeability will still be an inexact science. Moreover, while there have been numerous qualitative descriptions of the relative signalling pathways to the VEGF-mediated increase in permeability, there is still very little known about the quantitative contribution of these signalling pathways, for instance, are src and Ca2+ responses additive or synergistic? Perhaps the key area required for investigation is the dissection of the signalplex involving VEGF receptors, ion channels, and scaffolding proteins that regulate the signalling pathways downstream, for while this is being resolved for angiogenesis, it is some way off for permeability.
Conflict of interest: none declared.
Funding
This was supported by the British Heart Foundation (FS06/003). Funding to pay the open access publication charge was provided by the British Heart Foundation.
References
- 1.Senger DR, Galli SJ, Dvorak AM, Perruzzi CA, Harvey VS, Dvorak HF. Tumour cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science. 1983;219:983–985. doi: 10.1126/science.6823562. doi:10.1126/science.6823562. [DOI] [PubMed] [Google Scholar]
- 2.Senger DR, Perruzzi CA, Feder J, Dvorak HF. A highly conserved vascular permeability factor secreted by a variety of human and rodent tumor cell lines. Cancer Res. 1986;46:5629–5632. [PubMed] [Google Scholar]
- 3.Keck PJ, Hauser SD, Krivi G, Sanzo K, Warren T, Feder J, et al. Vascular permeability factor, an endothelial cell mitogen related to PDGF. Science. 1989;246:1309–1312. doi: 10.1126/science.2479987. doi:10.1126/science.2479987. [DOI] [PubMed] [Google Scholar]
- 4.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285:1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 5.Plouet J, Schilling J, Gospodarowicz D. Isolation and characterization of a newly identified endothelial cell mitogen produced by AtT-20 cells. EMBO J. 1989;8:3801–3806. doi: 10.1002/j.1460-2075.1989.tb08557.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ferrara N, Henzel WJ. Pituitary follicular cells secrete a novel heparin-binding growth factor specific for vascular endothelial cells. Biochem Biophys Res Commun. 1989;161:851–858. doi: 10.1016/0006-291x(89)92678-8. doi:10.1016/0006-291X(89)92678-8. [DOI] [PubMed] [Google Scholar]
- 7.Leung DW, Cachianes G, Kuang WJ, Goeddel DV, Ferrara N. Vascular endothelial growth factor is a secreted angiogenic mitogen. Science. 1989;246:1306–1309. doi: 10.1126/science.2479986. doi:10.1126/science.2479986. [DOI] [PubMed] [Google Scholar]
- 8.Foster RR, Hole R, Anderson K, Satchell SC, Coward RJ, Mathieson PW, et al. Functional evidence that vascular endothelial growth factor may act as an autocrine factor on human podocytes. Am J Physiol Renal Physiol. 2003;284:F1263–F1273. doi: 10.1152/ajprenal.00276.2002. [DOI] [PubMed] [Google Scholar]
- 9.Matsuzaki H, Tamatani M, Yamaguchi A, Namikawa K, Kiyama H, Vitek MP, et al. Vascular endothelial growth factor rescues hippocampal neurons from glutamate-induced toxicity: signal transduction cascades. FASEB J. 2001;15:1218–1220. [PubMed] [Google Scholar]
- 10.Bachelder RE, Crago A, Chung J, Wendt MA, Shaw LM, Robinson G, et al. Vascular endothelial growth factor is an autocrine survival factor for neuropilin-expressing breast carcinoma cells. Cancer Res. 2001;61:5736–5740. [PubMed] [Google Scholar]
- 11.Bates DO, Cui TG, Doughty JM, Winkler M, Sugiono M, Shields JD, et al. VEGF165b an inhibitory splice variant of vascular endothelial growth factor, is down-regulated in renal cell carcinoma. Cancer Res. 2002;62:4123–4131. [PubMed] [Google Scholar]
- 12.Olofsson B, Pajusola K, Kaipainen A, Von Euler G, Joukov V, Saksela O, et al. Vascular endothelial growth factor B, a novel growth factor for endothelial cells. Proc Natl Acad Sci USA. 1996;93:2576–2581. doi: 10.1073/pnas.93.6.2576. doi:10.1073/pnas.93.6.2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Joukov V, Pajusola K, Kaipainen A, Chilov D, Lahtinen I, Kukk E, et al. A novel vascular endothelial growth factor, VEGF-C, is a ligand for the Flt4 (VEGFR-3) and KDR (VEGFR-2) receptor tyrosine kinases. EMBO J. 1996;15:290–298. [PMC free article] [PubMed] [Google Scholar]
- 14.Achen MG, Jeltsch M, Kukk E, Makinen T, Vitali A, Wilks AF, et al. Vascular endothelial growth factor D (VEGF-D) is a ligand for the tyrosine kinases VEGF receptor 2 (Flk1) and VEGF receptor 3 (Flt4) Proc Natl Acad Sci USA. 1998;95:548–553. doi: 10.1073/pnas.95.2.548. doi:10.1073/pnas.95.2.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maglione D, Guerriero V, Viglietto G, Delli-Bovi P, Persico MG. Isolation of a human placenta cDNA coding for a protein related to the vascular permeability factor. Proc Natl Acad Sci USA. 1991;88:9267–9271. doi: 10.1073/pnas.88.20.9267. doi:10.1073/pnas.88.20.9267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muller YA, Li B, Christinger HW, Wells JA, Cunningham BC, de Vos AM. Vascular endothelial growth factor: crystal structure and functional mapping of the kinase domain receptor binding site. Proc Natl Acad Sci USA. 1997;94:7192–7197. doi: 10.1073/pnas.94.14.7192. doi:10.1073/pnas.94.14.7192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature. 1992;359:843–845. doi: 10.1038/359843a0. doi:10.1038/359843a0. [DOI] [PubMed] [Google Scholar]
- 18.Williams B. Factors regulating the expression of vascular permeability/vascular endothelial growth factor by human vascular tissues. Diabetologia. 1997;40:S118–S120. doi: 10.1007/s001250051423. doi:10.1007/s001250051423. [DOI] [PubMed] [Google Scholar]
- 19.Lee S, Chen TT, Barber CL, Jordan MC, Murdock J, Desai S, et al. Autocrine VEGF signaling is required for vascular homeostasis. Cell. 2007;130:691–703. doi: 10.1016/j.cell.2007.06.054. doi:10.1016/j.cell.2007.06.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Plate KH, Breier G, Weich HA, Risau W. Vascular endothelial growth factor is a potential tumour angiogenesis factor in human gliomas in vivo. Nature. 1992;359:845–848. doi: 10.1038/359845a0. doi:10.1038/359845a0. [DOI] [PubMed] [Google Scholar]
- 21.Couffinhal T, Kearney M, Witzenbichler B, Chen D, Murohara T, Losordo DW, et al. Vascular endothelial growth factor/vascular permeability factor (VEGF/VPF) in normal and atherosclerotic human arteries. Am J Pathol. 1997;150:1673–1685. [PMC free article] [PubMed] [Google Scholar]
- 22.Kamat BR, Brown LF, Manseau EJ, Senger DR, Dvorak HF. Expression of vascular permeability factor/vascular endothelial growth factor by human granulosa and theca lutein cells. Role in corpus luteum development. Am J Pathol. 1995;146:157–165. [PMC free article] [PubMed] [Google Scholar]
- 23.de Vries C, Escobedo JA, Ueno H, Houck K, Ferrara N, Williams LT. The fms-like tyrosine kinase, a receptor for vascular endothelial growth factor. Science. 1992;255:989–991. doi: 10.1126/science.1312256. doi:10.1126/science.1312256. [DOI] [PubMed] [Google Scholar]
- 24.Quinn TP, Peters KG, De Vries C, Ferrara N, Williams LT. Fetal liver kinase 1 is a receptor for vascular endothelial growth factor and is selectively expressed in vascular endothelium. Proc Natl Acad Sci USA. 1993;90:7533–7537. doi: 10.1073/pnas.90.16.7533. doi:10.1073/pnas.90.16.7533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pajusola K, Aprelikova O, Korhonen J, Kaipainen A, Pertovaara L, Alitalo R, et al. FLT4 receptor tyrosine kinase contains seven immunoglobulin-like loops and is expressed in multiple human tissues and cell lines. Cancer Res. 1992;52:5738–5743. [PubMed] [Google Scholar]
- 26.Olsson AK, Dimberg A, Kreuger J, Claesson-Welsh L. VEGF receptor signalling—in control of vascular function. Nat Rev Mol Cell Biol. 2006;7:359–371. doi: 10.1038/nrm1911. doi:10.1038/nrm1911. [DOI] [PubMed] [Google Scholar]
- 27.Glass CA, Harper SJ, Bates DO. The anti-angiogenic VEGF isoform VEGF165b transiently increases hydraulic conductivity, probably through VEGF receptor 1 in vivo. J Physiol (Lond) 2006;572:243–257. doi: 10.1113/jphysiol.2005.103127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ku DD, Zaleski JK, Liu S, Brock TA. Vascular endothelial growth factor induces EDRF-dependent relaxation in coronary arteries. Am J Physiol. 1993;265:H586–H592. doi: 10.1152/ajpheart.1993.265.2.H586. [DOI] [PubMed] [Google Scholar]
- 29.Ferrara N, Davis-Smyth T. The biology of vascular endothelial growth factor. Endocr Rev. 1997;18:4–25. doi: 10.1210/edrv.18.1.0287. doi:10.1210/er.18.1.4. [DOI] [PubMed] [Google Scholar]
- 30.Greenberg JI, Shields DJ, Barillas SG, Acevedo LM, Murphy E, Huang J, et al. A role for VEGF as a negative regulator of pericyte function and vessel maturation. Nature. 2008;456:809–813. doi: 10.1038/nature07424. doi:10.1038/nature07424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Unemori EN, Ferrara N, Bauer EA, Amento EP. Vascular endothelial growth factor induced interstitial collagenase expression in human endothelial cells. J Cell Physiol. 1992;153:557–562. doi: 10.1002/jcp.1041530317. doi:10.1002/jcp.1041530317. [DOI] [PubMed] [Google Scholar]
- 32.Yang R, Thomas GR, Bunting S, Ko A, Ferrara N, Keyt B, et al. Effects of vascular endothelial growth factor on hemodynamics and cardiac performance. J Cardiovasc Pharmacol. 1996;27:838–844. doi: 10.1097/00005344-199606000-00011. doi:10.1097/00005344-199606000-00011. [DOI] [PubMed] [Google Scholar]
- 33.Vajanto I, Rissanen TT, Rutanen J, Hiltunen MO, Tuomisto TT, Arve K, et al. Evaluation of angiogenesis and side effects in ischemic rabbit hindlimbs after intramuscular injection of adenoviral vectors encoding VEGF and LacZ. J Gene Med. 2002;4:371–380. doi: 10.1002/jgm.287. doi:10.1002/jgm.287. [DOI] [PubMed] [Google Scholar]
- 34.Wang WY, Whittles CE, Harper SJ, Bates DO. An adenovirus-mediated gene-transfer model of angiogenesis in rat mesentery. Microcirculation. 2004;11:361–375. doi: 10.1080/10739680490437568. doi:10.1080/10739680490437568. [DOI] [PubMed] [Google Scholar]
- 35.Curry FE, Michel CC. A fiber matrix model of capillary permeability. Microvasc Res. 1980;20:96–99. doi: 10.1016/0026-2862(80)90024-2. doi:10.1016/0026-2862(80)90024-2. [DOI] [PubMed] [Google Scholar]
- 36.Curry FE. Antipyrine and aminopyrine permeability of individually perfused frog capillaries. Am J Physiol. 1981;240:H597–H605. doi: 10.1152/ajpheart.1981.240.4.H597. [DOI] [PubMed] [Google Scholar]
- 37.Levick JR, Smaje LH. An analysis of the permeability of a fenestra. Microvasc Res. 1987;33:233–256. doi: 10.1016/0026-2862(87)90020-3. doi:10.1016/0026-2862(87)90020-3. [DOI] [PubMed] [Google Scholar]
- 38.Turner MR. Flows of liquid and electrical current through monolayers of cultured bovine arterial endothelium. J Physiol (Lond) 1992;449:1–20. doi: 10.1113/jphysiol.1992.sp019071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Curry FE. Mechanics and thermodynamics of transcapillary exchange. In: Michel CC, Renkin EM, editors. Handbook of Physiology The Cardiovascular System Microcirculation. 2nd ed. Bethesda: American Physiological Society; 1984. pp. 309–373. [Google Scholar]
- 40.Huxley VH, Curry FE, Adamson RH. Quantitative fluorescence microscopy on single capillaries: alpha-lactalbumin transport. Am J Physiol. 1987;252:H188–H197. doi: 10.1152/ajpheart.1987.252.1.H188. [DOI] [PubMed] [Google Scholar]
- 41.Renkin EM, Tucker VL. Measurement of microvascular transport parameters of macromolecules in tissues and organs of intact animals. Microcirculation. 1998;5:139–152. [PubMed] [Google Scholar]
- 42.Pappenheimer JR, Soto-Rivera A. Effective osmotic pressure of the plasma proteins and other quantities associated with the capillary circulation in the hindlimbs of cats and dogs. Am J Physiol. 1948;152:471–491. doi: 10.1152/ajplegacy.1948.152.3.471. [DOI] [PubMed] [Google Scholar]
- 43.DeMaio L, Antonetti DA, Scaduto RC, Jr, Gardner TW, Tarbell JM. VEGF increases paracellular transport without altering the solvent-drag reflection coefficient. Microvasc Res. 2004;68:295–302. doi: 10.1016/j.mvr.2004.06.007. doi:10.1016/j.mvr.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 44.Chang YS, Munn LL, Hillsley MV, Dull RO, Yuan J, Lakshminarayanan S, et al. Effect of vascular endothelial growth factor on cultured endothelial cell monolayer transport properties. Microvasc Res. 2000;59:265–277. doi: 10.1006/mvre.1999.2225. doi:10.1006/mvre.1999.2225. [DOI] [PubMed] [Google Scholar]
- 45.Satchell SC, Anderson KL, Mathieson PW. Angiopoietin 1 and vascular endothelial growth factor modulate human glomerular endothelial cell barrier properties. J Am Soc Nephrol. 2004;15:566–574. doi: 10.1097/01.asn.0000115397.22519.03. doi:10.1097/01.ASN.0000115397.22519.03. [DOI] [PubMed] [Google Scholar]
- 46.Behzadian MA, Windsor LJ, Ghaly N, Liou G, Tsai NT, Caldwell RB. VEGF-induced paracellular permeability in cultured endothelial cells involves urokinase and its receptor. FASEB J. 2003;17:752–754. doi: 10.1096/fj.02-0484fje. [DOI] [PubMed] [Google Scholar]
- 47.Kevil CG, Payne DK, Mire E, Alexander JS. Vascular permeability factor/vascular endothelial cell growth factor-mediated permeability occurs through disorganization of endothelial junctional proteins. J Biol Chem. 1998;273:15099–15103. doi: 10.1074/jbc.273.24.15099. doi:10.1074/jbc.273.24.15099. [DOI] [PubMed] [Google Scholar]
- 48.Clauss M, Sunderkotter C, Sveinbjornsson B, Hippenstiel S, Willuweit A, Marino M, et al. A permissive role for tumor necrosis factor in vascular endothelial growth factor-induced vascular permeability. Blood. 2001;97:1321–1329. doi: 10.1182/blood.v97.5.1321. doi:10.1182/blood.V97.5.1321. [DOI] [PubMed] [Google Scholar]
- 49.Hippenstiel S, Krull M, Ikemann A, Risau W, Clauss M, Suttorp N. VEGF induces hyperpermeability by a direct action on endothelial cells. Am J Physiol. 1998;274:L678–L684. doi: 10.1152/ajplung.1998.274.5.L678. [DOI] [PubMed] [Google Scholar]
- 50.Wang W, Merrill MJ, Borchardt RT. Vascular endothelial growth factor affects permeability of brain microvessel endothelial cells in vitro. Am J Physiol Cell Physiol. 1996;271:C1973–C1980. doi: 10.1152/ajpcell.1996.271.6.C1973. [DOI] [PubMed] [Google Scholar]
- 51.Albelda SM, Sampson PM, Haselton FR, McNiff JM, Mueller SN, Williams SK, et al. Permeability characteristics of cultured endothelial cell monolayers. J Appl Physiol. 1988;64:308–322. doi: 10.1152/jappl.1988.64.1.308. [DOI] [PubMed] [Google Scholar]
- 52.Fu BM, Shen S. Structural mechanisms of acute VEGF effect on microvessel permeability. Am J Physiol Heart Circ. 2003;284:H2124–H2135. doi: 10.1152/ajpheart.00894.2002. [DOI] [PubMed] [Google Scholar]
- 53.Bates DO, Curry FE. Vascular endothelial growth factor increases hydraulic conductivity of isolated perfused microvessels. Am J Physiol Heart Circ Physiol. 1996;271:H2520–H2528. doi: 10.1152/ajpheart.1996.271.6.H2520. [DOI] [PubMed] [Google Scholar]
- 54.Bates DO. The chronic effect of vascular endothelial growth factor on individually perfused frog mesenteric microvessels. J Physiol (Lond) 1998;513:225–233. doi: 10.1111/j.1469-7793.1998.225by.x. doi:10.1111/j.1469-7793.1998.225by.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Senger DR, Connolly DT, Van de Water L, Feder J, Dvorak HF. Purification and NH2-terminal amino acid sequence of guinea pig tumor-secreted vascular permeability factor. Cancer Res. 1990;50:1774–1778. [PubMed] [Google Scholar]
- 56.Levick JR, Michel CC. The effect of bovine albumin on the permeability of frog mesenteric capillaries. Q J Exp Physiol Cogn Med Sci. 1973;58:87–97. doi: 10.1113/expphysiol.1973.sp002194. [DOI] [PubMed] [Google Scholar]
- 57.Levick JR, Michel CC. The permeability of individually perfused frog mesenteric capillaries to T1824 and T1824-albumin as evidence for a large pore system. Q J Exp Physiol Cogn Med Sci. 1973;58:67–85. doi: 10.1113/expphysiol.1973.sp002192. [DOI] [PubMed] [Google Scholar]
- 58.Freedman FB, Johnson JA. Equilibrium and kinetic properties of the Evans blue-albumin system. Am J Physiol. 1969;216:675–681. doi: 10.1152/ajplegacy.1969.216.3.675. [DOI] [PubMed] [Google Scholar]
- 59.Renkin EM. Control of microcirculation blood-tissue exchange. In: Michel CC, Renkin EM, editors. Handbook of Physiology The Cardiovascular System Microcirculation. 2nd ed. Bethesda, MD: American Physiological Society; 1984. pp. 627–688. [Google Scholar]
- 60.Levick JR. An Introduction to Cardiovascular Physiology. London: Butterworths; 1991. [Google Scholar]
- 61.Hillman NJ, Whittles CE, Pocock TM, Williams B, Bates DO. Differential effects on Microvascular hydraulic conductivity (Lp) of vascular endothelial growth factor C (VEGF-C) and placental growth factor-1 (PlGF-1) J Vasc Res. 2001;38:176–185. doi: 10.1159/000051044. doi:10.1159/000051044. [DOI] [PubMed] [Google Scholar]
- 62.Fu BM, Shen S. Acute VEGF effect on solute permeability of mammalian microvessels in vivo. Microvasc Res. 2004;68:51–62. doi: 10.1016/j.mvr.2004.03.004. doi:10.1016/j.mvr.2004.03.004. [DOI] [PubMed] [Google Scholar]
- 63.Wu HM, Huang Q, Yuan Y, Granger HJ. VEGF induces NO-dependent hyperpermeability in coronary venules. Am J Physiol. 1996;271:H2735–H2739. doi: 10.1152/ajpheart.1996.271.6.H2735. [DOI] [PubMed] [Google Scholar]
- 64.Wu HM, Yuan Y, Zawieja DC, Tinsley J, Granger HJ. Role of phospholipase C, protein kinase C, and calcium in VEGF-induced venular hyperpermeability. Am J Physiol. 1999;276:H535–H542. doi: 10.1152/ajpheart.1999.276.2.H535. [DOI] [PubMed] [Google Scholar]
- 65.Wu LW, Mayo LD, Dunbar JD, Kessler KM, Baerwald MR, Jaffe EA, et al. Utilization of distinct signaling pathways by receptors for vascular endothelial cell growth factor and other mitogens in the induction of endothelial cell proliferation. J Biol Chem. 2000;275:5096–5103. doi: 10.1074/jbc.275.7.5096. doi:10.1074/jbc.275.7.5096. [DOI] [PubMed] [Google Scholar]
- 66.Wu LW, Mayo LD, Dunbar JD, Kessler KM, Ozes ON, Warren RS, et al. VRAP is an adaptor protein that binds KDR, a receptor for vascular endothelial cell growth factor. J Biol Chem. 2000;275:6059–6062. doi: 10.1074/jbc.275.9.6059. doi:10.1074/jbc.275.9.6059. [DOI] [PubMed] [Google Scholar]
- 67.Bates DO, Heald RI, Curry FE, Williams B. Vascular endothelial growth factor increases Rana vascular permeability and compliance by different signalling pathways. J Physiol (Lond) 2001;533:263–272. doi: 10.1111/j.1469-7793.2001.0263b.x. doi:10.1111/j.1469-7793.2001.0263b.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Murohara T, Horowitz JR, Silver M, Tsurumi Y, Chen D, Sullivan A, et al. Vascular endothelial growth factor/vascular permeability factor enhances vascular permeability via nitric oxide and prostacyclin. Circulation. 1998;97:99–107. doi: 10.1161/01.cir.97.1.99. [DOI] [PubMed] [Google Scholar]
- 69.Leenders W, Lubsen N, van Altena M, Clauss M, Deckers M, Lowik C, et al. Design of a variant of vascular endothelial growth factor-A (VEGF-A) antagonizing KDR/Flk-1 and Flt-1. Lab Invest. 2002;82:473–481. doi: 10.1038/labinvest.3780440. [DOI] [PubMed] [Google Scholar]
- 70.Whittles CE, Pocock TM, Wedge SR, Kendrew J, Hennequin LF, Harper SJ, et al. ZM323881 a novel inhibitor of vascular endothelial growth factor-receptor-2, tyrosine kinase activity. Microcirculation. 2002;9:513–522. doi: 10.1038/sj.mn.7800164. [DOI] [PubMed] [Google Scholar]
- 71.Castilla MA, Neria F, Renedo G, Pereira DS, Gonzalez-Pacheco FR, Jimenez S, et al. Tumor-induced endothelial cell activation: role of vascular endothelial growth factor. Am J Physiol Cell Physiol. 2004;286:C1170–C1176. doi: 10.1152/ajpcell.00306.2003. doi:10.1152/ajpcell.00306.2003. [DOI] [PubMed] [Google Scholar]
- 72.Waltenberger J, Claesson-Welsh L, Siegbahn A, Shibuya M, Heldin CH. Different signal transduction properties of KDR and Flt1, two receptors for vascular endothelial growth factor. J Biol Chem. 1994;269:26988–26995. [PubMed] [Google Scholar]
- 73.Cunningham SA, Arrate MP, Brock TA, Waxham MN. Interactions of FLT-1 and KDR with phospholipase C gamma: identification of the phosphotyrosine binding sites. Biochem Biophys Res Commun. 1997;240:635–639. doi: 10.1006/bbrc.1997.7719. doi:10.1006/bbrc.1997.7719. [DOI] [PubMed] [Google Scholar]
- 74.Criscuolo GR, Lelkes PI, Rotrosen D, Oldfield EH. Cytosolic calcium changes in endothelial cells induced by a protein product of human gliomas containing vascular permeability factor activity. J Neurosurg. 1989;71:884–891. doi: 10.3171/jns.1989.71.6.0884. doi:10.3171/jns.1989.71.6.0884. [DOI] [PubMed] [Google Scholar]
- 75.Bates DO, Curry FE. Vascular endothelial growth factor increases microvascular permeability via a Ca(2+)-dependent pathway. Am J Physiol. 1997;273:H687–H694. doi: 10.1152/ajpheart.1997.273.2.H687. [DOI] [PubMed] [Google Scholar]
- 76.Eliceiri BP, Paul R, Schwartzberg PL, Hood JD, Leng J, Cheresh DA. Selective requirement for Src kinases during VEGF-induced angiogenesis and vascular permeability. Mol Cell. 1999;4:915–924. doi: 10.1016/s1097-2765(00)80221-x. doi:10.1016/S1097-2765(00)80221-X. [DOI] [PubMed] [Google Scholar]
- 77.Wu MH, Yuan SY, Granger HJ. The protein kinase MEK1/2 mediate vascular endothelial growth factor- and histamine-induced hyperpermeability in porcine coronary venules. J Physiol (Lond) 2005;563:95–104. doi: 10.1113/jphysiol.2004.076075. doi:10.1113/jphysiol.2004.076075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Six I, Kureishi Y, Luo Z, Walsh K. Akt signaling mediates VEGF/VPF vascular permeability in vivo. FEBS Lett. 2002;532:67–69. doi: 10.1016/s0014-5793(02)03630-x. doi:10.1016/S0014-5793(02)03630-X. [DOI] [PubMed] [Google Scholar]
- 79.Pocock TM, Bates DO. In vivo mechanisms of vascular endothelial growth factor-mediated increased hydraulic conductivity of Rana capillaries. J Physiol (Lond) 2001;534:479–488. doi: 10.1111/j.1469-7793.2001.00479.x. doi:10.1111/j.1469-7793.2001.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Pocock TM, Williams B, Curry FE, Bates DO. VEGF and ATP act by different mechanisms to increase microvascular permeability and endothelial [Ca(2+)](i) Am J Physiol Heart Circ. 2000;279:H1625–H1634. doi: 10.1152/ajpheart.2000.279.4.H1625. [DOI] [PubMed] [Google Scholar]
- 81.Pocock TM, Foster RR, Bates DO. Evidence of a role for TRPC channels in VEGF-mediated increased vascular permeability in vivo. Am J Physiol Heart Circ. 2004;286:H1015–H1026. doi: 10.1152/ajpheart.00826.2003. doi:10.1152/ajpheart.00826.2003. [DOI] [PubMed] [Google Scholar]
- 82.Cheng HW, James AF, Foster RR, Hancox JC, Bates DO. VEGF activates receptor-operated cation channels in human microvascular endothelial cells. Arterioscler Thromb Vasc Biol. 2006;26:1768–1776. doi: 10.1161/01.ATV.0000231518.86795.0f. doi:10.1161/01.ATV.0000231518.86795.0f. [DOI] [PubMed] [Google Scholar]
- 83.Jho D, Mehta D, Ahmmed G, Gao XP, Tiruppathi C, Broman M, et al. Angiopoietin-1 opposes VEGF-induced increase in endothelial permeability by inhibiting TRPC1-dependent Ca2 influx. Circ Res. 2005;96:1282–1290. doi: 10.1161/01.RES.0000171894.03801.03. doi:10.1161/01.RES.0000171894.03801.03. [DOI] [PubMed] [Google Scholar]
- 84.Hamdollah Zadeh MA, Glass CA, Magnussen A, Hancox JC, Bates DO. VEGF-mediated elevated intracellular calcium and angiogenesis in human microvascular endothelial cells in vitro are inhibited by dominant negative TRPC6. Microcirculation. 2008;15:605–614. doi: 10.1080/10739680802220323. doi:10.1080/10739680802220323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ge R, Tai Y, Sun Y, Zhou K, Yang S, Cheng T, et al. Critical role of TRPC6 channels in VEGF-mediated angiogenesis. Cancer Lett. 2009;283:43–51. doi: 10.1016/j.canlet.2009.03.023. doi:10.1016/j.canlet.2009.03.023. [DOI] [PubMed] [Google Scholar]
- 86.Labrecque L, Royal I, Surprenant DS, Patterson C, Gingras D, Beliveau R. Regulation of vascular endothelial growth factor receptor-2 activity by caveolin-1 and plasma membrane cholesterol. Mol Biol Cell. 2003;14:334–347. doi: 10.1091/mbc.E02-07-0379. doi:10.1091/mbc.E02-07-0379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tahir SA, Park S, Thompson TC. Caveolin-1 regulates VEGF-stimulated angiogenic activities in prostate cancer and endothelial cells. Cancer Biol Ther. 2009;8:2286–2296. doi: 10.4161/cbt.8.23.10138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Shaul PW, Smart EJ, Robinson LJ, German Z, Yuhanna IS, Ying Y, et al. Acylation targets emdothelial nitric-oxide synthase to plasmalemmal caveolae. J Biol Chem. 1996;271:6518–6522. doi: 10.1074/jbc.271.11.6518. doi:10.1074/jbc.271.11.6518. [DOI] [PubMed] [Google Scholar]
- 89.Fleming I, Rueben A, Popp R, Fisslthaler B, Schrodt S, Sander A, et al. Epoxyeicosatrienoic acids regulate Trp channel dependent Ca2+ signaling and hyperpolarization in endothelial cells. Arterioscler Thromb Vasc Biol. 2007;27:2612–2618. doi: 10.1161/ATVBAHA.107.152074. doi:10.1161/ATVBAHA.107.152074. [DOI] [PubMed] [Google Scholar]
- 90.Liao WX, Feng L, Zhang H, Zheng J, Moore TR, Chen DB. Compartmentalizing VEGF-induced ERK2/1 signaling in placental artery endothelial cell caveolae: a paradoxical role of caveolin-1 in placental angiogenesis in vitro. Mol Endocrinol. 2009;23:1428–1444. doi: 10.1210/me.2008-0475. doi:10.1210/me.2008-0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liao Y, Plummer NW, George MD, Abramowitz J, Zhu MX, Birnbaumer L. A role for Orai in TRPC-mediated Ca2+ entry suggests that a TRPC:Orai complex may mediate store and receptor operated Ca2+ entry. Proc Natl Acad Sci USA. 2009;106:3202–3206. doi: 10.1073/pnas.0813346106. doi:10.1073/pnas.0813346106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Feng D, Nagy JA, Hipp J, Dvorak HF, Dvorak AM. Vesiculo-vacuolar organelles and the regulation of venule permeability to macromolecules by vascular permeability factor, histamine, and serotonin. J Exp Med. 1996;183:1981–1986. doi: 10.1084/jem.183.5.1981. doi:10.1084/jem.183.5.1981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Feng Y, Venema VJ, Venema RC, Tsai N, Behzadian MA, Caldwell RB. VEGF-induced permeability increase is mediated by caveolae. Invest Ophthalmol Vis Sci. 1999;40:157–167. [PubMed] [Google Scholar]
- 94.Nagy JA, Feng D, Vasile E, Wong WH, Shih SC, Dvorak AM, et al. Permeability properties of tumor surrogate blood vessels induced by VEGF-A. Lab Invest. 2006;86:767–780. doi: 10.1038/labinvest.3700436. [DOI] [PubMed] [Google Scholar]
- 95.Michel CC, Neal CR. Openings through endothelial cells associated with increased microvascular permeability. Microcirculation. 1999;6:45–54. [PubMed] [Google Scholar]
- 96.Bates DO, Harper SJ. Regulation of vascular permeability by vascular endothelial growth factors. Vascul Pharmacol. 2002;39:225–237. doi: 10.1016/s1537-1891(03)00011-9. doi:10.1016/S1537-1891(03)00011-9. [DOI] [PubMed] [Google Scholar]
- 97.Antonetti DA, Barber AJ, Hollinger LA, Wolpert EB, Gardner TW. Vascular endothelial growth factor induces rapid phosphorylation of tight junction proteins occludin and zonula occluden 1. A potential mechanism for vascular permeability in diabetic retinopathy and tumors. J Biol Chem. 1999;274:23463–23467. doi: 10.1074/jbc.274.33.23463. doi:10.1074/jbc.274.33.23463. [DOI] [PubMed] [Google Scholar]
- 98.Esser S, Wolburg K, Wolburg H, Breier G, Kurzchalia T, Risau W. Vascular endothelial growth factor induces endothelial fenestrations in vitro. J Cell Biol. 1998;140:947–959. doi: 10.1083/jcb.140.4.947. doi:10.1083/jcb.140.4.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Feng D, Nagy JA, Hipp J, Pyne K, Dvorak HF, Dvorak AM. Reinterpretation of endothelial cell gaps induced by vasoactive mediators in guinea-pig, mouse and rat: many are transcellular pores. J Physiol (Lond) 1997;504:747–761. doi: 10.1111/j.1469-7793.1997.747bd.x. doi:10.1111/j.1469-7793.1997.747bd.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Roberts WG, Palade GE. Neovasculature induced by vascular endothelial growth factor is fenestrated. Cancer Res. 1997;57:765–772. [PubMed] [Google Scholar]
- 101.Roberts WG, Palade GE. Increased microvascular permeability and endothelial fenestration induced by vascular endothelial growth factor. J Cell Sci. 1995;108:2369–2379. doi: 10.1242/jcs.108.6.2369. [DOI] [PubMed] [Google Scholar]
- 102.Satchell SC, Braet F. Glomerular endothelial cell fenestrations: an integral component of the glomerular filtration barrier. Am J Physiol Renal Physiol. 2009;296:F947–F956. doi: 10.1152/ajprenal.90601.2008. doi:10.1152/ajprenal.90601.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Morbidelli L, Chang CH, Douglas JG, Granger HJ, Ledda F, Ziche M. Nitric oxide mediates mitogenic effect of VEGF on coronary venular endothelium. Am J Physiol. 1996;270:H411–H415. doi: 10.1152/ajpheart.1996.270.1.H411. [DOI] [PubMed] [Google Scholar]
- 104.Morbidelli L, Pyriochou A, Filippi S, Vassiliades Y, Roussos C, Zhou Z, et al. The soluble guanylyl cyclase inhibitor NS-2028 reduces vascular endothelial growth factor-induced angiogenesis and permeability. Am J Physiol Regul Integr Comp Physiol. 2009 doi: 10.1152/ajpregu.00222.2009. [DOI] [PubMed] [Google Scholar]
- 105.Ikeda S, Ushio-Fukai M, Zuo L, Tojo T, Dikalov S, Patrushev NA, et al. Novel role of ARF6 in vascular endothelial growth factor-induced signaling and angiogenesis. Circ Res. 2005;96:467–475. doi: 10.1161/01.RES.0000158286.51045.16. doi:10.1161/01.RES.0000158286.51045.16. [DOI] [PubMed] [Google Scholar]
- 106.Sun H, Breslin JW, Zhu J, Yuan SY, Wu MH. Rho and ROCK signaling in VEGF-induced microvascular endothelial hyperpermeability. Microcirculation. 2006;13:237–247. doi: 10.1080/10739680600556944. doi:10.1080/10739680600556944. [DOI] [PubMed] [Google Scholar]
- 107.Aspenstrom P, Fransson A, Saras J. Rho GTPases have diverse effects on the organization of the actin filament system. Biochem J. 2004;377:327–337. doi: 10.1042/BJ20031041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tiruppathi C, Minshall RD, Paria BC, Vogel SM, Malik AB. Role of Ca2+ signaling in the regulation of endothelial permeability. Vascul Pharmacol. 2002;39:173–185. doi: 10.1016/s1537-1891(03)00007-7. doi:10.1016/S1537-1891(03)00007-7. [DOI] [PubMed] [Google Scholar]
- 109.Eriksson A, Cao R, Roy J, Tritsaris K, Wahlestedt C, Dissing S, et al. Small GTP-binding protein Rac is an essential mediator of vascular endothelial growth factor-induced endothelial fenestrations and vascular permeability. Circulation. 2003;107:1532–1538. doi: 10.1161/01.cir.0000055324.34758.32. doi:10.1161/01.CIR.0000055324.34758.32. [DOI] [PubMed] [Google Scholar]
- 110.Dejana E, Spagnuolo R, Bazzoni G. Interendothelial junctions and their role in the control of angiogenesis, vascular permeability and leukocyte transmigration. Thromb Haemost. 2001;86:308–315. [PubMed] [Google Scholar]
- 111.Dejana E, Orsenigo F, Lampugnani MG. The role of adherens junctions and VE-cadherin in the control of vascular permeability. J Cell Sci. 2008;121:2115–2122. doi: 10.1242/jcs.017897. doi:10.1242/jcs.017897. [DOI] [PubMed] [Google Scholar]
- 112.Taddei A, Giampietro C, Conti A, Orsenigo F, Breviario F, Pirazzoli V, et al. Endothelial adherens junctions control tight junctions by VE-cadherin-mediated upregulation of claudin-5. Nat Cell Biol. 2008;10:923–934. doi: 10.1038/ncb1752. doi:10.1038/ncb1752. [DOI] [PubMed] [Google Scholar]
- 113.Ha CH, Bennett AM, Jin ZG. A novel role of vascular endothelial cadherin in modulating c-Src activation and downstream signaling of vascular endothelial growth factor. J Biol Chem. 2008;283:7261–7270. doi: 10.1074/jbc.M702881200. doi:10.1074/jbc.M702881200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Adamson RH, Michel CC, Parker KH, Phillips CG, Wang W. Pathways through the intercellular clefts of frog mesenteric capillaries. J Physiol (Lond) 1993;466:303–327. [PMC free article] [PubMed] [Google Scholar]
- 115.Zhang X, Curry FR, Weinbaum S. Mechanism of osmotic flow in a periodic fiber array. Am J Physiol Heart Circ. 2006;290:H844–H852. doi: 10.1152/ajpheart.00695.2005. doi:10.1152/ajpheart.00695.2005. [DOI] [PubMed] [Google Scholar]
- 116.Qiu Y, Ferguson J, Neal CR, Kaura A, Wood E, Sage LS, et al. Transgenic VEGF165b isoform-specific over-expression in podocytes reduces glomerular permeability in vivo. J Am Soc Nephrol. 2010 doi: 10.1681/ASN.2009060617. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kamba T, Tam BY, Hashizume H, Haskell A, Sennino B, Mancuso MR, et al. VEGF-dependent plasticity of fenestrated capillaries in the normal adult microvasculature. Am J Physiol Heart Circ. 2006;290:H560–H576. doi: 10.1152/ajpheart.00133.2005. doi:10.1152/ajpheart.00133.2005. [DOI] [PubMed] [Google Scholar]
- 118.Peters S, Heiduschka P, Julien S, Ziemssen F, Fietz H, Bartz-Schmidt KU, et al. Ultrastructural findings in the primate eye after intravitreal injection of bevacizumab. Am J Ophthalmol. 2007;143:995–1002. doi: 10.1016/j.ajo.2007.03.007. doi:10.1016/j.ajo.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 119.Stan RV, Kubitza M, Palade GE. PV-1 is a component of the fenestral and stomatal diaphragms in fenestrated endothelia. Proc Natl Acad Sci USA. 1999;96:13203–13207. doi: 10.1073/pnas.96.23.13203. doi:10.1073/pnas.96.23.13203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fraser HM, Dickson SE, Lunn SF, Wulff C, Morris KD, Carroll VA, et al. Suppression of luteal angiogenesis in the primate after neutralization of vascular endothelial growth factor. Endocrinology. 2000;141:995–1000. doi: 10.1210/endo.141.3.7369. doi:10.1210/en.141.3.995. [DOI] [PubMed] [Google Scholar]
- 121.Pepper MS, Baetens D, Mandriota SJ, Di Sanza C, Oikemus S, Lane TF, et al. Regulation of VEGF and VEGF receptor expression in the rodent mammary gland during pregnancy, lactation, and involution. Dev Dyn. 2000;218:507–524. doi: 10.1002/1097-0177(200007)218:3<507::AID-DVDY1012>3.0.CO;2-5. doi:10.1002/1097-0177(200007)218:3<507::AID-DVDY1012>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 122.Matsumoto M, Nishinakagawa H, Kurohmaru M, Hayashi Y, Otsuka J. Pregnancy and lactation affect the microvasculature of the mammary gland in mice. J Vet Med Sci. 1992;54:937–943. doi: 10.1292/jvms.54.937. [DOI] [PubMed] [Google Scholar]
- 123.Schoefl GI. Studies on inflammation. III. Growing capillaries: their structure and permeability. Virchows Arch Path Anat. 1963;337:97–141. doi:10.1007/BF00963592. [PubMed] [Google Scholar]
- 124.Hurwitz H, Fehrenbacher L, Novotny W, Cartwright T, Hainsworth J, Heim W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–2342. doi: 10.1056/NEJMoa032691. doi:10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 125.Eremina V, Jefferson JA, Kowalewska J, Hochster H, Haas M, Weisstuch J, et al. VEGF inhibition and renal thrombotic microangiopathy. N Engl J Med. 2008;358:1129–1136. doi: 10.1056/NEJMoa0707330. doi:10.1056/NEJMoa0707330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ananthnarayan S, Bahng J, Roring J, Nghiemphu P, Lai A, Cloughesy T, et al. Time course of imaging changes of GBM during extended bevacizumab treatment. J Neurooncol. 2008;88:339–347. doi: 10.1007/s11060-008-9573-x. doi:10.1007/s11060-008-9573-x. [DOI] [PubMed] [Google Scholar]
- 127.Numnum TM, Rocconi RP, Whitworth J, Barnes MN. The use of bevacizumab to palliate symptomatic ascites in patients with refractory ovarian carcinoma. Gynecol Oncol. 2006;102:425–428. doi: 10.1016/j.ygyno.2006.05.018. doi:10.1016/j.ygyno.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 128.Plotkin SR, Stemmer-Rachamimov AO, Barker FG, 2nd, Halpin C, Padera TP, Tyrrell A, et al. Hearing improvement after bevacizumab in patients with neurofibromatosis type 2. N Engl J Med. 2009;361:358–367. doi: 10.1056/NEJMoa0902579. doi:10.1056/NEJMoa0902579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Ferrara N. Role of vascular endothelial growth factor in physiologic and pathologic angiogenesis: therapeutic implications. Semin Oncol. 2002;29:10–14. doi: 10.1053/sonc.2002.37264. [DOI] [PubMed] [Google Scholar]
- 130.Tornquist P, Alm A, Bill A. Permeability of ocular vessels and transport across the blood-retinal-barrier. Eye (Lond) 1990;4:303–309. doi: 10.1038/eye.1990.41. [DOI] [PubMed] [Google Scholar]
- 131.Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med. 2006;355:1419–1431. doi: 10.1056/NEJMoa054481. doi:10.1056/NEJMoa054481. [DOI] [PubMed] [Google Scholar]
- 132.Stitt AW, Gardiner TA, Archer DB. Histological and ultrastructural investigation of retinal microaneurysm development in diabetic patients. Br J Ophthalmol. 1995;79:362–367. doi: 10.1136/bjo.79.4.362. doi:10.1136/bjo.79.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Knudsen ST, Bek T, Poulsen PL, Hove MN, Rehling M, Mogensen CE. Macular edema reflects generalized vascular hyperpermeability in type 2 diabetic patients with retinopathy. Diabetes Care. 2002;25:2328–2334. doi: 10.2337/diacare.25.12.2328. doi:10.2337/diacare.25.12.2328. [DOI] [PubMed] [Google Scholar]