Abstract
OBJECTIVES
Hydrocephalus is a prototypical chronic condition that follows children into adulthood. The objectives of this study were to (1) review how the health care needs of young adults with hydrocephalus are not being met, (2) estimate the numbers of adults with childhood-onset hydrocephalus, (3) describe a novel program to provide care for young adults with hydrocephalus and other chronic pediatric conditions, and (4) propose national strategies to promote successful hydrocephalus transition care.
RESULTS
Adults with hydrocephalus need continuous access to expert surgical and medical providers. Existing care models fail to meet this need. The number of young adults who have hydrocephalus, are aged 18 to 35 and need treatment in the United States is predicted to exceed 40 000 annually within the next 2 decades. We are developing integrated teams of pediatric and adult medical and surgical specialists to provide continuous, coordinated, comprehensive care for individuals with hydrocephalus in a pediatric setting. This setting will train our future physician workforce on optimal transition care. Coordinated national efforts are also needed.
CONCLUSIONS
Providers need to implement appropriate management and transition care for individuals with hydrocephalus. We must work at local and national levels to transform the care model, improve the quality of health care delivery, and improve outcomes for young adults with hydrocephalus.
Keywords: hydrocephalus, health transition, medical education, advocacy
Through medical and surgical advances, the numbers of children with special health care needs are increasing,1,2 as are those who survive into adulthood.3 Each year, nearly 500 000 children in the United States with special health care needs become adults4 and thus need adult health care services.5
Although the exact number of individuals with hydrocephalus is unknown, the condition is not rare and is likely underappreciated.6 Annually, individuals with the diagnosis of hydrocephalus generate 69 000 hospital discharges in the United States7; approximately half involve children.8–11 Each year, US children with hydrocephalus alone generate 38 200 to 39 900 admissions, use 391 000 to 433 000 hospital days, and accumulate hospital charges of $2.0 billion (2003 dollars).11 In 2003, hydrocephalus accounted for 0.6% of all US pediatric admissions, 1.8% of all pediatric hospital days, and 3.1% of all pediatric hospital charges; in contrast, cystic fibrosis accounted for 0.3%, 0.6%, and 0.9%, respectively.11 Whereas the substantial contribution of cystic fibrosis to pediatric morbidity is widely recognized, that of hydrocephalus is obscure.6
Like cystic fibrosis, hydrocephalus is a prototypical chronic condition that follows children into adulthood. In contrast to cystic fibrosis, children who have hydrocephalus and benefited from innovative pediatric treatments often lack adequate care as they become adults. Transition programs for individuals with hydrocephalus are urgently needed.
There are 4 objectives of this article. The first is to review how and why the health care needs of young adults with hydrocephalus are not being met. The second is to present our estimates of the increasing numbers of adults with childhood-onset hydrocephalus. The third is to describe a novel program that we are developing at Primary Children's Medical Center (PCMC), where integrated teams of pediatric and adult medical and surgical specialists provide continuous, coordinated, comprehensive care for individuals with hydrocephalus and other chronic pediatric conditions. The fourth is to propose educational and national strategies to promote successful transitions for individuals with hydrocephalus.
HEALTH CARE NEEDS OF YOUNG ADULTS WITH HYDROCEPHALUS
To receive comprehensive care, adults with hydrocephalus need continuous access to expert surgical and medical providers. Recognition of surgical complications and access to surgical expertise are critical, because cerebrospinal fluid shunts can continue to fail in adulthood.12–14 Medical management for young adults with hydrocephalus must address monitoring for and treatment of adult conditions15 and facilitation of self-care (eg, medication knowledge, ability to discuss care with providers, insurance knowledge).16–20 For young adults with spina bifida, medical management must also address long-term follow-up for associated conditions (eg, epilepsy, cognitive delays, scoliosis, renal impairment, mobility issues)21; prevention of secondary conditions (eg, urologic infections, renal calculi, pressure ulcers, osteomyelitis)22; and facilitation of self-care (eg, bowel and bladder function).17–21 Vocational counseling is essential, because employment and financial independence are linked to well-being.16,23 Related life issues that the providers need to be cognizant of include autonomy,18 independent living,23,24 social integration,23 transportation, child care, insurability,16,23 psychological and/or behavioral services,23 assistance for advocate-parent(s),24 and end-of-life issues.18 Appropriate obstetric management can result in normal pregnancy and delivery for women with hydrocephalus.25–29 Other reproductive issues include genetic evaluation and counseling,28 contraception, parenting, and child care. Finally, patients' holistic well-being, including alternative therapies to address body, mind, and spirit, should be considered. Models of care for adolescents and young adults with hydrocephalus should address each of these health care needs.
Transition Care Models for Young Adults With Chronic Conditions
The goal of transition care for young adults with special health care needs is to maximize lifelong functioning and potential through the provision of high-quality, developmentally appropriate health care services that continue uninterrupted as the individual moves from adolescence to adulthood.4 It is patient centered, responsive, continuous, comprehensive, and coordinated4; however, leaders of the health care system are struggling with this national priority,30 including who should provide transition care, how it should be delivered, and how to finance it.31–33
Several models of transition care for adults with specific pediatric medical conditions exist, including cystic fibrosis,20 congenital heart disease,34 type 1 diabetes,35 and rheumatic disease.36–38 We are unaware of any formal transition care models for young adults with hydrocephalus (Harold Rekate, MD, written personal communication, November 7, 2008). Proposed approaches to transition that help to promote self-management for young adults with chronic conditions and bridge the communication gap between pediatric and adult care providers and include appropriate timing and sufficient preparation for the process itself,39 incorporation of a medical home model,5,40,41 establishment of joint clinics between pediatric and adult providers,42 and electronic personal health records43–45 that include appropriate legal documentation.
Existing transition care models and approaches usually emphasize transition to care that is provided by adult surgical and medicine providers in adult medicine settings. Indeed, only 10% of pediatric neurosurgeons report providing care to their patients as they transition to adulthood (Harold Rekate, MD, personal communication, November 7, 2008). Given a lack of a systematic approach to hydrocephalus transition and adult care, we have termed the state of existing care for young adult with hydrocephalus the “ad hoc” approach.
Ad Hoc Care Model Fails Adults Who Live With Childhood-Onset Hydrocephalus
Ad hoc approaches to follow-up care for young adults most often result in inconsistent and fragmented care. Within 3 years after closing 1 pediatric multidisciplinary clinic, one half to two thirds of patients failed to maintain adequate follow-up.46 In the United Kingdom (where health care coverage is universal), two thirds of patients' shunt function went unassessed after age 16.13 Individuals with childhood-onset hydrocephalus and their parents share troubling anecdotes about the ad hoc approach.33 One 19-year-old woman with shunt failure was admitted to a psychiatric facility for mental status changes, and the mother of a 29-year-old man with recurrent shunt failure was prosecuted for Munchausen's syndrome by proxy. Inappropriate follow-up results in serious morbidity46 and mortality.12 Adults without a designated provider to coordinate care often fail to maintain adequate follow-up care and subsequently endure severe and potentially preventable morbidity.
Ad Hoc Care Model Exists Because of Economic Challenges
The economic challenge of providing integrated health care for adults with chronic conditions is daunting.47 Whereas pediatric care for eligible individuals is supported by state and federal agencies through Medicaid, adult health care for adults with chronic conditions is often fragmented.33 Obtaining adequate private health insurance is challenging for adults with chronic conditions. Although individuals may qualify for Medicaid, the program has an uncertain future and is complicated by poor provider reimbursement and, therefore, a limited number of participating providers. As a result, health care options for adults with childhood-onset hydrocephalus are few, and although traditional integrated care is essential, it is rarely available.
Ad Hoc Care Models Fail Because Adult Health Care Providers Are not Trained to Care for Young Adults With Hydrocephalus
Health care for these individuals is increasingly delegated to adult surgical and medical practitioners. Historically, adult health care providers have not been or needed to be familiar with pediatric conditions such as hydrocephalus. From a surgical perspective, hydrocephalus that is diagnosed and treated in infancy is a very different disease from the type of hydrocephalus that begins in adulthood as a result of hemorrhage, infection, or tumor.48 The pathophysiology of the developing intracranial environment is significantly different from that with which adult neurosurgeons are familiar.
From a medical perspective, adults who live with childhood hydrocephalus have health care needs that are specific to the condition itself, as well as those that are common to all adults. Long-term management of these young adults' condition requires specific provider knowledge, skills, and experience with the underlying condition to render ongoing care and prevent unnecessary morbidity and mortality; however, current adult medicine training programs lack a dedicated curriculum that addresses conditions with pediatric onset. The vast majority of adult providers lack the specific knowledge, skills, and experience to provide adequate ongoing care and are ill prepared to manage an adult's childhood condition, in particular hydrocephalus.49 One exception lies in combined internal medicine and pediatric-trained practitioners. The scope and experience of dual-trained providers make them ideal to deliver long-term care for adults with chronic pediatric conditions.
EMERGING CHALLENGE: AN INCREASING NUMBER OF YOUNG ADULTS WITH HYDROCEPHALUS
PCMC is the pediatric center for Intermountain Healthcare (IH), a vertically integrated health care system in the Intermountain West (Utah, Montana, Idaho, Wyoming, and Nevada). We estimate that IH provides 1% of health care in the United States each year, on the basis of the volume of births (32 000; 0.8% of US totals) and pediatric cerebrospinal fluid shunt placements (63; 1.4% of US totals) in 2007.50 Although the number of individuals who have hydrocephalus and live in the United States is not known, using IH projections (that incorporate inpatient and outpatient encounters), we estimate that the number of people who live in the United States and are treated for hydrocephalus each year ranges between 120 000 and 150 000. One sixth of IH patients are young adults between 18 and 35 years of age (Flory Nkoy, MD, MS, oral personal communication, June 12, 2008). Using IH projections, we predict the number of young adults who have hydrocephalus, are aged 18 to 35, and are treated annually in the United States will exceed 40 000 within the next 2 decades (Fig 1).
FIGURE 1.
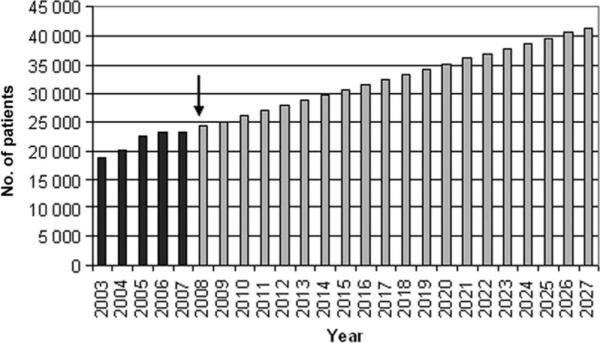
Current and projected numbers of patients with hydrocephalus, aged 18 to 35, treated in the United States. Dark bars indicate projections of numbers of patients based on the actual numbers treated at Intermountain Healthcare; lighter bars indicate future projections for young adults with hydrocephalus. Source data from Intermountain Healthcare.
A Novel Care Model for Young Adults With Chronic Pediatric Conditions at PCMC
Whereas existing models and approaches emphasize transition to care that is provided by adult medicine providers in adult medicine settings, at PCMC, we have chosen to maintain continuity of care programs for adults with chronic pediatric conditions such as hydrocephalus. Our goal is to provide an optimal setting where children, adolescents, and young adults with complex medical conditions can receive comprehensive and integrated19,20,22,52 medical care and establish continuity of care22,52,53 with a designated primary care physician.19,20,52 We are developing integrated teams of pediatricians, internists, and medicine-pediatrics–trained physicians to provide care in a familiar setting with nursing staff and social workers. As needed, generalists are supported by medical (eg, neurology, rehabilitation, genetics) and pediatric surgical (eg, urology, neurosurgery, orthopedics) subspecialists. Midlevel providers (eg, physician assistant[s], nurse practitioners) are also employed to provide continuity.52 Outpatient consultations with psychiatrists, occupational and physical therapists, and nutritionists are available as needed. When preferable for both patient and provider, the care team will facilitate transition from the pediatric to adult setting.33,43 Transition plans are being tailored to meet each patient's individualized needs and goals.33,34,41,53
Novel Care Model: A Setting for Training Future Providers
We are not aware of any other programs such as PCMC's whereby young adults with hydrocephalus receive ongoing care in a pediatric setting. We believe that this program is necessary in our setting until there adequate numbers of adult health care providers are trained to treat adults with chronic pediatric conditions comprehensively.40,54
The need for coordinated patient care opportunities and curriculum to improve education in transition care for trainees is certain. Pediatricians are extensively trained to care for children with special health care needs and increasingly must facilitate transition to adult care55–58; however, pediatricians are not trained to care for adults.58 In contrast, although well trained to care for adults, internal medicine and family medicine physicians have little exposure to caring for adults with developmental disabilities.58,59 Trainees in pediatrics, internal medicine, family medicine, and surgical specialties must identify the multifaceted needs of adolescents who have chronic medical conditions and will make the transition from pediatric to adult-centered care.
We believe that integrated clinic models that include generalists, nurses and social workers, and subspecialists and subspecialty surgeons as needed are the ideal forum to educate house officers, providing them opportunities to develop their medical knowledge and a framework for successful transition. We are developing curricula to address (1) identification of overall needs of individuals with chronic conditions as they transition from pediatric to adult-centered care; (2) barriers to transition of care; (3) optimal comprehensive medical and surgical care for patients in an adult-centered system; and (4) attitudes, knowledge, and skills required to care for adults with special health care needs.
A NATIONAL EMPHASIS ON TRANSITION CARE IS NEEDED FOR YOUNG ADULTS WITH CHRONIC CONDITIONS
A minimum standard for education in transition care should be developed and used nationally in pediatric and adult medicine training programs, similar to medical genetics for internal medicine training programs.60 Current residency requirements established by the Accreditation Council for Graduate Medical Education for trainees in internal medicine and family medicine training programs do not require delivery of curricula to address health care transition. Pediatric and combined medicine-pediatric training programs are required to teach trainees management strategies for children with developmental disabilities or special needs within the context of the medical home. Producing a future physician workforce that is competent to render developmentally appropriate health care and health care transition for individuals with hydrocephalus is paramount.61 Ensuring that these competencies are taught to primary care providers must be an integral component of training and certification requirements.61 Chronic condition management and/or transition care programs then must undergo evaluation after they are created and delivered to ensure that optimal quality of care for patients with hydrocephalus is provided. We need a future health care system in which all adults, including those with chronic pediatric conditions such as hydrocephalus, receive adult-oriented primary health care from appropriately trained providers.
Novel Care Model: An Economic Solution?
At PCMC, we are providing pediatric neurosurgical and medical care for young adults with hydrocephalus in the pediatric setting. Health care costs are the responsibility of state and federal payment systems. The remaining coverage is provided by a composite of private insurance and charity care. Significant difficulty in our model arises when patients reach adult age. While they are children, private insurers reimburse care because PCMC is the only pediatric specialty center in the Intermountain West. When they become young adults, private insurers can refuse to cover services that could be rendered at one of their contracted adult facilities. Although these facilities may be less optimal, payers are not obligated to continue to cover services at a pediatric specialty center for adult patients. If center certification were available for facilities that specialize in hydrocephalus care, much like that for individuals with cystic fibrosis, then access to and payment for appropriate quality care for young adults with hydrocephalus would emerge. Similar specialized programs of coordinated care for children and youth with high medical complexity and fragility have demonstrated cost savings. One such program for 227 children decreased hospital days from 7926 to 3831 and decreased hospital payments by $10.7 million during a 2- to 3-year study period.42 Evidence is building that timely and appropriate medical and surgical care can ultimately reduce costs. With a renewed national emphasis on comparative effectiveness, the care of children with hydrocephalus warrants additional study. For US children who have hydrocephalus and use 400 000 hospital days and $2 billion in charges ($2003), there is much room for improvement.
A NATIONAL EMPHASIS ON COORDINATED COMPREHENSIVE CARE FOR YOUNG ADULTS COULD IMPROVE OUTCOMES FOR INDIVIDUALS WITH HYDROCEPHALUS
The Cystic Fibrosis Foundation provides an excellent model of complex, chronic condition management that has transformed quality of care and outcomes for patients of all ages with cystic fibrosis during the 4 decades.21 Cystic fibrosis affects fewer people in the United States than hydrocephalus, including 30 000 individuals and 1100 new people each year.21 The Cystic Fibrosis Foundation funds and accredits more than 155 care centers nationwide that offer high-quality care, common protocols, and patient support.62,63 The high quality of specialized care has dramatically improved outcomes, including lung function and survival for patients with cystic fibrosis.21 The Cystic Fibrosis Foundation has achieved these outcomes for individuals with cystic fibrosis by (1) maintaining a patient registry for more than 40 years,21 (2) using this registry to define high-quality care,64 (3) reviewing and accrediting centers, (4) supporting robust quality improvement initiatives, and (5) providing center-specific reports on patient outcomes.
We suggest that the Hydrocephalus Association play a role in transforming the quality of care for all individuals with hydrocephalus by emphasizing coordinated comprehensive clinical care, following the model of the Cystic Fibrosis Foundation. The authors believe that to achieve what the Cystic Fibrosis Foundation accomplished during the past 40 years for individuals with hydrocephalus in the current health care system, the Hydrocephalus Association would need to partner with a broad range of stakeholders, including patients, families, researchers, care providers, government agencies, and payers to do the following: (1) partner with researchers such as those in the Hydrocephalus Clinical Research Network, a philanthropically funded research network of pediatric neurosurgeons and a partner of the Hydrocephalus Association, to extend a patient registry nationally; (2) simultaneously work with care providers (eg, National Association of Children's Hospitals and Related Institutions, American Academy of Pediatrics, American Academy of Neurologic Surgeons, Congress of Neurologic Surgeons) as well as opinion leaders within the field to define high-quality care; (3) collaborate with researchers and government agencies (eg, National Institutes of Health, Agency for Healthcare Research and Quality, Centers for Disease Control and Prevention) to refine and implement quality standards, review and accredit centers, support robust quality improvement initiatives, and provide center-specific reports on patient outcomes; and, last, (4) work with payers (eg, Center for Medicaid and Medicare Services) to streamline access to care and care delivery. By emphasizing coordinated comprehensive clinical care, the Hydrocephalus Association and its partners could transform care and ultimately improve outcomes for all individuals with hydrocephalus.
CONCLUSIONS
Medical and surgical care needs for adults with childhood-onset hydrocephalus often go unaddressed. All young adults need continuous and comprehensive care. In particular, those with chronic pediatric conditions must transition smoothly, regardless of the setting, to adult-centered care. It is paramount that medical and surgical providers become aware of and implement appropriate chronic condition management and transition care. We must work at local and national levels to transform the care model for patients with hydrocephalus.
ACKNOWLEDGMENTS
Dr Simon is a PCMC Foundation Scholar, and her work is supported in part by Award K23NS062900 from the National Institute of Neurological Disorders And Stroke, a PCMC Innovative a PCMC Innovative Research Grant and the Children's Health Research Center, University of Utah. Drs Simon and Walker are Hydrocephalus Clinical Research Network Investigators.
We thank Flory Nkoy for providing analytic support and Chris Maloney, Stephan Nemeth, and Dory Kranz, Executive Director of the Hydrocephalus Association for thoughtful feedback.
ABBREVIATIONS
- PCMC
Primary Children's Medical Center
- IH
Intermountain Healthcare
Footnotes
Portions of this work were presented in Dr Clark's Scientific Keynote lecture at the 10th National Conference on Hydrocephalus of the Hydrocephalus Association; Park City, Utah; June 20, 2008. www.pediatrics.org/cgi/doi/10.1542/peds.2008-3834
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
REFERENCES
- 1.Perrin JM, Bloom SR, Gortmaker SL. The increase of childhood chronic conditions in the United States. JAMA. 2007;297(24):2755–2759. doi: 10.1001/jama.297.24.2755. [DOI] [PubMed] [Google Scholar]
- 2.van der Lee JH, Mokkink LB, Grootenhuis MA, Heymans HS, Offringa M. Definitions and measurement of chronic health conditions in childhood: a systematic review. JAMA. 2007;297(24):2741–2751. doi: 10.1001/jama.297.24.2741. [DOI] [PubMed] [Google Scholar]
- 3.Blum RW. Transition to adult health care: setting the stage. J Adolesc Health. 1995;17(1):3–5. doi: 10.1016/1054-139X(95)00073-2. [DOI] [PubMed] [Google Scholar]
- 4.A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 pt 2):1304–1306. [PubMed] [Google Scholar]
- 5.Lotstein DS, McPherson M, Strickland B, Newacheck PW. Transition planning for youth with special health care needs: results from the National Survey of Children with Special Health Care Needs. Pediatrics. 2005;115(6):1562–1568. doi: 10.1542/peds.2004-1262. [DOI] [PubMed] [Google Scholar]
- 6.Williams MA, McAllister JP, Walker ML, et al. Priorities for hydrocephalus research: report from a National Institutes of Health-sponsored workshop. J Neurosurg. 2007;107(5 suppl):345–357. doi: 10.3171/PED-07/11/345. [DOI] [PubMed] [Google Scholar]
- 7.Patwardhan RV, Nanda A. Implanted ventricular shunts in the United States: the billion-dollar-a-year cost of hydrocephalus treatment. Neurosurgery. 2005;56(1):139–144. doi: 10.1227/01.neu.0000146206.40375.41. discussion 144–145. [DOI] [PubMed] [Google Scholar]
- 8.Wiswell TE, Tuttle DJ, Northam RS, Simonds GR. Major congenital neurologic malformations: a 17-year survey. Am J Dis Child. 1990;144(1):61–67. doi: 10.1001/archpedi.1990.02150250071035. [DOI] [PubMed] [Google Scholar]
- 9.Edwards RJ, Dombrowski SM, Luciano MG, Pople IK. Chronic hydrocephalus in adults. Brain Pathol. 2004;14(3):325–336. doi: 10.1111/j.1750-3639.2004.tb00072.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Casmiro M, Benassi G, Cacciatore FM, D'Alessandro R. Frequency of idiopathic normal pressure hydrocephalus. Arch Neurol. 1989;46(6):608. doi: 10.1001/archneur.1989.00520420026019. [DOI] [PubMed] [Google Scholar]
- 11.Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JR. Hospital care for children with hydrocephalus in the United States: utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr. 2008;1(2):131–137. doi: 10.3171/PED/2008/1/2/131. [DOI] [PubMed] [Google Scholar]
- 12.Buxton N, Punt J. Failure to follow patients with hydrocephalus shunts can lead to death. Br J Neurosurg. 1998;12(5):399–401. doi: 10.1080/02688699844574. [DOI] [PubMed] [Google Scholar]
- 13.Tomlinson P, Sugarman ID. Complications with shunts in adults with spina bifida. BMJ. 1995;311(7000):286–287. doi: 10.1136/bmj.311.7000.286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGirt MJ, Leveque JC, Wellons JC, 3rd, et al. Cerebrospinal fluid shunt survival and etiology of failures: a seven-year institutional experience. Pediatr Neurosurg. 2002;36(5):248–255. doi: 10.1159/000058428. [DOI] [PubMed] [Google Scholar]
- 15.McDonnell GV, McCann JP. Why do adults with spina bifida and hydrocephalus die? A clinic-based study. Eur J Pediatr Surg. 2000;10(suppl 1):31–32. doi: 10.1055/s-2008-1072411. [DOI] [PubMed] [Google Scholar]
- 16.Ito JA, Stevenson E, Nehring W, Alpeter A, Grant J. A qualitative examination of adolescents and adults with myelomeningocele: their perspective. Eur J Pediatr Surg. 1997;7(suppl 1):53–54. [PubMed] [Google Scholar]
- 17.Barf HA, Post MW, Verhoef M, Jennekens-Schinkel A, Gooskens RH, Prevo AJ. Life satisfaction of young adults with spina bifida. Dev Med Child Neurol. 2007;49(6):458–463. doi: 10.1111/j.1469-8749.2007.00458.x. [DOI] [PubMed] [Google Scholar]
- 18.Bailey S, O'Connell B, Pearce J. The transition from paediatric to adult health care services for young adults with a disability: an ethical perspective. Aust Health Rev. 2003;26(1):64–69. doi: 10.1071/ah030064. [DOI] [PubMed] [Google Scholar]
- 19.Michaud PA, Suris JC, Viner R. The adolescent with a chronic condition: part II—healthcare provision. Arch Dis Child. 2004;89(10):943–949. doi: 10.1136/adc.2003.045377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parker HW. Transition and transfer of patients who have cystic fibrosis to adult care. Clin Chest Med. 2007;28(2):423–432. doi: 10.1016/j.ccm.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 21.McDonnell GV, McCann JP. Issues of medical management in adults with spina bifida. Childs Nerv Syst. 2000;16(4):222–227. doi: 10.1007/s003810050502. [DOI] [PubMed] [Google Scholar]
- 22.Kinsman SL, Doehring MC. The cost of preventable conditions in adults with spina bifida. Eur J Pediatr Surg. 1996;6(suppl 1):17–20. doi: 10.1055/s-2008-1071031. [DOI] [PubMed] [Google Scholar]
- 23.Gupta N, Park J, Solomon C, Kranz DA, Wrensch M, Wu YW. Long-term outcomes in patients with treated childhood hydrocephalus. J Neurosurg. 2007;106(5 suppl):334–339. doi: 10.3171/ped.2007.106.5.334. [DOI] [PubMed] [Google Scholar]
- 24.Murphy N, Christian B. Disability in children and young adults: the unintended consequences. Arch Pediatr Adolesc Med. 2007;161(10):930–932. doi: 10.1001/archpedi.161.10.930. [DOI] [PubMed] [Google Scholar]
- 25.Liakos AM, Bradley NK, Magram G, Muszynski C. Hydrocephalus and the reproductive health of women: the medical implications of maternal shunt dependency in 70 women and 138 pregnancies. Neurol Res. 2000;22(1):69–88. doi: 10.1080/01616412.2000.11741040. [DOI] [PubMed] [Google Scholar]
- 26.Bradley NK, Liakos AM, McAllister JP, 2nd, Magram G, Kinsman S, Bradley MK. Maternal shunt dependency: implications for obstetric care, neurosurgical management, and pregnancy outcomes and a review of selected literature. Neurosurgery. 1998;43(3):448–460. doi: 10.1097/00006123-199809000-00030. discussion 460–461. [DOI] [PubMed] [Google Scholar]
- 27.Liakos AM, Bradley NK, McAllister JP, Magram G, Kinsman SL. Hydrocephalus and pregnancy: the medical implications of maternal shunt dependency. Eur J Pediatr Surg. 1997;7(suppl 1):51–52. [PubMed] [Google Scholar]
- 28.Cusimano MD, Meffe FM, Gentili F, Sermer M. Management of pregnant women with cerebrospinal fluid shunts. Pediatr Neurosurg. 1991;17(1):10–13. doi: 10.1159/000120558. [DOI] [PubMed] [Google Scholar]
- 29.Gast MJ, Grubb RL, Jr, Strickler RC. Maternal hydrocephalus and pregnancy. Obstet Gynecol. 1983;62(3 suppl):29s–31s. [PubMed] [Google Scholar]
- 30. [Accessed August 28, 2008];Healthy People 2010. Available at: www.healthypeople.gov/publications/.
- 31.Freed GL, Hudson EJ. Transitioning children with chronic diseases to adult care: current knowledge, practices, and directions. J Pediatr. 2006;148(6):824–827. doi: 10.1016/j.jpeds.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 32.While A, Forbes A, Ullman R, Lewis S, Mathes L, Griffiths P. Good practices that address continuity during transition from child to adult care: synthesis of the evidence. Child Care Health Dev. 2004;30(5):439–452. doi: 10.1111/j.1365-2214.2004.00440.x. [DOI] [PubMed] [Google Scholar]
- 33.Reiss J, Gibson R. Health care transition: destinations unknown. Pediatrics. 2002;110(6 pt 2):1307–1314. [PubMed] [Google Scholar]
- 34.Reid GJ, Irvine MJ, McCrindle BW, et al. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113(3) doi: 10.1542/peds.113.3.e197. Available at: www.pediatrics.org/cgi/content/full/113/3/e197. [DOI] [PubMed] [Google Scholar]
- 35.Weissberg-Benchell J, Wolpert H, Anderson BJ. Transitioning from pediatric to adult care: a new approach to the post-adolescent young person with type 1 diabetes. Diabetes Care. 2007;30(10):2441–2446. doi: 10.2337/dc07-1249. [DOI] [PubMed] [Google Scholar]
- 36.Jordan A, McDonagh JE. Recognition of emerging adulthood in UK rheumatology: the case for young adult rheumatology service developments. Rheumatology (Oxford) 2007;46(2):188–191. doi: 10.1093/rheumatology/kel368. [DOI] [PubMed] [Google Scholar]
- 37.McDonagh JE, Southwood TR, Shaw KL. The impact of a coordinated transitional care programme on adolescents with juvenile idiopathic arthritis. Rheumatology (Oxford) 2007;46(1):161–168. doi: 10.1093/rheumatology/kel198. [DOI] [PubMed] [Google Scholar]
- 38.McDonagh JE. Transition of care from paediatric to adult rheumatology. Arch Dis Child. 2007;92(9):802–807. doi: 10.1136/adc.2006.103796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Binks JA, Barden WS, Burke TA, Young NL. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88(8):1064–1073. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 40.Kelly AM, Kratz B, Bielski M, Rinehart PM. Implementing transitions for youth with complex chronic conditions using the medical home model. Pediatrics. 2002;110(6 pt 2):1322–1327. [PubMed] [Google Scholar]
- 41.Gordon JB, Colby HH, Bartelt T, Jablonski D, Krauthoefer ML, Havens P. A tertiary care-primary care partnership model for medically complex and fragile children and youth with special health care needs. Arch Pediatr Adolesc Med. 2007;161(10):937–944. doi: 10.1001/archpedi.161.10.937. [DOI] [PubMed] [Google Scholar]
- 42.Kennedy A, Sloman F, Douglass JA, Sawyer SM. Young people with chronic illness: the approach to transition. Intern Med J. 2007;37(8):555–560. doi: 10.1111/j.1445-5994.2007.01440.x. [DOI] [PubMed] [Google Scholar]
- 43.Tulu B, Horan TA. The electronic disability record: purpose, parameters, and model use case. J Am Med Inform Assoc. 2009;16(1):7–13. doi: 10.1197/jamia.M2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Grant RW, Wald JS, Schnipper JL, et al. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008;168(16):1776–1782. doi: 10.1001/archinte.168.16.1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Leath BA. Medical Homes and ePHRs Offer Potential for Improving Care for Persons With Chronic Illnesses and/or Disabilities. American Public Health Association; San Diego, CA: 2008. [Google Scholar]
- 46.Kaufman BA, Terbrock A, Winters N, Ito J, Klosterman A, Park TS. Disbanding a multidisciplinary clinic: effects on the health care of myelomeningocele patients. Pediatr Neurosurg. 1994;21(1):36–44. doi: 10.1159/000120812. [DOI] [PubMed] [Google Scholar]
- 47.Damiano PC, Momany ET, Tyler MC, Penziner AJ, Lobas JG. Cost of outpatient medical care for children and youth with special health care needs: investigating the impact of the medical home. Pediatrics. 2006;118(4) doi: 10.1542/peds.2005-3018. Available at: www.pediatrics.org/cgi/content/full/118/4/e1187. [DOI] [PubMed] [Google Scholar]
- 48.Vinchon M, Dhellemmes P. The transition from child to adult in neurosurgery. Adv Tech Stand Neurosurg. 2007;32:3–24. doi: 10.1007/978-3-211-47423-5_1. [DOI] [PubMed] [Google Scholar]
- 49.Newacheck PW, Taylor WR. Childhood chronic illness: prevalence, severity, and impact. Am J Public Health. 1992;82(3):364–371. doi: 10.2105/ajph.82.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Statistics USNCfH [Accessed August 9, 2009];Fast Stats. Available at: www.cdc.gov/nchs/fastats/births.htm.
- 51.Morgan DJ, Blackburn M, Bax M. Adults with spina bifida and/or hydrocephalus. Postgrad Med J. 1995;71(831):17–21. doi: 10.1136/pgmj.71.831.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Soanes C, Timmons S. Improving transition: a qualitative study examining the attitudes of young people with chronic illness transferring to adult care. J Child Health Care. 2004;8(2):102–112. doi: 10.1177/1367493504041868. [DOI] [PubMed] [Google Scholar]
- 53.Rosenbaum P, Stewart D. Perspectives on transitions: rethinking services for children and youth with developmental disabilities. Arch Phys Med Rehabil. 2007;88(8):1080–1082. doi: 10.1016/j.apmr.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 54.Blum RW, Garell D, Hodgman CH, et al. Transition from child-centered to adult healthcare systems for adolescents with chronic conditions: a position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993;14(7):570–576. doi: 10.1016/1054-139x(93)90143-d. [DOI] [PubMed] [Google Scholar]
- 55.Hallum A. Disability and the transition to adulthood: issues for the disabled child, the family, and the pediatrician. Curr Probl Pediatr. 1995;25(1):12–50. doi: 10.1016/s0045-9380(06)80013-7. [DOI] [PubMed] [Google Scholar]
- 56.Olsen DG, Swigonski NL. Transition to adulthood: the important role of the pediatrician. Pediatrics. 2004;113(3) doi: 10.1542/peds.113.3.e159. Available at: www.pediatrics.org/cgi/content/full/118/4/e1187. [DOI] [PubMed] [Google Scholar]
- 57.Williams MS. Adult dysmorphology: perspectives on approach to diagnosis and care. Am J Med Genet C Semin Med Genet. 2007;145C(3):227–229. doi: 10.1002/ajmg.c.30134. [DOI] [PubMed] [Google Scholar]
- 58.Suther S, Goodson P. Barriers to the provision of genetic services by primary care physicians: a systematic review of the literature. Genet Med. 2003;5(2):70–76. doi: 10.1097/01.GIM.0000055201.16487.61. [DOI] [PubMed] [Google Scholar]
- 59.Riegert-Johnson DL, Korf BR, et al. Outline of a medical genetics curriculum for internal medicine residency training programs. Genet Med. 2004;6(6):543–547. doi: 10.1097/01.gim.0000144561.77590.85. [DOI] [PubMed] [Google Scholar]
- 60.Rosen DS, Blum RW, Britto M, Sawyer SM, Siegel DM. Transition to adult health care for adolescents and young adults with chronic conditions: position paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33(4):309–311. doi: 10.1016/s1054-139x(03)00208-8. [DOI] [PubMed] [Google Scholar]
- 61. [Accessed September 19, 2009];Cystic Fibrosis Care Centers. Available at: www.cff.org/LivingWithCF/CareCenterNetwork/CFFoundation-accreditedCare Centers/.
- 62.McLaughlin SE, Diener-West M, Indurkhya A, Rubin H, Heckmann R, Boyle MP. Improving transition from pediatric to adult cystic fibrosis care: lessons from a national survey of current practices. Pediatrics. 2008;121(5) doi: 10.1542/peds.2007-2217. Available at: www.pediatrics.org/cgi/content/full/121/5/e1160. [DOI] [PubMed] [Google Scholar]
- 63.Yankaskas JR, Marshall BC, Sufian B, Simon RH, Rodman D. Cystic fibrosis adult care: consensus conference report. Chest. 2004;125(1 suppl):1S–39S. doi: 10.1378/chest.125.1_suppl.1s. [DOI] [PubMed] [Google Scholar]


