Abstract
We explored using the ActiGraph accelerometer to differentiate activity levels between participants in a physical activity (PA, n=54) or `successful aging' (SA) program (n = 52). The relationship between a PA questionnaire for older adults (CHAMPS) and accelerometry variables was also determined. Individualized accelerometry count thresholds (THRESHIND) measured during a 400-m walk were used to identify “meaningful activity.” Participants then wore the ActiGraph for 7 days. Results indicated more activity bouts·d−1 ≥ 10 min above THRESHIND in the PA group compared to SA group (1.1 ± 2.0 vs 0.5 ± 0.8, p = 0.05) and more activity counts·d−1 above THRESHIND for the PA group (28,101 ± 27,521) compared to the SA group (17,234 ± 15,620, p = 0.02). Correlations between activity counts·hr−1 and CHAMPS ranged from 0.27 – 0.42, p<0.01. The ActiGraph and THRESHIND may be useful for differentiating PA levels in older adults at risk for mobility disability.
An estimated 11 million older adults in the US, or approximately one-third of non-institutionalized adults ≥ 65 years, report having mobility disability (defined as having difficulty going outside the home) (Waldrop & Stern, 2003). Mobility disability poses a threat to the maintenance of independence for older adults and has been associated with higher incidence of certain chronic diseases, depressive symptoms, and an increased rate of institutionalization (Fried & Guralnik, 1997; Van Den Brink et al., 2006). Because evidence suggests that physical inactivity is strongly associated with mobility disability in older adults (Avlund, Vass, & Hendriksen, 2003; Buchner, Beresford, Larson, LaCroix, & Wagner, 1992; Depp & Jeste, 2006; Hirvensalo, Rantanen, & Heikkinen, 2000; Wannamethee, Ebrahim, Papacosta, & Shaper, 2005), effective physical activity interventions may play a major role in reducing the risk of mobility disability and associated sequelae. Accordingly, valid and accurate measurement of physical activity in persons at risk for physical disability is key to documenting current physical activity levels and measuring outcomes from interventions aimed at reducing the rate of decline in mobility.
Self-report measures (e.g., questionnaires, activity logs, surveys) have been commonly used across a wide range of ages to assess physical activity and offer an economical means of reaching a large number of people. However, the recall of physical activity required for such measures is a challenging cognitive task (Baranowski, 1988) and may expose recall and memory limitations, particularly among older individuals. Further, older adults are more likely to engage in light- to moderate-intensity physical activity, the most difficult type of activity to recall (Baranowski, 1988; Washburn, Jette, & Janney, 1990).
Motion sensors offer an objective, unobtrusive means of capturing movement of the body and are emerging as a viable alternative or supplement to traditional self-report measures. Accelerometers, a type of motion sensor, measure the acceleration of the trunk or limb to which it is attached, and have the capacity to document volume and intensity of activity. The theoretical basis for the use of accelerometers in physical activity assessment is that acceleration is directly proportional to muscular forces and thus is related to energy expenditure (Melanson & Freedson, 1996). The relationship between accelerometry “activity counts” and energy expenditure during locomotor activities has prompted the development of activity count “cut points” or thresholds that have been used to characterize activity intensity level (eg., moderate, hard, vigorous). In light of recent physical activity guidelines that specify intensity levels (Haskell et al., 2007) and the importance of relative intensity levels in older adult recommendations (Nelson et al., 2007), activity count cut points could prove useful in delineating “meaningful” activity with regard to health benefits. However, very few studies have included older adults in the development of such cut points.
In the few studies that have been conducted, results have been encouraging regarding the validity of the ActiGraph (formerly CSA) accelerometer (ActiGraph, LLC, Fort Walton Beach, FL) in older adults. Focht et al. (2003) monitored adults (age range: 45–86 yrs) during a supervised exercise session and reported acceptable convergent and concurrent validity for the ActiGraph. Boon et al. (2003) measured total energy expenditure in 20 older adults (mean ± SD age: 73 ± 8 yrs) via indirect calorimetry and found correlations ranging from 0.5 – 0.6 (P ≤ 0.03) with ActiGraph daily activity counts. Given the potentially beneficial impact that physical activity may have on the health and functioning of older adults at risk for physical disability in addition to the heightened challenges with self-reporting in some older adult populations, additional research exploring the usefulness of accelerometry as a physical activity assessment tool in older frailer adults is warranted.
The present investigation was funded as an ancillary study to the LIFE-P trial (Pahor et al., 2006) (see below) and served as an initial evaluation of the ActiGraph in an older adult sample with an elevated risk of major mobility disability. The overarching goal was to provide data to inform power calculations for a larger trial and conduct preliminary analyses with regard to convergent validity among physical activity measures. Specifically, the present study evaluated older adults at risk for mobility disability to address the following research objectives:
-
◆
Determine the practicality of and compliance with using the ActiGraph in non-supervised, naturalistic settings in men and women aged 70 – 89 years;
-
◆
Determine the capability of the ActiGraph to distinguish a difference in activity level between a subset of participants assigned to a physical activity (PA) program versus a health education (non-exercise, `successful aging' [SA]) program);
-
◆
Develop an individualized accelerometry-based activity count threshold associated with “meaningful” activity and evaluate its use in differentiating activity levels between the PA and SA programs; and,
-
◆
Determine the relationship of the ActiGraph variables with a validated physical activity questionnaire for older adults.
METHOD
Study design
Participants of the present study were a subgroup from both intervention arms of a larger study called the Lifestyle Interventions and Independence for Elders pilot (LIFE-P) study. Details of LIFE-P have been described previously (Pahor et al., 2006; Rejeski et al., 2005). Briefly, LIFE-P was a multi-center randomized controlled trial designed to compare a physical activity (PA) intervention to a successful aging (SA) intervention with regard to the effect on the Short Physical Performance Battery (SPPB) score, a measure of lower extremity physical function (Guralnik et al., 1994). The study was conducted at four field centers: Cooper Institute, University of Pittsburgh, Stanford University, and Wake Forest University. The Administrative Coordinating Center and Data Management and Quality Control Center were also located at Wake Forest University. The present sub-study was conducted at the University of Pittsburgh and Stanford University field centers. The appropriate institutional review board approvals were obtained. All participants provided written informed consent.
Participants
The following eligibility criteria for LIFE-P were designed, in part, to identify older, community-dwelling sedentary individuals at high risk for mobility disability:
-
◆
Aged 70– 89 years old;
-
◆
Self-reported low physical activity levels (< 20 minutes/week spent in regular physical activity within the last month);
-
◆
At risk for mobility disability as indicated by a summary score of < 9 on the SPPB;
-
◆
Ability to complete a 400-m walk in < 15 minutes without sitting or the use of an assistive device;
-
◆
Willing to provide informed consent and participate fully in either intervention and all assessment procedures; and,
-
◆
Planned residence in the area for the study duration.
In addition to English-speakers, participants who had a preference for communicating in Spanish were enrolled at the Stanford field center. Individuals were excluded if they had any medical condition that would limit participation in a moderate-intensity physical activity program, of if they had cognitive impairment as indicated by a Mini-Mental State Exam score of < 21 (Folstein, Folstein, & McHugh, 1975).
Intervention
Subjects were randomized, stratified by gender and field center, to the PA arm and participated in aerobic, strengthening, balance, and flexibility exercises. Walking was the primary mode of aerobic activity. Participants were required to attend an hour-long supervised exercise session 3 times per week for the first 2 months, 2 times per week for the next 4 months, and 1 time per week until the end of the 12-month intervention. As the class-based activity requirement was reduced, a shift to home-based physical activity was encouraged, with a goal of 3 times per week of home-based activity. Participants were taught how to exercise safely on their own, and tools/strategies were provided to help maintain compliance and to address possible barriers to the home-based activity requirements. The SA arm consisted of interactive classes and field trips focused on a range of non-exercise topics relevant for the older adult. Light, upper body stretching activities were conducted during the SA classes. Field trip activities included minimum walking (e.g., walking in a museum with frequent breaks); no other activity related actions were done.
Accelerometry
Physical activity data were collected at the 6- or 12-month time-point of LIFE-P using the ActiGraph model 7164 accelerometer (ActiGraph, LLC, Fort Walton Beach, FL). The ActiGraph is a one-dimensional accelerometer housed in a plastic enclosure measuring 5.1 × 4.1 × 1.5 cm with a weight of 42.4 g. The ActiGraph records the magnitude and intensity of movement by measuring acceleration and deceleration between the magnitudes of 0.05 and 2g (where g is equal to 9.825 m·s−2, the acceleration of gravity), within a frequency range of 0.25 to 2.5 Hz. Output from the ActiGraph is in the form of activity “counts,” where one count is equivalent to 16 milli-g per second. Motion can be measured over a user-defined epoch or period of time, with a data storage capacity of 22 consecutive days using a 1-minute epoch.
To our knowledge, there are no widely accepted accelerometer thresholds or “cut-points” with which to evaluate various activity levels in an older adult population. As a result, we calculated an “individualized activity count threshold” (THRESHIND) for each participant using data collected during a 400-meter walk. The average count·min−1 generated by a participant during the 400-m walk served as his/her THRESHIND. For subsequent analyses, activity counts above this level were operationally defined as “meaningful” activity. Activities related to the 400-m walk data collection are as follows. The ActiGraph was initialized approximately 30 minutes prior to the participant's clinic visit and programmed to record data in 1-minute epochs. Prior to the walk, the monitor was attached at the waistline using a clip and placed along the right midaxillary line. The beginning and end of the 400-m walk were identified on the ActiGraph by using the Event Marker Mode of the monitor. Specifically, research staff used a company-provided field test magnet that was momentarily placed along the left side of the activity monitor case at the start and end of the 400-m walk. Marking an event in this manner resulted in a negative sign for the activity count value corresponding to the beginning and end of the walk. As a result, the activity counts associated with the 400-m walk could be easily identified during subsequent analyses. In addition, staff recorded the start time and end time for the walk. Participants were instructed to walk 10 laps of a 20-meter distance at their usual pace and without overexertion. At the end of the 4th lap, subjects were asked to rate their level of exertion using a 4-point scale where 1 = “light,” 2 = “somewhat hard,” 3 = “hard,” and 4 = “very hard.” Participants with a rating of “hard” or “very hard” were required to adjust their walking pace to a “light” or “somewhat hard” intensity level. In addition, at the conclusion of the walk a subset of participants were asked to evaluate their perceived exertion level using the 15-point Borg Scale for Perceived Exertion (Borg, 1982). Activity counts during the first and last minute of the 400-m walk were deleted, with the remaining counts averaged and used to represent the THRESHIND in counts·min−1. Failure to complete the 400-m walk test within 15 minutes was defined as major mobility disability and resulted in the exclusion of 1 participant from this sub-study.
At the conclusion of the walk, participants kept the monitor on and wore it for the 7 days immediately following their clinic visit. During the 7-d monitoring period, participants were asked to put the monitor on each morning (after dressing) and remove the monitor just prior to going to bed at night. The monitor was also removed for bathing, showering, or any other activity that might result in exposure to water. In addition, participants were asked to keep a concurrent log to record the time(s) of day that the monitor was put on and removed. Participants were instructed to contact research staff by telephone with any questions about monitor use. Following the 7th complete day of activity monitoring, participants returned their log and activity monitor to research staff via mail.
Physical activity self-report
The Community Healthy Activities Model Program for Seniors (CHAMPS) questionnaire (Stewart, Mills et al., 2001) was used to assess physical activity level and has been shown to have acceptable validity, reliability and sensitivity to change in older adults (Harada, Chiu, King, & Stewart, 2001; King, Baumann, O'Sullivan, Wilcox, & Castro, 2002; King et al., 2000; Stewart, Verboncoeur et al., 2001). The CHAMPS questionnaire was interviewer-administered and is designed to assess weekly frequency and duration of activities typically undertaken by older adults. The recall timeframe is “a typical or normal week during the past 4 weeks.” Activities listed in the CHAMPS questionnaire were assigned a metabolic equivalent (MET) value specific for older adults, as described by Stewart et al. (2001) that provide for coding and classification of activities by rate of energy expenditure. Research staff used probing techniques during the interview to determine the actual time spent in those activities categorized as being at least moderate-intensity (MOD+), or ≥ 3 METs, where 1 MET is equivalent to the metabolic cost during quiet sitting. Outcome measures from the CHAMPS questionnaire include caloric expenditure per week and frequency per week for MOD+ activities, and all physical activities, including those of light intensity. Activities classified as light intensity were those with an energy expenditure of < 3 METs. CHAMPS data collected at 6- or 12-months were used in the present investigation.
Accelerometer data processing
A program was created for use with SAS v. 9.1.3 (SAS Institute, Inc., Cary, N.C.) to download, process, and calculate accelerometer variables. Daily plots were constructed for each participant that provided a visual display of average activity counts per hour and an indication of which hours the monitor was being worn, according to the participant's log. Our SAS program also generated printouts for each day of monitoring that listed the activity counts for each minute of the day, and whether the activity monitor was being worn, according to the log data. Visual inspection of these outputs was used to help identify monitor malfunctions and data entry errors or omissions. For example, negative numbers sporadically occurring throughout a file indicated a monitor malfunction. Similarly, zeroes occurring during times where it was confirmed that the monitor was being worn continuously during activity (e.g., during the 400-m walk) also indicated monitor malfunction. All spurious data were considered to be missing.
In addition to recording monitor “on” and “off” times, participants used the logs to document reasons for not wearing the monitor (e.g., forgetfulness, broken attachment clip, illness, etc.). Further, if a participant failed to document monitor “on” and “off” times, the associated day was treated as missing data.
Days on which the participant did not wear the monitor for at least 10 hours were eliminated from analysis (wearing time did not have to be continuous). A minimum of 5 days of recording was required to estimate per day averages of the accelerometry variables. Previous work in this area suggests that 3–4 days of monitoring in adults is sufficient to achieve 80% reliability for moderate or higher intensity physical activity (Matthews, Ainsworth, Thompson, & Bassett, 2002).
Statistical analysis
Data are presented as means ± SD, except where noted. Group differences in selected baseline characteristics were evaluated using t-tests. Descriptive statistics were used to summarize the practicality and compliance with the accelerometry protocol. T-tests were also employed to determine the capability of the accelerometry-derived variables to distinguish a difference in activity level between the PA and SA arms. As this was exploratory research, adjustments for multiple comparisons were not made. Spearman correlation coefficients were computed to evaluate convergent validity of accelerometry with the CHAMPS physical activity questionnaire.
RESULTS
Participant characteristics
Baseline characteristics of the 106 study participants are presented in Table 1. The group ranged in age from 70 to 86 years, with 67% women and 23% representing racial/ethnic minorities. Almost two-thirds of the group (62%) had achieved some level of college education. Self-reported health conditions included hypertension (70%), diabetes (26%), cancer (25%), myocardial infarction (9%), congestive heart failure (7%), and stroke (6%). The average SPPB score was 7.4 (0 = unable to complete all three components of the battery; 12 = highest level of performance), with 45% having a score ≤ 7. A low SPPB score has been shown to be predictive of increased risk of mobility disability in initially non-disabled older adults (Guralnik et al., 2000; Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995). Over half of the group (57%) reported difficulty in walking ¼ mile without stopping to rest. There were no between group differences in baseline characteristics.
Table 1.
Participant characteristics at baseline
| Physical Activity (N = 54) |
Successful Aging (N = 52) |
|||
|---|---|---|---|---|
| Characteristic | Mean ± SD or Percentage | Range | Mean ± SD or Percentage | Range |
| Age (years) | 77.6 ± 4.0 | 71 – 86 | 77.3 ± 4.5 | 70 – 85 |
| Weight (kg) | 85.7 ± 19.4 | 55 – 148 | 84.0 ± 18.4 | 47 – 157 |
| Height (cm) | 163.3 ± 10.6 | 142 – 188 | 164.9 ± 9.8 | 149 – 195 |
| BMI (kg·m−2) | 32.0 ± 5.7 | 21 – 44 | 30.7 ± 4.9 | 21 – 44 |
| Female N (%) | 36 (67%) | 35 (67%) | ||
| Race/Ethnicity N (%) | ||||
| White | 44 (83%) | 38 (73%) | ||
| African American | 2 (4%) | 8 (15%) | ||
| Latino, Hispanic or Spanish | 7 (13%) | 4 (8%) | ||
| Other | 1 (2%) | 2 (4%) | ||
| Physical function | ||||
| Short Physical Performance Battery (SPPB) score | 7.3 ± 1.8 | 2 – 9 | 7.4 ± 1.5 | 4 – 9 |
| SPPB score ≤ 7 N (%) | 25 (46%) | 23 (44%) | ||
| 400-m walk speed (m·sec−1) | 0.77 ± 0.20 | 0.45 – 1.22 | 0.80 ± 0.15 | 0.49 – 1.11 |
| Frequency of all activities per wk† | 11.8 ± 7.4 | 0 – 30 | 13.7 ± 9.0 | 1 – 36 |
| Frequency of moderate PA per wk† | 2.3 ± 3.5 | 0 – 15 | 3.0 ± 4.0 | 0 – 13 |
| Calories spent in all activities per wk† | 1860.7 ± 1490.8 | 0 – 5897 | 2178.8 ± 2090.4 | 111 – 10934 |
| Calories spent in moderate PA per wk† | 561.3 ± 893.9 | 0 – 4494 | 659.3 ± 1217.8 | 0 – 7775 |
| MET-hrs per wk (all activities)† | 21.2 ± 16.3 | 0 – 75 | 25.1 ± 22.3 | 1 – 96 |
| MET-hrs per wk (moderate PA)† | 6.1 ± 9.3 | 0 – 43 | 7.6 ± 12.6 | 0 – 68 |
From CHAMPS questionnaire
BMI = body mass index
PA = physical activity
Practicality of and compliance with using the ActiGraph
Factors related to the practicality of the accelerometer and compliance with the protocol were categorized as either monitor-related or participant-related factors. Monitor-related factors included unit malfunction and unit attachment issues. Of the 106 study participants, 3 experienced monitor malfunction resulting in a loss of 21 days of data. Four participants had problems with monitor attachment (e.g., monitor kept falling off, broken clip, etc.), resulting in a loss of 10 days of data. Participant-related factors included incomplete logs and not wearing the monitor. Eighteen participants (17%) submitted incomplete logs equivalent to a loss of 37 days of monitoring. Three participants did not wear the monitor daily per protocol for a variety of reasons (e.g., illness, vacationing, etc.), resulting in a loss of 6 days of data. Overall, 742 days of monitoring were possible (106 participants × 7 days), with monitor and participant-related factors accounting for an overall loss of 74 days, or approximately 10% of possible data. In general, the monitors were well tolerated with only one participant reporting the unit to be “uncomfortable.”
Capability of accelerometry variables and an individualized activity count threshold to differentiate activity levels between the PA and SA arms
Of the 106 participants enrolled in the sub-study, 3 experienced a monitor malfunction, 1 did not meet the criterion for number of days worn, 4 did not meet minimum requirements for hours worn per day, and 5 did not provide 400 m walk data sufficient to calculate individualized count thresholds. As a result, 93 participants (88%) were evaluated. Data were collected at the 6-month time-point for 80 participants and at the 12-month time-point for 13 participants (n = 5 PA arm; n = 8 SA arm).
Accelerometry variables are provided in Table 2. The arms were similar in terms of average hours per day the monitor was worn and average activity counts per hour, however, the SA arm wore the monitor for more days (6.8 days) compared to the PA arm (6.5 days, p = 0.02). The analytic sample displayed considerable variability in THRESHIND despite the fact that the 400m walk pace was restricted in terms of permitted perceived intensity level (i.e., “light” to “somewhat hard”). Physical exertion scores reported during the 400m walk were (mean ± SD) 1.56 ± 0.65 with an average 400m walk speed of 0.81 ± 0.19 m·sec−1. This was associated with a 400-m walk time of 9.1 ± 2.2 minutes, with a range of 5.5 to 15.0 minutes. No significant arm differences in perceived exertion (4 point scale) or walk speed were found for 6- and 12-month participants, thus data from the two time points were combined for reporting. At the conclusion of the walk, a subset of participants (n = 51) were queried using the Borg 15-point scale and reported an average rating of perceived exertion (RPE) of 11.8 ± 2.1. Despite a similarity in THRESHIND between arms during the 400-m walk, there was a trend toward more time spent above the THRESHIND in the PA arm (18.5 ± 27.2 min·day−1) compared to the SA arm (11.0 ± 11.4 min·day−1, p = 0.08). In addition, the PA group significantly exceeded the SA group in terms of mean activity counts above THRESHIND, and in number of bouts ≥ 10 min above THRESHIND.
Table 2.
Accelerometry and CHAMPS variables by group (mean ± SD)**
| Physical Activity (N = 50) |
Successful Aging (N = 43) |
|||||
|---|---|---|---|---|---|---|
| Mean ± SD | Range | Mean ± SD | Range | P value | ES | |
| Accelerometry variables | ||||||
| Number of days worn | 6.5 ± 0.8 | 5 – 7 | 6.8 ± 0.5 | 5 – 7 | 0.02 | 0.47 |
| Hours worn per day | 14.4 ± 1.3 | 12.0 – 17.2 | 14.5 ± 1.1 | 12.1 – 18.0 | 0.76 | 0.06 |
| Activity counts per hour | 8363.4 ± 4250.7 | 1236.0 – 21735.6 | 7474.0 ± 3601.6 | 1539.8 – 15460.6 | 0.28 | 0.23 |
| Activity counts per day | 119,927.4 ± 60501.7 | 18,268 – 272,302.3 | 107,463.8 ± 51361.3 | 22407 – 224,988 | 0.29 | 0.22 |
| ThreshIND (counts·min−1) | 1498.3 ± 726.2 | 149.3 – 3132.8 | 1407.0 ± 634.9 | 214.3 – 2843.3 | 0.52 | 0.13 |
| Time spent above ThreshIND (min·d−1) | 18.5 ± 27.2 | 0.6 – 165 | 11.0 ± 11.4 | 0.4 – 55.6 | 0.08 | 0.36 |
| Activity counts above ThreshIND (counts·d−1) | 28,100.9 ± 27,520.5 | 767.2 – 120,050.1 | 17,234.2 ± 15,619.5 | 1213.3 – 86,834.7 | 0.02 | 0.49 |
| Number of activity bouts ≥ 10 min above ThreshIND (bouts·d−1) | 1.1 ± 2.0 | 0 – 12.2 | 0.5 ± 0.8 | 0 – 4.0 | 0.05 | 0.40 |
| CHAMPS variables * | ||||||
| Calories spent (all activities) | 2788.2 ± 1880.9 | 0 – 8577.2 | 2155.1 ± 1662.1 | 0 – 8334.5 | 0.09 | 0.36 |
| Calories spent (mod+ activities) | 950.1 ± 1132.9 | 0 – 4374.2 | 565.4 ± 1066.7 | 0 – 5192.0 | 0.10 | 0.35 |
| MET-hours·wk−1 (all activities) | 31.7 + 20.9 | 0 – 96 | 23.8 + 16.9 | 0 – 76 | 0.05 | 0.41 |
| MET-hours·wk−1 (mod+ activities) | 11.1 + 13.7 | 0 - 53.6 | 6.0 + 10.5 | 0 – 47.5 | 0.05 | 0.42 |
| Frequency (all activities) | 16.4 ± 8.5 | 0 – 38 | 13.3 ± 7.3 | 0 – 41 | 0.06 | 0.39 |
| Frequency (mod+ activities) | 4.1 ± 4.3 | 0 – 18 | 2.3 ± 3.4 | 0 – 12 | 0.02 | 0.48 |
ThreshIND = individualized activity count threshold
mod+ activities = activities of a moderate intensity level or greater
CHAMPS = Community Healthy Activities Model Program for Seniors questionnaire
ES = effect size
N = 49 PA
Includes data from 6- (n=80) and 12-month (n=13) time points
Relationship between accelerometry variables and a physical activity questionnaire for older adults (CHAMPS)
Mean activity counts per day were positively correlated with all CHAMPS-derived variables (Table 3). Accelerometry variables using the THRESHIND showed no significant correlation to CHAMPS variables, with the exception of a positive correlation between activity counts above THRESHIND and calories expended in all activities (r = 0.25, p ≤ 0.05).
Table 3.
Physical activity self-report (CHAMPS Questionnaire) and accelerometry variables: Spearman correlations (N = 91)
| Accelerometry Variables | ||||
|---|---|---|---|---|
| CHAMPS Variables | Activity counts·hr−1 | Time spent above THRESHIND (min·d−1) | Activity counts above THRESHIND(counts·d−1) | Number of bouts ≥ 10 min above THRESHIND per day |
| Calories expended (all activities) | 0.42*** | 0.08 | 0.25* | 0.13 |
| Calories expended (mod+ activities) | 0.31** | 0.04 | 0.16 | 0.09 |
| Frequency of all activities | 0.33** | 0.10 | 0.19 | 0.17 |
| Frequency of mod+ activities | 0.27** | 0.03 | 0.14 | 0.08 |
p < 0.05,
p < 0.01,
p < 0.0001
DISCUSSION
It is important to note that one of the overarching goals of this exploratory research was to determine whether actigraphy, using the methods described, held promise for assessing physical activity (specifically walking behavior) in older adults. Toward that end, analyses were not intention to treat and P values produced by t-tests were not adjusted for multiple comparisons. Thus, our results should be viewed as those of an exploratory, pilot study.
One of the specific aims of this pilot study was to evaluate the practicality of the ActiGraph for use in a naturalistic environment with older adults at risk for mobility disability. To date, most accelerometer studies have been conducted in controlled, supervised and/or laboratory settings; (Brage, Wedderkopp, Franks, Andersen, & Froberg, 2003; Freedson et al., 1998; Melanson & Freedson, 1995; Nichols et al., 2000) thus, they have not directly addressed the issue of practicality. Our results suggest that the ActiGraph is a viable way to collect objective physical activity data in a free-living environment with older, functionally limited adults; only 10% of the data were not available for use due to monitor- and participant-related factors. In addition, compliance to the protocol was good with only 5 participants excluded for not meeting requirements for the number of days and/or hours per day that the monitor was worn. While “usable data” may constitute only one aspect of the practicality of an instrument, our findings are promising given a protocol that required older adults to wear a monitor for 7 consecutive days while keeping concurrent logs. A similar level of compliance was reported by Davis et al. (2006) in an accelerometry study of 203 adults ≥ 70 years old with protocol and log requirements comparable to the present study. They report retaining 80% of participants after accounting for monitor malfunction, participant-related factors, and data inclusion criteria. This compares favorably to our observation that 87% of participants provided usable data for the present study.
Our findings provide preliminary insight regarding the capability of the ActiGraph worn at the hip to detect a significant difference in the physical activity level between participants assigned to a PA group versus a SA health education intervention. We found that accelerometry variables related to individualized thresholds were more effective than accelerometry variables of overall activity (e.g., activity counts·day−1) in differentiating activity levels in this group of older adults. The ability to detect group differences using this individualized approach may prove useful in determining the efficacy of interventions aimed at increasing PA in older adults. Furthermore, it may serve as an indication of whether PA recommendations, based on relative intensity levels have been met.
The lack of significant group difference in overall measures of activity may have been partially attributed to the relative large variances associated with these measures. Matthews et al. (2007) found accelerometry to be effective differentiating groups in response to a 12-wk walking intervention in breast cancer survivors (n=23) aged > 45 years. They reported a significantly greater change in overall activity (activity counts·min−1·day−1) for the PA group (72.2 ± 114.6) compared to a control group (−16.8 ± 51.5, p = 0.01). Intensity-related accelerometry variables (i.e., mean change in time spent in moderate activity) reached marginal significance (9.4 ± 12 min PA vs 1.9 ± 6.7 min control; p=0.07).
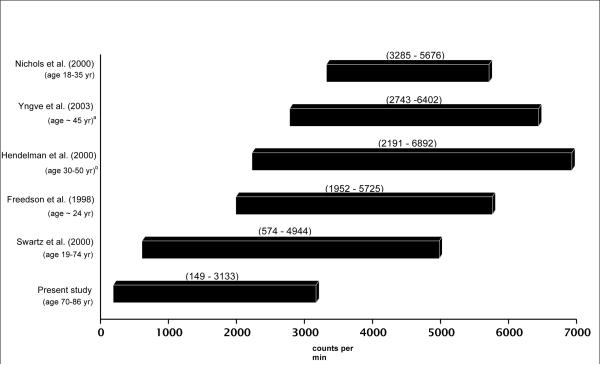
We conducted an “individualized calibration” of participants in order to determine an activity count threshold associated with walking at a usual to brisk pace that was representative of meaningful activity for our analytic sample. The 400m walk test was designed to limit intensity to less than or equal to “somewhat hard.” This relatively narrow range in relative intensity during the 400-m walk produced a wide range of individualized activity count thresholds (149 to 3133 counts·min−1). The observed variability in activity count thresholds may have been at least partially associated with the variability in 400-m walking speed. During post-hoc analysis, we found a significant correlation between walk speed and individualized activity count threshold (r = 0.67, p < 0.0001). Further, altered gait patterns often observed in older adults and/or variability in walking mechanics may have also contributed to the variability in individualized activity count thresholds (Bianchi, Angelini, & Lacquaniti, 1998; Gabell & Nayak, 1984; Herman, Giladi, Gurevich, & Hausdorff, 2005; McGibbon & Krebs, 2001).
Individualized thresholds indicative of “meaningful” activity proved valuable in identifying group differences in activity level in our sample of older adults, whereas the application of published accelerometry cut points associated with beneficial health outcomes (i.e., moderate-intensity PA) may have lead to misleading conclusions. Figure 1 displays an array of moderate-intensity cut points developed in adults along with the range of values from the present study. This figure highlights the considerable span of values associated with moderate-intensity activity both within and across studies. Furthermore, with the exception of the cut point range reported by Swartz et al. (2000), the overlap of our “meaningful activity” range with the moderate-intensity ranges of other published studies is minimal. Thus, the application of such cut points to data in the present study would have compromised our ability to detect important group differences in meaningful activity. Our results support published findings that the choice of cut point threshold has a considerable impact on outcomes related to time spent engaging in activity thought to promote health (Ham, Reis, Strath, Dubose, & Ainsworth, 2007; Matthews, 2005; Strath, Bassett, & Swartz, 2003). It may be that such values are most effective when derived in a group performing activities that are most similar to the analytic sample in which they will be applied. Given the lack of consistent intensity cut point values, an individualized approach to determining intensity-related thresholds appears to be a reasonable method to use for older adults with compromised physical function. Recent work in middle-aged adults show that an individualized calibration approach with accelerometry strengthens the association with over-ground walking speed and improves the prediction of free-living walking speed using accelerometry (Barnett & Cerin, 2006).
Figure 1.
ActiGraph activity count ranges associated with moderate intensity activity in adults
Note: numbers in parentheses represent activity count ranges
atrack walking; bbased on walking only equation
The accelerometer-based overall measure of activity (activity counts·d−1) was modestly correlated with CHAMPS measures of overall activity (calories expended in all activities, frequency of all activities), and CHAMPS intensity-related measures (calories expended in mod+ activities, frequency of mod+ activities). No significant association was found between intensity-related accelerometry measures and measures of moderate-intensity activity from the CHAMPS questionnaire (calories expended in mod+ activities, frequency of mod+ activities). This suggests that the activities captured using the individualized threshold are somewhat different than those captured as overall counts per day. The lack of association between measures with regard to intensity may be due to the fact that these instruments do not measure the same activity patterns. The CHAMPS items that comprise the mod+ intensity score are much more varied (e.g., housework, gardening, light strength-training) than the prime activity (walking) that would have contributed to counts exceeding the accelerometer-based individualized threshold. Given the lack of a definitive criterion with which to evaluate time spent at different intensities (LaMonte, Ainsworth, & Tudor-Locke, 2003), a prudent approach may be to include both self-report and objective measures of PA when attempting to characterize activity patterns.
This investigative, cross-sectional study included 6- and 12-month (n = 13) participants. This may have introduced selection bias or self-report differences with regard to the CHAMPS questionnaire. However, the influence of these factors on our primary aims is likely low, although cannot be completely discounted. Data collection time point in this cross-sectional study is not likely to significantly influence compliance and practicality issues, nor should it play a major role in the establishment of an individualized accelerometry cut-point or its use in subsequent analyses. It is possible that the 12-month participants may have been more accurate in their self-report of PA using the CHAMPS, by having completed the measure twice, whereas the 6-month participants had completed the CHAMPS at least once (at baseline). The relatively long time span between assessments (6 months) may have mitigated the chance of a repeated exposure to the CHAMPS having a strong influence on the CHAMPS vs accelerometry relationship in this group of older adults. The inclusion 12-month participants may have actually reduced the ability to determine between-arm differences using the ActiGraph in that exercise classs participation rates actually declined in the PA group from 70.7% during the early part LIFE-P study, to 60.9% during the latter stages of the study (Pahor et al., 2006).
Despite several methodological limitations, the present study provides preliminary evidence that accelerometry is a viable means of measuring PA in older adults at risk of mobility disability. Accelerometry was effective in differentiating PA levels between groups, particularly when applying individualized thresholds to identify activity relevant to beneficial health outcomes. In light of the emerging importance of light- to moderate-intensity PA to overall energy expenditure and health benefits (Abbott et al., 2004; Manini et al., 2006; Pescatello, Murphy, & Costanzo, 2000; Weuve et al., 2004), the identification of such activity is warranted, especially in older adult populations with low physical functioning. The individualized threshold proved useful for this group, whereas the application of published cut-points, primarily derived in younger populations, would likely have resulted in a misrepresentation of activity profiles in the present sample of older adults. Convergent validity with the CHAMPS questionnaire was modest using overall activity accelerometry values and low using accelerometry variables related to intensity. This suggests that the intensity-related variables of the two measures may be capturing different activity profiles and highlights the importance of further work in this area. Accelerometry can provide valuable objective data with regard to duration and intensity of activity. The development and validation of creative strategies (and further validation of this approach) with regard to intensity-related cut-points is central to optimizing its use among older, somewhat frail adults.
ACKNOWLEDGEMENTS
The Lifestyle Interventions and Independence for Elders (LIFE-P) Pilot Study was funded by a National Institutes on Health/National Institute on Aging Cooperative Agreement (#U01 AG22376) and sponsored in part by the Intramural Research Program, National Institute on Aging, NIH. This sub-study was supported in part by the Intramural Research Program, National Institute on Aging, NIH. We would also like to acknowledge Dr. David K. Ahn for his statistical analysis and programming contributions to this project and Ann Varady for her programming expertise.
Appendix: Research Investigators for Pilot Phase of LIFE
Cooper Institute, Dallas, TX
Steven N. Blair, P.E.D. – Field Center Principal Investigator
Timothy Church, M.D., Ph.D., M.P.H. – Field Center Co-Principal Investigator
Jamile A. Ashmore, Ph.D.
Judy Dubreuil, M.S.
Georita Frierson, Ph.D.
Alexander N. Jordan, M.S.
Gina Morss, M.A.
Ruben Q. Rodarte, M.S.
Jason M. Wallace, M.P.H.
National Institute on Aging
Jack M. Guralnik, M.D., Ph.D. – Co-Principal Investigator of the Study
Evan C. Hadley, M.D.
Sergei Romashkan, M.D., Ph.D.
Stanford University, Palo Alto, CA
Abby C. King, Ph.D. – Field Center Principal Investigator
William L. Haskell, Ph.D. – Field Center Co-Principal Investigator
Leslie A. Pruitt, Ph.D.
Kari Abbott-Pilolla, M.S.
Karen Bolen, M.S.
Stephen Fortmann, M.D.
Ami Laws, M.D.
Carolyn Prosak, R.D.
Kristin Wallace, M.P.H.
Tufts University
Roger Fielding, Ph.D.
Miriam Nelson, Ph.D.
Dr. Fielding's contribution is partially supported by the U.S. Department of Agriculture, under agreement No. 58-1950-4-401. Any opinions, findings, conclusion, or recommendations expressed in this publication are those of the author(s) and do not necessarily reflect the view of the U.S. Dept of Agriculture.
University of California, Los Angeles, Los Angeles, CA
Robert M. Kaplan, Ph.D., M.A.
VA San Diego Healthcare System and University of California, San Diego, San Diego, CA
Erik J. Groessl, Ph.D.
University of Florida, Gainesville, FL
Marco Pahor, M.D. – Principal Investigator of the Study
Michael Perri, Ph.D.
Connie Caudle
Lauren Crump, M.P.H
Sarah Hayden
Latonia Holmes
Cinzia Maraldi, M.D.
Crystal Quirin
Dr. Pahor is partially supported by the Geriatric Research, Education and Clinical Center (GRECC) of the Malcom Randall Veteran's Affairs Medical Center, North Florida/South Georgia Veterans Health System, Gainesville, FL.
University of Pittsburgh, Pittsburgh, PA
Anne B. Newman, M.D., M.P.H. – Field Center Principal Investigator
Stephanie Studenski, M.D., M.P.H. – Field Center Co-Principal Investigator
Bret H. Goodpaster, Ph.D., M.S.
Nancy W. Glynn, Ph.D.
Erin K. Aiken, B.S.
Steve Anthony, M.S.
Sarah Beck (for recruitment papers only)
Judith Kadosh, B.S.N., R.N.
Piera Kost, B.A.
Mark Newman, M.S.
Jennifer Rush, M.P.H. (for recruitment papers only)
Roberta Spanos (for recruitment papers only)
Christopher A. Taylor, B.S.
Pam Vincent, C.M.A.
The Pittsburgh Field Center was partially supported by the Pittsburgh Claude D. Pepper Center P30 AG024827.
Wake Forest University, Winston-Salem, NC
Stephen B. Kritchevsky, Ph.D. – Field Center Principal Investigator
Peter Brubaker, Ph.D.
Jamehl Demons, M.D.
Curt Furberg, M.D., Ph.D.
Jeffrey A. Katula, Ph.D., M.A.
Anthony Marsh, Ph.D.
Barbara J. Nicklas, Ph.D.
Jeff D. Williamson, M.D., M.P.H.
Rose Fries, L.P.M.
Kimberly Kennedy
Karin M. Murphy, B.S., M.T. (ASCP)
Shruti Nagaria, M.S.
Katie Wickley-Krupel, M.S.
Data Management, Analysis and Quality Control Center (DMAQC)
Michael E. Miller, Ph.D. – DMAQC Field Principal Investigator
Mark Espeland, Ph.D. – DMAQC Co-Principal Investigator
Fang-Chi Hsu, Ph.D.
Walter J. Rejeski, Ph.D.
Don P. Babcock, Jr., P.E.
Lorraine Costanza
Lea N. Harvin
Lisa Kaltenbach, M.S.
Wei Lang, Ph.D.
Wesley A. Roberson
Julia Rushing, M.S.
Scott Rushing
Michael P. Walkup, M.S.
The Wake Forest University Field Center is, in part, supported by the Claude D. Older American Independence Pepper Center #1 P30 AG21332.
Yale University
Thomas M. Gill, M.D.
Dr. Gill is the recipient of a Midcareer Investigator Award in Patient-Oriented Research (K24AG021507) from the National Institute on Aging.
The Lifestyle Interventions and Independence for Elders (LIFE-P) Pilot Study is funded by a National Institutes on Health/National Institute on Aging Cooperative Agreement #UO1 AG22376 and sponsored in part by the Intramural Research Program, National Institute on Aging, NIH.
References
- Abbott RD, White LR, Ross GW, Masaki KH, Curb JD, Petrovitch H. Walking and dementia in physically capable elderly men. Journal of the American Medical Association. 2004;292(12):1447–1453. doi: 10.1001/jama.292.12.1447. [DOI] [PubMed] [Google Scholar]
- Avlund K, Vass M, Hendriksen C. Onset of mobility disability among community-dwelling old men and women. The role of tiredness in daily activities. Age and Aging. 2003;32(6):579–584. doi: 10.1093/ageing/afg101. [DOI] [PubMed] [Google Scholar]
- Baranowski T. Validity and reliability of self-report of physical activity: An information processing perspective. Research Quarterly for Exercise and Sport. 1988;59:314–327. [Google Scholar]
- Barnett A, Cerin E. Individual calibration for estimating free-living walking speed using the MTI monitor. Medicine and Science in Sports and Exercise. 2006;38(4):761–767. doi: 10.1249/01.mss.0000210206.55941.b2. [DOI] [PubMed] [Google Scholar]
- Bianchi L, Angelini D, Lacquaniti F. Individual characteristics of human walking mechanics. Pflugers Archiv European Journal of Physiology. 1998;436(3):343–356. doi: 10.1007/s004240050642. [DOI] [PubMed] [Google Scholar]
- Boon H, Frisard M, Brown C, Jazwinski S, DeLany J, Ravussin E. Validation of accelerometers to assess physical activity in elderly subjects. Obes Res. 2003;11:A8. [Google Scholar]
- Borg GA. Psychophysical bases of perceived exertion. Medicine and Science in Sports and Exercise. 1982;14(5):377–381. [PubMed] [Google Scholar]
- Brage S, Wedderkopp N, Franks PW, Andersen LB, Froberg K. Reexamination of validity and reliability of the CSA monitor in walking and running. Medicine and Science in Sports and Exercise. 2003;35(8):1447–1454. doi: 10.1249/01.MSS.0000079078.62035.EC. [DOI] [PubMed] [Google Scholar]
- Buchner DM, Beresford SA, Larson EB, LaCroix AZ, Wagner EH. Effects of physical activity on health status in older adults. II. Intervention studies. Annual Review of Public Health. 1992;13:469–488. doi: 10.1146/annurev.pu.13.050192.002345. [DOI] [PubMed] [Google Scholar]
- Davis MG, Fox KR. Physical activity patterns assessed by accelerometry in older people. European Journal of Applied Physiology. 2006 doi: 10.1007/s00421-006-0320-8. DOI: 10.1007/s00421-006-0320-8. [DOI] [PubMed] [Google Scholar]
- Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. American Journal of Geriatric Psychiatry. 2006;14(1):6–20. doi: 10.1097/01.JGP.0000192501.03069.bc. [DOI] [PubMed] [Google Scholar]
- Focht BC, Sanders WM, Brubaker P, Rejeski WJ. Initial validation of the CSA activity monitor during rehabilitative exercise among older adults with chronic disease. Journal of Aging and Physical Activity. 2003;11:293–304. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Medicine and Science in Sports and Exercise. 1998;30(5):777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Fried LP, Guralnik JM. Disability in older adults: evidence regarding significance, etiology, and risk. Journal of the American Geriatrics Society. 1997;45(1):92–100. doi: 10.1111/j.1532-5415.1997.tb00986.x. [DOI] [PubMed] [Google Scholar]
- Gabell A, Nayak US. The effect of age on variability in gait. Journal of Gerontology. 1984;39(6):662–666. doi: 10.1093/geronj/39.6.662. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Pieper CF, Leveille SG, Markides KS, Ostir GV, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2000;55(4):M221–231. doi: 10.1093/gerona/55.4.m221. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. New England Journal of Medicine. 1995;332(9):556–561. doi: 10.1056/NEJM199503023320902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology. 1994;49(2):M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Ham SA, Reis JP, Strath SJ, Dubose KD, Ainsworth BE. Discrepancies between methods of identifying objectively determined physical activity. Medicine and Science in Sports and Exercise. 2007;39(1):52–58. doi: 10.1249/01.mss.0000235886.17229.42. [DOI] [PubMed] [Google Scholar]
- Harada ND, Chiu V, King AC, Stewart AL. An evaluation of three self-report physical activity instruments for older adults. Medicine and Science in Sports and Exercise. 2001;33(6):962–970. doi: 10.1097/00005768-200106000-00016. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–1093. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- Hendelman D, Miller K, Baggett C, Debold E, Freedson P. Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Medicine and Science in Sports and Exercise. 2000;32(9 Suppl):S442–449. doi: 10.1097/00005768-200009001-00002. [DOI] [PubMed] [Google Scholar]
- Herman T, Giladi N, Gurevich T, Hausdorff JM. Gait instability and fractal dynamics of older adults with a “cautious” gait: why do certain older adults walk fearfully? Gait and Posture. 2005;21(2):178–185. doi: 10.1016/j.gaitpost.2004.01.014. [DOI] [PubMed] [Google Scholar]
- Hirvensalo M, Rantanen T, Heikkinen E. Mobility difficulties and physical activity as predictors of mortality and loss of independence in the community-living older population. Journal of the American Geriatrics Society. 2000;48(5):493–498. doi: 10.1111/j.1532-5415.2000.tb04994.x. [DOI] [PubMed] [Google Scholar]
- King AC, Baumann K, O'Sullivan P, Wilcox S, Castro C. Effects of moderate-intensity exercise on physiological, behavioral, and emotional responses to family caregiving: a randomized controlled trial. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2002;57(1):M26–36. doi: 10.1093/gerona/57.1.m26. [DOI] [PubMed] [Google Scholar]
- King AC, Pruitt LA, Phillips W, Oka R, Rodenburg A, Haskell WL. Comparative effects of two physical activity programs on measured and perceived physical functioning and other health-related quality of life outcomes in older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2000;55(2):M74–83. doi: 10.1093/gerona/55.2.m74. [DOI] [PubMed] [Google Scholar]
- LaMonte MJ, Ainsworth BE, Tudor-Locke C. Assessment of physical activity and energy expenditure. In: Andersen RE, editor. Obesity: Etiology, Assessment, Treatment and Prevention. Human Kinetics; Champaign, IL: 2003. pp. 111–137. [Google Scholar]
- Manini TM, Everhart JE, Patel KV, Schoeller DA, Colbert LH, Visser M, et al. Daily activity energy expenditure and mortality among older adults. Journal of the American Medical Association. 2006;296(2):171–179. doi: 10.1001/jama.296.2.171. [DOI] [PubMed] [Google Scholar]
- Matthews CE. Calibration of accelerometer output for adults. Medicine and Science in Sports and Exercise. 2005;37:S512–S522. doi: 10.1249/01.mss.0000185659.11982.3d. [DOI] [PubMed] [Google Scholar]
- Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr. Sources of variance in daily physical activity levels as measured by an accelerometer. Medicine and Science in Sports and Exercise. 2002;34(8):1376–1381. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- Matthews CE, Wilcox S, Hanby CL, Der Ananian C, Heiney SP, Gebretsadik T, et al. Evaluation of a 12-week home-based walking intervention for breast cancer survivors. Supportive Care in Cancer. 2007;15:203–211. doi: 10.1007/s00520-006-0122-x. [DOI] [PubMed] [Google Scholar]
- McGibbon CA, Krebs DE. Age-related changes in lower trunk coordination and energy transfer during gait. Journal of Neurophysiology. 2001;85(5):1923–1931. doi: 10.1152/jn.2001.85.5.1923. [DOI] [PubMed] [Google Scholar]
- Melanson EL, Jr., Freedson PS. Validity of the Computer Science and Applications, Inc. (CSA) activity monitor. Medicine and Science in Sports and Exercise. 1995;27(6):934–940. [PubMed] [Google Scholar]
- Melanson EL, Jr., Freedson PS. Physical activity assessment: a review of methods. Critical Reviews in Food Science and Nutrition. 1996;36(5):385–396. doi: 10.1080/10408399609527732. [DOI] [PubMed] [Google Scholar]
- Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- Nichols JF, Morgan CG, Chabot LE, Sallis JF, Calfas KJ. Assessment of physical activity with the Computer Science and Applications, Inc., accelerometer: laboratory versus field validation. Research Quarterly for Exercise and Sport. 2000;71(1):36–43. doi: 10.1080/02701367.2000.10608878. [DOI] [PubMed] [Google Scholar]
- Pahor M, Blair SN, Espeland M, Fielding R, Gill TM, Guralnik JM, et al. Effects of a physical activity intervention on measures of physical performance: Results of the lifestyle interventions and independence for Elders Pilot (LIFE-P) study. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2006;61(11):1157–1165. doi: 10.1093/gerona/61.11.1157. [DOI] [PubMed] [Google Scholar]
- Pescatello LS, Murphy D, Costanzo D. Low-intensity physical activity benefits blood lipids and lipoproteins in older adults living at home. Age Ageing. 2000;29(5):433–439. doi: 10.1093/ageing/29.5.433. [DOI] [PubMed] [Google Scholar]
- Rejeski WJ, Fielding RA, Blair SN, Guralnik JM, Gill TM, Hadley EC, et al. The lifestyle interventions and independence for elders (LIFE) pilot study: design and methods. Contemporary Clinical Trials. 2005;26(2):141–154. doi: 10.1016/j.cct.2004.12.005. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Medicine and Science in Sports and Exercise. 2001;33(7):1126–1141. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- Stewart AL, Verboncoeur CJ, McLellan BY, Gillis DE, Rush S, Mills KM, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences. 2001;56(8):M465–470. doi: 10.1093/gerona/56.8.m465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strath SJ, Bassett DR, Jr., Swartz AM. Comparison of MTI accelerometer cut-points for predicting time spent in physical activity. International Journal of Sports Medicine. 2003;24(4):298–303. doi: 10.1055/s-2003-39504. [DOI] [PubMed] [Google Scholar]
- Swartz AM, Strath SJ, Bassett DR, Jr., O'Brien WL, King GA, Ainsworth BE. Estimation of energy expenditure using CSA accelerometers at hip and wrist sites. Medicine and Science in Sports and Exercise. 2000;32(9 Suppl):S450–456. doi: 10.1097/00005768-200009001-00003. [DOI] [PubMed] [Google Scholar]
- Van Den Brink CL, Van Den Bos GA, Tijhuis M, Aijanseppa S, Nissinen A, Giampaoli S, et al. Hierarchy levels, sum score, and worsening of disability are related to depressive symptoms in elderly men from three European countries. Journal of Aging and Health. 2006;18(1):125–141. doi: 10.1177/0898264305280988. [DOI] [PubMed] [Google Scholar]
- Waldrop J, Stern SM. Disability Status: 2000. U.S. Census Bureau, Census 2000 Brief Series. C2KBR-17. U.S. Department of Commerce; Washington, DC: 2003. [Google Scholar]
- Wannamethee SG, Ebrahim S, Papacosta O, Shaper AG. From a postal questionnaire of older men, healthy lifestyle factors reduced the onset of and may have increased recovery from mobility limitation. Journal of Clinical Epidemiology. 2005;58(8):831–840. doi: 10.1016/j.jclinepi.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Washburn RA, Jette AM, Janney CA. Using age-neutral physical activity questionnaires in research with the elderly. Journal of Aging and Health. 1990;2:341–356. [Google Scholar]
- Weuve J, Kang JH, Manson JE, Breteler MM, Ware JH, Grodstein F. Physical activity, including walking, and cognitive function in older women. Journal of the American Medical Association. 2004;292(12):1454–1461. doi: 10.1001/jama.292.12.1454. [DOI] [PubMed] [Google Scholar]
- Yngve A, Nilsson A, Sjostrom M, Ekelund U. Effect of monitor placement and of activity setting on the MTI accelerometer output. Medicine and Science in Sports and Exercise. 2003;35(2):320–326. doi: 10.1249/01.MSS.0000048829.75758.A0. [DOI] [PubMed] [Google Scholar]