Abstract
Background
Prostate cancer is the most common type of cancer among men.
Objectives
To investigate the trace elements (Se, Zn, Cu and Cd) and vitamin E status of some Nigerian prostate cancer (PCa) patients relative to their prostate-specific antigen (PSA) values.
Methods
Prostate cancer patients were assigned into groups 1, 2 and 3 with PSA of 5–10 ng/ml, 11–20 ng/ml and > 20 ng/ml, respectively.
Results
The results showed that the levels of whole blood superoxide dismutase (SOD) and serum Se and Zn were significantly lower (p< 0.05) in the PCa patients. Specifically, levels of SOD, Se and Zn decreased by 67%, 30% and 35%; 70%, 52% and 41%; 81%, 58% and 47%, in subjects with PSA of 5–10 ng/ml, 11–20 ng/ml and > 20 ng/ml, respectively. There were no significant differences (p> 0.05) in levels of Cu and Cd. Serum Cu/ Zn ratio were significantly higher in PCa patients. The Cu/ Zn ratios were 1: 1.2: 1.3 for subjects in groups 1, 2 and 3, respectively. Vitamin E levels in PCa patients were significantly lower and followed the order; normal > PSA (5–10) > PSA (11–20) > PSA (> 20).
Conclusions
Deficiency of vitamin E, Zn and Se may be risk factors for development of PCa.
Key words: Lipid peroxidation, Prostate cancer, PSA values, Trace elements, Vitamin E
Introduction
In the United States, prostate cancer is the most commonly diagnosed cancer in men and the second leading cause of cancer deaths. It is estimated that 220,000 cases of PCa may be diagnosed yearly, and this is expected to increase with the expanding geriatric population1. Despite the extensive clinical and experimental studies over decades, the pathogenesis of Prostate cancer remains unknown. The biochemical and molecular mechanisms responsible for and associated specifically with the development and progression of Prostate cancer are largely unidentified2. Coupled with this is the largely ignored role of altered cellular metabolism as an essential factor in Prostate cancer; although transformations of metabolism are implicated in virtually all malignant cells3. The combination of molecular/biochemical relationships is required to identify critical events in Prostate cancer process.
Interest in the essential trace elements as cancer preventative agents was stimulated with the observation that selenium supplementation (200 µg per day) induced a 61% reduction in colorectal cancer in the treatment arm of the Nutritional Prevention of Cancer Trial, a randomized placebo controlled trial for skin cancer prevention4. Further epidemiologic evidence for the preventive role of selenium in selenium-poor populations in Linxian, China5 showed that combined intervention with selenium, vitamin E, and â-carotene was related to reduced incidence and mortality of gastric cancer and total cancer. Also, vitamin E has been shown to be a promising candidate for Prostate cancer prevention in the á-tocopherol â-carotene cancer prevention study, a controlled smoking trial where á-tocopherol reduced Prostate cancer incidence by 32% and mortality by 41%6. The SUpplementation en Vitamines et Mineraux AntioXidants (SUVIMAX) study found a significant reduction in Prostate cancer rates among men receiving a multivitamin containing 30 mg vitamin E, although the protective effect could not be attributed to any specific micronutrient 7. In vitro studies have demonstrated that vitamin E can inhibit DNA synthesis 8, reduce invasion 9, and induce apoptosis 10. Only a few studies have evaluated the mechanism of the combination of vitamin E and selenium in PCa 11. Because oxidative stress increases with depletion of trace elements in diseased states as well as androgen exposure in Prostate cancer 12, a putative risk factor for Prostate cancer therefore is the elevated level of malondialdehyde (an index of oxidative stress). Futhermore, oxidative stress can ameliorate the activities of several selenoenzymes and thereby reduced the preventive efficiency of selenium and zinc as well as their related proteins 13. Other trace elements, such as zinc, copper and cadmium are also necessary for the development and progression of Prostate cancer. For example, the total zinc levels in the prostate are ten times higher than those in other soft tissues 14. Zn is an essential trace element required for normal functions of several enzyme systems such as dehydrogenases, phosphatases, 5á-reductases, carboxypeptidases and carbonic anhydrase 15. In contrast, the Prostate cancer cells lose their ability to amass Zn and thus the essential roles of Zn are compromised in Prostate cancer cells 16.
In the present study, the extent of lipid peroxidation, serum concentrations of selenium, zinc, copper, cadmium and vitamin E were determined relative to the PSA values of the subjects.
Methods
Subjects
Total of 170 participants were recruited from the Cancer Screening Unit (CSU), University College Hospital (UCH), Ibadan, between 24 and 73 years of age who resided in the South-Western part of Nigeria. 120 participants had PSA in the range of 5.0–43.8 ng/ml, specifically, they were grouped into low-grade PSA (5–10 ng/ml) (n= 33), medium-grade PSA (11–20 ng/ml) (n=45) and high-grade PSA (> 20 ng/ml) (n= 42). Likewise, 50 apparently normal subjects were recruited as control and had PSA value < 3.0 ng/ml. Exclusion criteria included abstinence from hormonal and/ radiation therapy, use of prescription and non-prescription preparations known to alter PSA (e.g. Saw Palmetto, Finesteride), hormone levels and blood pressure. Those who were eligible were invited and screened during which their blood samples were collected. Written informed consent was obtained from each participant, and the Human Ethical Committee at the Oyo State Ministry of Health, Ibadan, Nigeria, approved the study.
Sample collection
Blood samples were drawn from an antecubital vein of subjects into containers containing EDTA and another portion in plain centrifuge tubes. All sample collection procedures were conducted with a minimal light exposure. The samples in plain centrifuge tubes were allowed to clot, and spun at 3,000 g for 15 minutes in an MSC bench centrifuge to obtain serum which was used for the estimation of total protein, PSA, lipid peroxidation and trace elements (Se, Zn, Cu and Cd). The blood samples in EDTA tubes were spun at 3,000 g for 15 minutes to obtain plasma which was used for the estimation vitamin E, while portion of the whole blood was used for determination of superoxide dismutase level.
Laboratory and clinical methods
We measured PSA in serum using electrochemiluminesence immunoassays (ECLIAs) from Roche Diagnostics in combination with a Roche/Hitachi MODULAR ANALYTICS device. The sera total protein levels were determined according to the method of Lowry et al.17 using bovine serum albumin as standard, while the extent of lipid peroxidation was estimated by the method of Buege and Aust18. The plasma vitamin E levels were estimated according to the method described by Meshali and Nightingale19. Whole blood superoxide dismutase level was assayed by the method of McCord and Fridovich.20 Standard precautions for trace element determination were taken, samples with signs of hemolysis were discarded. The serum trace elements levels were determined by direct method using atomic absorption spectroscopy (AAS), Shimadzu model AA-580 fitted with a Shimadzu PR-5 graphic printer following the manufacturer's analytical techniques at the International Institute of Tropical Agriculture (IITA), Ibadan, Nigeria. The determination of selenium concentration was done by digesting the serum with a mixture of nitric and perchloric acid. After hydride generation and using a sodium borohydride method, the selenium concentration was determined (AAS Model AA-580). To monitor the reproducibility and accuracy of the analytical techniques, reagent blanks and known samples were interspersed with the test samples.
Statistical analysis
All values were expressed as the mean S.D. (n > 30 in all the groups). Data were analyzed using one-way ANOVA followed by the post-hoc Duncanmultiple range test for analysis of biochemical data using SPSS version 11 (SPSS Inc Chicago, IIinois). Values were considered statistically significant at p< 0.05.
Results
Table 1 reveals some changes in the levels of total protein, superoxide dismutase, vitamin E and Cu/Zn ratio among prostate cancer patients studied. Plasma vitamin E levels were significantly (p< 0.05) decreased in PCa subjects when compared to normal. Precisely, vitamin E levels were decreased by 30%, 47% and 77% in subjects with PSA (5–10 ng/ml), PSA (11–20 ng/ml) and PSA (>20 ng/ml), respectively. Furthermore, there were no significant differences (p> 0.05) in the levels of serum total protein in PCa subjects with PSA (5–10 ng/ml) and PSA (11–20 ng/ml) when compared to normal (PSA < 3.0 ng/ml). However, the serum total protein levels were significantly (p< 0.05) reduced in PCa subjects with PSA > 20 ng/ml. There was a positive correlation between the mean age of the patients and their PSA values, i.e. PSA values increased with increase in the mean age of the patients. In addition, the ratios of serum Cu/Zn increased with increase in PSA values of the subjects. Concisely, the serum Cu/Zn ratios were 1: 1.2: 1.3 in subjects with PSA (5–10 ng/ml), PSA (11–20 ng/ml) and PSA (> 20 ng/ml), respectively (Table 1). Also, the whole blood superoxide dismutase levels decreased significantly (p<0.05) in PCa patients when compared to normal.
Table 1.
Changes in total protein, superoxide dismutase, vitamin E and Cu/Zn ratio among prostate cancer patients
| Subjects | ||||
| Grouping | Normal (PSA <3) |
PSA (5–10) |
PSA (11–20) |
PSA (>20) |
| Mean age (years) | 31.55 ±5.25 | 49.75 ± 8.84* | 64.30 ± 12.05* | 68.50 ± 10.20* |
| Total protein (mg/dL) | 0.81 ± 0.21 | 0.78 ± 0.33 | 0.75 ± 0.45 | 0.43 ± 0.11* |
| Vitamin E(mg/dL) | 5.65 ± 0.97 | 3.93 ± 0.81* | 2.97 ± 0.67* | 1.30 ± 0.56* |
| Cu/Zn ratio | 0.59 ± 0.06 | 0.88 ± 0.08* | 1.08 ± 0.23* | 1.15 ± 0.28* |
| SOD (U/mg protein) | 0.85 ± 0.08 | 0.28 ± 0.05* | 0.25 ± 0.07* | 0.16 ± 0.05* |
Values are Means ± S.D
Unit of PSA = ng/ml
Significantly different from normal at p< 0.05
SOD = Superoxide Dismutase
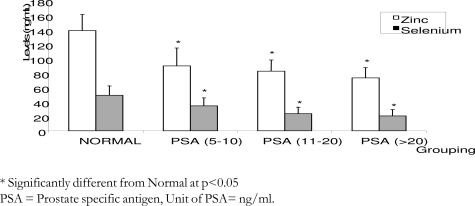
Figure 1 depicts the levels of serum selenium and zinc in PCa subjects. The serum selenium and zinc levels were significantly lower (p< 0.05) in all categories of patients studied. Specifically, the levels of serum selenium decreased by 30%, 52% and 58%, while the levels of serum zinc decreased by 35%, 41% and 47%, in subjects with PSA of 5–10 ng/ml, 11–20 ng/ml and > 20 ng/ml, respectively.
Figure 1.
Changes in serum zinc and selenium levels among prostatic cancer patients
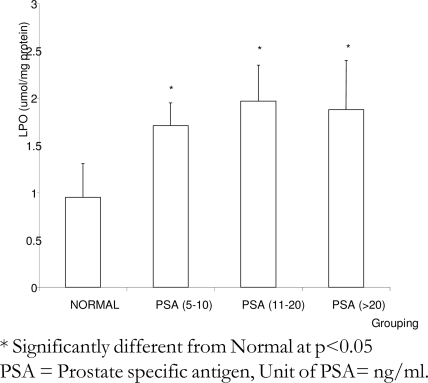
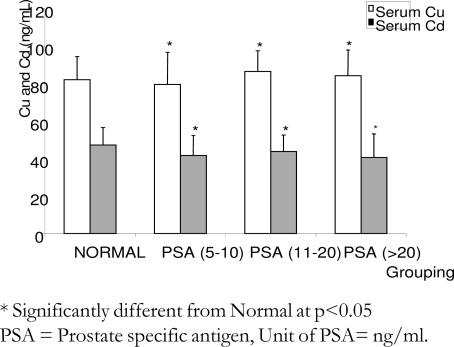
Figure 2 shows the extent of accumulation of lipid peroxidation products in sera of the subjects studied. The levels of serum lipid peroxidation products were significantly (p< 0.05) higher in Prostate cancer patients when compared to normal. Furthermore, the levels of lipid peroxidation products were elevated by 80%, 107% and 98% in subjects with PSA of 5–10 ng/ml, 11–20 ng/ml and >20 ng/ml, respectively. In figure 3, there were no significant differences (p>0.05) in the levels of serum copper and cadmium of the subjects with Prostate cancer when compared to normal.
Figure 2.
Changes in the levels of lipid peroxidation products among prostatic cancer patients
Figure 3.
Changes in serum cooper and calcium levels among prostatic cancer patients
Discussion
We conducted a fairly large study consisting of 120 suspected Prostate cancer subjects, and 50 apparently normal subjects as control. Overall, lower levels of plasma vitamin E, serum selenium and zinc were observed in these subjects. These parameters were inversely associated with the PSA values of the subjects. This inverse association between serum trace elements and PSA values points to a higher risk of Prostate cancer among the subjects.
Selenium has been hypothesized to play a role in preventing cancers21. Epidemiologic studies have demonstrated an inverse association between circulating selenium levels and cancers of the prostate, lung and colorectum 22. This observation was confirmed in the present study. In contrast, with respect to skin cancer hypothesis, recent analyses suggest that selenium supplementation actually increases the risk of non-melanoma skin cancer, particularly squamous cell carcinoma, among participants with higher baseline serum selenium levels23. However, secondary analyses showed reductions in risk of other cancers, especially prostate cancer; after approximately 4.5 years of treatment and 7.5 years of follow-up, prostate cancer incidence among persons receiving selenium supplements was half that experienced by the placebo group24. The mechanisms by which selenium may decrease cancer risk were summarized by Rayman25. The mechanisms include among others the role of selenium in cell cycle arrest, decreasing cells proliferation, inducing apoptosis, facilitating DNA repair by activation of p53, disruption of androgen receptor signaling, and being a key component of selenoenzymes26, 27, which incorporate selenium as selenocysteine, an infrequently occurring amino acid, into their active center28. The unique redox characteristics of selenocysteine confer important antioxidant properties to these selenoenzymes, such as glutathione peroxidases, selenoprotein P, and thioredoxin reductase, which are all expressed in the prostate29. Because of the low levels of selenium in this study, the essential functions of this element will be hindered in the Prostate cancer patients studied. However, selenium supplementation in Prostate cancer patients may be greatly influenced by genetic variation in the antioxidant enzyme, superoxide dismutase (SOD) genes. Chan et al,30 conducted a cross-sectional epidemiologic study of plasma selenium, an SOD2 variant and aggressive prostate cancer in men. They observed an unexpected positive association between plasma selenium and aggressive disease. Also, an SOD2 variant, a substitution of alanine for valine at amino acid 16 in the antioxidant enzyme SOD, was not statistically significantly associated with aggressive disease, although the relative risks (RRs) for one or two alanine alleles were above 1.0. Two patterns emerged in the analysis of the plasma selenium and SOD2: men with low selenium and two alanine alleles had a higher risk of aggressive disease (compared with low selenium and none or one alanine alleles); high selenium seemingly protected men with two alanine alleles; and men with high selenium and none or one alanine allele had a higher risk of aggressive disease (compared with low selenium and none or one alanine allele). In light of these findings, they concluded that the data “indicate caution against broad use of selenium supplementation for men with prostate cancer” and that “complete interpretation of results should depend on assessment of SOD2 genotype in trial participants.”
Our interest was to explore interactions of vitamin E and trace elements in Prostate cancer patients since evidence from animal and human studies showed an association between trace elements and antioxidative nutrients in cancers (including á- and â-carotenes and vitamin E)31.
In the present study, a significant decrease in plasma vitamin E levels in Prostate cancer patients was observed. The mean level of plasma vitamin E in subjects with PSA (5–10 ng/ml), PSA (11–20 ng/ml) and PSA (> 20 ng/ml) differs significantly from the normal (PSA < 3.0 ng/ml). The results are in agreement with other workers32. Decreasein vitamin E in these patients could be due to the possibility that vitamin E reacts very rapidly with molecular oxygen and free radicals generated during prostate carcinogenesis. This argument was supported by the fact that lipid peroxidation products were significantly higher in the Prostate cancer subjects relative to normal. The role of reactive oxygen species in the etiology of different cancers is well known,33.
It is therefore suggested that vitamin E acts as a free radical scavenger protecting polyunsaturated fatty acids from peroxidation reactions in the Prostate cancer subjects32.
Many laboratory studies have shown that the loss of a unique capability to retain high levels of zinc is an important factor in the development and progression of malignant prostate cells. In this study, we found that serum zinc levels in the Prostate cancer group were significantly lower than the control. The cancer group showed the lowest zinc level, whereas the control group consisting mostly of subjects with PSA < 3.0 ng/ml showed the highest zinc level. This observation is consistent with the findings of Whelan et al.34 and Lekili et al.35, which found that the plasma zinc levels were significantly lower in Prostate cancer than benign prostate hyperplasia (BPH) patients. They also found remarkable differences in the plasma concentrations of zinc in patients with Prostate cancer before and after therapy34. Other researchers also found that the level of zinc in tissues from Prostate cancer was significantly lower than that in BPH or normal tissues36. Zinc plays some unique biochemical functions in the body; it can induce G2/M cell cycle phase arrest and apoptosis which can be accompanied by increased mRNA expression of p21 37. Apart from cell cycle arrests, Zn is an important component of several metalloproteins required for DNA synthesis, immune function and antioxidant activity1. In order to avoid unnecessary delay and facilitate early detection of PCa when the PSA value ranged from 4.1 ng/mL to 10.0 ng/mL, serum zinc or better put serum Cu/Zn ratio (since the level of serum Cu and Cd remain unchanged in this study) could be a better marker (or complementary index) than free/total PSA ratio for the detection of Prostate cancer.
Conclusion
In the studied subjects, lowered vitamin E, selenium and zinc levels were associated with higher lipid peroxidation and increased risk of Prostate cancer, which seems more prominent in subjects with PSA values > 5.0 ng/ml. The decrease in serum selenium and zinc in the Prostate cancer patients may be indicative of an inter-relationship of these elements and/or their respective metalloenzymes. This study may therefore serves as a basis for recommending supplementation with vitamin E, selenium and zinc in the long-term management of prostate health.
References
- 1.Jarrard DF. Does Zinc Supplementation Increase the Risk of Prostate Cancer? Arch Ophthalmol. 2005;123:102–103. doi: 10.1001/archopht.123.1.102. [DOI] [PubMed] [Google Scholar]
- 2.Ostrander EA, Stanford JL. Genetics of prostate cancer: Too many loci; too few genes. Am J Hum Genet. 2000;67:1367–1375. doi: 10.1086/316916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costello LC, Franklin RB. “Why Do Tumor Cells Glycolyze?” From Glycolysis Through Citrate To Lipogenesis. Mol Cell Biochem. 2005;280:1–8. doi: 10.1007/s11010-005-8841-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters U, Chatterjee N, Church TR, Mato C, Sturup S, Foster CB, Schatzkin A, Hayes RB. High Serum Selenium and Reduced Risk of Advanced Colorectal Adenoma in a Colorectal Cancer Early Detection Program. Cancer Epidemiol Biomarkers Prev. 2006;15:315–320. doi: 10.1158/1055-9965.EPI-05-0471. PubMed. [DOI] [PubMed] [Google Scholar]
- 5.Blot WJ, Li JY, Taylor PR, Guo W, Dawsey S, Wang GQ, Yang CS, Zheng SF, Gail M, Li GY, Yu Y, Liu B, Tangrea J, Sun Y, Liu F, Fraumeni JF, Zhang YH, Li B. Nutrition intervention trials in Linxian, China: supplementation with specific vitamin/mineral combinations, cancer incidence, and disease-specific mortality in the general population. J Natl Cancer Inst. 1993;85:1483–1492. doi: 10.1093/jnci/85.18.1483. [DOI] [PubMed] [Google Scholar]
- 6.Heinonen OP, Albanes D, Virtamo J, Taylor PR, Huttunen JK, Hartman AM, Haapakoski J, Malila N, Rautalahti M, Ripatti S, Maenpaa H, Teerenhovi L, Koss L, Virolainen M, Edwards BK. Prostate cancer and supplementation with alpha-tocopherol and beta-carotene: incidence and mortality in a controlled trial. J Natl Cancer Inst. 1998;90:440–446. doi: 10.1093/jnci/90.6.440. PubMed. [DOI] [PubMed] [Google Scholar]
- 7.Meyer F, Galan P, Douville P, Bairati I, Kegle P, Bertrais S, Estaquio C, Hercberg S. Antioxidant vitamin and mineral supplementation and prostate cancer prevention in the SU.VI.MAX trial. Int J Cancer. 2005;116:182–186. doi: 10.1002/ijc.21058. PubMed. [DOI] [PubMed] [Google Scholar]
- 8.Sigounas G, Anagnostou A, Steiner M. dl-alphatocopherol induces apoptosis in erythroleukemia, prostate, and breast cancer cells. Nutr Cancer. 1997;28:30–35. doi: 10.1080/01635589709514549. PubMed. [DOI] [PubMed] [Google Scholar]
- 9.Zhang M, Altuwaijri S, Yeh S. RRR-alpha-tocopheryl succinate inhibits human prostate cancer cell invasiveness. Oncogene. 2004;23:3080–3088. doi: 10.1038/sj.onc.1207435. PubMed. [DOI] [PubMed] [Google Scholar]
- 10.Zu K, Hawthorn L, Ip C. Up-regulation of c-Jun-NH2-kinase pathway contributes to the induction of mitochondria-mediated apoptosis by alpha-tocopheryl succinate in human prostate cancer cells. Mol Cancer Ther. 2005;4:43–50. PubMed. [PubMed] [Google Scholar]
- 11.Zhang H, Wu Y, Malewicz B, Lu J, Li S, Marshall J, Ip C, Dong Y. Augmented suppression of androgen receptor signaling by a combination of alpha-tocopheryl succinate and methylseleninic acid. Cancer. 2006;107:2942–2948. doi: 10.1002/cncr.22345. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iynem AH, Alademir AZ, Obek C, Kural AR, Konukoglu D, Akçay T. The effect of prostate cancer and antiandrogenic therapy on lipid peroxidation and antioxidant systems. Int Urol Nephrol. 2004;36:57–62. doi: 10.1023/b:urol.0000032676.31470.b2. PubMed. [DOI] [PubMed] [Google Scholar]
- 13.Pryor WA, Stone K, Zang LY, Bermudez E. Fractionation of aqueous cigarette tar extracts: fractions that contain the tar radical cause DNA damage. Chem Res Toxicol. 1998;11:441–448. doi: 10.1021/tx970159y. PubMed. [DOI] [PubMed] [Google Scholar]
- 14.Mawson CA, Fischer MI. The occurrence of zinc in the human prostate gland. Can J Med Sci. 1952;30:336–339. doi: 10.1139/cjms52-043. PubMed. [DOI] [PubMed] [Google Scholar]
- 15.Chirulescu Z, Chiriloiu C, Suciu A, Pirvulescu R. Variations of zinc, calcium and magnesium in normal subjects and in patients with neoplasias. Med Interne. 1987;25:257–261. PubMed. [PubMed] [Google Scholar]
- 16.Costello LC, Liu Y, Zou J, Franklin RB. Evidence for a zinc uptaketransporter in human prostate cancer cells which is regulated by prolactin and testosterone. J Biol Chem. 1999;274:17499–17504. doi: 10.1074/jbc.274.25.17499. PubMed. [DOI] [PubMed] [Google Scholar]
- 17.Lowry OH, Rosenbrough NJ, Farr AL, Randall RJ. Protein measurement with Folin phenol reagent. J Biol Chem. 1951;193:265–275. [PubMed] [Google Scholar]
- 18.Buege JA, Aust SD. Microsomal lipid peroxidation. Methods Enzymol. 1978;30:302–310. doi: 10.1016/s0076-6879(78)52032-6. [DOI] [PubMed] [Google Scholar]
- 19.Meshali MM, Nightingale CH. Improved method for micro-determination of plasma vitamin E in laboratory rats. J Pharm Sci. 1974;63:1084–1086. doi: 10.1002/jps.2600630710. [DOI] [PubMed] [Google Scholar]
- 20.McCord JM, Fridovich I. Superoxide dismutase, an enzymatic function for erythrocuperin. J Biol Chem. 1969;244:6049–6055. [PubMed] [Google Scholar]
- 21.Jacobs ET, Jiang R, Alberts DS, Greenberg ER, Gunter EW, Karagas MR, Lanza E, Ratnasinghe L, Reid ME, Schatzkin A, Smith-Warner SA, Wallace K, Martínez ME. Selenium and colorectal adenoma: results of a pooled analysis. J Natl Cancer Inst. 2004;96:1669–1675. doi: 10.1093/jnci/djh310. PubMed. [DOI] [PubMed] [Google Scholar]
- 22.Etminan M, Fitzgerald JM, Gleave M, Chambers K. Intake of selenium in the prevention of prostate cancer: a systematic review and metaanalysis. Cancer Causes Control. 2005;16:1125–1131. doi: 10.1007/s10552-005-0334-2. [DOI] [PubMed] [Google Scholar]
- 23.Duffield-Lillico AJ, Slate EH, Reid ME, Turnbull BW, Wilkins PA, Combs GF, Park HK, Gross EG, Graham GF, Stratton MS, Marshall JR, Clark LC. Selenium supplementation and secondary prevention of nonmelanoma skin cancer in a randomized trial. J Natl Cancer Inst. 2003;95:1477–1481. doi: 10.1093/jnci/djg061. PubMed. [DOI] [PubMed] [Google Scholar]
- 24.Vogt TM, Ziegler RG, Patterson BH, Graubard BI. Racial differences in serum selenium concentration: Analysis of US population data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2007;166:280–288. doi: 10.1093/aje/kwm075. PubMed. [DOI] [PubMed] [Google Scholar]
- 25.Rayman MP. Selenium in cancer prevention: a review of the evidence and mechanism of action. Proc Nutr Soc. 2005;64:527–542. doi: 10.1079/pns2005467. PubMed. [DOI] [PubMed] [Google Scholar]
- 26.Zhao H, Whitfield ML, Xu T, Botstein D, Brooks JD. Diverse effects of methylseleninic acid on the transcriptional program of human prostate cancer cells. Mol Biol Cell. 2004;15:506–519. doi: 10.1091/mbc.E03-07-0501. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dong Y, Lee SO, Zhang H, Marshall J, Gao AC, Ip C. Prostate specific antigen expression is down regulated by selenium through disruption of androgen receptor signaling. Cancer Res. 2004;64:19–22. doi: 10.1158/0008-5472.can-03-2789. PubMed. [DOI] [PubMed] [Google Scholar]
- 28.Kryukov GV, Castellano S, Novoselov SV, Lobanov AV, Zehtab O, Guigó R, Gladyshev VN. Characterization of mammalian selenoproteomes. Science. 2003;300:1439–1443. doi: 10.1126/science.1083516. PubMed. [DOI] [PubMed] [Google Scholar]
- 29.Lincoln DT, Ali Emadi EM, Tonissen KF, Clarke FM. The thioredoxin-thioredoxin reductase system: over-expression in human cancer. Anticancer Res. 2003;23:2425–2433. PubMed. [PubMed] [Google Scholar]
- 30.Platz EA, Brady JB, Lippma SM. Selenium, genetic variation, and prostate cancer risk: Epidemiology reflects back on selenium and vitamin E cancer prevention trial. J Clin Oncol. 2009;27:3569–3572. doi: 10.1200/JCO.2009.22.2117. PubMed. [DOI] [PubMed] [Google Scholar]
- 31.Beno I, Klvanová J, Magálová T, Brtkova A. Blood levels of natural antioxidants in gastric and colorectal precancerous lesions and cancers in Slovakia. Neoplasma. 2000;47:37–40. [PubMed] [Google Scholar]
- 32.Lal G, Yadav SPS, Aggarwal SK, Bansal S, Chugh K, Lal H. Plasma vitamin E status in head and neck cancer. Indian J Clin Biochem. 1996;11:46–48. PubMed. [Google Scholar]
- 33.Badjatia N, Satyam A, Singh P, Seth A, Sharma A. Altered antioxidant status and lipid peroxidation in Indian patients with urothelial bladder carcinoma. Urol Oncol. 2009 Jan 24; doi: 10.1016/j.urolonc.2008.12.010. PMID: 19171490. [DOI] [PubMed] [Google Scholar]
- 34.Whelan P, Walker BE, Kelleher J. Zinc, vitamin A and prostatic cancer. Br J Urol. 1983;55:525–528. doi: 10.1111/j.1464-410x.1983.tb03362.x. PubMed. [DOI] [PubMed] [Google Scholar]
- 35.Lekili M, Ergen A, Celebi I. Zinc plasmalevels in prostatic carcinoma and BPH. Int Urol Nephrol. 1991;23:151–154. doi: 10.1007/BF02549712. PubMed. [DOI] [PubMed] [Google Scholar]
- 36.Brys M, Nawrocka AD, Miekos E, Zydek C, Foksinski M, Barecki A, Krajewska WM. Zinc and cadmium analysis in human prostate neoplasms. Biol Trace Elem Res. 1997;59:145–152. doi: 10.1007/BF02783239. PubMed. [DOI] [PubMed] [Google Scholar]
- 37.Liang JY, Liu YY, Zou J, Franklin RB, Costello LC, Feng P. Inhibitory effect of zinc on human prostatic carcinoma cell growth. Prostate. 1999;40:200–207. doi: 10.1002/(sici)1097-0045(19990801)40:3<200::aid-pros8>3.0.co;2-3. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]