Abstract
Background
Management of surgical emergencies in Nigeria is characterised by mismatch between supply of facilities and demand for care. This study aimed to evaluate the waiting time between presentation at hospital with acute abdominal disease and operative intervention.
Patients and Method
We prospectively studied adult patients with abdominal diseases requiring emergency operation. The interval between presentation and first contact with emergency room doctors was defined as T1; time from contact to decision to operate as T2; time taken to resuscitate patient T3 and to commencement of operation T4. Causes of delay and its impact on outcome of treatment were noted.
Results
There were 488 patients, mean age 32 ±1.7SD years. TT ranged between 0.8 and 79.0 hours, mean 22.3 ± 10.0 hours. In 81.6% operative intervention was delayed beyond 6 hours of which financial constraints accounted for 53.8%. T3 accounted for the longest delay (0.5 -53.0hours). Patients of lower socio-economic class had longer T3 (p<0.005). Waiting for complementary investigations caused delay in 22.1%. Post-operative complications (p=0.0001) and their severity were higher in patients with longer TT. Prolonged TT (p<0.001), ASA grade (0.005) and time from onset of symptoms to admission (p=0.009) were associated with mortality. Patients whose operations were delayed beyond 24 hours had a longer hospital stay.
Conclusion
Emergency abdominal operations were delayed in our patients mainly because of scarce financial resources. Delayed interventions were associated with higher morbidity and mortality.
Introduction
The emotional and psychological trauma following emergency admission can increase significantly if surgical intervention is unduly delayed. Although some surgical emergencies can and often should be dealt with some hours or even days after admission, there remains a group of conditions for which surgery should be available within hours or even minutes of arrival1,2,3. In these patients, a delay could mean loss of life or permanent disability. Strangulated hernia carries a mortality of 10–37% compared to 1% in simple obstruction4,5,6. Therefore, the timing of surgical intervention is essential for successful outcome in emergency surgery. In practice the timing of operative intervention is influenced by many factors including clinical diagnosis, complications of disease, consequences of delay, work load of physicians and availability of theatre space7,8,9.
Recent reports from developing countries have indicated increasing difficulties with the preparation of patients for emergency surgery and getting the patients to theatre within a time limit felt acceptable by the operating surgeon1,4,10,11. In developed countries, advanced imaging technology and critical care support have improved diagnostic accuracy and facilitated changes in operative timing in acute care surgery. In addition, patients are promptly resuscitated hence delays are occasioned after adequate resuscitation12,13. Unfortunately, in developing nations government hospitals provide few supplies for resuscitation, forcing patients to provide their own2,10,14. Delayed procurement of these supplies and inadequate low-technology apparatus often leads to delayed surgical intervention which is associated with increased morbidity and mortality.
In our institution, patients with emergency abdominal diseases present late after other forms of treatment have failed and life-threatening complications have set in2,15. In addition, many of them have intercurrent medical problems such as diabetes and cardiorespiratory disease which could deteriorate if the conditions were not expeditiously treated. These patients require prompt resuscitation including blood transfusion and haemodynamic monitoring. Unfortunately the patients must buy the needed medical supplies before treatment can begin. Emergency surgery has been defined as immediate life saving operation where resuscitation is carried out simultaneously with surgical treatment16. Because of the factors militating against prompt surgical intervention in our patients, emergency surgery has come to include operations performed sometimes days after the diagnosis of life threatening disease. The aim of this study was to determine the waiting time between diagnosis and surgical intervention in patients with abdominal surgical emergencies. We also determined the causes of delay and its effect on outcome of treatment.
Method
This prospective study was conducted in the department of Surgery Ahmadu Bello University Teaching Hospital Zaria between January 2005 and December 2006. Consecutive adult patients in whom a clinical diagnosis of abdominal disease requiring emergency operative treatment were included. Patients who were admitted following abdominal trauma and those admitted for observation were excluded from the study. As per protocol, time taken for preparing patient for surgery which includes detailed history taking, proper clinical examination, essential investigations and resuscitation should not exceed six hours1,7,14,15. Waiting time was defined as follows: waiting at hospital for the first contact with emergency room doctors T1; time between contact and decision to operate T2; time taken to resuscitate patient T3 and time to the commencement of operation T4. The total waiting time TT, was from presentation at hospital to commencement of operation. The ASA score at the time of diagnosis and at commencement of operation were noted. The causes of delay and its impact on the outcome of treatment were noted. Socio-economic class was classified into upper, middle and lower based on the modification of the National Statistics Socio-Economics Classification (NS-SEC)17.
For meaningful comparison of outcome of treatment we used a complication stratification and severity score previously described as follows18:
Severity 0: No complication.
Severity 1: Minor complication with minimal patient discomfort.
Severity 2: Moderate complication, significant patient compromised or prolonged hospital stay.
Severity 3: Severe complication, life threatening, need for another surgicalprocedure or admission to intensive care unit (ICU).
Severity 4: Death.
Therefore, the need for another surgical procedure is considered as a severe complication to the primary surgery. It is taken into account if it happened during the same admission and related to the primary procedure.
All emergency cases were seen immediately after admission by the emergency room doctors. A decision was then made about resuscitation and investigations. A treatment plan was organised by the senior registrar and timing of operation was confirmed after discussion with the consultant. All cases were booked for operation at the time of the consultant decision to operate. Theatre delay was defined as any factor contributing towards a delay in operating on an emergency general surgical patient following the consultant decision to operate and his contacting the operating theatre.
Emergency treatment voucher which is a short-term credit facility was used for patients that could not immediately pay for surgery if the patient or his relatives undertake to pay later. All operations were performed in the emergency theatre which was solely dedicated for emergency operations.
Data were analysed using the SPSS statistical software (version 17.0, SPSS, Chicago IL). Data were analysed with mortality being the initial outcome. This was followed by analysis based on severity of complications score as the outcome. Data ware reported as proportions, means ± SD or median (range). Categorical variables and proportions were compared with Fisher exact test. The Mann.Whitney test was used for univariate analysis of continuous variables when comparing two independent groups. Direct logistic regression was used to identify independent preoperative risk factors significant for prediction of mortality and severity of complication. Factors included in the model were age, sex, interval from onset of disease to presentation at hospital, ASA score at the time of surgery, total waiting time, and duration of surgery. A p-value of less than 0.05 was taken as significant.
Result
There were 488 patients, 301 males and 187 females giving a male to female ratio of 1.6:1. Their age ranged from 15 to 68 years, mean of 32 ± 1.7 SD years. The interval from onset of disease to presentation at hospital ranged from 0.5 to 168 hours. Thirty six (7.4%) patients presented within 3 hours of onset of their illness. The TT ranged from 0.8 to 79 hours as shown in Table 1, mean of 22.3 ± 10.0.
Table 1.
Waiting time for emergency abdominal operations
| Total Waiting Time (hours) |
Number | % |
| 0– 6 | 90 | 18.4 |
| 7–12 | 52 | 10.7 |
| 13–24 | 102 | 21 |
| 25– 48 | 166 | 34 |
| > 48 | 78 | 16 |
The longest waiting was at the resuscitation time (T3) which ranged 0.5 to 53.0 hours as shown in Table 2. The proportion of patients in the upper, middle and lower socio-economic classes were 16.6%, 25.0% and 58.4% respectively. Patients of lower socioeconomic class had significantly longer T3 compared to others (p< 0.005). The causes of delayed surgical intervention are shown in Table 3. Of the 214 patients that had delayed surgical intervention because of financial constraint 176 (82.2%) were of the lower socio-economic class. These patients were unable to purchase the prescribed materials for resuscitation or pay for surgery. Emergency treatment voucher was used for 122 (25.0%) patients. Despite efforts at resuscitation, the ASA score deteriorated with prolonged TT. The proportion of patients with ASA e″3E increased from 35% at presentation to 42% at commencement of operation in patients waiting for more than 24 hours. In 230 (47.1%) patients, operation was performed between 9.00PM and 8.00AM. The duration of operation ranged from 0.7 to 8.0 hours with a median of 2.7. Prolonged TT was associated with longer operation time. The mean operation time for patients that had surgery within 6 hours of admission was 1.8 ± 0.75 hours.
Table 2.
Waiting time from presentation to commencement of operation
| Waiting Time | Range (Hours) | Mean ± SD (Hours) |
| T1 | 0.1 − 1.6 | 0.5 ± 1.2 |
| T2 | 0.1 − 1.2 | 0.2 ± 1.0 |
| T3 | 0.5 − 53.0 | 9.4 ± 5.6 |
| T4 | 0.2 − 7.4 | 1.3 ± 1.8 |
| TT | 0.8 − 79.0 | 22.3 ± 10.0 |
T1 =waiting at hospital for the first contact with emergency room doctors
T2 =time between contact and decision to operate
T3 =time taken to resuscitate patient
T4 =adequate resuscitation to commencement of operation
TT = presentation to commencement of surgery
Table 3.
Causes and mean duration of delay beyond six hours in 398 patients
| Cause | Number | % | Waiting Time Mean ± SD |
| Financial constraint | 214 | 53.8 | 19.2 ± 17.3 |
| Delayed investigation results | 96 | 24.1 | 12.5 ± 8.3 |
| Late night admission | 52 | 13.1 | 8.0 ± 3.5 |
| Lack of cross matched blood | 31 | 7.8 | 12.3 ± 6.0 |
| Lack of theatre space | 28 | 7.0 | 6.1 ± 2.2 |
| Problem of personnel | 15 | 3.8 | 3.7 ± 2.1 |
| Other | 5 | 1.3 | 8.0 ± 6.5 |
Note: many patients had multiple causes.
SD = Standard deviation.
The operation time was 2.3 ±1.5 and 3.5 ±1.8 for patients that had operation within 24 hours or later respectively. The median operation time in patients with appendicitis was 0.85 hours compared to 2.20 in patients with perforated bowel. Three patients presented with obstructed inguinal hernias 1–3 hours after onset of symptoms. At admission they had colicky abdominal pain and vomiting. The hernias were irreducible and tenderness was localised to the site of the hernia. Their pulse rates were 76–86/minute while their temperature and leucocytes counts were normal. At the time of surgery 28–36 hours after admission they had developed persistent generalised abdominal pain and tenderness, had pulse rates of 125–142/minute, had fever and leucocytosis of 11–15x103/L. These patients required resection and anastamosis of bowel because of gangrenous changes which probably developed while the patients were on admission.
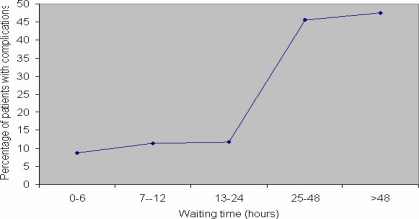
Post-operative complications increased with TT (Figure 1). Three hundred thirty two (68.0%) patients did not have any complications (severity score of 0). Overall, 23 (4.7%) patients died (severity score of 4). The median (range) severity of post-operative complication in patients operated within 6 hours of diagnosis was 0 (0–4) compared to 2 (0–4) in patients that waited for more than 24.0 hours (p<0.001). The characteristics of patients with post-operative complications are shown in table 4.
Figure 1.
Waiting time and postoperative complications
Table 4.
Characteristics of patients with or without post-operative complications
| With complications | Without complications | ||||||
| Characteristics | n | Mean (SD) | Standard error | n | Mean (SD) | Standard error | p-value |
| Age (years) | 156 | 33.5 (6.5) | 3.55 | 332 | 32.0 12.5) | 2.76 | 0.382 |
| Male | 95 | 202 | 0.758 | ||||
| Female | 61 | 130 | |||||
| Time from onset of symptom to hospital admission (hours) |
156 | 58.0 (17.5) | 10.60 | 332 | 26.7 (5.2) | 4.3 | 0.001 |
| Time from hospital admission to surgery (hours) |
156 | 37.4 (12 .6) | 7.91 | 332 | 16.8 ( 7.5) | 4.6 | 0.0001 |
| Duration of operation (hours) | 156 | 4.5 (1.7) | 0.75 | 332 | 2.3 (1.5) | 0.25 | 0.005 |
| Hospital stay (days) | 156 | 17.0 (4.9) | 3.20 | 332 | 5.8 (3.7) | 1.6 | 0.001 |
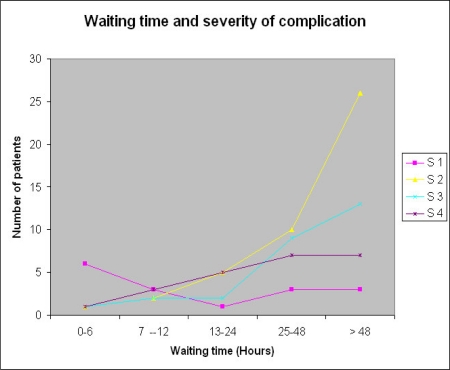
These patients had a mean TT of 37.4 ± 12.6 hours compared to 16.8 ± 7.5 in those without postoperative complications (p=0.0001). The TT is also a significant determinant of severity of complications (Figure 2). Multiple regression analysis in table 5 shows that the TT (p=0.0001), ASA grade (p=0.003) and time from onset of symptoms to hospital admission (p=0.0001) are significantly associated with severity of complications. The TT is also a significant determinant of post-operative mortality. Univariate analysis (Table 6) revealed that the factors that predicted mortality were TT (p=0.0001), duration of illness before presentation at hospital (p<0.005), ASA grade at commencement of surgery (p=0.0001), socio-economic class (p<0.001), duration of surgery (p<0.01) and intraperitoneal abscess (p<0.005). Multivariate analysis (Table 7) revealed that independent mortality-related factors ware the ASA grade (p<0.005), the time elapsed between onset of symptoms and hospital admission (p<0.009) and the TT (p<0.001). Prolonged TT was also associated with longer hospital stay. Among the 240 patients that had operations within 24 hours of admission the mean hospital stay was 5.3 ± 2.7 days compared to 14.8 ±6.1 in those delayed beyond 24 hours (p=0.01). Other factors associated with prolonged hospital stay ware ASA grade and presence of complications (p=0.0001).
Figure 2.
Waiting time and severity of complication
Table 5.
Results of logistic regression analysis of factors associated with severity of post-operative complications
| Variable | Estimate | Standard error | Wald test | Odds ratio | P-value |
| Time from onset of symptom to hospital admission (hours) |
−0.705 | 0.08 | 38.4 | 0.35 | 0.0001 |
| Time from hospital admission | −0.701 | 0.11 | 59.3 | 0.47 | 0.0001 |
| to surgery (hours) ASA grade | −0.628 | 0.13 | 20.2 | 0.55 | 0.003 |
| Duration of operation (hours) | −0.517 | 0.12 | 18.5 | 0.49 | 0.001 |
| Age (years) | −0.245 | 0.27 | 2.6 | 1.35 | 0.085 |
| Sex | −0.221 | 0.25 | 1.7 | 1.06 | 0.271 |
ASA= American Society of Anaesthesiologists
Table 6.
Univariate analysis of factors associated with post-operative mortality
| Variable | Deaths | X2 | p-value | |
| No. | (%) | |||
| Sex | 1.24, 1df, | 0.39 | ||
| Male (n=301) | 13 | (4.3) | ||
| Female (n=187) | 10 | (5.3) | ||
| Social Class | 8.27, 2df | 0.001 | ||
| Class I (n=81) | 1 | (1.2) | ||
| Class II (n=122) | 4 | (3.3) | ||
| Class III (n=285) | 18 | (6.3) | ||
| ASA grade at presentation | 57.24, 4df | 0.0001 | ||
| I or II (n=273) | 7 | (2.5) | ||
| III (n=205) | 13 | (6.3) | ||
| IV (n=10) | 3 | (30) | ||
| Age (years) | ||||
| 15–24 (n=166) | 8 | (4.8) | ||
| 25–49 (n=259) | 11 | (4.4) | ||
| Greater or equal to 50 (n=63) |
4 | (5.8) | ||
| Time from onset of symptoms to hospital admission (hours) |
12.75, 1df | 0.005 | ||
| < 48 (n=327) | 8 | (2.4) | ||
| Greater or equal to 48 (n=161) |
15 | (9.3) | ||
| Time from hospital admission to surgery (hours) |
46.25, 3df | 0.0001 | ||
| < 24 (n=240) | 3 | (1.2) | ||
| Greater or equal to 24 (n=248) |
20 | (8.1) | ||
| Operative diagnosis | 17.92, 1df | 0.005 | ||
| Appendicitis (n=248) | 2 | (0.8) | ||
| Intestinal obstruction | ||||
| (n=123) | 7 | (5.7) | ||
| Intestinal perforation | ||||
| (n=59) | 7 | (11.9) | ||
| Intra peritoneal | ||||
| abscess (n=34) | 6 | (17.7) | ||
| Other (n=24) | 1 | (4.2) | ||
ASA= American Society of Anaesthesiologists
Table 7.
Results of logistic regression analysis of factors associated with post-operative mortality
| Variable | Deaths | Odds ratio | 95% CI | p-value | ||
| No. | (%) | |||||
| Sex | 0.75 | |||||
| Male (n=301) | 13 | (4.3) | 1.00 | |||
| Female (n=187) | 10 | (5.3) | 1.28 | 0.57–1.32 | ||
| ASA grade at presentation | 0.005 | |||||
| I or II (n=273) | 7 | (2.5) | 1.00 | |||
| III (n=205) | 13 | (6.3) | 2.35 | 1.65–4.97 | ||
| IV (n=10) | 3 | (30) | 3.99 | 1.22–5.36 | ||
| Age (years) | 0.35 | |||||
| 15–24 (n=166) | 8 | (4.8) | 1.00 | |||
| 25–49 (n=259) | 11 | (4.4) | 0.80 | 0.53–1.34 | ||
| Greater or equal to 50 (n=63) |
4 | (5.8) | 1.08 | 0.75–1.50 | ||
| Time from onset of symptomsto hospital admission (hours) |
0.009 | |||||
| < 48 (n=327) | 8 | (2.4) | 1.00 | |||
| Greater or equal to 48 (n=161) |
15 | (9.3) | 3.97 | 1.54–4.58 | ||
| Time from hospital admission to surgery (hours) |
<0.001 | |||||
| < 24 (n=240) | 3 | (1.2) | 1.00 | |||
| Greater or equal to 24 (n=248) |
20 | (8.1) | 4.96 | 2.65–7.68 | ||
| Operative diagnosis | 0.005 | |||||
| Appendicitis | ||||||
| (n=248) | 2 | (0.8) | 1.00 | |||
| Intestinal obstruction | ||||||
| (n=123) | 7 | (5.7) | 0.89 | 0.64–2.63 | ||
| Intestinal perforation | ||||||
| (n=59) | 7 | (11.9) | 2.61 | 1.73–7.81 | ||
| Intra peritoneal | ||||||
| abscess (n=34) | 6 | (17.7) | 3.27 | 2.64–12.59 | ||
| Other (n=24) | 1 | (4.2) | 1.25 | 0.92–1.75 | ||
ASA= American Society of Anaesthesiologists
Discussion
This study has shown that patients with emergency abdominal diseases waited for too long before they had surgical intervention. The waiting time, ASA grade of the patient and the time elapsed between onset of symptoms and hospital admission had the maximum impact on the postoperative mortality. The same factors in addition to the duration of surgery are related to the severity of the postoperative complications. In this study, 81.6% of patients had surgical intervention more than 6 hrs after admission compared to 54.2% to 90.4% reported from other developing countries1,19,20. In developed countries, most emergency operations are performed within one hour of admission but delay beyond 3 hours is seen in about 15.0% of patients12,13. The mean waiting time in our patients was 22.3 ± 10.0SD which compares favourably to 39.5 to 44.0 hours reported from our sub-region1,19,20. In developing countries it is not unusual for emergency operations to be delayed beyond 48 hours1,2,4,19,20. Prolongation of the waiting time was usually a result of prolonged T3, the time taken for the patient to be resuscitated. For most inflammatory and obstructive conditions responsible for acute abdomen a period of preoperative resuscitation is usually necessary. The dangers of inappropriate hasty surgery have been highlighted by the National Confidential Enquiry into Perioperative Deaths (NCEPOD)16. However, the optimum time of surgery is a balance of the benefits of resuscitation weighted against the risks of progression of disease. In this study, delayed resuscitation was usually due to inability of the patients to immediately purchase the materials for resuscitation because of financial constraint. This is similar to other reports from our sub-region1,20,21. The Bamako initiative has given a prominent role to community financing through user fees22. The inequitable impact of user fee is such that it deters the poor more than the rich from using health facilities. Emergency treatment voucher was used to cover for surgical fees pending the time the patient was able to pay. This is similar to the indigenous patient's loan scheme of the Sokoto initiative which significantly reduced maternal mortalty23. The impact of user fee particularly in relation to equity should be properly designed and implemented otherwise it will widen the gap between the rich and the poor on access to health services. In this study following essential resuscitation, the mean delay in operating on abdominal emergencies was 2.8 hours, similar to the findings in developed countries12,13,24.
Waiting for complementary investigations was the second most common cause of delay in our patients and accounted for 22.1%. Many of these investigations were delayed because the patients could not pay for them on time or the staffs to perform them were not available. In a study from Libreville, waiting for complementary investigations was the most common cause of delay1. Other studies have shown that greater attention to emergency investigations would result in more timely interventions in emergently hospitalised patients2,25. Admissions at night are important causes of delayed surgical intervention. Most of these patients had acute appendicitis. Many reports have shown that with appropriate use of intravenous fluid and antibiotics such operations can be safely delayed to the following morning without increasing morbidity9,26. Prolongation of T4 (booking to start of operation) in our setting was mainly due to non-availability of theatre staff including surgeons, anaesthetist and nurses, and was usually due to inadequate staffing13,27.
However, it may also be due to poor commitment of the staff. A report from Pakistan revealed that the most common cause of delayed surgical intervention in their patients (36.3%) was inefficiency of the surgical team9. Another report from Ibadan, Nigeria revealed inefficiency of the doctors of the surgical team to be the major cause of poor emergency theatre time utilization21. In the present study, it is salutary to note that lack of electricity, anaesthetic gasses, operation gowns and linen which featured prominently in a previous study from our institution did not contribute to delays2. Several studies have demonstrated worse outcome in patients who waited too long for emergency operations4,10,20,28. The waiting time is an independent predictor of mortality and severity of morbidity. Prolonged delay would also influence the course of time-defendant diseases. In this as in other studies, patients that presented with simple obstruction required resection and anastamosis of bowel because of gangrenous changes due to delayed surgical intervention4,19,20. Prolonged delay in patients with appendicitis has also been shown to be associated with significantly higher risk of complications25,29,30. The better outcome of early surgical intervention in our study compared with prolonged delay is consistent with other reports1,4,20,26. Delayed surgical interventions also resulted in a high proportion of emergency operations occurring late at night. At that time there is increased reluctance to involve more senior members of staff and standards of care may be compromised.
In conclusion, this study has shown that a significant portion of our patients waited too long for emergency abdominal surgery which resulted in high morbidity and mortality. The main constraints in our setting are poverty and institutional organizational problems. Although the surgeon may not influence the long delays before patients with acute abdominal emergencies in our sub-region present to the hospital, once in the hospital, these patients should be promptly resuscitated to facilitate the safe conduct of both anaesthesia and surgery. Patients scheduled for emergency surgery should be taken to the theatre within an acceptable time limit, perhaps within 60 minutes of the decision to operate. By reducing the waiting time for surgical intervention, this would reduce mortality and morbidity. We suggest that our emergency treatment voucher should be made to also procure consumables to enable prompt resuscitation of the patient. The commencement of the national health insurance scheme (NHIS) in Nigeria is laudable as it would provide solution to most of these problems. However, for it to be effective the NHIS must provide cover for the lower socio-economic class which constitutes a significant portion of our patients. Finally, hospitals should be provided with efficient management system which would make surgical services readily available and affordable.
References
- 1.Zue AS, Josseaume A, Nsafu DN, Gloisy-Guibal L, Carpentier JP. Surgical emergencies at Libreville hospital centre. Ann Fr Anesth Reanim. 2003;22:189–195. doi: 10.1016/s0750-7658(03)00008-x. [DOI] [PubMed] [Google Scholar]
- 2.Eguma SA, Kalba DU. An audit of emergency anaesthesia and surgery. Nig J Surg Resch. 2003;5:140–147. [Google Scholar]
- 3.John M, Jonathan TC, Jessica EG, Robert W, Hobart WH. The surgical hospitalist: a new model for emergency surgical care. J Am Coll Surg. 2007;205:704–711. doi: 10.1016/j.jamcollsurg.2007.05.008. [DOI] [PubMed] [Google Scholar]
- 4.Lankester BJA, Britton DC, Holbrook AG, Umpleby HC, Tate JT, Budd J. Emergency surgery: atavistic refuge for the general surgeon? J Roy Soc Med. 2001;94:180–182. doi: 10.1177/014107680109400407. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eze JC. Obstructed inguinal hernia: Role of technical Aid program. JNMA. 2004;96:850–852. PubMed. [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmed A. Fibrous stricture of the small intestine following strangulated inguinal hernia: Report of two cases. Ann Afr Med. 2006;5:56–58. [Google Scholar]
- 7.Chianakwana GU, Ihegihu CC, Okafor PI, Anyanwu SN, Mbonu OO. Adult surgical emergencies in a developing country:the experience of Nnamdi Azikiwe university teaching hospital Nnewi, Anambra State, Nigeria. World J Surg. 2005;29:804–807. doi: 10.1007/s00268-005-7670-y. PubMed. [DOI] [PubMed] [Google Scholar]
- 8.Sicard N, Tousignant P, Pineault R, Dube S. Non-patient factors related to rate of ruptured appendicitis. Br J Surg. 2007;94:214–221. doi: 10.1002/bjs.5428. PubMed. [DOI] [PubMed] [Google Scholar]
- 9.Jawaid M, Amin MF, Khan RA, Iqbal SA. Waiting time for emergency surgeries in a tertiary care public hospital — a performance audit. Pak J Med Sci. 2005;21:133–137. PubMed. [Google Scholar]
- 10.Kingham PT, Kamara TB, Cherian MN, Gosselin RA, Simkins M, Meissner MC. Quantifying Surgical Capacity in Sierra Leone. Arch Surg. 2009;144:122–127. doi: 10.1001/archsurg.2008.540. [DOI] [PubMed] [Google Scholar]
- 11.Solabgeru BA, Duze AT, Kuranga SA, Adekanye AO, Afoegbu CK, Adelowo EO. Surgical emergencies in a Nigerian university hospital. Nig Postgrad Med J. 2003;10:140–143. [PubMed] [Google Scholar]
- 12.Wyatt MG, Houghton PW, Brodribb AJ. Theatre delay for emergency general surgical patients. Ann R Coll Surg Engl. 1990;72:236–238. [PMC free article] [PubMed] [Google Scholar]
- 13.Magee TR, Galland RB, Ramesh S, Dehn TC. Theatre delay for general surgical emergencies: a prospective audit. Ann R Coll Surg Engl. 1995;77:121–124. PubMed. [PubMed] [Google Scholar]
- 14.Toure CT, Dieng M. Emergency care in tropical areas: status report based on surgical emergencies in Senegal. Med Trop. 2002;62:237–241. PubMed. [PubMed] [Google Scholar]
- 15.Ameh EA. Typhoid ileal perforation in children: a scourge in developing countries. Ann Trop Pediatr. 1999;19:267–272. doi: 10.1080/02724939992356. [DOI] [PubMed] [Google Scholar]
- 16.Camping EA, Delvin HB, Haile RW, Ingram GS, Lunn JL. A report of the confidential enquiry into perioperative death. London: NCEPOD; 1997. Who operates when? [Google Scholar]
- 17.Chandola T, Jenkinson C. The new UK National Statistics socio-economic classification (NS-SEC) investigating social class differences in self-reported health status. J Public Health Med. 2000;22:182–190. doi: 10.1093/pubmed/22.2.182. [DOI] [PubMed] [Google Scholar]
- 18.Pillai SB, van Rij AM, Williams S, Thomson IA, Putterill MJ, Greig S. Complexity and risk adjusted modelfor measuring surgical outcome. Br J Surg. 1999;86:1567–1572. doi: 10.1046/j.1365-2168.1999.01286.x. [DOI] [PubMed] [Google Scholar]
- 19.Aderenmu AO, Adeoti ML, Oguntola AS, Oboro VO, Fadiora SO, Akanbi OO, Bello TO. Pattern and outcome of emergency surgery in a new Nigerian teaching hospital;The LAUTECH Oshogbo experience. Nig Postgrad Med J. 2006;13:172–175. [PubMed] [Google Scholar]
- 20.Mbah N, Opara WE, Agwu NP. Waiting time among acute abdominal emergencies in a Nigerian teaching hospital: causes of delay and consequences. Nig J Surg Resch. 2006;8:64–68. [Google Scholar]
- 21.Windokun A, Obideyi A. Audit of emergency theatre utilization. Afr J Med Sci. 2002;31:59–62. [PubMed] [Google Scholar]
- 22.Wiseman V. Reflections on the impact of the Bamako initiative and the role of user fees. Trop Doc. 2005;35:193–194. doi: 10.1258/004947505774938639. PubMed. [DOI] [PubMed] [Google Scholar]
- 23.Ahmed Y, Shehu CE, Nwobodo EI, Ekele BA. Reducing maternal mortality from ruptured uterus: the Sokoto initiative. Afr J Med Sci. 2004;33:135–138. PubMed. [PubMed] [Google Scholar]
- 24.Pearsy RM, Dana EC, Lanigan CJ, Pook JAR. Organisational failures in urgent and emergency surgery: A potential peri-operative risk factor. Anaesthesia. 2002;56:684–689. doi: 10.1046/j.1365-2044.2001.01374-4.x. PubMed. [DOI] [PubMed] [Google Scholar]
- 25.Bell CM, Redelmeier DA. Waiting for urgent procedures on the weekend among emergently hospitalized patients. Am J Med. 2004;117:175–181. doi: 10.1016/j.amjmed.2004.02.047. [DOI] [PubMed] [Google Scholar]
- 26.Chung CH, Ng CP, Lai KK. Delays by patients, emergency physicians and surgeons in the management of acute appendicitis:retrospective study. Hong Kong Med J. 2000;6:254–259. [PubMed] [Google Scholar]
- 27.Jonnalagadda R, Walround ER, Hariharan S, Walrond M, Prasad C. Evaluation of the reasons for cancellations and delays of surgical procedures in a developing country. Int J Clin Pract. 2005;59:716–720. doi: 10.1111/j.1742-1241.2004.00354.x. [DOI] [PubMed] [Google Scholar]
- 28.Wani RA, Parry FQ, Bhat NA, Wani MA, Bhat TH, Farzana F. Non-traumatic terminal ileal perforation. World J Emerg Surg. 2006;1:1–4. doi: 10.1186/1749-7922-1-7. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Green JM. When is faster better? Operative timing in acute care surgery. Critical care. 2008;14:423–427. doi: 10.1097/MCC.0b013e328306589e. PubMed. [DOI] [PubMed] [Google Scholar]
- 30.Ditillo MF, Dziura JD, Ravinovici R. Is it safe to delay appendectomy in adult with acute appendicitis? Ann Surg. 2006;244:650–660. doi: 10.1097/01.sla.0000231726.53487.dd. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]