From 1992 to 2004, melanoma incidence for all categories of tumor thickness increased 3.1% annually, and there was a 3.8% annual increase in the thickest cancers (Breslow depth, >4 mm), which have the least favorable prognosis.1–3 Since most melanomas are discovered by the patient or a partner, skin self-examination (SSE) with the assistance of a partner has the potential to improve long-term survival.4–6 Given the challenge of examining difficult-to-see body areas (eg, the back), partner assistance is important.7
By creating a workbook from our experience with 130 in-person interventions that increased SSE and partner-assisted skin examination (PASE),7–9 we extend our group's previous research. The workbook codifies the dialog of the in-person intervention with exercises that amplify skills and provide a framework for the patient and partner to understand the significance of melanoma by “story telling” about other people with melanoma in a way that is a call to action. Herein, we compare the efficacy of the workbook with that of in-person training.
Methods
Participants
We included in our study people aged 21 to 80 years with a history of stage I or IIA melanoma who had (1) treatment at least 6 weeks prior to participation, (2) sufficient vision to read a newspaper in English, and (3) a cohabitating partner. Subjects were offered nominal payment. The institutional review board of Northwestern University approved the study.
Interventions
In-Person Intervention
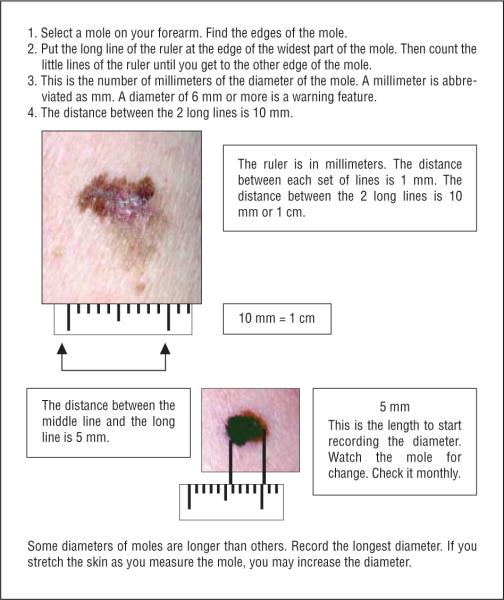
Partners jointly assessed border irregularity and color variation and measured the diameter of images of melanomas presented in the skills quiz. After the quiz, the research assistant reviewed with the partners the ABCDE criteria of melanoma (asymmetry, border irregularity, color variegation, diameter ≥6 mm, and evolution). During the previously described 15-minute intervention,7 use of a millimeter ruler and a handheld lighted magnifying lens was demonstrated. Participants received an enabling kit that contained a ruler, a magnifying lens, a laminated card with color examples of the ABCDE rule, and body maps.
Workbook
We gave participants a 39-page illustrated workbook (with 72 color figures) that was designed to prompt reflection about the personal risk of developing a melanoma and to explain the biology of melanoma. It also instructed on the use of enabling kit tools. In addition, the workbook included stories about people with melanoma and 12 confidence-building exercises. The skills training exercises were designed to build participants' confidence in their ability to identify border irregularity and color variation and to measure the diameter of moles (Figure). Inspiring stories of people who found their melanoma in the early stage were recounted. The experiences of well-known people who died of melanoma detected late in the course of the disease, such as Maureen Reagan and Bob Marley, were presented as cautionary tales of ignoring symptoms and failing to take action by seeing a physician. Patients and partners read the workbook together and wrote questions and comments on the pages of the manuals. The extensive written comments in all of the workbooks by the end of the study provided evidence that all participants had used the workbooks actively.
Figure Ruler.
Ruler exercise. Skills training exercise designed to build patient confidence in ability to measure the diameter of moles.
Measures
Baseline surveys and 1-month and 4-month follow-up assessments were separately completed by patients and partners, as previously described7–9 (Table 1). Scores from 5 questions were averaged to create a single index measure of self-efficacy in performing SSE (α=.92); the average score from 4 questions was used to measure attitudes toward SSE (α=.85); and the average score from 6 questions was used to measure knowledge of SSE (α=.81).
Table 1.
Measures Used to Evaluate Interventions
| Category | Baseline Responses | 1- and 4-Month Responses |
|---|---|---|
| SSE behavior | 0 (Never) | 0 (Never) |
| How often does the participant perform SSE with a partner? | 1 (Once or twice in the past year) | 1 (Once in the last month) |
| How often do they review skin examination guidelines? | 2 (Monthly) | 2 (Two or three times in the last month) |
| 3 (Weekly) | 3 (Weekly) | |
| 4 (Daily) | 4 (Daily) | |
|
| ||
| Self-efficacy | 0 (Not at all confident) | 0 (Not at all confident) |
| How confident are you that you can carefully examine your face, body, top of ears, back, and back of legs every month? (5 separate items) | 1 (Slightly confident) | 1 (Slightly confident) |
| 2 (Somewhat confident) | 2 (Somewhat confident) | |
| 3 (Very confident) | 3 (Very confident) | |
| 4 (Extremely confident) | 4 (Extremely confident) | |
|
| ||
| SSE attitudes | 0 (Not at all important) | 0 (Not at all important) |
| How important is it to you that you... | 1 (Slightly important) | 1 (Slightly important) |
| Know how to examine your skin for signs of sun damage? | 2 (Somewhat important) | 2 (Somewhat important) |
| Know the difference between a melanoma and a mole? | 3 (Very important) | 3 (Very important) |
| Carefully examine the skin of your face and body? | 4 (Extremely important) | 4 (Extremely important) |
| Have a partner help examine places (such as the back) that you cannot see yourself? | ||
|
| ||
| Knowledge of SSE | 0 (Not at all confident) | 0 (Not at all confident) |
| How confident are you that you know... | 1 (Slightly confident) | 1 (Slightly confident) |
| How to examine your skin for signs of a melanoma? | 2 (Somewhat confident) | 2 (Somewhat confident) |
| The difference between a melanoma and a mole? | 3 (Very confident) | 3 (Very confident) |
| How to examine your moles for an asymmetrical border or color? | 4 (Extremely confident) | 4 (Extremely confident) |
| How to examine your moles for an irregular border? | ||
| How to examine your moles for consistent (even) color? | ||
| How to use a ruler to measure the diameter of your mole? | ||
Abbreviation: SSE, skin self-examination.
Statistical Analysis
A series of 2 (intervention: in-person or workbook) × 3 (measurement time: baseline, 1-month, and 4-month follow-up) repeated measures analysis of covariance tests were used to assess changes in the outcomes. Sex and age were added to the analyses as covariates. Significant main effects of intervention (F values associated with P<.05) reflect differences between the in-person and workbook interventions, whereas significant main effects of measurement time reflect changes from baseline to follow-up periods. Finally, significant intervention × time interactions reflect differences between the interventions in the magnitude of change from baseline to follow-up periods.
Results
Forty participants were randomly assigned to either the in-person training (n = 19) or workbook intervention (n = 21) (Figure). No differences existed between participants' demographic characteristics (Table 2) (P>.05 for all χ2 tests).
Table 2.
Baseline Demographic Characteristics by Intervention
| Participants, No. (%) |
||
|---|---|---|
| Characteristic | In-Person (n=19) | Workbook (n=21) |
| Sex | ||
| Male | 9 (47) | 10 (48) |
| Female | 10 (53) | 11 (52) |
| Age, y | ||
| 18–29 | 2 (11) | 5 (24) |
| 30–39 | 4 (21) | 3 (14) |
| 40–49 | 5 (26) | 3 (14) |
| 50–59 | 3 (16) | 5 (24) |
| 60–69 | 3 (16) | 3 (14) |
| >70 | 2 (11) | 2 (10) |
| Education level | ||
| High school | 5 (26) | 5 (24) |
| Technical school | 1 (5) | 3 (14) |
| Some college | 4 (21) | 6 (29) |
| College graduate | 6 (32) | 6 (29) |
| Graduate school | 3 (16) | 1 (5) |
| Skin type | ||
| Always sunburn, never tan | 3 (16) | 6 (29) |
| Sunburn easily, tan minimally | 12 (63) | 7 (33) |
| Sunburn sometimes, tan gradually | 4 (21) | 6 (29) |
| Rarely sunburn, tan easily | 0 | 1 (5) |
| Never sunburn, always tan | 0 | 0 |
| Don't know | 0 | 1 (5) |
| Family history of skin cancer | ||
| Yes | 3 (16) | 8 (38) |
| No | 14 (74) | 13 (62) |
| Don't know | 2 (10) | 0 |
Patients in both the in-person and workbook groups significantly increased PASE following the interventions (Table 3). A significant main effect of time from the intervention (baseline, 1 month, and 4 months) was found for the variable “performed SSE with a partner” (F2,72=25.67, P<.001, η2=0.42). A nonsignificant intervention × time interaction was observed (F2,72=1.62, P>.05, η2=0.04), which suggests that the change in PASE was similar for those who received the in-person and the workbook interventions.
Table 3.
Mean (SD) Scores After In-Person Training Compared With Those After SSE Workbook Intervention on SSE Behavioral Outcomes, Self-efficacy, Attitudes, and Knowledge
| Follow-up Montha |
F Value Interactionb | ||||
|---|---|---|---|---|---|
| Category | Intervention | Baseline | 1 | 4 | |
| Performed SSE with a partner | In person | 0.00 (0.00) | 1.68 (0.17) | 1.10 (0.10) | 1.62 (NS) |
| Workbook | 0.00 (0.00) | 1.53 (0.16) | 1.33 (0.10) | ||
| Reviewed skin examination guidelines | In person | 0.00 (0.00) | 0.20 (0.14) | 0.16 (0.09) | 23.31 (P<.001) |
| Workbook | 0.00 (0.00) | 1.30 (0.14) | 0.71 (0.09) | ||
| SSE self-efficacy | In person | 0.20 (0.11) | 2.53 (0.18) | 2.92 (0.15) | 1.33 (NS) |
| Workbook | 0.49 (0.10) | 2.72 (0.17) | 2.82 (0.14) | ||
| SSE attitudes | In person | 0.92 (0.15) | 2.83 (0.16) | 2.80 (0.15) | 1.22 (NS) |
| Workbook | 0.96 (0.14) | 2.63 (0.15) | 2.92 (0.15) | ||
| SSE knowledge | In person | 0.12 (0.03) | 2.89 (0.11) | 3.31 (0.08) | 1.50 (NS) |
| Workbook | 0.11 (0.03) | 3.10 (0.10) | 3.41 (0.07) | ||
Abbreviations: NS, not significant; SSE, skin self-examination.
Data refer to the measures from each category detailed in Table 1.
Significance value for time × intervention interaction included.
Patients who received the workbook reviewed the SSE materials more often at both the 1-month and 4-month follow-ups than did those who had in-person training and received the kit that contained an SSE card with figures illustrating the ABCDE rule. After examining the pattern of means for this variable, we found some evidence that while no patients in either intervention reviewed SSE guidelines at baseline, the mean score increase was higher in the workbook intervention than in the in-person intervention at both the 1-month (0.20 for in-person compared with 1.30 for workbook) and 4-month (0.16 vs 0.71) follow-ups.
Participants were also compared with regard to the SSE-related psychological variables: self-efficacy, attitude, and knowledge. All 3 variables demonstrated a significant time effect: SSE self-efficacy (F2,72=62.03, P<.001, η2=0.63), SSE attitude (F2,72=26.98, P<.001, η2=0.43), and SSE knowledge (F2,72=283.55, P<.001, η2=0.89). The intervention (workbook vs in-person training) showed no significant difference in the 3 variables over the 3 times: SSE efficacy (F2,72=1.33, P>.05, η2=0.04), SSE attitude (F2,72=1.22, P>.05, η2=0.03), and SSE knowledge (F2,72=1.50, P>.05, η2=0.04). The means for these 3 variables were lowest at preintervention and increased at both the short-term and long-term follow-ups. The nonsignificant intervention × time interaction suggests these postintervention increases were similar in each intervention.
Comment
The in-person partner training and workbook interventions were equally effective at increasing postintervention PASE. However, at the 4-month follow-up, there were significant differences in the frequency of reviewing SSE guidelines: participants in the in-person training group reported reviewing the guidelines less frequently than did those in the workbook group. The workbook's detailed presentation of how to perform assessment of border irregularity and color variation and how to measure the diameter (Figure) may have become a reference to answer concerns that arose during SSE and PASE. Future research with this high-risk population will explore whether the workbook decreases (1) the time spent by health care personnel addressing patient concerns and/or (2) the frequency of urgent appointments made by anxious patients. Standardizing the intervention in a workbook reduced the influence of extraneous variables such as the ability and availability of health care personnel.
Previously, the in-person training was shown to increase scores in the psychological variables related to SSE, such as attitudes toward SSE self-efficacy and SSE knowledge.8,9 Consistent with these prior findings, we report herein that patients assigned to the in-person intervention reported increases in these variables' scores. When we compared the mean scores on these psychological variables of those assigned to either of the 2 interventions, we found no significant interaction effects; thus, we conclude that the workbook and in-person interventions influenced SSE self-efficacy and attitudes in a similar manner.
While this preliminary study has a small sample size, the workbook has promise as a cost-effective method for increasing SSE in those at risk to develop melanoma. In areas of importance to broader information dissemination (eg, cost-effectiveness and ease of dissemination), a take-home workbook offers the potential to reach those at risk of developing melanoma while placing less demand on the time and resources of health care personnel.
Acknowledgments
Funding/Support: This research was supported by grant 5R21 CA-103833-02 from the National Cancer Institute (Dr Robinson).
Footnotes
Financial Disclosure: None reported.
Disclaimer: Dr Robinson is editor of the Archives and was not involved in the editorial evaluation or decision to accept this work for publication.
References
- 1.Linos E, Swetter SM, Cockburn MG, Colditz GA, Clarke CA. Increasing burden of melanoma in the United States. J Invest Dermatol. 2009;129(7):1666–1674. doi: 10.1038/jid.2008.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ries LG, Melbert D, Krapcho M, et al. SEER Cancer Statistics Review. National Cancer Institute; 1975–2004. [Accessed January 4, 2008]. (November 2006 SEER data submission). http://seer.cancer.gov/csr/1975_2004/ [Google Scholar]
- 3.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2008. CA Cancer J Clin. 2008;58(2):71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 4.McPherson M, Elwood M, English DR, Baade PD, Youl PH, Aitken JF. Presentation and detection of invasive melanoma in a high-risk population. J Am Acad Dermatol. 2006;54(5):783–792. doi: 10.1016/j.jaad.2005.08.065. [DOI] [PubMed] [Google Scholar]
- 5.Carli P, De Giorgi V, Palli D, et al. Italian Multidisciplinary Group on Melanoma Dermatologist detection and skin self- examination are associated with thinner melanomas; results from a survey of Italian multidisciplinary group on melanoma. Arch Dermatol. 2003;139(5):607–612. doi: 10.1001/archderm.139.5.607. [DOI] [PubMed] [Google Scholar]
- 6.Brady MS, Oliveria SA, Christos PJ, et al. Patterns of detection in patients with cutaneous melanoma. Cancer. 2000;89(2):342–347. doi: 10.1002/1097-0142(20000715)89:2<342::aid-cncr19>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 7.Robinson JK, Turrisi R, Stapleton J. Efficacy of a partner assistance intervention designed to increase skin self-examination performance. Arch Dermatol. 2007;143(1):37–41. doi: 10.1001/archderm.143.1.37. [DOI] [PubMed] [Google Scholar]
- 8.Robinson JK, Turrisi R, Stapleton J. Examination of mediating variables in a partner assistance intervention designed to increase performance of skin self-examination. J Am Acad Dermatol. 2007;56(3):391–397. doi: 10.1016/j.jaad.2006.10.028. [DOI] [PubMed] [Google Scholar]
- 9.Robinson JK, Stapleton J, Turrisi R. Relationship and partner moderator variables increase self-efficacy of performing skin self-examination. J Am Acad Dermatol. 2008;58(5):755–762. doi: 10.1016/j.jaad.2007.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]