Abstract
Background
A third-generation TKA system was designed to address problems encountered with earlier designs including a high rate of patellofemoral complications. At a minimum of 5 years, we previously reported survivorship of 98.7% using revision for any reason as the endpoint for a cohort that includes the patients described in this report. That cohort was unique in that a tibial component that uses four short pegs for fixation was used in a subset of patients undergoing cruciate-retaining TKA and the tibial and femoral components were precoated with polymethylmethacrylate.
Questions/purposes
We now report the survival rate, postoperative function, complications, radiographic loosening, and osteolysis at a minimum of 10 years postoperatively.
Patients and Methods
We retrospectively reviewed 161 patients who underwent 179 TKAs. The patella was resurfaced in all cases and all components were cemented. Patients were evaluated clinically and radiographically for evidence of component loosening and osteolysis. Forty of the 161 patients (with 44 TKAs) had died and eight patients (nine knees) were lost to followup. For the remaining 113 patients (126 knees), the minimum followup was 10 years (mean, 11.7 years; range, 10.0–13.9 years).
Results
Survivorship at a minimum of 10 years postoperatively using revision for any reason and revision for aseptic loosening were 97.7% and 100%, respectively. Three knees were revised: one for infection, one for periprosthetic fracture, and one for postoperative arthrofibrosis. There were no reoperations for patellar component maltracking, wear or loosening, tibiofemoral polyethylene wear, osteolysis, or aseptic loosening. Hospital for Special Surgery scores improved from a mean of 47.7 (range, 23–78) preoperatively to 85.4 (range, 33–100).
Conclusions
This cruciate-retaining design had a low risk of implant failure or revision and the design changes eliminated the patellar failures seen with earlier iterations at up to 10 years.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
TKA reliably relieves the pain of end-stage knee arthropathy [26, 35, 42, 46]. Although numerous reports describe the long-term results of TKA, many of the systems described are not currently in use [1, 2, 16, 18, 39, 44, 50]. Of greater utility would be long-term reports of currently used prostheses developed to address issues associated with earlier implants.
Bozic et al. reported the comparative results of cruciate-retaining and cruciate-substituting TKA using the Nexgen® knee arthroplasty system (Zimmer, Inc, Warsaw, IN) at intermediate-term followup [8]. This system was designed to address issues identified with previous designs (Miller-Galante I [MGI] and Miller-Galante II [MGII], both manufactured by Zimmer, Warsaw, IN), that included a high rate of patellofemoral complications [45]. Specifically, the use of a metal-backed patella and a nonanatomic femoral component in the earlier designs led to a high incidence of patellar maltracking and full-thickness wear of the metal-backed patella with subsequent damage to the femoral component and a high rate of patellar component loosening. The third-generation design includes a three-pegged, all-polyethylene patellar component and a femoral component with a deeper, more anatomic femoral trochlea. Further, the instrumentation was improved to facilitate appropriate external rotation of the femoral and tibial components to enhance patellofemoral tracking. This system also is unique in that the tibial component uses four short pegs for fixation (as opposed to a keel or stem) and the cemented tibial and femoral components are precoated with polymethylmethacrylate (as were the cemented versions of the MGI and MGII) in an attempt to enhance component fixation. Some midterm reports suggest improved survival of this device relative to earlier implant designs [9, 22, 25, 28, 30]. The study by Bozic et al. also confirmed high survivorship of this design at a mean 5.8 years postoperatively [8].
The purpose of our study was to evaluate the longer-term results of a subset of patients, previously reported, who had a cruciate-retaining prosthesis and a tibial component with four short pegs implanted for fixation at a minimum of 10 years postoperatively. In particular, we sought to determine: (1) implant survivorship, (2) clinical function, (3) rate of complications including patellofemoral complications, and (4) radiographic osteolysis and implant loosening.
Patients and Methods
Between July 1994 and July 1997, four of us performed 334 TKAs in 287 patients. During this period, all patients with an intact posterior-cruciate ligament and less than 20° preoperative flexion contracture were considered candidates for a cruciate-retaining (NexGen®) implant. Patients who did not meet these criteria underwent arthroplasty using a posterior-stabilized or constrained implant. One hundred sixty-seven (186 knees) of the 287 patients thus underwent replacement with the NexGen® cruciate-retaining prosthesis. All tibial baseplates used the same modular locking mechanism for the net-molded UHMWPE insert manufactured from 1900H resin. The tibial component in six patients (seven knees) was stemmed, leaving 161 patients (179 knees) who had a four-pegged tibial component available for study. Of the 18 bilateral procedures, 11 were performed simultaneously, and seven were staged at a minimum of 6 weeks apart (range, 6–10 weeks). There were 101 women and 60 men with a mean age of 64.2 years (range, 25.9–85.2 years) at the time of surgery. Mean patient height and weight were 66.2 inches (range, 59–76 inches) and 186 pounds (range, 119–303 pounds), respectively. The predominant diagnosis was osteoarthritis (128 patients; 80.0%), followed by rheumatoid arthritis in 11 (6.8%), avascular necrosis in four (2.5%), posttraumatic arthritis in three (1.9%), and other diagnoses in 15 (9.3%). Forty patients (44 knees) had died before the 10-year followup and eight (nine knees) were lost to followup. For the remaining 113 patients (126 knees), the minimum followup was 10 years (mean, 11.7 years; range, 10.0–13.9 years). The families of the 40 patients who had died were contacted and none of these patients had undergone a revision procedure before death. Forty-three patients (51 knees) were seen in our clinic at last followup, and 70 patients (75 knees) underwent remote clinical evaluation either by a local orthopaedic surgeon, a telephone evaluation, or a mailed questionnaire that included the portions of the Hospital for Special Surgery (HSS) knee score that can be self-reported (including pain, walking ability, and the use of an assist device) along with a written prescription for radiographs to be sent to our office.
Surgery was performed by one of four surgeons (AGR, JJJ, RAB, JOG). Femoral and tibial components were precoated with polymethylmethacrylate, and a pressurizing gun was used for cementation in all cases. All patellae were resurfaced with a cemented all-polyethylene component with three pegs. A standard medial parapatellar arthrotomy was performed in all cases. All components were implanted using a measured resection technique, followed by appropriate soft tissue balancing. The femoral valgus cut angle was measured using an intramedullary guide, and proper external rotation of the femoral component was assessed using a guide that referenced the posterior condylar axis combined with bony landmarks (including Whiteside’s line and the epicondylar axis). The tibial resection was performed using a standard extramedullary alignment guide. The postoperative protocol was identical in each case, including anticoagulation with warfarin for 4 weeks and prophylactic antibiotics for 48 hours postoperatively.
Patients were evaluated postoperatively at 3 weeks, 6 weeks, 3 months, 6 months, and then yearly. Annual clinical evaluation was performed using the HSS knee score [20]. This score assigns points based on pain, function, ROM, quadriceps strength, deformity, and instability (100 points total). A completed score at a minimum 10-years postoperatively was available for the 43 patients (51 knees) who returned to our office for a physical examination.
Radiographic evaluation was performed preoperatively and 6 weeks postoperatively using a full-length mechanical axis view, standing AP, lateral, and Merchant views. Standing AP, lateral, and Merchant views were obtained annually thereafter. Radiographs were evaluated by one nontreating surgeon (AJS) for component positioning and the presence of radiolucent lines 1 mm or greater in width as measured with a digital radiographic system [13]. Serial radiographs were examined for evidence of osteolysis, defined as a radiolucency with a minimum diameter of 10 mm in at least one dimension and 5 mm in diameter in the second dimension, loss of trabeculation, and the presence of a sclerotic rim [37]. Radiolucencies were categorized as progressive or nonprogressive based on lucency width and extent on serial films and localized according to the anatomic zones of the Knee Society Total Knee Arthroplasty Roentgenographic Evaluation and Scoring System [13]. The Insall index was determined on the lateral projection, defined as the ratio of the length of the patellar tendon on its deep surface to the greatest diagonal length of the patella [21]. Radiographic data at a minimum of 10 years were collected for 63 of the 179 knees (35.2%) (Fig. 1).
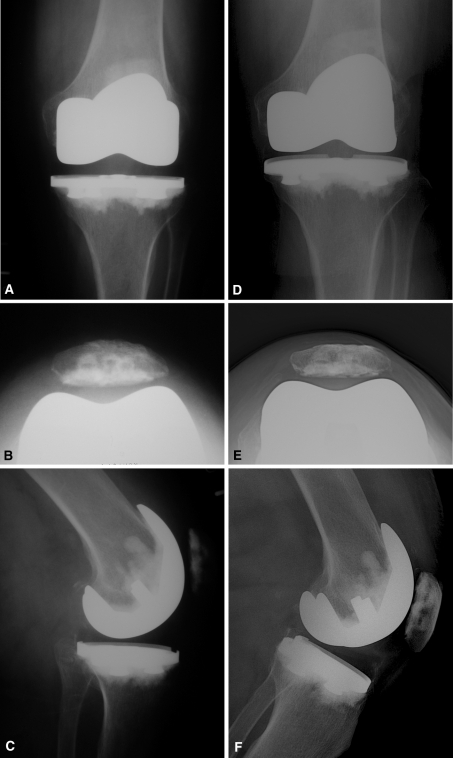
Fig. 1A–F.
(A) AP, (B) Merchant, and (C) lateral view radiographs obtained 6 weeks after cruciate-retaining TKA using a four-pegged tibial component in a 74-year-old woman are shown. (D) AP, (E) Merchant, and (F) lateral view radiographs show the knee 12.5 years postoperatively.
Kaplan-Meier survivorship analysis [24] was performed using revision for any reason and revision for aseptic loosening as end points; data from all 161 patients and 179 knees were used in this analysis at the time of the last evaluation. A separate survival analysis was performed, which included the eight patients (nine knees) lost to followup and which assumed all prostheses failed in the patients lost to followup.
Results
For the 161 patients (179 knees) Kaplan-Meier survivorship analysis revealed 97.7% (95% confidence limit, 96.3%–99.0%) survivorship at a minimum of 10 years postoperatively using revision for any reason as the end point and 100% using revision for aseptic loosening as the end point (Fig. 2). Assuming all nine knees in the eight patients lost to followup failed owing to aseptic loosening, the worst-case scenario analysis revealed a 10-year implant survivorship of 92.4% (95% confidence limit, 90.1%–94.7%) using revision for any reason as the end point and 94.6% (95% confidence limit, 92.6%–96.6%) using revision for aseptic loosening as the end point (Fig. 3).
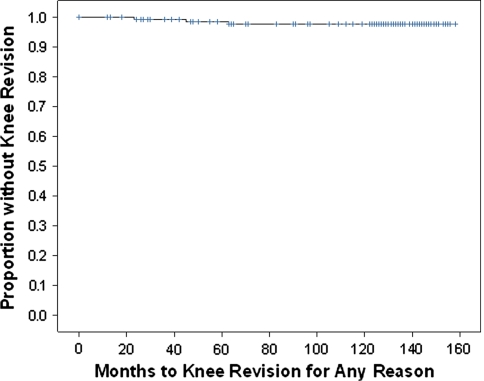
Fig. 2.
Kaplan-Meier survival analysis of the 179 knees revealed 97.7% (95% confidence limit, 96.3%–99.0%) survivorship at a minimum of 10 years postoperatively using revision for any reason as the end point.
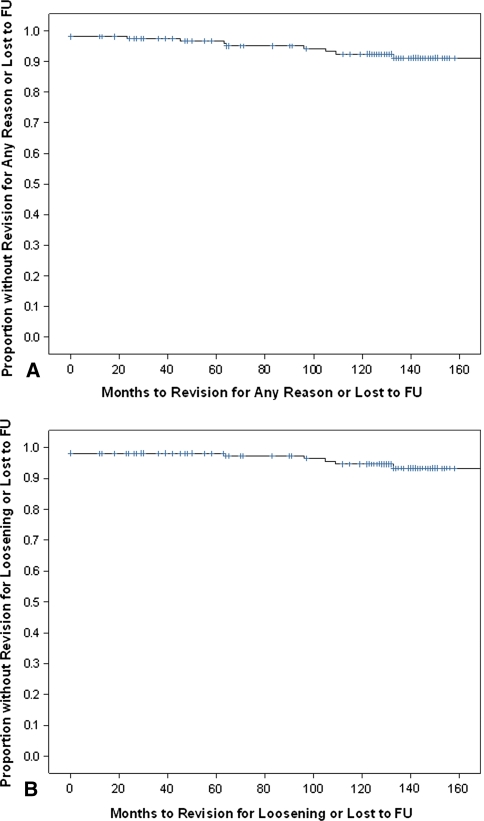
Fig. 3A–B.
(A) The worst-case scenario Kaplan-Meier survival analysis assuming all nine knees in eight patients lost to followup failed owing to aseptic loosening revealed a 10-year implant survivorship of 92.4% (95% confidence limit, 90.1%–94.7%) using revision for any reason as the end point. (B) The worst-case scenario Kaplan-Meier survival analysis assuming all nine knees in the eight patients lost to followup failed owing to aseptic loosening revealed a 10-year implant survivorship of 94.6% (95% confidence limit, 92.6%–96.6%) using revision for aseptic loosening as the end point. FU = followup.
Functional analysis for the entire cohort at the time of the last physical examination revealed improved ROM from a mean preoperative flexion contracture of 5.8° (range, 0°–20°) to a mean of 0.6° (range, 0°–15°) extension at the time of the most recent clinical followup (mean, 8.9 years; range, 1.1–13.2 years). The mean preoperative flexion of 107.6° (range, 75°–140°) improved to a mean of 116.2° (range, 85°–130°) postoperatively. HSS knee scores for patients who had a complete evaluation at a minimum 10-years postoperatively improved from a mean of 47.7 (range, 23–78) preoperatively to a mean of 85.4 (range, 33–100). Five knees in five patients had a score less than 70, or patients reported the inability to walk on the self-reported evaluation; all five cited arthritis in another joint as a factor limiting their ability to ambulate. Two of these five patients also had a major comorbidity, including disseminated cancer in one and peripheral arterial disease in another, as limiting their ambulatory capacity. The remaining three patients had manipulation under anesthesia after the index arthroplasty for poor postoperative ROM. At the most recent followup, two of these patients had full extension and flexion to 110° and 130°, respectively. The remaining patient had multiple patellar realignment procedures before the index arthroplasty, and at her most recent followup, she had a 10° flexion contracture and additional flexion to 85°.
Complications occurred in 24 of the entire cohort of 161 patients (14.9%). Two complications occurred intraoperatively, including one laceration of the medial collateral ligament, which was repaired primarily and treated with a hinged knee brace for 6 weeks, and one fracture of the medial femoral condyle, which was treated with screw fixation at the time of surgery. Seven knees (3.9%) had manipulation under anesthesia for poor ROM. A deep venous thrombosis was diagnosed in four knees (2.2%), and a hematoma developed in three knees (1.7%); all were treated nonoperatively. Two patients (1.2%) experienced a postoperative ileus and a gastrointestinal ulcer respectively, which both eventually resolved. Six knees (3.4%) underwent reoperation during the followup period; the components were retained in three of six knees. The three component revisions included one two-stage exchange for a deep infection, one revision for stiffness, and one supracondylar femur fracture treated with a modular tumor endoprosthesis (the components were well-fixed intraoperatively). The three remaining reoperations included one irrigation and débridement for an early postoperative infection, one periprosthetic femur fracture treated with a retrograde intramedullary nail, and one arthroscopic arthrolysis for postoperative stiffness; all three components were retained. There were no reoperations or specific complications related to the patellofemoral joint or to wear of the bearing surface.
Nonprogressive radiolucencies were identified on radiographs in association with 21 of the 63 tibial components (33.3%) and eight of the femoral components (12.7%). The majority of radiolucencies surrounding the tibial and femoral components were seen in Zones 1 and 4, respectively. No components were radiographically loose and osteolysis was not identified in any patient. The mean Insall ratio was 0.79 (SD, 0.14; range, 0.6–1.2), and the mean valgus angle was 3.58° (SD, 2.05°; range, 0°–6°). The mean patellar tilt was 0.85° (range, 0°–4°), and the mean lateral displacement was 1.34 mm (range, 0–4 mm).
Discussion
The contemporary prosthesis used in our study was developed to improve implant survival, wear behavior, and address problems associated with earlier implants, including high rates of patellofemoral maltracking and loosening. The purposes of this study were to determine the outcomes of primary TKA using this implant with a focus on identifying patellofemoral and wear-related complications (including osteolysis), overall survivorship, and clinical outcomes. We previously reported results for a larger cohort of patients at a minimum of 5 years [8] (that included the subset of patients described in this report) and wanted to ensure that durable results were obtained at a minimum of 10 years.
Our study has several limitations. First, eight patients (nine knees) were lost to followup. Assuming all nine knees in these eight patients lost to followup failed owing to aseptic loosening, the worst-case scenario analysis revealed 10-year implant survivorship rates of 92% and 95% using revision for any reason and for aseptic loosening, respectively, as end points. Six of the eight patients (seven of nine knees) were seen within 3 years of the time of this investigation and at that time none of these patients had undergone a reoperation or revision, and none had experienced a complication. Second, we did not have minimum 10-year followup radiographs for all 179 knees, and it is possible radiographic findings (such as osteolysis) may have been identified and thus underestimated in our study. We have made the assumption in our survival analysis that these implants were not loose, malfunctioning, or in need of revision. Further, not all patients were seen physically by one of the authors at a minimum of 10 years, with 70 of the 113 patients living far enough from our offices that a telephone questionnaire and/or physical examination by another physician was used for the analysis, and based on the lack of a complete physical examination, a complete HSS knee score could not be calculated at a minimum of 10 years for all patients included in this study. Finally, outcomes such as ROM measurements and the radiographic analysis did not have multiple observers and may be subject to interobserver variability.
There are few long-term studies available to document the longevity of contemporary cruciate-retaining total knee implants (Table 1) [3, 4, 7, 14, 41, 43, 52]. Our results compare favorably with those of prior studies with 98% and 100% survivorship rates with revision for any reason and aseptic loosening as end points at 10 years. The system described in this series is unique in that it incorporates the use of a four-pegged tibial design. Potential advantages of this design include preservation of proximal tibial bone, ease of preparation and component insertion, and the potential for reduced stress shielding of the proximal tibia by avoiding fixation deep in the tibial metaphysis [5, 11, 29, 32, 51]. Although the use of polymethylmethacrylate precoating has been associated with problems when used for a cemented femoral stem of a THA [36, 48], in this series aseptic loosening of precoated tibial and femoral components was not seen. A cement gun was used in all cases and proper pressurization and meticulous cementation technique may be additional factors in achieving durable long-term implant fixation [40].
Table 1.
Minimum 10-year results with contemporary cruciate-retaining prosthesis
| Study | Number of knees | Implant* | Followup (years) | Implant survival (%)† | Implant survival (%)‡ | Functional outcome§ | Mean postoperative knee flexion (degrees) | Comments |
|---|---|---|---|---|---|---|---|---|
| Ritter et al. [41] | 4583 | AGC | 15 | 98.86 | NA | 81 [A] | 110 | 210 lost to followup |
| Faris et al. [14] | 201 | AGC | 13 | 97.32 | NA | 87 [B] | NA | All had noncemented femoral components |
| Parsch et al. [38] | 141 | PFC | 14 | 91 | 97 | 76 [B] | NA | 65 knees evaluated |
| Attar et al. [3] | 354 | PFC | 15 | 81.7 | NA | NA | NA | 15 of 277 patients alive at 15 years |
| Rodricks et al. [43] | 160 | PFC | 15 | 91.5 | 97.2 | 89 [B] | 112 | 63 of 64 alive patients available for review |
| Wright et al. [52] | 523 | Kinemax | 11 | 96.1 | 97.2 | 88 [C] | NA | 34 patients (14%) lost to followup; questionnaire only |
| Bourne et al. [7] | 100 | Genesis II | 10 | 96 | NA | 91 [B] | 112 | 18% of series had posterior-stabilized knee |
| Barrington et al. [4] | 127 | NexGen | 10 | 97 | NA | 94 [B] | 116–118 | 87 knees in patients still alive; 71 with radiographs |
| Current study | 179 | NexGen | 10 | 97.7 | 100 | 85 [D] | 116 | Current study |
* Implants included AGC® (Biomet Inc, Warsaw, IN), PFC® (DePuy Orthopaedics, Inc, Warsaw, IN), Kinemax® (Stryker Orthopaedics, Mahway, NJ), Genesis II® (Smith and Nephew, Inc, Memphis, TN), Kinematic™ (Howmedica, Rutherford, NJ), and NexGen® (Zimmer, Inc, Warsaw, IN); †revision for any reason used as end point; ‡revision for aseptic loosening used as end point; §scoring systems: [A] scoring system not specified; [B] Knee Society score; [C] WOMAC; [D] Hospital for Special Surgery score; NA = information not provided.
Functional results after TKA in our series were comparable to results in other long-term studies of contemporary cruciate-retaining implants (Table 1).
There were no reoperations or revisions owing to issues related to the patellofemoral articulation in this series. This is in contrast to previous experience with first-generation implants, especially those with a metal-backed patella and a nonanatomic femoral trochlea, which had a higher incidence of component loosening, patellofemoral maltracking, and surface abrasion of a well-fixed femoral component secondary to wear-through of the metal-backed patella [45]. The all-polyethylene, three-pegged patellar component, used in conjunction with a deeper femoral trochlea and improved understanding of femoral and tibial component rotation, provided reliable long-term survival.
In our series, there were no complications attributable to wear or failure of the modular insert and osteolysis was not identified among the portion of the cohort who had radiographs at a minimum of 10 years. Although the orthopaedic literature is mixed regarding the wear-related effects of cruciate retention versus substitution [10, 12, 17, 23, 27, 31, 33, 34, 47, 49], two studies identified osteolysis and wear problems associated with a posterior stabilized design [15, 37]. In addition to shape, the properties of the polyethylene constitute one of the critical variables affecting wear of the tibial insert. The devices used in our series incorporated net-molded UHMWPE, a material that reportedly has superior wear characteristics [6, 19].
We report the longer-term outcomes of a series of patients who underwent cruciate-retaining cemented TKA using a third-generation design with four short pegs for tibial fixation. At a minimum 10-year followup, this implant continues to provide reliable clinical function with a low risk of revision or reoperation.
Acknowledgments
We acknowledge Peggy Arp, Reggie Barden, Laura Quigley, and Nicholas Ting for assistance with preparation of this manuscript.
Footnotes
One or more of the authors (CDV, AGR, JJJ, RAB, JOG) have received consulting fees, royalties, and/or research funding from Zimmer, Inc (Warsaw, IN). The institution of one or more of the authors (CDV, AGR, JJJ, RAB, JOG) has received funding from Zimmer, Inc.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Aglietti P, Buzzi R, Felice R, Giron F. The Insall-Burstein total knee replacement in osteoarthritis: a 10-year minimum follow-up. J Arthroplasty. 1999;14:560–565. doi: 10.1016/S0883-5403(99)90077-3. [DOI] [PubMed] [Google Scholar]
- 2.Archibeck MJ, Berger RA, Barden RM, Jacobs JJ, Sheinkop MB, Rosenberg AG, Galante JO. Posterior cruciate ligament-retaining total knee arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am. 2001;83:1231–1236. doi: 10.2106/00004623-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 3.Attar FG, Khaw FM, Kirk LM, Gregg PJ. Survivorship analysis at 15 years of cemented press-fit condylar total knee arthroplasty. J Arthroplasty. 2008;23:344–349. doi: 10.1016/j.arth.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 4.Barrington JW, Sah A, Malchau H, Burke DW. Contemporary cruciate-retaining total knee arthroplasty with a pegged tibial baseplate: results at a minimum of ten years. J Bone Joint Surg Am. 2009;91:874–878. doi: 10.2106/JBJS.G.01609. [DOI] [PubMed] [Google Scholar]
- 5.Bertin KC. Tibial component fixation in total knee arthroplasty: a comparison of pegged and stemmed designs. J Arthroplasty. 2007;22:670–678. doi: 10.1016/j.arth.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Berzins A, Jacobs JJ, Berger R, Ed C, Natarajan R, Andriacchi T, Galante JO. Surface damage in machined ram-extruded and net-shape molded retrieved polyethylene tibial inserts of total knee replacements. J Bone Joint Surg Am. 2002;84:1534–1540. doi: 10.2106/00004623-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Bourne RB, Laskin RS, Guerin JS. Ten-year results of the first 100 Genesis II total knee replacement procedures. Orthopedics. 2007;30(8 suppl):83–85. [PubMed] [Google Scholar]
- 8.Bozic KJ, Kinder J, Meneghini RM, Zurakowski D, Rosenberg AG, Galante JO. Implant survivorship and complication rates after total knee arthroplasty with a third-generation cemented system: 5 to 8 years followup. Clin Orthop Relat Res. 2005;430:117–124. doi: 10.1097/01.blo.0000146539.23869.14. [DOI] [PubMed] [Google Scholar]
- 9.Chew JT, Stewart NJ, Hanssen AD, Luo ZP, Rand JA, An KN. Differences in patellar tracking and knee kinematics among three different total knee designs. Clin Orthop Relat Res. 1997;345:87–98. doi: 10.1097/00003086-199712000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Chiu YS, Chen WM, Huang CK, Chiang CC, Chen TH. Fracture of the polyethylene tibial post in a NexGen posterior-stabilized knee prosthesis. J Arthroplasty. 2004;19:1045–1049. doi: 10.1016/j.arth.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 11.Completo A, Fonseca F, Simões JA. Strain shielding in proximal tibia of stemmed knee prosthesis: experimental study. J Biomech. 2008;41:560–566. doi: 10.1016/j.jbiomech.2007.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Dennis DA, Komistek RD, Colwell CE, Jr, Ranawat CS, Scott RD, Thornhill TS, Lapp MA. In vivo anteroposterior femorotibial translation of total knee arthroplasty: a multicenter analysis. Clin Orthop Relat Res. 1998;356:47–57. doi: 10.1097/00003086-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Ewald FC. The Knee Society Total Knee Arthroplasty Roentgenographic Evaluation and Scoring System. Clin Orthop Relat Res. 1989;248:9–12. [PubMed] [Google Scholar]
- 14.Faris PM, Keating EM, Farris A, Meding JB, Ritter MA. Hybrid total knee arthroplasty: 13-year survivorship of AGC total knee systems with average 7 years followup. Clin Orthop Relat Res. 2008;466:1204–1209. doi: 10.1007/s11999-008-0195-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fehring TK, Murphy JA, Hayes TD, Roberts DW, Pomeroy DL, Griffin WL. Factors influencing wear and osteolysis in press-fit condylar modular total knee replacements. Clin Orthop Relat Res. 2004;428:40–50. [DOI] [PubMed]
- 16.Font-Rodriguez DE, Scuderi GR, Insall JN. Survivorship of cemented total knee arthroplasty. Clin Orthop Relat Res. 1997;345:79–86. doi: 10.1097/00003086-199712000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Forster MC. Survival analysis of primary cemented total knee arthroplasty: which designs last? J Arthroplasty. 2003;18:265–270. doi: 10.1054/arth.2003.50051. [DOI] [PubMed] [Google Scholar]
- 18.Gill GS, Joshi AB, Mills DM. Total condylar knee arthroplasty:16- to 21-year results. Clin Orthop Relat Res. 1999;367:210–215. doi: 10.1097/00003086-199910000-00026. [DOI] [PubMed] [Google Scholar]
- 19.Haman JD, Wimmer MA, Galante JO. Surface damage and wear in fixed, modular tibial inserts: the effects of conformity and constraint. In: Bellemans J, Ries MD, Victor J, editors. Total Knee Arthroplasty—A Guide to Get Better Performance. Heidelberg, Germany: Springer; 2005. pp. 85–90. [Google Scholar]
- 20.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed] [Google Scholar]
- 21.Insall J, Salvati E. Patella Position in the normal knee joint. Radiology. 1971;101:101–104. doi: 10.1148/101.1.101. [DOI] [PubMed] [Google Scholar]
- 22.Ip D, Wu WC, Tsang WL. Comparison of two total knee prostheses on the incidence of patella clunk syndrome. Int Orthop. 2002;26:48–51. doi: 10.1007/s00264-001-0316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacobs WC, Clement DJ, Wymenga AB. Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev. 2005;4:CD004803. doi: 10.1002/14651858.CD004803.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Kaplan EL, Meier P. Nonparametric estimation from incomplete observation. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 25.Kavolus CH, Hummel MT, Barnett KP, Jennings JE., Jr Comparison of the Insall-Burstein II and NexGen Legacy total knee arthroplasty systems with respect to patella complications. J Arthroplasty. 2008;23:822–825. doi: 10.1016/j.arth.2007.07.016. [DOI] [PubMed] [Google Scholar]
- 26.Knutson K, Lewold S, Robertsson O, Lidgren L. The Swedish knee arthroplasty register: a nation-wide study of 30, 003 knees 1976–1992. Acta Orthop Scand. 1994;65:375–386. doi: 10.3109/17453679408995475. [DOI] [PubMed] [Google Scholar]
- 27.Li G, Zayontz S, Most E, Otterberg E, Sabbag K, Rubash HE. Cruciate-retaining and cruciate-substituting total knee arthroplasty: an in vitro comparison of the kinematics under muscle loads. J Arthroplasty. 2001;16(8 suppl 1):150–156. doi: 10.1054/arth.2001.28367. [DOI] [PubMed] [Google Scholar]
- 28.Lonner JH, Jasko JG, Bezwada HP, Nazarian DG, Booth RE., Jr Incidence of patellar clunk with a modern posterior-stabilized knee design. Am J Orthop. 2007;36:550–553. [PubMed] [Google Scholar]
- 29.Lonner JH, Klotz M, Levitz C, Lotke PA. Changes in bone density after cemented total knee arthroplasty: influence of stem design. J Arthroplasty. 2001;16:107–111. doi: 10.1054/arth.2001.16486. [DOI] [PubMed] [Google Scholar]
- 30.Ma HM, Lu YC, Kwok TG, Ho FY, Huang CY, Huang CH. The effect of the design of the femoral component on the conformity of the patellofemoral joint in total knee replacement. J Bone Joint Surg Br. 2007;89:408–412. doi: 10.2106/JBJS.D.03054. [DOI] [PubMed] [Google Scholar]
- 31.Mariconda M, Lotti G, Milano C. Fracture of posterior-stabilized tibial insert in a Genesis knee prosthesis. J Arthroplasty. 2000;15:529–530. doi: 10.1054/arth.2000.4810. [DOI] [PubMed] [Google Scholar]
- 32.Miller CW, Pettygrow R. Long-term clinical and radiographic results of a pegged tibial baseplate in primary total knee arthroplasty. J Arthroplasty. 2001;16:70–75. doi: 10.1054/arth.2001.16490. [DOI] [PubMed] [Google Scholar]
- 33.Misra AN, Hussain MR, Fiddian NJ, Newton G. The role of the posterior cruciate ligament in total knee replacement. J Bone Joint Surg Br. 2003;85:389–392. doi: 10.1302/0301-620X.85B3.13182. [DOI] [PubMed] [Google Scholar]
- 34.Most E, Zayontz S, Li G, Otterberg E, Sabbag K, Rubash HE. Femoral rollback after cruciate-retaining and stabilizing total knee arthroplasty. Clin Orthop Relat Res. 2003;410:101–113. doi: 10.1097/01.blo.0000062380.79828.2e. [DOI] [PubMed] [Google Scholar]
- 35.NIH Consensus Statement on total knee replacement. NIH Consens State Sci Statements. 2003;20:1–3. [PubMed]
- 36.Ong A, Wong KL, Lai M, Garino JP, Steinberg ME. Early failure of precoated femoral components in primary total hip arthroplasty. J Bone Joint Surg Am. 2002;84:786–792. doi: 10.2106/00004623-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 37.O’Rourke MR, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Osteolysis associated with a cemented modular posterior-cruciate-substituting total knee design: five to eight-year follow-up. J Bone Joint Surg Am. 2002;84:1362–1371. doi: 10.2106/00004623-200208000-00011. [DOI] [PubMed] [Google Scholar]
- 38.Parsch D, Krüger M, Moser MT, Geiger F. Follow-up of 11–16 years after modular fixed-bearing TKA. Int Orthop. 2009;33:431–435. doi: 10.1007/s00264-008-0543-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pavone V, Boettner F, Fickert S, Sculco TP. Total condylar knee arthroplasty: a long-term followup. Clin Orthop Relat Res. 2001;388:18–25. doi: 10.1097/00003086-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Peters CL, Craig MA, Mohr RA, Bachus KN. Tibial component fixation with cement: full- versus surface-cementation techniques. Clin Orthop Relat Res. 2003;409:158–168. doi: 10.1097/01.blo.0000058638.94987.20. [DOI] [PubMed] [Google Scholar]
- 41.Ritter MA, Berend ME, Meding JB, Keating EM, Faris PM, Crites BM. Long-term followup of anatomic graduated components posterior cruciate-retaining total knee replacement. Clin Orthop Relat Res. 2001;388:51–57. doi: 10.1097/00003086-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 42.Robertsson O, Knutson K, Lewold S, Lidgren L. The Swedish Knee Arthroplasty Register 1975–1997: an update with special emphasis on 41, 223 knees operated on in 1988–1997. Acta Orthop Scand. 2001;72:503–513. doi: 10.1080/000164701753532853. [DOI] [PubMed] [Google Scholar]
- 43.Rodricks DJ, Patil S, Pulido P, Colwell CW., Jr Press-fit condylar design total knee arthroplasty: fourteen to seventeen-year follow-up. J Bone Joint Surg Am. 2007;89:89–95. doi: 10.2106/JBJS.E.00492. [DOI] [PubMed] [Google Scholar]
- 44.Rodriguez JA, Bhende H, Ranawat CS. Total condylar knee replacement: a 20-year followup study. Clin Orthop Relat Res. 2001;388:10–17. doi: 10.1097/00003086-200107000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Rosenberg AG, Andriacchi TP, Barden R, Galante JO. Patellar component failure in cementless total knee arthroplasty. Clin Orthop Relat Res. 1988;236:106–114. [PubMed] [Google Scholar]
- 46.Saleh KJ, Mulhall K, Hofmann A, Bolognesi M, Laskin R. Primary total knee arthroplasty outcomes. In: Barrack R, Booth R, Lonner J, McCarthy J, Mont M, Rubash H, editors. Orthopaedic Knowledge Update: Hip and Knee Reconstruction 3. Chicago, IL: American Academy of Orthopaedic Surgeons; 2006. pp. 93–110. [Google Scholar]
- 47.Sorger JI, Federle D, Kirk PG, Grood E, Cochran J, Levy M. The posterior cruciate ligament in total knee arthroplasty. J Arthroplasty. 1997;12:869–879. doi: 10.1016/S0883-5403(97)90156-X. [DOI] [PubMed] [Google Scholar]
- 48.Sylvain GM, Kassab S, Coutts R, Santore R. Early failure of a roughened surface, precoated femoral component in total hip arthroplasty. J Arthroplasty. 2001;16:141–148. doi: 10.1054/arth.2001.20541. [DOI] [PubMed] [Google Scholar]
- 49.Tanzer M, Smith K, Burnett S. Posterior-stabilized versus cruciate-retaining total knee arthroplasty: balancing the gap. J Arthroplasty. 2002;17:813–819. doi: 10.1054/arth.2002.34814. [DOI] [PubMed] [Google Scholar]
- 50.Thadani PJ, Vince KG, Ortaaslan SG, Blackburn DC, Cudiamat CV. Ten- to 12-year followup of the Insall-Burstein I total knee prosthesis. Clin Orthop Relat Res. 2000;380:17–29. doi: 10.1097/00003086-200011000-00004. [DOI] [PubMed] [Google Scholar]
- 51.Lenthe GH, Willems MM, Verdonschot N, Waal Malefijt MC, Huiskes R. Stemmed femoral knee prostheses: effects of prosthetic design and fixation on bone loss. Acta Orthop Scand. 2002;73:630–637. doi: 10.1080/000164702321039589. [DOI] [PubMed] [Google Scholar]
- 52.Wright RJ, Sledge CB, Poss R, Ewald FC, Walsh ME, Lingard EA. Patient-reported outcome and survivorship after Kinemax total knee arthroplasty. J Bone Joint Surg Am. 2004;86:2464–2470. doi: 10.2106/00004623-200411000-00016. [DOI] [PubMed] [Google Scholar]