Abstract
Background
Adding soluble particulate poragens to antimicrobial-loaded bone cement increases the permeability of the bone cement and increases the antimicrobial release, but the mechanical effect of adding poragens is not well known.
Questions/purposes
We therefore asked the following questions: (1) Does the poragen fraction in antimicrobial-loaded bone cement affect its antimicrobial release? (2) Does poragen fraction in antimicrobial-loaded bone cement affect its compressive strength; and (3) Does the effect on compressive strength change over time in elution?
Methods
Antimicrobial-loaded bone cement made in the proportions of 40 g polymer powder, 20 mL monomer liquid, 1 g tobramycin powder and one of six different doses of poragen powder (0, 1, 2, 4, 8, or 16 g of particulate xylitol per batch) was formed into standardized test cylinders and eluted for 30 days. We determined the cumulative recovered tobramycin and the change in compressive strength over 30 days of elution.
Results
Antimicrobial release progressively increased with increasing poragen fraction. Compressive strength progressively decreased with increasing poragen fraction and with increasing time in elution. Poragen fractions greater than 2 g per batch caused the compressive strength to decrease below 70 MPa over 30 days of elution.
Clinical Relevance
The use of poragens can increase elution of antimicrobials from antimicrobial-loaded bone cement. However, for implant fixation, to avoid deleterious reduction of compressive strength, the amount of poragen that can be added in addition to 1 g of antimicrobial powder may be limited to 2 g per batch.
Introduction
Local delivery of antimicrobials from antimicrobial-loaded bone cement (ALBC) is a recognized modality for the management of established orthopaedic infections, capable of achieving concentrations sufficient to kill bacteria in biofilm [4, 21]. Several studies demonstrate a substantial improvement in controlling infection with the use of ALBC [3, 20]. The antimicrobial dose in the six FDA-approved ALBC products in the United States (0.5–1.0 g aminoglycoside per batch of cement) is limited by the mechanical requirements for implant fixation and is not sufficient for treatment of established infections [10]. Surgeons formulate high-dose ALBC as an off-label application used to treat orthopaedic infections. These formulations are hand-mixed by the surgeon in the operating room with substantially higher antimicrobial doses than their premixed commercial counterparts, using up to 14 g of antimicrobial powder per batch of bone cement [10]. The increased delivery of antimicrobials from high-dose formulations comes at the expense of decreased mechanical strength. Antimicrobial loads greater than 4.5 g per batch cause unacceptable degradation in mechanical properties of the bone cement [3, 5, 12]. In these studies antimicrobial powder is acting as the poragen, not an additional inert particulate powder.
Several authors have explored the addition of an inert poragen to increase antimicrobial release [11, 18]. The increase in permeability is dose- and particle size-dependent [17]. Increased antimicrobial release occurs when a low dose of antimicrobial powder (1 g) is added to bone cement made porous with high doses of inert poragen [18], but mechanical testing was not performed in these studies [11, 17, 18].
We asked if (1) increasing fractions of poragen added to ALBC with 1 g tobramycin progressively increase antimicrobial release from the cement; (2) increasing fractions of poragen added to ALBC progressively decrease its compressive strength; and (3) the mechanical effect caused by adding a poragen to ALBC change over time in elution as the antimicrobial powder diffuses from the pores.
Materials and Methods
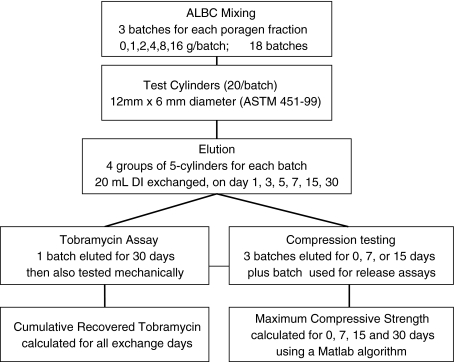
We made 28 ALBC test cylinders with six different poragen doses (0, 1, 2, 4, 8, or 16 g per batch of cement) (Fig. 1). Four groups of five standardized ALBC cylinders for each poragen fraction (20 cylinders per batch) were eluted in 20 mL of deionized water. Total eluant exchange was performed on Days 1, 3, 7, 15, and 30, maintaining infinite sink conditions throughout. One group for each poragen fraction underwent all 5 eluant exchanges and the eluate from that group was assayed for tobramycin concentration. In three groups for each poragen fraction, elution was terminated before 30 days of elution based on the mechanical testing schedule below (Fig. 1). All four groups of cylinders, for each poragen fraction were mechanically tested following completion of elution.
Fig. 1.
A flowchart summarizes the experimental design.
Three groups, one at each time period (7, 15 and 30 days) and one non-eluted group (4 groups total) were mechanically tested to failure in compression, for each poragen fraction. The entire protocol was performed in triplicate, three batches for each poragen fraction (60 cylinders per poragen fraction, total 360 cylinders). All three replicates underwent elution for tobramycin release and mechanical testing.
The ALBC was made using Simplex P® (Stryker, Kalamazoo, MI), mixed in proportions of 40 g polymer powder, 20 mL liquid monomer, 1 g tobramycin sulfate powder (X-gen pharmaceuticals, Northport, NY), and particulate xylitol (XyloSweet®; Xlear, Orem, UT) as the poragen in one of the following doses, 0, 1, 2, 4, 8, or 16 g. The particle size of the xylitol was 106–212 μm using ASTM E-11 sieves [17]. The polymer powder, tobramycin powder, and xylitol powder were first mixed homogeneously using a mixing bowl. The monomer was then added and the ALBC mixed by hand without vacuum. All mixes were half batches to minimize waste. Standardized ALBC test cylinders, 12 mm in length and 6 mm in diameter (ASTM 451-99a1) [1], were made using a Teflon® mold. The ALBC was introduced into the mold in the dough phase and allowed to fully polymerize. The ends of the cylinders were machined square and flat in the mold using low cutting speed to prevent melting and smearing of the polymethylmethacrylate, producing 28 cylinders. Each test cylinder was weighed and precise length and diameter measurements were made. Cylinders were transilluminated under magnification to discard any specimens containing visible defects. Twenty test specimens were then selected randomly from the remaining cylinders for study.
One group of five test cylinders from each of six poragen fractions (0, 1, 2, 4, 8, or 16 g in a batch of cement) was eluted for tobramycin release in glass scintillation vials with 20 mL of deionized water (DI) (Fig. 1). Total eluant exchange was performed on Days 1, 3, 7, 15, and 30, maintaining infinite sink conditions throughout. Tobramycin concentration in the eluate was measured by disc diffusion bioassay using concentration standards on every plate [6]. Each eluate sample was assayed in triplicate and averaged to determine the concentration. Cumulative recovered tobramycin (Mt) was calculated by summing the recovered tobramycin sulfate from all eluant exchanges up to time t. The procedure was repeated for three separate mixes for each poragen fraction.
Compressive strength was measured using four groups of five cylinders (including the group used for tobramycin release assays) made of ALBC from each poragen fraction, eluted as described above, one group after elution durations of 0, 7, 15, and 30 days. Each cylinder was loaded to failure in compression at 24 mm per minute in an MTS Sintech 1/S material test frame (MTS Systems Co, Ltd, Eden Prairie, MN). Load displacement data were analyzed using a custom MATLAB® (The Mathworks Inc, Natick, MA) algorithm to establish the maximum compressive strength in accordance with ASTM Standard 451-99-a1 [1].
We determined differences in antimicrobial release and differences in compressive strength between each poragen fraction using ANOVA.
We determined the effect of time in elution on compressive strength using Repeated Measures ANOVA.
Results
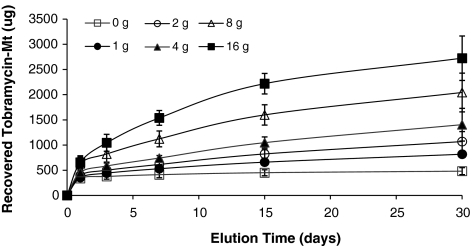
Tobramycin release increased (p < 0.001) with poragen fraction. For ALBC containing 1 g xylitol per batch, 440 μg tobramycin was recovered by 3 days and 816 μg after 30 days (Fig. 2). For ALBC containing 16 g xylitol per batch, 1043 μg tobramycin was recovered by 3 days and 2722 μg after 30 days (Fig. 2).
Fig. 2.
The graph shows a plot of cumulative recovered mass of tobramycin sulfate (Mt) over time in elution (days) for the six different poragen fractions (0, 1, 2, 4, 8, 16 g xylitol). Data are expressed as the mean of five samples at each time point for each poragen fraction; error bars = SD. Tobramycin elution increased with time (p < 0.001) and with poragen fraction (p < 0.001).
Compressive strength decreased with increasing (p < 0.001) poragen fraction.
Compressive strength decreased (p < 0.001) with increasing time in elution. The greatest loss in compressive strength occurred during the first 7 days of elution (Fig. 3). For ALBC with the poragen fraction of 1 g per batch, compressive strength decreased 7.4% to 82 MPa by Day 7 and 10.5% to 79 MPa by Day 30. For the poragen fraction of 16 g per batch, compressive strength decreased 27.8% to 55.3 MPa by Day 7 and 35.4% to 49.5 MPa by Day 30 (Fig. 3). Compressive strength remained above 70 MPa for the duration of the 30 day elution period for poragen fractions of 0, 1, and 2 grams per batch but not for 4, 8, and 16 grams per batch (Fig. 3).
Fig. 3.
The graph shows a plot of compressive strength over time in elution (days) for the six different poragen fractions (0, 1, 2, 4, 8, 16 g xylitol). Data are expressed as the mean of five samples; error bars = SD. Compressive strength decreased with increasing poragen fraction (p < 0.001) and increasing time in elution (p < 0.001). The dashed line represents the control (no antimicrobial) [Ctrl (No Ab)]. The lower horizontal line represents the ISO standard of 70 MPa.
Discussion
Adding soluble inert particulate poragens to ALBC increases its permeability and increases the release of antimicrobials, but the mechanical effect of adding inert poragens has not been adequately studied. We asked whether (1) increasing fractions of poragen added to ALBC would progressively increase its antimicrobial delivery; (2) increasing fractions of poragen added to ALBC would progressively decrease its compressive strength; and (3) the compressive strength of ALBC would change over time in elution.
There are several limitations to our study. First, we performed only in vitro experiments producing pharmacokinetic data. The use of xylitol as a poragen needs to be tested in an in vivo model. Xylitol’s safety for human ingestion and ability to prevent dental caries has been documented in the dental literature [15] making it a desirable choice of particulate poragen material for its apparent antimicrobial effect, but its use in orthopaedic applications has not been clinically studied. The dental literature does not report use of xylitol as a poragen for local antimicrobial delivery, and the flora in the mouth is different from that typically encountered in musculoskeletal infections. Second, the cylinders were only tested uniaxially in compression following the ISO standard for compressive loading of orthopaedic bone cement which designates 70 MPa as the minimum acceptable strength [9]. The mechanical stresses that implant fixation sustains in vivo are much more complicated. Changes in compressive strength are considered to be consistent with the changes in other mechanical properties seen in more complex loading patterns [13]. Although compression is a good indicator of mechanical properties, creep or fatigue testing is necessary to more definitively characterize the mechanical effects from poragens. Third, we tested bone cement from only one manufacturer. The material properties of cements from differing manufacturers vary [2] so similar studies need to be carried out using the other available bone cements. Fourth, tobramycin was the only antimicrobial powder studied, and xylitol was the only poragen studied. Antimicrobial release and mechanical properties of the ALBC may change with the use of different antimicrobials and poragens. Chemical interaction between tobramycin and xylitol was not considered important in this case based upon the structures and water solubilities of xylitol and tobramycin. Interactions between other antimicrobials, poragen materials, and cements could be important. Further studies would be necessary to make determinations about other ALBC formulations.
Finally, the fraction of poragen in this study was calculated in grams per batch (proportional to weight fraction), however, it is volume fraction that determines the pore-forming capacity that leads to the changes in permeability, antimicrobial release, and mechanical performance. Due to the variation in density of antimicrobial powders and poragen materials, the volume fraction can differ by several multiples of the weight fraction with poragens of differing densities. The density of tobramycin formulations can vary by 3.5 times [19]. Volume fraction, determined by direct measurement, not calculated form material properties, is the correct value to use when comparing ALBC formulations made with different poragens. The density of particulate xylitol used in this study, as measured by volume displacement in non-solvent fluid, is 33% greater than PMMA. In this study the weight dose per batch under states the effect by more than 2 times (2 g xylitol per batch = 3.2 wt% = 1.5 vol%). To allow comparison with future investigations of other poragen materials our data should be related to volume fractions of 0.75, 1.50, 3, 5.75, and 11 volume %, not dose weights of 1, 2, 4, 8, and 16 g per batch.
The addition of hydrophilic poragens, such as dextran, glycine, and most antimicrobial powder, has been reported to increase antimicrobial released from ALBC [7, 11, 16–18] (Table 1). Our data are qualitatively consistent with these published data but cannot be quantitatively compared because the volume fraction in those studies is unknown. Hanssen and Spangehl discuss surgeon formulated “high dose” ALBC used to treat active infection, concluding that increased local delivery is achieved with increased antimicrobial dose in the ALBC [7]. McLaren et al. reported that ALBC with large weight fractions of inert poragen increased antimicrobial release from ALBC that contains a low antimicrobial dose compared to ALBC containing the same dose of antimicrobial but no additional inert poragen [18]. In other experiments McLaren et al. showed that the permeability increase caused by poragens is dependent on particle size [17]. Although high doses of antimicrobial powder can act as a poragen, this can be expensive and the particle size of the antimicrobial powder cannot be selected by the orthopaedic surgeon. Using low-cost soluble particulate poragens to increase porosity has the benefit of increasing the delivery of antimicrobials from ALBC using smaller doses of costly antimicrobial powder and the particle size of the poragen is independent of the antimicrobial choice.
Table 1.
The table shows comparison of the results reported by studies based on poragen fraction and type
| Study | Year | Poragen | Poragen fraction | Result |
|---|---|---|---|---|
| (1) Does poragen fraction change antimicrobial release? | ||||
| Hanssen and Spangehl [7] | 2004 | Multiple different antimicrobials | N/A | increasing dose of antimicrobials increases amtimicrobial delivery to the patient |
| Keuchle et al. [11] | 1999 | Dextran | 25 wt% | 25% dextran increases antimicrobial delivery |
| McLaren et al. [18] | 2006 | Xylitol, glycine | 32 vol% | 28 g of xylitol or glycine both increase porosity; porosity increase was greater for xylitol than glycine |
| McLaren et al. [17] | 2007 | Xylitol | 32 vol% | sucrose and xylitol causes similar increase in porosity when controlled for particle size |
| McLaren et al. [16] | 2007 | Sucrose, xylitol, erythritol | 32 vol% | all three fillers increase porosity of PMMA |
| Nugent et al. [current study] | 2009 | Xylitol | 0.75, 1.50, 3, 5.75, 11 vol% | xylitol (100–200 μm particle size) produced porosity leading to dose dependent increased antimicrobial delivery |
| (2) Does poragen fraction change compressive strength? | ||||
| Lautenschlager et al. [12] | 1976 | Gentamicin sulfate | 0, 3, 7, 14 wt% | gentamicin sulfate caused dose dependent loss in compressive strength but elution did not decrease strength. |
| Lewis and Bhattaram [13] | 2006 | Gentamicin sulfate | 4.22 wt% | low dose ALBC did not decrease mechanical properties for multiple different t cements |
| Nugent et al. [current study] | 2009 | Xylitol | 0.75, 1.50, 3, 5.75, 11 vol% | increasing amounts of xylitol caused dose dependant decrease in compressive strength |
| (3) Does the effect of poragen fraction on compressive strength change over time? | ||||
| Lewis and Janna [14] | 2006 | Gentamicin | 2.2, 4.25, 11/50 wt% | increasing antibiotic load causes a dose dependent reduction in fatigue life under elution |
| He et al. [8] | 2002 | Gentamicin | 0, 1.7, 3.4, 6.5, 9.4 wt% | above 3–4 wt%, compressive strength decreases with time in elution |
| Nugent et al. [current study] | 2009 | Xylitol | 0.75, 1.50, 3, 5.75, 11 vol% | increasing poragen fraction caused dose dependent loss of compressive strength and that loss of compressive strength progressed with time in elution |
Our results are also consistent with the observations of other investigators who report compressive strength of ALBC progressively decreases with increasing dose of antimicrobial powder (Table 1) [12, 13]. Lautenschlager et al. reported decreasing compressive strength of ALBC caused by adding increasing amounts of antimicrobial powder per batch of cement, without elution [12]. Lewis and Bhattaram reviewed several investigations studying different antimicrobials, doses and cement manufacturers [13]. These reviewed data have conflicting results showing strength degradation caused by adding poragens in some and not in others. This led Lewis and Bhattaram to study compressive strength of ALBC containing different amounts of antimicrobial powder. Low dose ALBC (1 g per batch) had no difference in compression strength and fatigue properties of the ALBC compared to control cement without any antimicrobial powder [13]. In comparison, our Day 0 compressive strength did decrease for poragen fractions of 2 g per batch or less, and our Day 1–30 data showed increasing loss of compressive strength following elution, for doses of 4 g per batch and greater.
The mechanical strength of ALBC related to time in elution is less extensively studied. Lewis and Janna reported decreasing fatigue life of ALBC with increasing time in elution [14], which is consistent with our data showing decreasing compressive strength as the time in elution increases. He et al. similarly found that compression strength of ALBC decreased substantially after 48 weeks of elution for 4 g and 6 g of gentamicin per batch of cement; however, the density of the gentamicin is unknown [8], Therefore volume percent cannot be calculated for comparison with other data.
Our data show increasing poragen fraction in ALBC leads to increasing antimicrobial release and decreasing compressive strength, and increasing time in elution leads to decreasing compressive strength of ALBC.
Acknowledgments
We thank Himanshu Kaul BSE for assistance with this study.
Footnotes
All the authors received funding from the Herbert T. Lewis Fund in the Orthopaedic Research and Education Foundation.
This work was performed at Banner Good Samaritan Medical Center, Phoenix AZ and the Center for Interventional Biomaterials, Arizona State University, Tempe AZ.
References
- 1.American Society for Testing and Materials. Standard Specifications for Acrylic Bone Cement. F451-99. West Conshohocken, PA: American Society for Testing and Materials; 2002.
- 2.Belkoff SM, Maroney M, Fenton DC, Mathis JM. An in vitro biomechanical evaluation of bone cements used in percutaneous vertebroplasty. Bone. 1999;25(2 Suppl 1):23S–26S. doi: 10.1016/S8756-3282(99)00128-3. [DOI] [PubMed] [Google Scholar]
- 3.Cui Q, Mihalko WM, Shields JS, Ries M, Saleh KJ. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J Bone Joint Surg Am. 2007;89:871–882. doi: 10.2106/JBJS.E.01070. [DOI] [PubMed] [Google Scholar]
- 4.Diefenbeck M, Mückley T, Hofmann GO. Prophylaxis and treatment of implant-related infections by local application of antibiotics. Injury. 2006;37(2 Suppl 1):S95–S104. doi: 10.1016/j.injury.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 5.Duncan CP, Masri BA. The role of antibiotic-loaded cement in the treatment of an infection after a hip replacement. Instr Course Lect. 1995;44:305–313. [PubMed] [Google Scholar]
- 6.Fernandes PB, Ramer N, Rode RA, Freiberg L. Bioassay for A-56268 (TE-031) and identification of its major metabolite, 14-hydroxy-6-methyl erythromycin. Eur J Clin Microbiol Infect Dis. 1988;7:73–76. doi: 10.1007/BF01962181. [DOI] [PubMed] [Google Scholar]
- 7.Hanssen AD, Spangehl MJ. Practical applications of antibiotic-loaded bone cement for treatment of infected joint replacements. Clin Orthop Relat Res. 2004;427:79–85. doi: 10.1097/01.blo.0000143806.72379.7d. [DOI] [PubMed] [Google Scholar]
- 8.He Y, Trotignon JP, Loty B, Tcharkhtchi A, Verdu J. Effect of antibiotics on the properties of poly(methylmethacrylate)-based bone cement. J Biomed Mater Res. 2002;63:800–806. doi: 10.1002/jbm.10405. [DOI] [PubMed] [Google Scholar]
- 9.International Organization for Standardization. Implants for Surgery—Acrylic Resin Cements. ISO 5833-2002. Geneva, Switzerland: International Organization for Standardization; 2002.
- 10.Jiranek WA, Hanssen AD, Greenwald AS. Antibiotic-loaded bone cement for infection prophylaxis in total joint replacement. J Bone Joint Surg Am. 2006;88:2487–2500. doi: 10.2106/JBJS.E.01126. [DOI] [PubMed] [Google Scholar]
- 11.Kuechle DK, Landon GC, Musher DM, Noble PC. Elution of vancomycin, daptomycin, and amikacin from acrylic bone cement. Clin Orthop Relat Res. 1991;264:302–308. [PubMed] [Google Scholar]
- 12.Lautenschlager EP, Jacobs JJ, Marshall GW, Meyer PR., Jr Mechanical properties of bone cements containing large doses of antibiotic powders. J Biomed Mater Res. 1976;10:929–938. doi: 10.1002/jbm.820100610. [DOI] [PubMed] [Google Scholar]
- 13.Lewis G, Bhattaram A. Influence of a pre-blended antibiotic (gentamicin sulfate powder) on various mechanical, thermal, and physical properties of three acrylic bone cements. J Biomater Appl. 2006;20:377–408. doi: 10.1177/0885328206055124. [DOI] [PubMed] [Google Scholar]
- 14.Lewis G, Janna S. Estimation of the optimum loading of an antibiotic powder in an acrylic bone cement. Acta Orthopaedica. 2006;77:622–627. doi: 10.1080/17453670610012700. [DOI] [PubMed] [Google Scholar]
- 15.Makinen KK, Bennett CA, Hujoel PP, Isokangas PJ, Isotupa KP, Pape HR, Jr, Makinen PL. Xylitol chewing gums and caries rates: a 40-month cohort study. J Dent Res. 1995;74:1904–1913. doi: 10.1177/00220345950740121501. [DOI] [PubMed] [Google Scholar]
- 16.McLaren AC, McLaren SG, Hickmon MK. Sucrose, xylitol, and erythritol increase PMMA permeability for depot antibiotics. Clin Orthop Relat Res. 2007;461:60–63. doi: 10.1097/BLO.0b013e31811f350d. [DOI] [PubMed] [Google Scholar]
- 17.McLaren AC, McLaren SG, McLemore R, Vernon BL. Particle size of fillers affects permeability of polymethylmethacrylate. Clin Orthop Relat Res. 2007;461:64–67. doi: 10.1097/BLO.0b013e31811f350d. [DOI] [PubMed] [Google Scholar]
- 18.McLaren AC, McLaren SG, Smeltzer M. Xylitol and glycine fillers increase permeability of PMMA to enhance elution of daptomycin. Clin Orthop Relat Res. 2006;451:25–28. doi: 10.1097/01.blo.0000229321.53040.a1. [DOI] [PubMed] [Google Scholar]
- 19.McLaren RL, McLaren AC, Vernon B. Generic Tobramycin elutes from bone cement faster than proprietary Tobramycin. Clin Orthop Relat Res. 2008;466:1372–1376. doi: 10.1007/s11999-008-0199-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Osterman PA, Seligson D, Henry SL. Local antibiotic therapy for severe open fractures: a review of 1085 consecutive cases. J Bone Joint Surg Br. 1995;77:93–97. [PubMed] [Google Scholar]
- 21.Belt H, Neut D, Schenk W, Horn JR, Mei HC, Busscher HJ. Staphylococcus aureus biofilm formation on different gentamicin-loaded polymethylmethacrylate bone cements. Biomaterials. 2001;22:1607–1611. doi: 10.1016/S0142-9612(00)00313-6. [DOI] [PubMed] [Google Scholar]