Abstract
Aims
To compare the medical costs and prevalence of health conditions of family members of persons with an alcohol or drug dependence (AODD) diagnosis to family members of persons with diabetes and asthma.
Setting
Kaiser Permanente of Northern California (KPNC)
Participants
Family members of persons diagnosed with AODD between 2002 and 2005, and matched samples of family members of persons diagnosed with diabetes and asthma.
Measurements
Logistic regression was used to determine whether the family members of persons with AODD were more likely to be diagnosed with medical conditions than family members of persons with diabetes or asthma. Multivariate models were used to compare health services cost and utilization of AODD family members and diabetes and asthma family members. Analyses were for the year before, and two years after, initial diagnosis of the index person.
Findings
In the year before initial diagnosis of the index person, AODD family members were more likely to be diagnosed with substance use disorders, depression and trauma than diabetes or asthma family members. AODD family members had higher total health care costs than diabetes family members in the year after, and the second year after, the index date ($217 and $293, respectively). AODD family members had higher total health care costs than asthma family members in the year before, and second year after, the index date ($104 and $269, respectively).
Conclusions
AODD family members have unique patterns of health conditions compared to the diabetes and asthma family members, and have similar, or higher, health care cost and utilization.
Keywords: alcohol, drug, dependence, costs, family, diabetes, asthma
Introduction
Having a family member with an alcohol or drug problem affects family functioning and dynamics[1–4], which may lead to increased risk of developing patterns of illness and behavioral problems [5]. A number of studies have shown that family members of alcoholics, or persons with an alcohol or drug disorder, have increased prevalence of medical and psychiatric conditions, and increased medical cost and utilization, compared to the family members of persons without alcohol or drug disorders [5–11]. No studies, however, have investigated how these persons compare to the family members of person with other chronic conditions.
The literature on the effect of chronic illness and disabilities on family health describes how disability and chronic illness affect the whole family [1, 12]. Studies show that resource limits and stress are likely to affect utilization and cost of family members with a disabled parent or child [12]. This is consistent with a conceptual framework of family functioning which suggests that more stressful home environments, such as those with families of individuals with alcohol use disorders, results in poorer functioning and worse physical symptoms [13]. In general, the literature argues that disabilities and chronic health problems result in increased disease risk and emotional or behavioral problems in family members [1, 12]. If substance use disorders are to be viewed as chronic illnesses, the question arises whether the effects (in terms of health conditions and healthcare utilization) on family members of persons with these disorders are similar to those of persons with other chronic conditions.
Alcohol and drug dependence share many features with other chronic illnesses[14], and other chronic illnesses, such as diabetes and asthma, also have negative effects on the psychological health of family members [15, 16], which may cause increased use of health services. In a review article that argued for treating drug dependence as a chronic condition, McLellan et al. demonstrated that with respect to vulnerability, onset, and course, drug dependence is similar to other chronic conditions such as type 2 diabetes and asthma [14]. Extending this analogy, we compare the prevalence of health conditions, and the utilization and cost of medical services, of the family members of persons with an alcohol or drug dependence diagnosis (AODD) to those of the family members of persons with diabetes and asthma. These conditions were selected because of the McClellan review, as well as their high prevalence in the population and diversity with respect to etiology and age of onset. For comparison, we also include the family members of persons without AODD who visited a primary care department for any reason. Our focus in this paper is on the years immediately surrounding the time when the person was diagnosed with AODD, diabetes or asthma.
Methods
Setting
Kaiser Permanente of Northern California (KPNC) is a nonprofit, integrated health care delivery system providing comprehensive health services to more than 3.2 million members. KPNC operates over 54 outpatient clinics and 16 hospitals. All persons included in this study were drawn from KPNC membership.
Selection of potential index persons
To compare family members of persons with AODD to family members of persons with diabetes and asthma, we first identified persons with AODD, persons with diabetes, and persons with asthma. The following process was performed for each condition to identify the pool of potential index persons. Using automated clinical databases [17], we identified all visits and hospitalizations at KPNC facilities between January 1, 2001 and December 31, 2005 during which a diagnosis for one of the conditions of interest was made. We then selected the first encounter for each person (between 2002 and 2005) that was not preceded by another such encounter within the prior year. The “index date” was the date of this first encounter. The following ICD-9-CM codes were used to define conditions: 303 and 304 (“Alcohol dependence syndrome”, “Drug dependence”); 250 (“Diabetes mellitus”); 493 (“Asthma”). Diagnoses can be made in any health plan department and a diagnosis does not mean that the person has received specialty substance use, diabetes, or asthma treatment. The result was a pool of potential index persons for each condition. We also identified a pool of persons who visited a primary care department but who were not diagnosed with AODD between 2002 and 2005. For this group, we extracted all primary care visits between 2002 and 2005, then randomly selected 500,000 persons who made at least one visit during this time (and who did not receive an AODD diagnosis), then randomly selected one visit as the index visit.
Selection of index persons included in analyses
Our goal was to compare the family members of persons with AODD to family members of, for example, persons with diabetes. To focus the analysis on the difference in the impact of AODD and diabetes on family members, we wanted the index persons to be as similar as possible in all other respects. We therefore performed a matching process whereby persons in the pool of potential index AODD persons were matched (one to one) to persons in the pool of potential diabetes persons by gender, age (within 5 years), year of index visit, membership status (subscriber, spouse, or dependent), and medical costs in the year before the index visit (within $500 dollars up to $5000, within $1000 up $10,000, within $5000 up to $25,000, within $25,000 up to $50,000, and over $50,000). We matched by medical costs for two reasons. First, to control in some way for severity of the index person. In this context, we view health care costs as a proxy for severity. Second, we were concerned that if AODD index persons were higher utilizers of health care services than diabetes or asthma index persons, this may reflect a higher propensity to use services, and the other members of the family might share similar propensities to use services. By requiring that AODD index persons had similar resource use to their matched diabetes and asthma index persons, we largely removed these as explanatory factors. This was a conservative approach taken to enhance our ability to interpret the results as relating to the condition per se rather than to family correlations of service use. Only index persons who were continuous members of KPNC in the year before their index date and who had family members during the index month were eligible to be matched. Furthermore, no overlap was allowed between person groups – e.g., AODD persons who also had diabetes were ineligible to be index persons in that comparison.
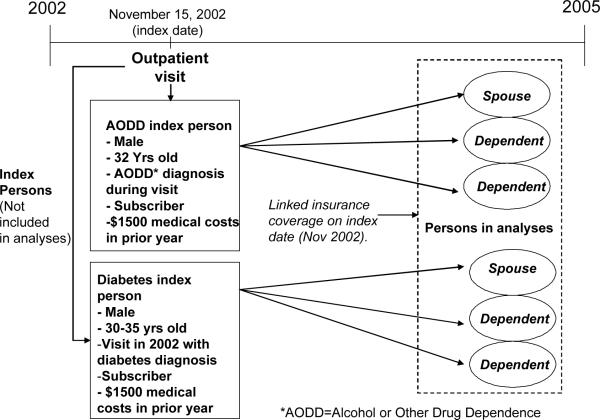
Figure 1 illustrates an example of a matched pair of index AODD and diabetes persons. After matching AODD index persons to diabetes index persons, we then matched them to asthma persons and non-AODD persons, each in a separate process. This resulted in a somewhat different set of AODD index persons in each analysis. Thus, the cohort of AODD family members that were compared to diabetes family members was somewhat different from the cohort that was compared to asthma family members or to non-AODD family members.
Figure 1.
Example of Selection of Family Members
Identification of family members
We identified all KPNC members who were family members of the index persons during the month of the index date. Similar to other recent studies,[6, 18] we defined the family from the health plan perspective: persons who shared a membership account number (during the index month) with the index persons. The KPNC membership account number links together subscribers and their spouses and dependents. Regardless of whether the index person was the subscriber, a spouse, or a dependent, this method identified the other members to whom their coverage was connected. We refer to these family members by the condition of the index person: “AODD family members”, “diabetes family members”, “asthma family members”, and “non-AODD family members”. Family members were included in analyses only if they were continuous members of KPNC throughout the analysis year and were a family member of the index person in that year.
Medical conditions
We extracted from KPNC automated databases all inpatient and outpatient diagnoses received by each family member in the year before their index date. We selected, a priori, a list of 24 conditions shown to account for about 80% of adult medical costs in this health plan[19] (broadening HIV to include all sexually transmitted diseases, and excluding pregnancy), and augmented that list with three conditions especially prevalent in children (attention-deficit/hyperactivity disorder (ADHD), behavioral problems, and otitis media). As we have done in other work,[6] we used the Johns Hopkins ACG Case-Mix system (version 8.0) to group diagnoses into Expanded Diagnosis Clusters (EDCs). The EDC methodology assigns ICD codes to one of 264 EDCs. We then mapped these EDCs to our list of conditions. For example, our condition “hypertension” was a mapping of the EDCs “CAR14” (“Hypertension w/o major complications”) and “CAR15” (“Hypertension w/ major complications”). (For a list of the mappings, see Table 2). The prevalence of each condition was determined separately for adults and children, and only conditions having at least 2% prevalence among either the AODD or comparison family members were used for subsequent analysis.
Table 2.
Prevalence of medical and mental health conditions in the year before the index date: Family members of AODD persons compared to family members of diabetes persons.
| Number (Percent) of persons receiving medical diagnoses during year | ||||||
|---|---|---|---|---|---|---|
| Adults | Children | |||||
| Medical/Mental Health Conditions‡ | Family members of AODD persons (N=20224) | Family members of diabetes persons (N=21381) | Odds Ratio (95% CI)§ | Family members of AODD persons (N=16342) | Family members of diabetes persons (N=16314) | Odds Ratio (95% CI)§ |
| Acid related disorders (GAS01, GAS06, GAS08) | 1347 (6.7) | 1515 (7.1) | 0.92 (0.85 to 0.99)* | ¶ | ¶ | ¶ |
| Asthma (ALL04, ALL05) | 1164 (5.8) | 1270 (5.9) | 0.94 (0.86 to 1.02) | 1397 (8.5) | 1505 (9.2) | 0.91 (0.84 to 0.98)* |
| Attention deficit disorder (PSY05) | ¶ | ¶ | ¶ | 602 (3.7) | 431 (2.6) | 1.33 (1.17 to 1.52)* |
| Depression (PSY09) | 1153 (5.7) | 702 (3.3) | 1.74 (1.58 to 1.92)* | ¶ | ¶ | ¶ |
| Diabetes (END06–END09, EYE13) | 1044 (5.2) | 1538 (7.2) | 0.69 (0.63 to 0.75)* | ¶ | ¶ | ¶ |
| Hypertension (CAR14, CAR15) | 2728 (13.5) | 3168 (14.8) | 0.86 (0.80 to 0.91)* | ¶ | ¶ | ¶ |
| Lower Back Pain (MUS14) | 2273 (11.2) | 2375 (11.1) | 0.99 (0.93 to 1.06) | ¶ | ¶ | ¶ |
| Otitis media (EAR01) | 778 (3.8) | 819 (3.8) | 0.98 (0.88 to 1.08) | 2377 (14.5) | 2218 (13.6) | 1.07 (1.00 to 1.4)* |
| Pneumonia (RES02) | 1098 (5.4) | 1119 (5.2) | 1.02 (0.93 to 1.11) | 703 (4.3) | 758 (4.6) | 0.91 (0.82 to 1.01) |
| Substance use disorders (PSY02) | 872 (4.3) | 400 (1.9) | 2.33 (2.06 to 2.63)* | ¶ | ¶ | ¶ |
| Trauma (EYE12, GSU12, MUS02, MUS04, MUS08, MUS09, NUR15, NUR16, REC03, REC04, SKN01) | 3295 (16.3) | 2936 (13.7) | 1.20 (1.13 to 1.26)* | 3184 (19.5) | 2603 (16.0) | 1.22 (1.15 to 1.29)* |
Conditions were a subset of 25 conditions that represent about 80% of KP's health care spending (Ray, 2000), plus ADHD, behavior problems, and otitis media, which were considered a priori to be conditions more prevalent among children. The subset consists of those conditions that occurred in at least 2% of either the AODD family members or the comparison family members, and excluded pregnancy. Conditions of the uterus and headache met the 2% criterion, but are not included in this table because there were no significant differences in these conditions in any of the comparisons.
Conditions were identified by grouping relevant Expanded Diagnosis Clusters (EDCs) as defined by the Johns Hopkins ACG Case-Mix System. The EDCs used are in parentheses. Conditions that did not reach 2% prevalence were: arthritis, behavior problems, benign prostatic hyperplasia, breast cancer, chronic obstructive pulmonary disorder, congestive heart failure, colorectal cancer, cerebrovascular disease, ischemic heart disease, lung cancer, prostate cancer, psychoses, and renal failure.
Odds ratio from logistic regression adjusting for gender, age, age-squared, income (in quintiles based on median family income by census block group from the 2000 US census), primary facility where member received care, family size(as a categorical variable), gender of the index person, role of the index person (subscriber, spouse or dependent), and cost of the index person in the year before the index date.
Both family groups had less than 2% of persons with this condition
Difference between family members of AODD persons and family members of diabetes persons was significant at p<=0.05, after adjusting for covariables.
Cost and Utilization Data
For each family member, we estimated the cost of health services received between January 1, 2001 and December 31, 2005. All analyses were restricted to the year before, and the two years after, the index date. Costs for services provided directly by KPNC were obtained from the Cost Management Information System, an automated system that integrates hospital, emergency department, outpatient visit, laboratory and radiology databases with the program's financial ledger. Costs (including program and facility overhead) are generated for each service, as defined by the system, using standard accounting methods and program-specific relative value units for each service. We used these cost data to estimate the average cost of: (1) hospitalizations by Diagnosis Related Group (DRG) and within DRG, by length of stay; (2) emergency department (ED) visits; (3) outpatient office visits by department (e.g., “Pediatrics”, “Psychiatry”) and provider type (e.g., “physician”, “registered nurse”). Hospitalizations, ED visits, and office visits were extracted from automated databases and assigned the costs described above. Pharmacy costs were obtained from KPNC's Pharmacy Information Management System, an automated clinical database that records each prescription drug dispensed at any of the outpatient pharmacies in the KPNC system, along with the medication acquisition cost.
For covered services provided by non-KPNC vendors, we used the payments made by KPNC to those vendors as the cost of those services. Costs not included in these analyses were dental costs, patient out-of-pocket expenses, and certain administrative and overhead costs associated with health plan membership (such as marketing expense). The Consumer Price Index was used to adjust all costs to 2005 dollars. Two measures of utilization were included in the analyses: Number of inpatient hospital days and number of outpatient visits to KP providers.
Analyses
To analyze if the prevalence of medical conditions was higher among AODD family members than comparison family members, we constructed a dataset with one record per person and a flag indicating if they did or did not receive a diagnosis for each of the selected conditions in the year before their index date. To test for differences in the prevalence of the conditions, we used logistic regression, controlling for gender, age, age-squared, income (in quintiles based on median family income by census block group from the 2000 US census), family size (as a categorical variable), primary facility used by the member, gender of the index person, role of the index person (subscriber, spouse or dependent), and cost of the index person in the year before the index date. Models were run separately for adults (18 years of age and over) and children.
To analyze cost and utilization, we created a cost dataset consisting of a record for each family member for the year before, and the two years after, their index date. “Year −1” (year negative one) was the year before the index date. All results are per person and the costs of the index AODD and comparison persons were not included in any analyses.
For each year, we ran a general linear model in which cost was the dependent variable. In these models we also adjusted for gender and age at index date (as a categorical variable with 18 age levels, in five year increments, for each gender), census-block income, family size, primary facility used by the member, gender and age of the index person, role of the index person, and cost of the index person in the year of analysis. The cost subgroups separately assessed were: hospital, emergency department, outpatient primary care (consisting of the departments of medicine, family practice, pediatrics and gynecology), outpatient psychiatry department, chemical dependency (CD) treatment, pharmacy, and other outpatient services (e.g., specialty department visits like optometry or neurology, as well as covered outpatient services provided by non-KP providers). To account for correlation among family members, we tested including “family” as a random effect. However, because the pattern of results and confidence intervals of preliminary analyses were virtually identical, and because the hierarchical model was far more computationally intensive, we did not include the random effect in our final models. To test how sensitive the cost results were to outliers, we reran the model excluding 23 persons with total costs over $500,000. Statistical analyses were performed using SAS software (Cary, NC).
Results
Subject characteristics
There were 25,464 eligible index AODD persons of which 17,345 were matched to an index diabetes person, 19,930 to an index asthma person, and 20,320 to a Non-AODD person. (Many index AODD persons found matches in all three comparison groups.)
Because index person gender, age, and health care costs were used to match, AODD index persons were virtually identical to the index persons of the comparison groups. For example, the AODD index persons, and the diabetes index persons to whom they were matched, were, on average, 47 years of age, had medical costs of about $5300 in the year before their index dates, and 66% were male (Table 1). AODD family members had a somewhat different age distribution, lived in census blocks with lower income, and were from smaller families than diabetes family members. Compared to asthma family members, AODD family members lived in census blocks with lower income, were from smaller families, and were more costly. Compared to family members of the random group of non-AODD persons, AODD family members were more likely to be female, had a somewhat different age distribution, lived in census blocks with lower income, were from smaller families, and were more costly.
Table 1.
Demographic characteristics of family members of persons with alcohol or other drug dependence (AODD) diagnosis and family members of persons with diabetes, asthma, and visits to primary care in the year before the index date.†
| Characteristics | Family Members of AODD Persons Used for Comparisons to Family Members of Diabetes Persons (N=36566) | Family Members of Diabetes Persons (N=37695) | Family Members of AODD Persons Used for Comparisons to Family Members of Asthma Persons (N=44933) | Family Members of Asthma Persons (N=46787) | Family Members of AODD Persons Used for Comparisons to Family Members of Non-AODD Persons (N=45441) | Family Members of Non-AODD Persons (N=46511) |
|---|---|---|---|---|---|---|
| Gender§ | ||||||
| Male | 15638 (43) | 16358 (43) | 20133 (45) | 21171 (45) | 20028 (44) | 20824 (45) |
| Female | 20928 (57) | 21337 (57) | 24800 (55) | 25616 (55) | 25413 (56) | 25687 (55) |
| Age group (%) *§ | ||||||
| 00–<19 years old | 17646 (48) | 17639 (47) | 20457 (46) | 21013 (45) | 20751 (46) | 20578 (44) |
| 19–<45 years old | 9729 (27) | 10413 (28) | 12502 (28) | 13621 (29) | 12538 (28) | 13503 (29) |
| 45–<65 years old | 7884 (22) | 8338 (22) | 10732 (24) | 10972 (24) | 10811 (24) | 11147 (24) |
| 65+ years old | 1307 (4) | 1305 (3) | 1242 (3) | 1181 (3) | 1341 (3) | 1283 (3) |
| Mean age of family members at index date | 28.2 | 28.4 | 28.8 | 28.6 | 28.9 | 29.0 |
| Income based on census block group*ठ| ||||||
| 1st (bottom) quintile | 7331 (20) | 7727 (20) | 8851 (20) | 8162 (17) | 8955 (20) | 7909 (17) |
| 2nd quintile | 7087 (19) | 7328 (19) | 8562 (19) | 8392 (18) | 8847 (19) | 7891 (17) |
| 3rd quintile | 6837 (19) | 6559 (17) | 8441 (19) | 8694 (19) | 8546 (19) | 8437 (18) |
| 4th quintile | 6534 (18) | 6729 (18) | 8018 (18) | 8724 (19) | 8084 (18) | 8785 (19) |
| 5th (top) quintile | 5496 (15) | 5629 (15) | 7013 (16) | 8960 (19) | 6977 (15) | 9347 (20) |
| Unknown | 3281 (9) | 3723 (10) | 4048 (9) | 3855 (8) | 4032 (9) | 4142 (9) |
| Family Size *ठ| ||||||
| 2 | 7012 (19) | 6732 (18) | 6907 (15) | 6480 (14) | 7232 (16) | 6908 (15) |
| 3 | 6437 (18) | 6493 (17) | 7908 (18) | 7783 (17) | 7936 (17) | 8051 (17) |
| 4 | 11085 (30) | 11476 (30) | 14067 (31) | 15050 (32) | 14155 (31) | 14989 (32) |
| 5+ | 12032 (33) | 12994 (34) | 16051 (36) | 17474 (37) | 16118 (35) | 16563 (36) |
| Unadjusted mean total cost of health services ($)ठ| 2255 | 2138 | 2235 | 2102 | 2233 | 2020 |
| Characteristics of index persons | ||||||
| Number of index persons | 17345 | 17329 | 19930 | 19975 | 20320 | 20329 |
| Percent of index persons that were male | 66 | 66 | 63 | 63 | 64 | 64 |
| Mean age of index person at index date | 47 | 47 | 42 | 42 | 42 | 42 |
| Unadjusted mean total cost of health services for the index person ($) | 5209 | 5318 | 4096 | 4003 | 4355 | 4173 |
Family members were the family members of an “index” person who had a visit or hospitalization in which they received a diagnosis of AODD, diabetes or asthma, or (for the non-AODD group), who had any visit to a primary care department, but were not diagnosed with AODD between 2002 and 2005. Each index person was assigned an index date which was the date that the person was first diagnosed with their condition (between 2002 and 2005, without a prior diagnosis of that condition in the previous year). For non-AODD index persons, the index date was the date of a randomly chosen primary visit between 2002 and 2005. AODD index persons were then matched (1:1) to the diabetes, asthma, and non-AODD index persons by age, gender, month of the index date, membership role (subscriber, spouse, or dependent), and health care costs in the year before the index date. Matching was performed separately for each comparison group, resulting in three different sets of AODD index persons. Index persons who did not match were dropped. “Family members” of index persons do not include the index person.
Family members of AODD persons were significantly different from family members of diabetes persons at p<=0.05.
Family members of AODD persons were significantly different from family members of asthma persons at p<=0.05.
Family members of AODD persons were significantly different from family members of non-AODD persons at p<=0.05.
Prevalence of diagnosed medical conditions
Thirteen medical conditions were diagnosed in more than 2% of adults (in any of the family groups), and six conditions were diagnosed in more than 2% of children. In the year before the index date, adult AODD family members were less likely to be diagnosed with acid related disorders, diabetes, and hypertension than adult diabetes family members, and were more likely to be diagnosed with depression, substance use disorders and trauma (Table 2). Child AODD family members were more likely to be diagnosed with ADHD, otitis media and trauma than child diabetes family members, and less likely to be diagnosed with asthma. Compared to adult family members of asthma persons, adult AODD family members were less likely to be diagnosed with acid related disorders, asthma, diabetes, and otitis media, and were more likely to be diagnosed with depression, substance use disorders and trauma (Table 3). Child AODD family members were less likely to be diagnosed with asthma, otitis media, and pneumonia than child asthma family members, but were more likely to be diagnosed with ADHD and trauma. Compared to adult non-AODD family members, adult AODD family members were less likely to be diagnosed with diabetes, but were more likely to be diagnosed with depression, lower back pain, pneumonia, substance use disorders and trauma (Table 4). Child AODD family members were more likely to be diagnosed with ADHD and trauma than child non-AODD family members.
Table 3.
Prevalence of medical and mental health conditions in the year before the index date: Family members of AODD persons compared to family members of asthma persons.
| Number (Percent) of persons receiving medical diagnoses during year | ||||||
|---|---|---|---|---|---|---|
| Adults | Children | |||||
| Medical/Mental Health Conditions‡ | Family members of AODD persons (N=25996) | Family members of asthma persons (N=27268) | Odds Ratio (95% CI)§ | Family members of AODD persons (N=18937) | Family members of asthma persons (N=19519) | Odds Ratio (95% CI)§ |
| Acid related disorders (GAS01, GAS06, GAS08) | 1696 (6.5) | 1890 (6.9) | 0.93 (0.86 to 0.99)* | ¶ | ¶ | ¶ |
| Asthma (ALL04, ALL05) | 1434 (5.5) | 1726 (6.3) | 0.87 (0.81 to 0.94)* | 1617 (8.5) | 2512 (12.9) | 0.64 (0.60 to 0.69)* |
| Attention deficit disorder (PSY05) | ¶ | ¶ | ¶ | 708 (3.7) | 616 (3.2) | 1.19 (1.06 to 1.33)* |
| Depression (PSY09) | 1535 (5.9) | 1117 (4.0) | 1.45 (1.34 to 1.57)* | ¶ | ¶ | ¶ |
| Diabetes (END06–END09, EYE13) | 1327 (5.1) | 1612 (5.9) | 0.82 (0.76 to 0.89)* | ¶ | ¶ | ¶ |
| Hypertension (CAR14, CAR15) | 3290 (12.7) | 3428 (12.6) | 0.97 (0.92 to 1.03) | ¶ | ¶ | ¶ |
| Lower Back Pain (MUS14) | 2892 (11.1) | 2992 (11.0) | 1.01 (0.96 to 1.07) | ¶ | ¶ | ¶ |
| Otitis media (EAR01) | 983 (3.8) | 1158 (4.2) | 0.89 (0.81 to 0.97)* | 2786 (14.7) | 3317 (17.0) | 0.91 (0.86 to 0.97)* |
| Pneumonia (RES02) | 1347 (5.2) | 1482 (5.4) | 0.95 (0.88 to 1.02) | 811 (4.3) | 1225 (6.3) | 0.71 (0.64 to 0.78)* |
| Substance use disorders (PSY02) | 1086 (4.2) | 598 (2.2) | 1.94 (1.75 to 2.15)* | ¶ | ¶ | ¶ |
| Trauma (EYE12, GSU12, MUS02, MUS04, MUS08, MUS09, NUR15, NUR16, REC03, REC04, SKN01) | 4234 (16.3) | 4087 (15.0) | 1.10 (1.05 to 1.15)* | 3634 (19.2) | 3625 (18.6) | 1.03 (0.98 to 1.09) |
Conditions were a subset of 25 conditions that represent about 80% of KP's health care spending (Ray, 2000), plus ADHD, behavior problems, and otitis media, which were considered a priori to be conditions more prevalent among children. The subset consists of those conditions that occurred in at least 2% of either the AODD family members or the comparison family members, and excluded pregnancy. Conditions of the uterus and headache met the 2% criterion, but are not included in this table because there were no significant differences in these conditions in any of the comparisons. Conditions were identified by grouping relevant Expanded Diagnosis Clusters (EDCs) as defined by the Johns Hopkins ACG Case-Mix System. The EDCs used are in parentheses. Conditions that did not reach 2% prevalence were: arthritis, behavior problems, benign prostatic hyperplasia, breast cancer, chronic obstructive pulmonary disorder, congestive heart failure, colorectal cancer, cerebrovascular disease, ischemic heart disease, lung cancer, prostate cancer, psychoses, and renal failure.
Odds ratio from logistic regression adjusting for gender, age, age-squared, income (in quintiles based on median family income by census block group from the 2000 US census), primary facility where member received care, family size(as a categorical variable), gender of the index person, role of the index person (subscriber, spouse or dependent), and cost of the index person in the year before the index date.
Both family groups had less than 2% of persons with this condition
Difference between family members of AODD persons and family members of asthma persons was significant at p<=0.05, after adjusting for covariables.
Table 4.
Prevalence of medical and mental health conditions in the year before the index date: Family members of AODD persons compared to family members of non-AODD primary care utilizers.
| Number (Percent) of persons receiving medical diagnoses during year | ||||||
|---|---|---|---|---|---|---|
| Adults | Children | |||||
| Medical/Mental Health Conditions‡ | Family members of AODD persons (N=26204) | Family members of non-AODD persons (N=27364) | Odds Ratio (95% CI)§ | Family members of AODD persons (N=19237) | Family members of non-AODD persons (N=19147) | Odds Ratio (95% CI)§ |
| Acid related disorders (GAS01, GAS06, GAS08) | 1740 (6.6) | 1857 (6.8) | 0.96 (0.90 to 1.03) | ¶ | ¶ | ¶ |
| Asthma (ALL04, ALL05) | 1472 (5.6) | 1536 (5.6) | 0.98 (0.91 to 1.06) | 1653 (8.6) | 1684 (8.8) | 0.98 (0.92 to 1.06) |
| Attention deficit disorder (PSY05) | ¶ | ¶ | ¶ | 719 (3.7) | 581 (3.0) | 1.27 (1.13 to 1.42)* |
| Depression (PSY09) | 1571 (6.0) | 1023 (3.7) | 1.64 (1.52 to 1.78)* | ¶ | ¶ | ¶ |
| Diabetes (END06–END09, EYE13) | 1359 (5.2) | 1539 (5.6) | 0.88 (0.82 to 0.95)* | ¶ | ¶ | ¶ |
| Hypertension (CAR14, CAR15) | 3396 (13.0) | 3454 (12.6) | 1.00 (0.95 to 1.06) | ¶ | ¶ | ¶ |
| Lower Back Pain (MUS14) | 2926 (11.2) | 2774 (10.1) | 1.10 (1.04 to 1.16)* | ¶ | ¶ | ¶ |
| Otitis media (EAR01) | 990 (3.8) | 1072 (3.9) | 0.95 (0.87 to 1.04) | 2815 (14.6) | 2829 (14.8) | 1.04 (0.98 to 1.11) |
| Pneumonia (RES02) | 1402 (5.4) | 1273 (4.7) | 1.14 (1.05 to 1.23)* | 828 (4.3) | 875 (4.6) | 0.98 (0.88 to 1.08) |
| Substance use disorders (PSY02) | 1091 (4.2) | 577 (2.1) | 2.0 (1.80 to 2.21)* | ¶ | ¶ | ¶ |
| Trauma (EYE12, GSU12, MUS02, MUS04, MUS08, MUS09, NUR15, NUR16, REC03, REC04, SKN01) | 4300 (16.4) | 3918 (14.3) | 1.16 (1.11 to 1.22)* | 3698 (19.2) | 3301 (17.2) | 1.13 (1.07 to 1.19)* |
Conditions were a subset of 25 conditions that represent about 80% of KP's health care spending (Ray, 2000), plus ADHD, behavior problems, and otitis media, which were considered a priori to be conditions more prevalent among children. The subset consists of those conditions that occurred in at least 2% of either the AODD family members or the comparison family members, and excluded pregnancy. Conditions of the uterus and headache met the 2% criterion, but are not included in this table because there were no significant differences in these conditions in any of the comparisons.
Conditions were identified by grouping relevant Expanded Diagnosis Clusters (EDCs) as defined by the Johns Hopkins ACG Case-Mix System. The EDCs used are in parentheses. Conditions that did not reach 2% prevalence were: arthritis, behavior problems, benign prostatic hyperplasia, breast cancer, chronic obstructive pulmonary disorder, congestive heart failure, colorectal cancer, cerebrovascular disease, ischemic heart disease, lung cancer, prostate cancer, psychoses, and renal failure.
Odds ratio from logistic regression adjusting for gender, age, age-squared, income (in quintiles based on median family income by census block group from the 2000 US census), primary facility where member received care, family size(as a categorical variable), gender of the index person, role of the index person (subscriber, spouse or dependent), and cost of the index person in the year before the index date.
Both family groups had less than 2% of persons with this condition
Difference between family members of AODD persons and family members of non-AODD persons was significant at p<=0.05, after adjusting for covariables.
Cost and utilization
After adjusting for all co-variables, AODD family members had significantly higher total health care costs per person than diabetes family members in each of the two years after the index date ($217 (about 10%) more in the first year, and $293 (about 13%) more in the second year, Table 5.) AODD family members had higher total health care costs than asthma family members in the year before, and the second year after, the index date ($104 (5%) and $269 (12%) higher, respectively), and higher total costs than non-AODD family members in all three years of analysis. Regardless of the group to which the AODD family members were compared, or the year of comparison, the AODD family members consistently had higher ED-related costs, alcohol and drug program costs, and psychiatry costs than the comparison family members, and more visits.
Table 5.
Per Person Mean Adjusted Annual Cost and Utilization of Family Members of Persons With Alcohol or Other Drug Dependence (AODD) Diagnosis, Compared to Diabetes, Asthma, and Non-AODD Family Members, by Year in Relation to Index Date.
| Difference in cost of family members of persons with AODD compared to family members of persons with diabetes, asthma, and non-AODD primary care utilizers (95% CI)‡ | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| AODD family members compared to diabetes family members | AODD family members compared to asthma family members | AODD family members compared to Non-AODD family members | |||||||
| Cost/Utilization Type | Year(−1) | Year1 | Year 2 | Year(−1) | Year1 | Year 2 | Year(−1) | Year1 | Year 2 |
| All hospital-related costs | 5 (−101 to 110) | 61 (−62 to 185) | 122 (−26 to 270) | 70 (−15 to 154) | 17 (−89 to 122) | 166 (40 to 292)* | 74 (3 to 146)* | 104 (−2 to 210) | 94 (−33 to 221) |
| ED-related costs | 12 (7 to 18)* | 13 (6 to 20)* | 12 (4 to 21)* | 8 (3 to 13)* | 10 (3 to 16)* | 11 (3 to 19)* | 19 (13 to 24)* | 19 (12 to 26)* | 24 (16 to 32)* |
| Outpatient primary care-related visit costs | −15 (−28 to −2)* | −10 (−26 to 5) | −11 (−31 to 9) | −48 (−59 to −36)* | −44 (−58 to −30)* | −40 (−58 to −22)* | −8 (−19 to 3) | −8 (−23 to 6) | −4 (−23 to 15) |
| Outpatient alcohol & drug program visit costs | 26 (21 to 31)* | 69 (61 to 76)* | 40 (29 to 50)* | 27 (23 to 31)* | 81 (74 to 88)* | 37 (28 to 46)* | 27 (22 to 32)* | 74 (66 to 81)* | 29 (20 to 39)* |
| Outpatient psychiatry dept visit costs | 47 (39 to 54)* | 73 (62 to 83)* | 48 (36 to 60)* | 32 (25 to 40)* | 59 (50 to 69)* | 34 (23 to 46)* | 38 (31 to 45)* | 63 (54 to 73)* | 35 (23 to 47)* |
| Outpatient pharmacy costs | 16 (0 to 32)* | 36 (18 to 55)* | 32 (2 to 62)* | 2 (−12 to 15) | 3 (−14 to 20) | 12 (−13 to 36) | 24 (10 to 38)* | 11 (−8 to 31) | 33 (7 to 60)* |
| Other outpatient costs | 14 (−14 to 41) | −24 (−78 to 30) | 49 (−32 to 131) | 13 (−17 to 43) | −18 (−51 to 15) | 49 (−18 to 116) | 35 (5 to 65)* | 30 (8 to 53)* | 71 (5 to 137)* |
| Total costs† | 104 (−22 to 231) | 217 (65 to 370)* | 293 (93 to 493)* | 104 (1 to 208)* | 107 (−20 to 235) | 269 (101 to 437)* | 209 (116 to 301)* | 293 (168 to 419)* | 283 (110 to 456)* |
| Number of inpatient hospital days | 0.02 (−0.01 to 0.05) | 0.03 (0.00 to 0.07) | 0.03 (−0.02 to 0.08) | 0.04 (0.02 to 0.07)* | 0.02 (−0.01 to 0.05) | 0.06 (0.00 to 0.11)* | 0.04 (0.01 to 0.06)* | 0.04 (0.00 to 0.07)* | 0.56 (0.38 to 0.73) |
| Number of outpatient visits | 0.49 (0.38 to 0.60)* | 1.14 (0.99 to 1.29)* | 0.69 (0.50 to 0.87)* | 0.18 (0.08 to 0.28)* | 1.05 (0.91 to 1.19)* | 0.34 (0.18 to 0.50)* | 0.47 (0.37 to 0.57)* | 1.22 (1.08 to 1.37)* | 0.05 (0.01 to 0.09)* |
Positive values indicate that family members of AODD were more costly than comparison family members. Differences in costs and utilization were estimated using generalized linear models. A separate model was run for each comparison group and for each cost/utilization type. Co-variables included in the model were gender and age at index date (as a categorical variable with 18 age levels, in five year increments, for each gender), census block income group (in quintiles), primary facility where person received care, family size, gender and age of the index person, role of the index person, and cost of the index person in the year of analysis. Numbers in parentheses represent lower and upper bounds of 95% confidence interval. All costs are in 2005 $US.
Mean unadjusted total costs per diabetes family member in years −1, 1, and 2, respectively, were $2138, $2142 and $2191. Corresponding costs for asthma family members were $2103, $2201, and $2181. Corresponding costs for non-ADHD family members were $2020, $2013, and $2125.
Significantly different from comparison family members at p=.05.
When we excluded family members with costs over $500,000, AODD family members cost $147 (Confidence Interval (CI): $35 to $259) more than diabetes family members in the year before the index date, $120 (CI: $27 to $212) more than asthma family members, and $209 (CI: $123 to $295) more than non-AODD family members.
Discussion
Prior research suggests that families of alcoholics are affected by the alcoholic's behavior [2, 3, 20–22], and that the prevalence of many health conditions, and the cost of health services, for these family members are greater than for the family members of persons without an alcohol or drug problem [6]. The current findings extend and strengthen previous findings by showing that the family members of AODD persons are more likely to be diagnosed with depression, substance use disorders, and trauma than family members of persons with diabetes or asthma. Their health care utilization and costs are also similar to, or higher, than the family members of persons with diabetes and asthma.
Each group of families was more likely to be diagnosed with conditions related to the condition of the index person – diabetes family members were more likely to be diagnosed with diabetes, asthma family members with asthma, and AODD family members with substance use disorders. These results are consistent with the fact that each of these conditions has genetic and environmental components.
Although the study does not allow us to determine causality, the findings that AODD family members were consistently more likely to be diagnosed with substance use disorders, depression and trauma than diabetes or asthma family members, suggests that there is something unique about the stressors of having an AODD person in the family, or something unique about the physical or psychosocial environment of the AODD families. It has been suggested that different disorders have specific effects on caregivers due, for example, to their symptoms as well as to social reactions to them [23]. AODD is linked with job instability, irritable moods, unreliability, not fulfilling marital or parental roles and obligations, and family conflict [24, 25]. In turn, these family stressors predict increased risk for depression [26, 27]. Children of persons with AODDs experience distress due to the conflict between their parents, and research has also found a strong link between AODD and child neglect [24]. Neglect and higher rates of driving under the influence may in part explain the increased risk of trauma in AODD family members. Moreover, aggression is common among children of persons with AODD [28] and is in turn predictive of risk-taking behaviors in adolescents [29]. Although there are no studies comparing these effects in the family members of alcoholics with those of diabetics or asthmatics, the nature of AODD makes it plausible that these particular stressors are more pronounced among family members of persons with AODD. These results are also consistent with a conceptual framework of family functioning whereby having a family member with AODD leads to worse physical and mental functioning [13]. Other explanations for the higher rates of AODD and psychiatric disorders in family members of AODD individuals are heritability (for the findings among children) and selection of similar partners (for the findings among adults.) With respect to alcohol dependence, there is some evidence of assortative mating whereby individuals predisposed to alcohol dependence marry individuals with a similar disposition [30]. The degree to which this occurs among persons with diabetes or asthma is unknown. In addition, genetic and other environmental factors (excluding those created by the index persons themselves) likely play some role in the differences we found. The fact that AODD family members were less likely to have diabetes than family members of those with diabetes suggests that genetic and other environmental factors, such as family similarity of health and health-care seeking behaviors, are also contributing factors to these findings.
The increased health care costs and utilization we find among AODD family members compared to diabetes or asthma family members may reflect their higher prevalence of substance use disorders, depression and trauma, even though the prevalence of other conditions, such as acid-related disorders, asthma, diabetes and hypertension tended to be lower in the AODD family members. That the AODD family members' higher costs were primarily in the emergency, alcohol and drug treatment, and psychiatry departments is consistent with this hypothesis.
Our findings that AODD family members have more health conditions and consistently higher cost than non-AODD family members is consistent with our earlier study, but the differences are somewhat smaller [6]. This was expected and is due to the fact that we matched index persons on health care costs. By matching high-utilizing AODD index persons to high-utilizing non-AODD persons we necessarily included non-AODD index persons who had more health problems than the group in the earlier study.
Limitations
We chose in this analysis to analyze the year before, and the two years after the index person's diagnosis. Typically, chronic illnesses manifest themselves in some way prior to a diagnosis, and we assume that most index persons had their condition before being diagnosed with it. (Because we only checked for diagnoses one year prior to the index date, they may also have been diagnosed at some earlier time in their life.) By analyzing family members in the year before the diagnosis, we factor out effects that might purely be related to treatment of the index person, although these effects are of interest too, and they may be seen in the years following the diagnosis. However, we cannot draw conclusions about how the effect of having a family member with a chronic illness may be cumulative and change over time. Future studies should analyze family differences over longer periods of time, and, crucially, as they relate to successful treatment of the index person's condition.
This study does not allow us to determine the reasons for differences seen between the AODD family members and the comparison family members. Although we hypothesize that having an AODD family member results in additional family stressors (or stressors of a type more likely to result in health services utilization), the other factors we discussed (i.e., assortative mating and genetic factors) may explain some of these differences.
The apparently higher prevalence of health conditions among the AODD family members may be partly the result (rather than the cause) of higher utilization. Persons with more visits have a greater chance of being diagnosed with conditions. Also, persons whose family members have a certain condition (for example, alcohol dependence) may be more prone to seek and/or receive a diagnosis for that same condition, or related conditions. From the health services standpoint, this is still important in that seeking and/or receiving a diagnosis may drive health services utilization and cost.
Conclusion
This study joins other literature arguing that substance use disorders have similarities to other chronic diseases. Our findings show that these similarities extend to family members as well. We found that there are unique patterns with respect to the health conditions that family members are diagnosed with, and. that AODD family members had the same, or higher, health services utilization and costs as family members of persons with diabetes and asthma. Key questions our study raises are whether the AODD families' increased prevalence of certain health conditions, and the higher cost of health services, persist over time and whether they would be reduced with successful treatment of the index person.
Acknowledgments
This study was funded by the National Institute on Alcohol Abuse and Alcoholism R01 AA15183. The authors report no conflict of interest.
Footnotes
The authors report no conflict of interest.
REFERENCES
- 1.Reiss D, Steinglass P, Howe G. The family organization around the illness. In: Cole RE, Reiss D, editors. How do Families Cope with Chronic Illness? Lawrence Erlbaum Associates; Hillsdale, NJ: 1993. pp. 173–213. [Google Scholar]
- 2.Steinglass P, Bennett LA, Wolin SJ, Reiss D. The Alcoholic Family. Basic Books; New York: 1987. [Google Scholar]
- 3.Wiseman JP. The Other Half. Wives of Alcoholics and Their Social-Psychological Situation. Aldine de Gruyter; New York: 1991. [Google Scholar]
- 4.Spear SF, Mason M. Impact of chemical dependency on family health status. Int J Addict. 1991;26:179–87. doi: 10.3109/10826089109053179. [DOI] [PubMed] [Google Scholar]
- 5.Lennox RD, Scott-Lennox JA, Holder HD. Substance abuse and family illness: evidence from health care utilization and cost-offset research. J Ment Health Pol Econ. 1992;19:83–95. doi: 10.1007/BF02521310. [DOI] [PubMed] [Google Scholar]
- 6.Ray GT, Mertens JR, Weisner C. The excess medical cost and health problems of family members of persons diagnosed with alcohol or drug problems. Med Care. 2007;45:116–22. doi: 10.1097/01.mlr.0000241109.55054.04. [DOI] [PubMed] [Google Scholar]
- 7.Holder HD, Hallan JB. Impact of alcoholism treatment on total health care costs: a six-year study. Adv Alcohol Subst Abuse. 1986;6:1–15. doi: 10.1300/J251v06n01_01. [DOI] [PubMed] [Google Scholar]
- 8.Roberts KS, Brent EE. Physician utilization and illness patterns in families of alcoholics. J Stud Alcohol. 1982;43:119–28. doi: 10.15288/jsa.1982.43.119. [DOI] [PubMed] [Google Scholar]
- 9.Woodside M, Coughey K, Cohen R. Medical costs of children of alcoholic -- pay now or pay later. J Subst Abuse. 1993;5:281–7. doi: 10.1016/0899-3289(93)90069-n. [DOI] [PubMed] [Google Scholar]
- 10.Svenson LW, Forster DI, Woodhead SE, Platt GH. Individuals with a chemical-dependent family member. Does their health care use increase? Can Fam Physician. 1995;41:1488–93. [PMC free article] [PubMed] [Google Scholar]
- 11.Lipscomb HJ, Dement JM, Li L. Health care utilization of families of carpenters with alcohol or substance abuse-related diagnoses. Am J Ind Med. 2003;43:361–8. doi: 10.1002/ajim.10214. [DOI] [PubMed] [Google Scholar]
- 12.Altman BM, Cooper PF, Cunningham PJ. The case of disability in the family: impact on health care utilization and expenditures for nondisabled members. Milbank Q. 1999;77:39–75. iv. doi: 10.1111/1468-0009.00124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moos RH, Moos BS. The process of recovery from alcoholism III: Comparing functioning in families of alcoholics and matched control families. J Stud Alcohol. 1984;45:111–8. doi: 10.15288/jsa.1984.45.111. [DOI] [PubMed] [Google Scholar]
- 14.McLellan AT, Lewis DC, O'Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284:1689–95. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 15.Holmes AM, Deb P. The effect of chronic illness on the psychological health of family members. J Ment Health Pol Econ. 2003;6:13–22. [PubMed] [Google Scholar]
- 16.Lim JW, Zebrack B. Caring for family members with chronic physical illness: a critical review of caregiver literature. Health Qual Life Outcomes. 2004;2:50. doi: 10.1186/1477-7525-2-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Selby JV. Linking automated databases for research in managed care settings. Ann Intern Med. 1997;127:719–24. doi: 10.7326/0003-4819-127-8_part_2-199710151-00056. [DOI] [PubMed] [Google Scholar]
- 18.Bonomi AE, Boudreau DM, Fishman PA, Meenan RT, Revicki DA. Is a family equal to the sum of its parts? estimating family-level well-being for cost-effectiveness analysis. Qual Life Res. 2005;14:1127–33. doi: 10.1007/s11136-004-2578-9. [DOI] [PubMed] [Google Scholar]
- 19.Ray GT, Collin F, Lieu T, Fireman B, Colby CJ, Quesenberry CP, et al. The cost of health conditions in a health maintenance organization. Med Care Res Rev. 2000;57:92–109. doi: 10.1177/107755870005700106. [DOI] [PubMed] [Google Scholar]
- 20.Collins RL, Leonard KE, Searles JS, editors. Alcohol and the Family. Research and Clinical Perspectives. The Guilford Press; New York: 1990. [Google Scholar]
- 21.Velleman R, Copello A, Maslin J, editors. Living with Drink. Women Who Live with Problem Drinkers. Addison-Wesley Longman; New York: 1998. [Google Scholar]
- 22.Ames G. Maternal Alcoholism and Family life: A Cultural Model of Research and Intervention [Ph.D. Dissertation] University of California; San Francisco: 1982. [Google Scholar]
- 23.Magliano L, Fiorillo A, De Rosa C, Malangone C, Maj M. Family burden in long-term diseases: a comparative study in schizophrenia vs. physical disorders. Soc Sci Med. 2005;61:313–22. doi: 10.1016/j.socscimed.2004.11.064. [DOI] [PubMed] [Google Scholar]
- 24.Orford J. Alcohol and the family: an international review of the literature with implications for research and practice. In: Kozlowski LT, Annis HM, Cappell HD, Glaser FB, Goodstdt MS, Israel Y, et al., editors. Research Advances in Alcohol and Drug Problems. Vol 10. Plenum Press; New York: 1990. pp. 81–155. [Google Scholar]
- 25.Hurcom C, Copello A, Orford J. The family and alcohol: effects of excessive drinking and conceptualizations of spouses over recent decades. Subst Use Misuse. 2000;35:473–502. doi: 10.3109/10826080009147469. [DOI] [PubMed] [Google Scholar]
- 26.Moos RH, Schutte KK, Brennan PL, Moos BS. Theinterplay between life stressors and depressive symptoms among older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60:P199–206. doi: 10.1093/geronb/60.4.p199. [DOI] [PubMed] [Google Scholar]
- 27.Swindle RW, Jr., Cronkite RC, Moos RH. Life stressors, social resources, coping, and the 4-year course of unipolar depression. J Abnorm Psychol. 1989;98:468–77. doi: 10.1037//0021-843x.98.4.468. [DOI] [PubMed] [Google Scholar]
- 28.Edwards EP, Eiden RD, Colder C, Leonard KE. The development of aggression in 18 to 48 month old children of alcoholic parents. J Abnorm Child Psychol. 2006;34:409–23. doi: 10.1007/s10802-006-9021-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Redeker NS, Smeltzer SC, Kirkpatrick J, Parchment S. Risk factors of adolescent and young adult trauma victims. Am J Crit Care. 1995;4:370–8. [PubMed] [Google Scholar]
- 30.Grant JD, Heath AC, Bucholz KK, Madden PA, Agrawal A, Statham DJ, et al. Spousal concordance for alcohol dependence: evidence for assortative mating or spousal interaction effects? Alcohol Clin Exp Res. 2007;31:717–28. doi: 10.1111/j.1530-0277.2007.00356.x. [DOI] [PubMed] [Google Scholar]