Abstract
This study examined the feasibility of using Ecological Momentary Assessment (EMA) to examine important domains relevant to interregulatory health processes in overweight adolescent females in their natural environments. Participants were 20 overweight adolescent females engaged in a cognitive–behavioral and motivational interviewing intervention aimed at weight loss and improving mood (11–19 years old, 80% white, 15% African American, mean BMI = 39). During this EMA protocol, participants were asked to report their physical activity (PA), nutrition, mood, and sleep during 14 cellular phone calls over three extended weekends (Thursday to Monday). Simultaneously, participants wore an actigraph (armband and watch communicator) that provided instantaneous PA feedback (steps taken and kilocalories) and sleep parameters (duration and efficiency). EMA compliance rates for the armband and phone calls were 74.7 ± 0.3% and 64.2 ± 0.3%, respectively. Data from the armband and phone calls are presented to illustrate the depth of information acquired by utilizing this innovative methodology.
Pediatric obesity
Recent estimates show that nearly 32% of children in the United States are overweight, which is dramatically higher than the prevalence reported in the 1980s (ref. 1). Childhood obesity is associated with psychological, neurologic, pulmonary, gastrointestinal, circulatory, and endocrine conditions (2,3). Most pediatric obesity interventions are marked by modest changes in weight or adiposity and substantial relapse (4). More comprehensive assessments documenting specific behavior change are needed, eliminating methodology compromised by self-report and retrospective recall (5). Moreover, given exclusion criteria in many pediatric obesity trials, children with mood disorders (depression) and medical comorbidities (sleep problems) do not receive the interventions. Domains such as mood and sleep may be essential dimensions of assessment as mediators or moderators of weight-loss treatment. Therefore, we sought not only to examine the feasibility of adding methodologically sound technology to an empirically validated weight-management intervention, but also to examine interregulatory processes across behaviors (i.e., eating, physical activity (PA), mood, and sleep) in an objective manner.
Ecological Momentary Assessment (EMA) is an innovative form of data collection that provides objective data on patterns of behaviors within a participant’s natural environment. EMA helps to circumvent sources of bias inherent in other retrospective self-report measures (6). In adults, multiple applications of EMA methodology have provided insight into food intake and maintenance of weight-related disorders (7), and initial research has demonstrated its utility in pediatric samples with psychopathology (8). Thus, EMA methodology may assist weight-loss efforts by clarifying the antecedents of participants’ eating behavior (6), by improving accuracy of self-monitoring (9) and by specifying the temporal relationships of the target behaviors (10). The aims of this pilot study were to (i) examine the feasibility of utilizing EMA in overweight children participating in an empirically validated cognitive– behavioral weight-management intervention, and (ii) examine the relationship between EMA and weight (primary) and behavioral outcomes (secondarily; mood and sleep). To our knowledge, no studies have examined the utility of complementary EMA methodologies (phone calls and actigraphy) to measure interregulatory health processes in obese adolescents participating in a weight-loss trial. In this brief report, we discuss pilot data primarily regarding aim 1 (EMA utilization).
METHODS
This study was conducted alongside the Weight Management Center at Children’s Hospital of Pittsburgh and approved by the University’s Institutional Review Board. Informed assent and consent were obtained from 20 English-speaking participants (11–19 years old, 80% white, 15% African American, mean BMI = 39). Exclusion criteria consisted of no: (i) guardian/parental involvement in the weight- management protocol, (ii) suicidal/homicidal plan requiring immediate hospitalization, (iii) participation in a current empirically validated weight intervention, or (iv) diabetes or cardiovascular disease. The intervention consisted of four weekly, four bi-weekly, and three monthly individual sessions. Information focusing on nutrition, PA, and behavior change was presented in ~45-min sessions using cognitive–behavioral therapy and motivational interviewing followed by ~30 min of PA.
EMA–cellular phone methodology
Similar to previous protocols (8), participants received calls from a trained staff member for three extended weekends across the intervention. Participants were called twice on weekdays and four times on weekends for a total of 14 calls between 4 PM Thursday and 9 PM Monday. Each call consisted of a brief structured interview to evaluate current eating, PA, affect, and social context and lasted between 5 and 10 min.
EMA–BodyMedia Sensewear device
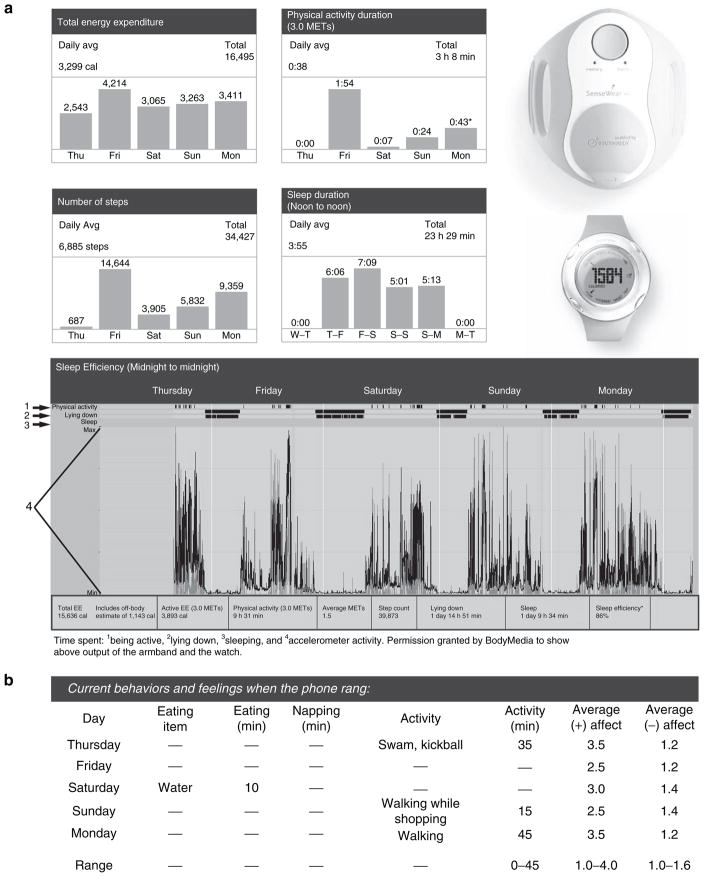
The BodyMedia SenseWear Weight Management System (see Figure 1) acts as a metabolic monitor that allows for convenient collection of data to determine calories expended, PA duration and intensity, and sleep duration and efficiency. This device includes an armband that measures and stores data and a watch display that shows up-to-the-minute feedback (i.e., steps taken and calories burned). Additionally, the data can be downloaded to produce user-friendly charts that are helpful in goal setting.
Figure 1.
Ecological Momentary Assessment (EMA) data for one participant. (a) One participant’s armband data acquired across one weekend. (b) Participant’s phone call data across the same weekend (compliance = 85% phone and 82% armband). MET, metabolic equivalent.
RESULTS AND DISCUSSION
Of the female adolescents (n = 20) who participated in this pilot study, mean armband and telephone compliance (measured as the percent of time the armband was worn and percent of completed phone calls) were 74.7 ± 0.3% and 64.2 ± 0.3%, respectively. Figure 1 illustrates the depth of data obtained using this novel methodology across one participant’s weekend. In this figure, actigraph recordings of PA and sleep parameters are shown, and accelerometer data demonstrate episodes of wakefulness and sleep via the sleep efficiency graph. Figure 1 also illustrates phone call data over the same weekend, thus elucidating temporal relationships across PA, eating, mood, and sleep. These health processes are then summarized to provide feedback to participants on their real-time activities.
To provide the most-effective weight-management interventions for children and adolescents, practitioners are encouraged to assess all factors that target weight-related behavior change. Tools that simultaneously measure these complex factors may further increase the efficacy of interventions. The ability to determine the temporal relationships among these complex interregulatory variables (e.g., whether a decrease in sleep efficiency results in lower levels of vigorous PA the subsequent day) has implications on which behaviors to target. The compliance rates in our pilot data for EMA calls (64.2%) and armband duration (74.7%) reveal the feasibility of using these methodologies for assessment of activity, mood, and sleep in a sample of overweight adolescent girls. Our findings should be interpreted in light of certain study limitations. The methodologies utilized in this pilot project require replication with a larger, more heterogeneous sample, and perhaps adding a control group who present as overweight with no mood or sleep disturbances.
The implications of this research suggest that technological devices that gather objective data have reasonably high compliance rates, and may inform measurement of treatment outcomes in adolescents who are obese. Further investigation is needed to determine whether including EMA in weight-loss interventions ultimately contributes to overall treatment efficacy.
Acknowledgments
We acknowledge the dedicated assistance of all of our research lab members who have assisted in making participant phone calls, Stefanie Weiss (University of Michigan), Kim Dunlap (Miami University), Kristen Vogt (Slippery Rock University), Jenna Shuck (Chatham University), and Jennifer Jakubak, KayLoni Olson, Ashley Block, Linnea Warren, Amy Phillips, Kristin Johnson, Brian Thoma (University of Pittsburgh), Ronette Blake, Jenn Jones, Glory Ojiere, Amy Gillio, and Erica Stein. This paper is written with support from mechanism K12-HD043441 (D.L.R.), K23HD061598 (D.L.R.), The State Tobacco Fund–Pittsburgh Mind-Body Center HL076852/076858 (D.L.R.), and R21DA024144 (J.S. and R.E.D.).
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
References
- 1.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 2.Deckelbaum RJ, Williams CL. Childhood obesity: the health issue. Obes Res. 2001;9 (Suppl 4):239S–243S. doi: 10.1038/oby.2001.125. [DOI] [PubMed] [Google Scholar]
- 3.Must A, Strauss RS. Risks and consequences of childhood and adolescent obesity. Int J Obes Relat Metab Disord. 1999;23 (Suppl 2):S2–11. doi: 10.1038/sj.ijo.0800852. [DOI] [PubMed] [Google Scholar]
- 4.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity (Silver Spring) 2008;16:1009–1018. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 5.Lichtman SW, Pisarska K, Berman ER, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327:1893–1898. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 6.Smyth JM, Soefer MH, Hurewitz A, Stone AA. The effect of tape-recorded relaxation training on well-being, symptoms, and peak expiratory flow rate in adult asthmatics: a pilot study. Psychol Health. 2001;14:487–501. [Google Scholar]
- 7.Hilbert A, Tuschen-Caffier B. Maintenance of binge eating through negative mood: a naturalistic comparison of binge eating disorder and bulimia nervosa. Int J Eat Disord. 2007;40:521–530. doi: 10.1002/eat.20401. [DOI] [PubMed] [Google Scholar]
- 8.Silk JS, Dahl RE, Ryan ND, et al. Pupillary reactivity to emotional information in child and adolescent depression: links to clinical and ecological measures. Am J Psychiatry. 2007;164:1873–1880. doi: 10.1176/appi.ajp.2007.06111816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burke LE, Warziski M, Starrett T, et al. Self-monitoring dietary intake: current and future practices. J Ren Nutr. 2005;15:281–290. doi: 10.1016/j.jrn.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 10.Biddle SJ, Gorely T, Marshall SJ, Cameron N. The prevalence of sedentary behavior and physical activity in leisure time: A study of Scottish adolescents using ecological momentary assessment. Prev Med. 2009;48:151–155. doi: 10.1016/j.ypmed.2008.10.025. [DOI] [PubMed] [Google Scholar]