Abstract
In this study, we used recovery preference exploration (RPE) to explore how clinicians practicing in an inpatient medical rehabilitation facility assign meaning to alternative paths of recovery from profound disability. Through the RPE procedure, 33 clinicians ranked preference for recovery from 18 imagined activity limitations and provided narrative explanations for their choices. We used mixed methods, including grounded theory, to identify themes that expressed their recovery choices. Sixteen themes emerged that were classified into separate but linked procedural and conditional reasoning taxonomies. These theme taxonomies represented logical scientific inquiries vs. more phenomenological inquiries into lifeworld meanings, respectively. Just over two thirds (66.8%) of all quotes specified themes from the conditional reasoning taxonomy. The RPE procedure appeared to simulate a lived experience of imagined disability for the clinicians through which contexts and meanings began to emerge independent of the clinicians’ scientific attitudes.
Keywords: disabled persons, grounded theory, health care professionals, moral perspectives, health concepts, imagination, mixed methods, phenomenology, recovery, rehabilitation, values
Clinical reasoning has been a source of interest to clinicians who must be able to apply more than facts to succeed in the practice of their professions. Coined by Schon as “reflection in action,” the knowledge of how professionals think before, during, and after their interaction with a patient is essential in both the early education of students as well as the ongoing development of practitioners as they strive for proficiency and excellence in their work. (Schon, 1983) In an attempt to understand both the art and science of practice, scholars have considered ideas associated with “reflection in action,” “tacit knowledge,” “knowing in action,” and other related terms (Coles, 1989; Dreyfus, 1986; Klienman, 1980; Polanyi, 1967; Schon, 1983). The idea that clinicians might categorize information, transform it into ideas, and draw on their existing knowledge and experience in ways that are not easily expressed in words or simple actions has been the focus of clinical reasoning studies among occupational therapists, physical therapists, nurses, and physicians (Benner & Tanner, 1987; Cohn, 1989; Jensen, Shepard, & Hack, 1990; Neistadt & Seymour, 1995).
In a study of occupational therapists, Mattingly and Fleming distinguished three forms of reasoning used to solve clinical problems: procedural, conditional, and interactive. Procedural reasoning connotes medical problem solving that focuses on “physical ailments and what procedures might possibly alleviate them or remediate the person’s functional performance problems” (Mattingly & Fleming, 1994, p. 17). Using procedural reasoning, the practitioner generates a hypothesis that asks, “What is the problem to be solved and procedure to be applied?” For the physician, it involves formulating a diagnosis and treatment plan for the clinical condition. For the therapist, it necessitates determining which techniques and procedures will solve problems in daily functioning.
In an effort to understand the person within his or her lifeworld (Barry, Stevenson, Britten, Barber, & Bradley, 2001), a practitioner will use conditional reasoning to look beyond the highly specialized world of being a clinician (Good & DelVecchio Good, 2000). This view brings the person and the specific life they inhabit into focus. A full accounting of the past life and the implications of the disease or disability within that life is used to construct a meaningful idea of how the future might play out. This type of reasoning can be cast as a way to understand the patient from a phenomenological point of view by asking: What is meaningful to this person? What is meaningful to this individual given her perceptions of herself and others? What is meaningful in the contexts of her social and cultural lifeworlds (Mattingly & Fleming, 1994) and the physical world surrounding her?
Interactive reasoning is used to support the professional to “interact with and better understand the person” (Mattingly & Fleming, 1994, p. 17). It is the form of reasoning that generates questions such as: What is the best way for me to interact with this person and begin to understand her better? How does she feel about the treatment? What is she like? How can I tailor treatment to her? Practitioners engage in interactive reasoning to develop treatment plans that are customized and allow for adaptations to a particular person’s life situation.
These three forms of reasoning can help clinicians understand the lifeworlds that people with disabilities find themselves inhabiting, applying theories of health environment integration (HEI).
HEI, a biopsychoecological model of illness and disability, is consistent with concepts included in the International Classification of Functioning Disability and Health (ICF; World Health Organization, 2001). It applies four spheres representing mind, body, physical world, and society to “conceptualize the functional interaction between the person and the environment,” as shown in Figure 1 (Stineman, 2001; Stineman, Ross, Maislin, & Gray, 2007). The intersection of these four spheres provides a broad context beyond the medical condition for reflecting the multiple ways disability is produced, measured (objectively), and perceived (subjectively). The four spheres and intersections among them that make up the external life-world can be segmented into measurable domains and concepts and analyzed through procedural reasoning. Elements from the external spheres are reflected in the internal lifeworld and form a substrate from which the personal landscape of thoughts and meanings emerges. Not directly accessible to the outsider, conditional reasoning is necessary to explore idiosyncratic meanings and to offer a glimpse of the internal lifeworlds of people with disabilities.
Figure 1.
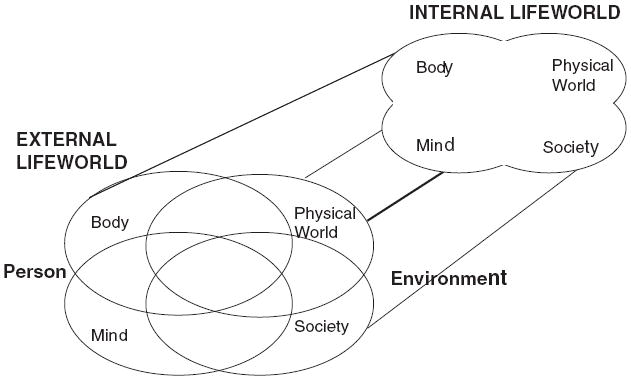
The Spheres of HEI Model
Identification of the most effective treatments for people with disabilities—and empowering them—depends on the clinician’s ability to synthesize information at the intersection of all four spheres. It further depends on the combination of objective and subjective information through the use of both procedural and conditional reasoning to inform interactive communications with patients (Stineman, 2000). This balanced type of reasoning is expected to be facilitated by the clinician, gaining an understanding of his or her own values and beliefs about activity limitation. It includes the perceived relative importance and meaning of recovery from different types of limitation. Gaining knowledge of one’s own attitudes by opening up a frank understanding of personal feelings about disability makes it easier to avoid the tendency to impose personal beliefs on others.
In an effort to understand how therapists, physicians, and nurses view the implications of recovery for patients with significant disability, we performed a procedure referred to as recovery preference exploration (RPE; Stineman et al., 2007). RPE yields quantitative and qualitative data about a single individual’s recovery preferences (Kurz, Saint-Louis, Burke, & Stineman, 2008; Stineman et al., 2007). The clinician is asked to imagine that he or she is completely dependent in all 18 activities of the FIM (Functional Independence Measure; Hamilton, Granger, Sherwin, Zielezny, & Tashman, 1987). RPE was used to elicit information about the complexity of the reasoning process and to explore the meaning of disability relative to the clinician’s self-perception. RPE also provided a way to understand how the idiosyncratic contexts of the clinician’s sociocultural world and physical environment might drive his or her own recovery preference pattern should he or she experience profound disability.
In this project, we used RPE to focus on the clinician’s own ideas about recovery. In the imagined circumstance of complete disability, the context of the clinician’s imagined world switches from being the professional care provider to being the patient care receiver. This switch is intended to encourage conditional reasoning—the kind of reasoning that is crucial to ensuring that the most meaningful, person-specific, functional goals and priorities are established.
Methods
Sample
This study was conducted in conjunction with a larger quantitative study of the recovery preferences of 93 clinicians from an urban hospital (Rist, Freas, Maislin, & Stineman, 2008). The protocol was approved by the participating hospital’s Institutional Review Board and the clinicians signed consent forms agreeing to the release of de-identified quantitative and qualitative results. Purposive sampling, to ensure a variety of clinician types and ages, was done to select clinician transcripts for this qualitative study of clinicians’ recovery preferences. The qualitative results from 33 clinicians are examined in this article. Out of these 33 clinicians, there were 3 medical students, 10 physicians, 11 nurses, 1 occupational therapist, 1 physical therapist, 1 recreational therapist, and 6 psychologists.
Procedure
The RPE procedure (Stineman et al., 2007) is based on the “Features Resource Trade-Off Game” designed by Stineman, Maislin, Nosek, Fiedler, and Granger (1998). In this game, between two and five individuals with similar traits plan out their ideal recovery as a group. The nominal group process is used, allowing each group member to have equal input (Van de Ven & Delbecq, 1972). In contrast, the RPE procedure operates at the individual level through partial decentering (Feffer & Jahelka, 1968). Decentering is a technique applied in social psychology and family therapy to enhance empathy and help people understand someone else’s point of view. In RPE the individual is asked to take a point of view different from his current circumstances by imagining complete disability. However, unlike complete decentering where the individual would adopt another person’s values and lifeworld, here the individual is asked to apply his/her own values and lifeworlds to the state of imagined disability.
The RPE procedure requires that the clinician make tradeoffs between imagined recovery from one type of disability vs. another type of disability, yielding quantitative utilities (Sox, Blatt, Higgins, & Marton, 1988). Utilities represent a measure that quantifies the strength of an individual’s preference for particular outcomes, such as recovery from specific activity limitations. Along with yielding utilities, the RPE procedure generates qualitative information through which the clinician expresses values, life contexts, and beliefs about different types of disabilities. The procedures and game board1 used in this study were identical to those previously described (Kurz et al., 2008).
Using the game board to plan ideal recovery, the clinician selects a pattern of movements toward imagining complete independence by moving from lower to higher levels of independence across the activities on the board, without knowing how much recovery will be possible. Specifically, the board lists the 18 functional independence measure (FIM™) activities on the left-hand side and four levels of functioning (some assistance, supervision, take longer/need device, and completely independent) across the top (Granger, Hamilton, Keith, Zielezny, & Sherwin, 1986). The FIM was applied to RPE because it is mandated by Medicare as the standard assessment that must be used to measure activity limitation among all patients undergoing inpatient rehabilitation; however, any functional status measure can be applied to RPE (Stineman, Ross, Maislin, Marchuk, et al., 2007).
The 18 FIM activities express two broad constructs: physical abilities, including eating, grooming, bathing, dressing the upper body, dressing the lower body, toileting, bladder management, bowel management, bed/chair/wheelchair transfer, toilet transfer, tub/shower transfer, walking/wheelchair use, and stairs; and cognitive and communication functions, including comprehension, expression, social interaction, problem solving, and memory (Stineman et al., 1998). The clinicians were asked to imagine that they were completely dependent in all 18 FIM items. They then ordered their preferred sequence of recovery across the 18 FIM items and within 4 imagined levels of independence in each activity. The recovery process was divided into four stages each, with 18 moves per stage, for a total of 72 moves. Applying these 72 moves the clinician imagined advancing from being completely dependent in all 18 FIM items to being completely independent in all 18 FIM items. After each stage, the clinicians were asked to explain the reasons for their choices. The clinicians’ responses were audiotaped and then transcribed.
Analytic Methods
The analytic approach applied mixed methods (Creswell, Fetters, & Ivankova, 2004; National Institutes of Health Office of Behavioral and Social Science Research, 1999), recognizing that both deductive and inductive reasoning are required to determine the meaning of disability and to build a taxonomy of themes. The objective was to gain insight into the forms of reasoning clinicians apply when thinking about the implications of patients’ functional loss. We hypothesized that themes might be loosely classified according to the mind, body, physical world, and society spheres of HEI and according to the extent that they embodied procedural and conditional reasoning.
The data that emerge from RPE simultaneously attach a (quantitative) utility and (qualitative) meaning to each functional activity. They identify (qualitative) life contexts through narrative that provides rationale for those utilities. In the current study, we applied the resulting narrative to thematic analysis to determine the idiopathic phenomenological meaning of recovering the ability to perform the various activities with increasing levels of independence.
The qualitative aspects of RPE complimented the quantitative choices throughout the procedure, giving meaning to the utilities. The narrative analysis was designed to capture the phenomenological nature of disability, applying cognitive and social construction paradigms. Anything spoken by the clinician was viewed as a legitimate “manifestation of the essence of meaning,” and was applied to help make sense of and conceptualize the inner logic driving each clinician’s unique imagined recovery choices (Stewart & Mickunas, 1990). We assumed that people create their lifeworld meanings through personal experience. For clinicians, their personal experiences are continuously shaped and refined by membership in a community of caregivers (Whitman, 1993). The role of RPE was to facilitate the creation of a simulated lived experience for the clinician where he or she moved in an imaginary lifeworld from being the professional care provider to the patient care receiver, allowing meanings to emerge independent of the clinician’s scientific attitude.
To analyze the transcripts, the constant comparative method of grounded theory was used (Glaser & Strauss, 1967). First, the transcripts were read by at least three readers. Each reader read the transcript alone and bracketed parts of the transcript where the clinician gave a specific reason for his or her recovery choices. Then each reader compiled a list of codes under which the various bracketed sections of the transcripts would fit. Next, the readers came to consensus for the codes present in the transcripts, the portions of the transcripts to be coded for each, and the working definitions of the codes. As new codes were discovered, previously read transcripts were reread and recoded, and code definitions were revised. New transcripts were read until no new codes emerged. At this point, saturation was reached and the reading and coding of more new transcripts ended. The coded transcripts were then loaded into Ethnograph v5.0 (Qualis Research Associates, 2001) and frequency data for the appearance of each code was generated.
In addition to generating a list of codes, and definitions for each of the codes, taxonomies of themes were created by the members of the research team. Five team members each came up with their own taxonomy, and then met and combined their ideas. The spheres of HEI as they relate to the various forms of reasoning provided the foundation through which the taxonomies were formulated. The taxonomies were revised as additional codes were discovered, collapsed, or the definitions changed. Two linked thematic taxonomies emerged, organizing the themes found in the clinician transcripts so as to roughly distinguish between codes involving procedural and conditional reasoning. The frequency of themes across the taxonomies was applied to explore the cognitive strategies employed by the clinicians when thinking about the relative importance of recovering from various activity limitations.
The quantitative analysis determined the total number of appearances of each theme among all clinicians, the proportion of time each theme appeared with other themes within a text segment, the themes that were most commonly linked, and the FIM activities each theme tended to be linked to.
Results
Sample
The average age of all participants was 37.5 years old, with a standard deviation of 10.2 years. Twelve males and 21 females participated in the study. Of the 33 participants, there were 24 White, 4 African American, and 5 Asian individuals.
Frequency of Themes
There were a total of 16 themes identified in the clinician transcripts, which were grouped into six broad headings referred to as domains. Table 1 shows the number of times each theme was mentioned for all 33 clinicians. The most common theme was “building a foundation” (22 appearances), followed by “autonomy” (18 appearances); the least-common themes were “self-concept/self-esteem,” “frequency of event,” “life fulfillment,” and “physical environment accessibility” (4 appearances each).
Table 1.
Frequency of Themes and Multicoding
| Theme | Total # of Appearances (%) | % of Quotes That are Multicoded | Themes it Appears With (# of Times) |
|---|---|---|---|
| Procedural Reasoning Taxonomy | |||
| Building a Foundation | 22 (13.0%) | 50.0% | CB(1), AU(1), P(1), RPT(1), CE(1), LF+SI(1), BR(1), LF(1), BR+AD+CE(1), BR+SI+SA(1), AD+CE(1) |
| Balance of Recovery | 14 (8.3%) | 50.0% | AU(1), AD(1), RPT+AD(1), BF(1), AU+AD(1), BF+AD+CE(1), BF+SA+SI(1) |
| Frequency of Event | 4 (2.4%) | 75.0% | P(1), AD(1), RPT(1) |
| Conditional Reasoning Taxonomy | |||
| Acceptance of Deficit | 17 (10.1%) | 82.4% | P(1), RPT(2), AU+P(1), FE(1), BR(1), SA(1), CE(2), AU(1), BR+RPT(1), BR+AU(1), BF+BR+CE(1), BF+CE(1) |
| Personal/Privacy | 15 (8.9%) | 66.7% | FE(1), AD(1), AD+AU(1), BF(1), AU(1), RPT+CE(1), PR(2), PR+SA(1), CE(1) |
| Reflection of Personality Traits | 11 (6.5%) | 72.7% | AD(2), BF(1), P+CE(1), AU(1), SC/SE(1), BR+AD(1), FE(1) |
| Pride/Humiliation | 9 (5.3%) | 66.7% | CE(1), P(2), P+SA(1), SA(1), AU+CB(1) |
| Self-Concept/Self-Esteem | 4 (2.4%) | 25.0% | RPT(1) |
| Autonomy | 18 (10.7%) | 50.0% | BR(1), BF(1), P+AD(1), P(1), RPT(1), AD(1), BR+AD(1), LF(1), PR+CB(1) |
| Clinical Experience (Taxonomy linking theme) | 16 (9.5%) | 75.0% | SA(1), ADC(2), PR(1), BF(1), P+RPT(1), AD(2), P(1), BF+BR+AD(1), CB(1), AD+BF(1) |
| Ability to Direct Care/Communicate Need | 9 (5.3%) | 33.3% | SI(1), CE(2) |
| Life Fulfillment | 4 (2.4%) | 75.0% | LF+BF(1), AU(1), BF(1) |
| Social Acceptance | 9 (5.3%) | 77.8% | SI(2), CE(1), AD(1), P+PR(1), PR(1), BR+BF+SI(1) |
| Social Integration | 7 (4.1%) | 71.4% | SA(2), ADC(1), LF+BF(1), SA+BR+BF(1) |
| Caregiver Burden/Relationship | 6 (3.6%) | 50.0% | BF(1), AU+PR(1), CE(1) |
| Physical Environment Accessibility | 4 (2.4%) | 25.0% | SA+SI(1) |
Note. AD = Acceptance of Deficit; SA = Social Acceptance; CE = Clinical Experience; FE = Frequency of Event; LF = Life Fulfillment; RPT = Reflection of Personality Traits; SI = Social Integration; P = Personal/Privacy; PR = Pride/Humiliation; BF = Building a Foundation; AU = Autonomy; BR = Balance of Recovery; CB = Caregiver Burden/Relationship; ADC = Ability to Direct Care/Communicate Need; SC/SE = Self Concept/Self Esteem; PEACC = Physical Environment Accessibility.
Many of the clinician quotes had more than one theme present in them. Out of a total of 169 quotes, 103 quotes (60.9%) had two or more themes present. Table 1 displays the percentage of quotes coded as a particular theme that are multi-coded and the themes present in the multi-coded quotes.
Thematic Taxonomies
The domains were categorized into the procedural reasoning taxonomy, which contains 4 themes, and the conditional reasoning taxonomy, which contains 13 themes (see Figures 2 and 3). Across all clinicians, 23.7% and 66.8% of quotes were from the procedural and conditional reasoning taxonomies, respectively. The theme of clinical experience is present in both taxonomies, because the analysis of quotes coded “clinical experience” (9.5%) appeared to incorporate and synthesize past experiences with patients applying both conditional and procedural forms of reasoning. Because clinical experience appears to depend on both types of reasoning, it was conceptualized as the thematic bridge across the taxonomies and thus is present in both. As a thematic bridge, clinical experience provides a pathway to think about how procedurally oriented concerns can be combined with contextual insights.
Figure 2.
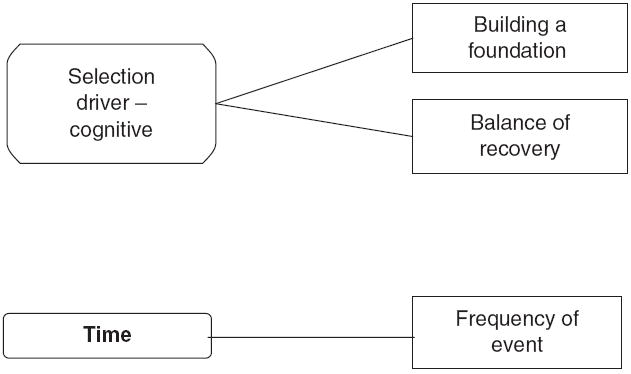
Procedural Reasoning Taxonomy
Figure 3.
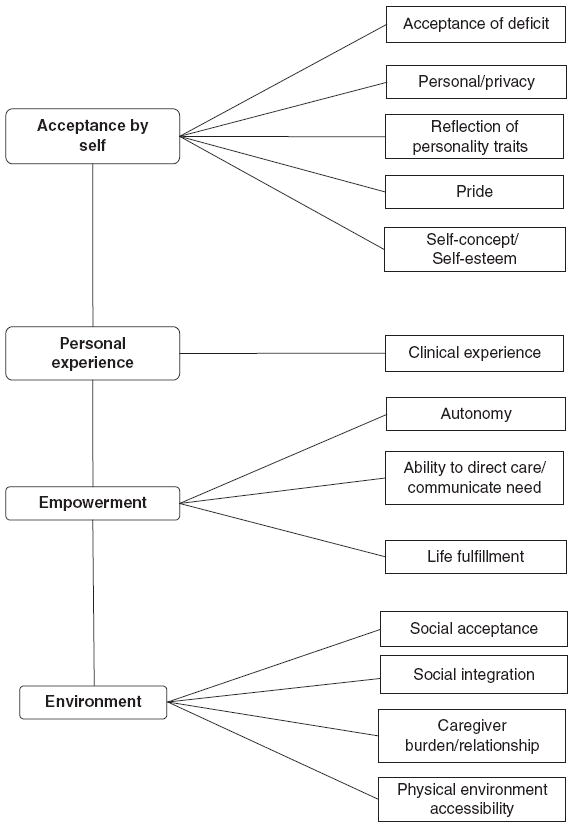
Conditional Reasoning Taxonomy
Quotes Illustrating Themes From the Procedural Reasoning Taxonomy
The procedural reasoning taxonomy is shown in Figure 2. This is a highly logic-based taxonomy. It expresses conceptual relationships between measurable and observable concepts about activity limitation according to interactions between the personal and environmental spheres of HEI. It includes three domains: selection drivers, clinical experience, and time. To illustrate the domains and themes, a short definition and a representative quote is included. Whenever possible, a quote with a single code was selected to illustrate each theme. The full codebook of complete definitions is available from the first author.
Selection Drivers
The selection drivers represent the logic-based strategies applied in establishing recovery preference priorities. Selection drivers include two themes: building a foundation and balance of recovery.
Building a foundation
When clinicians said that certain functions were critical for building their future recovery process, their remarks were coded as “building a foundation.” Some clinicians mentioned bladder and bowel management or bathing, which were coded as “building a foundation.” However, the cognitive FIM items were more commonly associated with this theme, as they were viewed as essential for starting the recovery process. The clinicians reasoned that having cognitive skills would allow him or her to compensate for disabilities in other areas. The following quote is an example of how a psychologist saw the cognitive items as an essential part of recovery. The quote further illustrates how the perceived importance of these fundamental activities resulted from her desires to interact with the environment.
I chose to recover in problem solving first, because that seemed the core of everything else. Once I can solve the problems I encounter, then it’s really going to be six feet in the right direction. Also, in order to solve problems effectively, I need to know what’s going on around me, so that is why comprehension is number 2. It is going to be quite frustrating if nobody can understand what I am going through, so that is why point number 3 is talk or express myself. It would be good to remember what I have done to solve the problems, so that is why memory is number 4.
Balance of recovery
Balance of recovery is distinct from building a foundation. Balance of recovery refers to a desire to progress in several areas simultaneously, instead of a desire to achieve gains in a few specific areas. The clinicians speculated that they would use those gains to help aid recovery in other areas, as described in this quote:
I want to be able to at least be able to do all of the activities with some assistance. You know rather than to go forward in any one, I would rather have more control in a wider spectrum of functions.
Time
The time domain contained one theme, “frequency of event,” and included a concern for how often or when help is needed in performing the activity in the day. The assumption is that an activity limitation that needs to be assisted only once or twice daily is less troubling than one that must occur throughout the day. For example, one female physician described her choice to make gains in bladder management before bowel management because she urinated more often than she had a bowel movement: “Bladder management first, because I tend to urinate more than I have a bowel movement, so if I could do that more independently that is more important.”
Quotes Illustrating Themes From the Conditional Reasoning Taxonomy
The conditional reasoning taxonomy is depicted in Figure 3. Compared to the procedural reasoning taxonomy, it is more complex and holistic. It is intended to reflect broader but less-measurable concepts about the subjective lifeworlds people find themselves inhabiting. Concepts emerge according to the reflection of the physical body, mental, social, and physical environment spheres of HEI within the internal life-world. The conditional reasoning taxonomy includes four broad domains: acceptance of self, personal experience, empowerment, and environment, several of which have multiple themes. Themes in this taxonomy are defined and presented in order as they appear in Figure 3, with example clinician quotes.
Acceptance of Self
The category “acceptance of self” included six subthemes: acceptance of deficit, personal/privacy, reflection of personality traits, pride, and self-concept/ self-esteem.
Acceptance of deficit
This code was used when clinicians’ narratives expressed recovery choices that were made based on their willingness to accept help in some areas in exchange for independence in other areas. Because the clinicians were limited to a certain number of moves for each stage of recovery, they had to prioritize their imagined functional goals. In many of these quotes, clinicians seemed to refer to their recovery choices as a trade-off. An example of this willingness to forego gains in one area to achieve them in another is described in this quote from a female nurse: “I am willing to be dependent physically with the exception of personal hygiene; I’d like to get that back first—bladder and bowel. I would be satisfied to be fully dependent physically, as long as I was not incontinent.”
Other clinicians were willing to get to the level of take longer/need a device as long as they were at that level in several FIM items. For example, a medical student noted she would rather have partial independence in many activities, than be completely independent in some items and completely dependent in other items. She stated, “I would rather be able to do things on my own, but with a device I would be able to do more things than be completely independent in some things and completely dependent on somebody for other things.”
Personal/privacy
Quotes coded as personal/ privacy expressed a desire to accomplish a task in private without the help of others. Bladder and bowel management and bathing were often the functional activities linked with the privacy theme, as seen in this quote from a male nurse: “And the other area of priority was bowel and bladder management which is kind of a personal issue and one that I would like to maintain some degree of independence with.” However, not all clinicians mentioned bowel and bladder management in quotes coded as personal/privacy. Some clinicians made choices for recovery based on how personal they considered various functions to be, as illustrated in this quote from a female nurse: “I continued to value expression of self, cognitive domains more so than physical, prioritizing the less personal as last, and the things that are most personal I would be able to do for myself.”
Reflection of personality traits
In quotes coded as reflection of personality traits, clinicians made recovery choices based on their personality or culture. Clinicians chose to recover in various areas, most commonly walking and the cognitive FIM items, because they saw themselves as verbal individuals, had a desire to be able to interact with others, or felt that they could tolerate having certain disabilities better than others. For example, one male physician made a recovery choice based on his personality type: “Essentially, the interaction with the world is really, you know, either by gesture or your words, and I guess I’m a pretty verbal person, so I felt that that was most important for me to express myself.”
Pride
The theme of pride appeared when clinicians referred to the desire to maintain their pride or dignity or avoid humiliation as a reason for their recovery choices. The theme of humiliation was grouped with pride instead of personal/privacy because humiliation was understood as a loss of pride or dignity, instead of a loss of privacy. All of the quotes coded as pride referred to bladder or bowel management. A female occupational therapist used the desire for privacy in toileting functions as her rationale for why she chose to recover in those areas first: “Well I chose bowel management, bladder management, and toileting first just for dignity reasons.”
Self-concept/self-esteem
The self-concept/self-esteem code was used when the clinicians commented on how the ability or inability to perform a particular task would impact on feelings about self. This code differed from personal/privacy and pride themes, which referred specifically to feelings of privacy, pride, or humiliation. The theme of self-concept/ self-esteem can be seen in this quote by a female psychologist: “Grooming and bathing, just because I think it would help my self-concept while I’m in the hospital, if I could actually comb my hair and take care of myself.”
Personal Experience
The broad domain of “personal experience” included one theme: clinical experience.
Clinical experience
When explaining their choices for recovery, some clinicians would use their medical knowledge or experience with patients to justify their choices for recovery. This theme appeared in both the procedural and conditional reasoning taxonomies, as it represented cognitive strategies that appeared to combine both types of reasoning. In examples of procedural reasoning strategies, some clinicians were willing to give up gains in mobility areas because they knew that adaptive equipment was available, whereas others sought to avoid devices such as feeding tubes or catheters. In examples of conditional reasoning strategies, other clinicians expressed their impressions about the feelings patients appeared to have as they observed them experiencing various types of activity limitations. Clinicians never spoke of their own experiences with illness or disability, but instead focused on their observations of others’ experiences with illness or disability. For example, the female nurse quoted below believed that comprehension and expressing oneself was very important based on her interactions with patients and her experiences as a clinician.
My experience has been that people who can’t understand what’s happening are terrified, and who can’t express themselves are terrified. If you can understand what’s happening and make needs known, then I have a lot of faith that the staff will help all these other things. And maybe that’s something that a lay person may not have the same confidence in. But because I work in this field I know that if I can express, understand and express, that I will get help. And that’s why the communication and the problem solving, and memory, which is part of comprehension, is pretty high on my list. [Note: this quote was double-coded with “ability to direct care.”]
Empowerment
The “empowerment” category included 3 themes, all of which relate to the ability of the individual to understand and take responsibility for his or her own welfare. These include autonomy, ability to direct care/communicate need, and life fulfillment.
Autonomy
In quotes coded as autonomy, clinicians expressed their desire to do a task by themselves and to be less reliant on others. Many clinicians expressed their desire to be able to perform toileting functions by themselves as their reason for why they chose to recover in certain areas, as seen in this quote from a female nurse: “In terms of ADLs [activities of daily living], toileting, and bladder and bowel management, that came next. Those are just basic vital needs that I would like to be able to meet on my own, and not be dependent for.”
Ability to direct care/communicate need
If a clinician expressed a desire to direct his or her own care and vocalize his or her needs and desires to others, the quote was coded as ability to direct care/ communicate need. All of the quotes coded as ability to direct care/communicate need focused on making gains in the cognitive FIM items. By regaining abilities in the cognitive FIM items, clinicians, like the female psychologist whose quote is shown below, thought that they could effectively communicate their needs and desires to others even if they were incapable of meeting those needs by themselves.
My first reasoning was that I felt like if I can communicate my needs, then I’m better likely to get my needs met, even if I can’t do them myself. So I wanted to be able to tell people what I needed, you know, my preferences about things.
Life fulfillment
In these quotes, clinicians made recovery choices based on a desire to increase the amount of satisfaction, enjoyment, or meaning in their lives. For example, in the following quote, a female medical student thought that early recovery in the cognitive FIM items would increase her life fulfillment:
I thought comprehension was most important, as were other cerebral areas, such as talking, expressing myself, memory, and social interaction. I thought those were the most important, because I felt like without your mind and your soul, and your ability to communicate with other people, life wouldn’t be quite as fulfilling.
Environment
This broad domain has 4 themes: social acceptance, social integration, caregiver burden/relationship, and physical environment accessibility.
Social acceptance
In quotes that expressed the theme of social acceptance, the clinicians referred to a desire to avoid having others shun or ignore them and to have positive social interactions. Many clinicians were particularly concerned with the impact of being able to bathe, groom themselves, or use the toilet on their social interactions, as evidenced by this quote from a female physician: “I chose to max out grooming to a completely independent level initially because that could be something that could benefit my image in public.” [Note: this theme was double-coded with “self-concept/self-esteem.”]
However, not all clinicians connected social acceptance with the physical FIM items. Some recognized the importance of cognition, as seen in the following quote by a female nurse:
Social interaction is important to me, because I will obviously be dependent on others and hopefully I will be able to have enough of a positive attitude that people will not try to avoid me, and will come when I ask them to assist me.
Social integration
While social acceptance deals with the concepts of having positive social interactions and avoiding being shunned or ignored, the theme social integration was present when clinicians expressed the desire to be included in social activities or to transact equally with others in the behavioral setting. Most clinicians talked about how cognitive and toileting functions would allow them to better integrate into society. One male physician thought that the ability to eat was important for integrating into society and relating to others:
Eating is so enjoyable, it is nice to be able you know interact while eating. It is a very social behavior. It is one of the most social behaviors that we do. And to have some ability to share a meal with people is very important.
Caregiver burden/relationship
Whereas social acceptance and social integration themes focus on society as a whole, caregiver burden/relationship themes focus specifically on those people who would have to care for the clinician if he or she was disabled. For quotes coded as caregiver burden/relationship, the clinicians showed a desire to achieve functional gains to make it easier for others to care for him or her. The caregiver burden/relationship quotes deal mainly with being independent in cognitive functions and bladder and bowel management. For example, some clinicians mentioned that they would prefer to regain abilities in tasks like bladder and bowel management, which others might find distasteful to provide them with assistance in performing.
I want independence in bowel and bladder, so I moved it to supervision, to put the least burden on anybody. As I move to supervision—people don’t mind watching you as much as they mind helping you. Then it becomes a lot easier for people to take care of you at this point. [male nurse; note: this quote was double-coded with “clinical experience”]
Physical environment accessibility
The theme of physical environment accessibility deals with the ability of a person to fully participate and perform activities in the physical environment. The physical environment factors are external to the individual and can have a “positive or negative impact on the individual’s . . . capacity to execute actions or tasks” (World Health Organization, 2001, p. 16). In explaining their recovery preferences, a few clinicians mentioned how certain abilities would affect their capacity to function in the environment around them. The following quote from a female psychologist demonstrates the theme of physical environment accessibility:
I didn’t at any point move stairs at all, just because I figured I can live in an apartment, and just getting in and out of my place we have an elevator . . . so if I cannot crawl up the stairs, it’s really not much of a problem.
Discussion
Themes discovered in the clinician transcripts could be classified into two linking taxonomies: the procedural reasoning taxonomy, which primarily reflects deductive choice strategies, and the conditional reasoning taxonomy, which primarily reflects inductive choice strategies. These taxonomies are bridged by the personal (clinical) experience domain, which includes both forms of reasoning.
Procedural and Conditional Thematic Taxonomies
Within the procedural reasoning taxonomy, a distinct subset of themes are present, reflecting the dominant clinical voice. Procedural reasoning is similar to the deductive hypothetical or propositional cognitive processes advocated in the medical problem-solving literature. Professional education based on the medical problem-solving model teaches clinicians how to see patients through the “medical gaze” (Good & Good, 1989). As a concept so innate to the practice of medicine, it is not surprising that building a foundation from the procedural reasoning taxonomy was the most common theme identified in the clinician transcripts. Building a foundation is akin to formulating a treatment plan. It involves planning an imaginary logical sequence of functional skill acquisition necessary to support the recovery of other skills. Balance of recovery and frequency of event, additional themes in the procedural reasoning taxonomy, represent similarly objective, logically important concepts. Themes from this taxonomy suggest that recovery choices are being made based on the functional usefulness of particular abilities, without consideration of a person’s particular desires, motivation, life contexts, or individual meanings of certain abilities. Because they are devoid of subjective context, procedural reasoning taxonomy themes represent the types of knowledge applied when analyzing the external lifeworld of the HEI spheres moving among various objective, unidimensional measures of relevance to people as they interact with the environment.
In contrast to the procedural reasoning taxonomy, the conditional reasoning taxonomy themes primarily reflect clinicians’ subjective thoughts as they attempt to imagine how specific activity limitations might change their personal lifeworlds. Themes were deliberately arranged so that the top of the taxonomy reflects perceptions of self, whereas themes at the base are related to the social and physical environments surrounding the person. Empowerment at the mid-portion of the taxonomy includes themes that express how recovery of particular activity limitations would shape an individual’s potential to interact with and take control of his or her life within the environment. Themes at the bottom of the taxonomy relate to contexts that arise from the environment.
Autonomy and acceptance of deficit were the most frequently coded themes of the conditional reasoning taxonomy. Interestingly, these themes related to antithetical concepts: the desire for independence and the acceptance of help, reflecting concepts of recovery trade-offs inherent within the choice-making procedures of RPE. The conditional reasoning taxonomy includes themes reflective of the internal lifeworld. Conditional reasoning is needed to translate measurable information from the external lifeworld (mind, body, physical world, and society spheres of HEI) into its internal lifeworld meanings (see Figure 1). In general, most conditional taxonomy themes that appeared in the clinician transcripts cannot be limited to a single mind, body, physical environment, or society sphere, and therefore the connections among the spheres of HEI are not segmented as they are in the procedural reasoning taxonomy. For example, the theme of social acceptance might appear to be a society-based theme. However, this theme also contains elements of the mind sphere, because it deals with how subjects believe others perceive them. Social integration involved the desire to transact equally with others in the social setting. This theme encompasses the society sphere (social setting), the mind (what the person with disabilities might perceive as transacting equally), and the body (the physical motor skills that are needed to transact). Quotes describing the clinician’s recovery preferences were commonly coded for multiple themes, introducing the possibility of even greater complexities as more spheres interact with each other without quantifiable limits to form the context for the clinician’s choices.
Because of the professional expertise and knowledge they bring, we would expect that clinicians would tend to use procedural reasoning in preference to conditional reasoning when imagining optimal recovery patterns. This was not the case. Just over two-thirds of all quotes were from the conditional reasoning taxonomy (66.8%), compared to only 23.7% from the procedural reasoning taxonomy. This suggests that the clinicians actually relied more heavily on inductive than on deductive forms of logic when performing RPE. It might be that the experience of imagining disability during RPE stimulated clinicians’ tendencies to think conditionally rather than procedurally. If this is true, RPE might prove a way to bridge the internal and external lifeworlds, or at least to help clinicians appreciate the subjective experience of disability as a lived phenomenon.
Bridging the Taxonomies
The theme clinical experience expresses the clinician’s passageway from the objective toward the subjective lifeworld of the imagined patient. Procedural reasoning is a part of this theme because the clinician uses medical knowledge and experience to identify a problem and the need for a solution. Conditional reasoning is evident as the clinician tries to solve this problem. Instead of just using one’s acquired professional knowledge to solve the problem of imagined disability (procedural reasoning), the clinician begins to imagine how the disability would affect the self within one’s lifeworld (conditional reasoning). Personal experience, which for the clinician primarily reflected their clinical experience, operates as a thematic bridge linking the procedural and conditional taxonomies. It symbolizes the flow and synthesis of thoughts through multiple concepts and levels of reasoning.
Applications to Training and Practice
The spheres of HEI provide a mechanism for further conceptualizing the thematic taxonomies. They help clarify relationships between procedural and conditional reasoning when expanding attempts to consider the patient’s experiences of disability beyond the medical diagnosis. HEI views people as beings whose activities can be either facilitated or impeded by both internal and external lifeworld contexts. When setting therapeutic objectives to reduce activity limitation, procedural reasoning is used to measure mental and physical impairment. Similarly, procedural reasoning allows the clinician to understand how activity limitations translate into problems the patient will face when interacting with the environment. Clinical observations, tests, and various imaging techniques in medicine all relate to understanding the external (or physical) rather than the internal (subjective) lifeworld. Each measurable sphere—the body, mind, physical environment, and society, with all their interconnections—has a corresponding, not directly measurable representation in HEI, reflecting the personal internal lifeworld. Conditional reasoning will be essential when recognizing the affect of disability on perceptions within that internal world (Mattingly & Fleming, 1994). Conditional reasoning will allow for individual interpretations of the subjective experience of impairment and its phenomenological expression as meanings according to personal circumstances. Because the external and internal lifeworlds and the types of reasoning needed to understand each are so different, a link is needed between the two worlds. With further research, we might find that RPE can serve as this link.
We believe that the ultimate value of RPE might prove to be in its potential to enhance conditional reasoning among interdisciplinary teams of patients, clinicians, and caregivers. Toward this end, RPE might be applied in educating nurses, physicians, and therapists about the implications of living with disabilities. The process of imagining recovery though RPE might help practitioners understand the inside lifeworlds of patients with disabilities, albeit from the outside. It might further increase their tendency to use conditional reasoning when thinking about disability and treatment planning. With their newfound perspective, clinicians will be better prepared for face-to-face encounters with patients as they begin the process of interactive reasoning, the third and most essential form. Applying interactive reasoning, clinicians can traverse the traditional clinician–patient divide. They are primed to ask and listen to patient answers to questions such as, “How do you feel about treatments?” and “How can I tailor treatments to you?” The best answers to these questions depend on the balanced application of all three forms of reasoning to both the quantitative and qualitative expressions of interactions among body, mind, society, and physical environment.
The thematic taxonomies presented are incomplete because although they capture procedural and conditional reasoning, they could not include themes for interactive reasoning. To obtain themes appropriate to informing interactive reasoning, RPE will need to be completed with patients, because values expressed by patients will be necessary to achieve a legitimate understanding of disability as a lived experience. Yet, it is encouraging that some of the themes emerging from the clinician taxonomies reflect concepts identified as important by persons with disabilities, such as issues relevant to an accessible and usable environments (Lutz & Bowers, 2005).
Ultimately, it will be the match between self-perception and how underlying impairments in conjunction with the structure of the surrounding environment affects a person’s abilities to perform the activities most important to him or her. Interactive reasoning, by definition, focuses on discovering the best ways for clinicians to interact with and understand the needs of patients. Consequently, it describes more a process than content. In future work we hope to explore ways to combine patients’ and clinicians’ experiences of the RPE process, in an effort to enhance clinicians’ capacities to supplement procedural with conditional reasoning, thus better informing the interactive reasoning process. We believe combining clinician and patient RPE experiences could enhance the quality of clinicians’ interactive reasoning, “lessoning the divide” between the clinician’s lens and the patient’s voice (Crow, 1996). If this future work proves successful, RPE might yield a deeper understanding of patient values, offering the means to make the patient’s personal life focus central to clinical and research interventions.
Acknowledgments
We acknowledge the many individuals who contributed to various aspects of this project. The research reported in this article was funded through the National Institutes of Health (R21-HD04588).
Biographies
Margaret G. Stineman, MD, is a professor of physical medicine and rehabilitation in the Departments of Physical Medicine and Rehabilitation, and a professor of epidemiology in the Center for Clinical Epidemiology and Biostatistics, University of Pennsylvania, Philadelphia, Pennsylvania, USA.
Pamela M. Rist, BSE, was a research assistant at the Department of Physical Medicine and Rehabilitation, University of Pennsylvania, Philadelphia, Pennsylvania, USA, at the time of this research, and is currently a candidate for the 2-year Master of Science degree from the Department of Epidemiology at the Harvard School of Public Health, Boston, Massachusetts, USA.
Janice P. Burke, OTR, PhD, is the chair and professor at the Department of Occupational Therapy, Thomas Jefferson University, Philadelphia, Pennsylvania, USA.
Footnotes
Note A blank game board is shown as Figure 1 in Kurz et al. (2008). An earlier version appears in Stineman et al. (1998).
Contributor Information
Margaret G. Stineman, University of Pennsylvania, Philadelphia, Pennsylvania, USA
Pamela M. Rist, University of Pennsylvania, Philadelphia, Pennsylvania, USA
Janice P. Burke, Thomas Jefferson University, Philadelphia, Pennsylvania, USA
References
- Barry CA, Stevenson FA, Britten N, Barber N, Bradley CP. Giving voice to the lifeworld. More humane, more effective medical care? A qualitative study of doctor-patient communication in general practice. Social Science & Medicine. 2001;54:487–505. doi: 10.1016/s0277-9536(00)00351-8. [DOI] [PubMed] [Google Scholar]
- Benner P, Tanner C. Clinical judgment: How expert nurses use intuition. American Journal of Nursing. 1987;87(1):23–31. [PubMed] [Google Scholar]
- Cohn ES. Fieldwork education: Shaping a foundation for clinical reasoning. American Journal of Occupational Therapy. 1989;43(4):240–244. doi: 10.5014/ajot.43.4.240. [DOI] [PubMed] [Google Scholar]
- Coles R. The call of stories. Boston: Houghton Mifflin Company; 1989. [Google Scholar]
- Creswell JW, Fetters MD, Ivankova NV. Designing a mixed methods study in primary care. Annals of Family Medicine. 2004;2(1):7–12. doi: 10.1370/afm.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow L, editor. Exploring the divide. Leeds: Disability Press; 1996. Chapter 4: Including all of our lives: Renewing the social model of disability. [Google Scholar]
- Dreyfus H. Mind over machine: The power of human intuition and expertise in the ear of the computer. New York: Free Press; 1986. [Google Scholar]
- Feffer M, Jahelka M. Implications of the decentering concept for the structuring of projective content. Journal of Consulting and Clinical Psychology. 1968;32(4):434–441. doi: 10.1037/h0026101. [DOI] [PubMed] [Google Scholar]
- Glaser BG, Strauss AL. The discovery of grounded theory: Strategies for qualitative research. New York: Aldine De Gruyter; 1967. [Google Scholar]
- Good BJ, DelVecchio Good MJ. “Fiction” and “historicity” in doctors’ stories: Social and narrative dimensions of learning medicine. In: Garro CMLC, editor. Narrative and the cultural construction of illness and healing. Berkeley: University of California Press; 2000. pp. 50–69. [Google Scholar]
- Good M, Good B. Disabling practitioners: Hazards of learning to be a doctor in American medical education. American Journal of Orthopsychiatry. 1989;59(2):303–309. doi: 10.1111/j.1939-0025.1989.tb01663.x. [DOI] [PubMed] [Google Scholar]
- Granger CV, Hamilton BB, Keith RA, Zielezny M, Sherwin F. Advances in functional assessment for medical rehabilitation. Topics in Geriatric Rehabilitation. 1986;1:59–74. [Google Scholar]
- Hamilton BB, Granger CV, Sherwin FS, Zielezny M, Tashman JS. A uniform national data system for medical rehabilitation. In: Fuhrer MJ, editor. Rehabilitation outcomes: Analysis and measurement. Baltimore, MD: Paul H Brookes; 1987. [Google Scholar]
- Jensen GM, Shepard KF, Hack LM. The novice versus the experienced clinician: Insights into the work of the physical therapist. Physical Therapy. 1990;70(5):314–323. doi: 10.1093/ptj/70.5.314. [DOI] [PubMed] [Google Scholar]
- Klienman A. Patients and healers in the context of culture. Los Angeles: University of California Press; 1980. [Google Scholar]
- Kurz AE, Saint-Louis N, Burke JP, Stineman MG. Exploring the personal reality of disability and recovery: A tool for empowering the rehabilitation process. Qualitative Health Research. 2008;18(1):90–105. doi: 10.1177/1049732307309006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutz BJ, Bowers BJ. Disability in everyday life. Qualitative Health Research. 2005;15:1037–1054. doi: 10.1177/1049732305278631. [DOI] [PubMed] [Google Scholar]
- Mattingly C, Fleming MH. Clinical reasoning forms of inquiry in a therapeutic practice. Philadelphia: F.A Davis; 1994. [Google Scholar]
- National Institutes of Health Office of Behavioral and Social Science Research. Qualitative methods in health research: Opportunities and considerations in application and review, organized by the NIH culture and qualitative research interest group. 1999 Retrieved October 18, 2004, from http://obssr.od.nih.gov/Documents/Publications/Qualitative.PDF.
- Neistadt ME, Seymour SG. Treatment activity preferences of occupational therapists in adult physical dysfunction settings. American Journal of Occupational Therapy. 1995;49(5):437–443. doi: 10.5014/ajot.49.5.437. [DOI] [PubMed] [Google Scholar]
- Polanyi M. The tacit dimension. Garden City, NY: Doubleday; 1967. [Google Scholar]
- Qualis Research Associates. Ethnograph Version 5.08 [computer software] 2001 Available from www.QualisResearch.com.
- Rist P, Freas D, Maislin G, Stineman G. An analysis of recovery preference exploration: Rehabilitation professionals’ beliefs about recovery. Archives of Physical Medicine & Rehabilitation. 2008;89:1600–1606. doi: 10.1016/j.apmr.2007.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schon D. The reflective practitioner: How professionals think in action. Basic Books; 1983. [Google Scholar]
- Sox HC, Blatt MA, Higgins MC, Marton KI. Medical decision making. Boston: Butterworth; 1988. [Google Scholar]
- Stewart D, Mickunas A. Exploring phenomenology: A guide to the field and its literature. Athens: Ohio University Press; 1990. [Google Scholar]
- Stineman MG. Medical humanism and empowerment in medicine. Disability Studies Quarterly. 2000;20(1):11–16. [Google Scholar]
- Stineman MG. A model of health environmental integration. Topics in Stroke Rehabilitation. 2001;8(2):34–45. doi: 10.1310/0L5G-NQHY-GH4K-HV58. [DOI] [PubMed] [Google Scholar]
- Stineman MG, Maislin G, Nosek M, Fiedler R, Granger CV. Comparing consumer and clinician values for alternative functional states: Application of a new feature trade-off consensus building tool. Archives of Physical Medicine and Rehabilitation. 1998;79:1522–1529. doi: 10.1016/s0003-9993(98)90413-0. [DOI] [PubMed] [Google Scholar]
- Stineman MG, Ross RN, Maislin G, Gray D. Population-based study of home accessibility features and the activities of daily living: Clinical and policy implications. Disability & Rehabilitation. 2007;29:1165–1175. doi: 10.1080/09638280600976145. [DOI] [PubMed] [Google Scholar]
- Stineman MG, Ross RN, Maislin G, Marchuk N, Hijirida S, Weiner M. Recovery preference exploration. American Journal of Physical Medicine & Rehabilitation. 2007;86(4):272–281. doi: 10.1097/PHM.0b013e3180383acb. [DOI] [PubMed] [Google Scholar]
- Van de Ven AH, Delbecq AL. The nominal group as a research instrument for exploratory health studies. American Journal of Public Health. 1972;62(3):337–342. doi: 10.2105/ajph.62.3.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitman N. A review of constructivism: Understanding and using a relatively new theory. Family Medicine. 1993;25(8):517–521. [PubMed] [Google Scholar]
- World Health Organization. International classification of functioning, disability and health: ICF. Geneva: Author; 2001. [Google Scholar]


