Abstract
Objectives
This study examined differences in the trajectory of depressive symptoms between Hispanic, black, and white Americans in middle and old age.
Methods
Data came from a national sample of Americans with up to 6 repeated assessments spanning 11 years. Hierarchical linear models with time-varying covariates were used.
Results
Hispanics started with the worst depressive symptomatology, followed by black Americans, while white Americans had the fewest symptoms. These differences, however, diminished over time. More importantly, net of socioeconomic and health differentials, the depressive symptoms trajectory did not differ between blacks and whites; while Hispanics still started with worse symptoms and had a greater rate of reduction in symptomatology compared to whites.
Discussion
Significant ethnic differences exist in both the intercept and rate of change in depressive symptoms in middle aged and older Americans. These variations are substantially confounded by socioeconomic and health differentials.
Keywords: depressive symptoms, hierarchical linear models, Hispanics, race, ethnicity
INTRODUCTION
A number of longitudinal studies have documented that depressive symptoms rise moderately after midlife (Kim & Durden, 2007; Mirowsky & Kim, 2007; Yang, 2007). There is also evidence that the increase in depressive symptoms is a function of socioeconomic status (SES) and health conditions in late life. With SES and health adjusted, depressive symptoms tend to decrease slightly in old age (Lynch & George, 2002; Mirowsky & Ross, 1992; Steffen et al., 2005; Yang 2007).
There is, however, very limited understanding of ethnic variations in depressive symptom changes over time. Little is known about the trajectory of depressive symptoms among Hispanic Americans and how it compares with that of white and black Americans. A number of hypotheses, such as the double jeopardy, cumulative disadvantage, age-as-leveler, and persistent health inequality, provide insights for understanding ethnic differences in health changes (Dannefer 2003; Dowd & Bengtson 1978; Ferraro & Farmer 1996a). For instance, the double jeopardy theory posits that being both old and an ethnic minority creates a double disadvantage to the health of older minorities (Ferraro & Farmer 1996a). Cumulative disadvantage suggests that the health gap between ethnic groups increases with age (Dannefer, 2003), while persistent health inequality postulates stability in ethnic differences in heath (Ferraro & Farmer 1996a). In contrast, the concept of age-as-leveler proposes that racial inequality in health decreases with advancing age because the basic challenges of aging on health supersedes the impact of racial discrimination or the coping strategies adopted by minority persons to deal with racial discrimination throughout the life course may help in dealing with age discrimination (Ferraro & Farmer 1996a). Nevertheless, empirical studies on these hypotheses are largely based on analyses of physical health measures. Few of them have focused on changes in depressive symptoms.
Among the limited number of studies of racial differences in depressive symptomatology, the analyses have focused on black/white or white/non-white differences (e.g., George & Lynch 2003, Klein, Shankman, & Rose 2008, Lynch & George 2002, Taylor & Lynch 2004). Many important research questions remain unanswered. For example, what is the trajectory of depressive symptoms like among Hispanics? Do Hispanics have the same rate of change in depressive symptoms as whites and blacks? These are serious gaps in knowledge given the increasingly diverse U.S. population (Angel & Angel, 2006).
In addition, research on ethnic differences in changes in depressive symptoms could be significantly improved by being more dynamic with the incorporation of time-varying covariates. This is because explanatory variables of depressive symptoms (e.g., marital status, income, and prior health conditions) may change substantially over time. This is particularly true if a long period of observation is involved (e.g., 10 or more years).
The present study aims to fill these important gaps by characterizing the trajectory of depressive symptoms in middle aged and older Americans and how it differs across Hispanic, black, and white Americans. We address these research questions using data from a national sample of Americans aged 51 and older with up to 6 repeated assessments over 11 years, and dynamic models incorporating time-varying covariates.
In the following, we offer several hypotheses regarding ethnic differences in the trajectory of depressive symptoms. These hypotheses are grounded in a conceptual framework that ethnicity, age, gender and SES are key dimensions of social stratification, with SES being a function of the other three. Moreover, ethnic differences in the trajectory of depressive symptoms are partially mediated by socioeconomic and health status. Similar frameworks have been articulated by other investigators for analyzing health changes in adulthood (Crimmins & Seeman, 2001; House, Lantz, & Herd, 2005).
Hypothesis 1: Among individuals age 51 and over, blacks and Hispanics have higher levels of depressive symptoms than whites, with Hispanics having the highest symptomatology (H1a). However, relative to whites, blacks and Hispanics have more moderate rates of increase over time (H1b). Finally, Hispanics have a more gradual increase in depressive symptoms than blacks (H1c).
One would expect significant ethnic variations in the trajectory of depressive symptoms because of ethnic stratification, a system involving ethnic groups interacting in patterns of dominance and subordination (Jackson, Antonucci, & Gibson, 1990; Williams, 1997). Ethnic stratification may influence physical and mental health through several mechanisms, including less advantaged socioeconomic position, constraints placed on life style choices, or stress as a result of perception of discrimination (Crimmins, Hayward, & Seeman, 2004; Robert & House 2000). These processes may expose members of minority groups to greater depressive symptomatology compared to whites. Moreover, there is evidence that Hispanic elders exhibit greater depressive symptoms than older blacks (Mui, 1993). Therefore, we hypothesize that blacks and Hispanics have greater depressive symptoms than whites, and that Hispanics suffer even worse symptomatology than blacks (H1a).
With regard to the rate of change in depressive symptoms, the double jeopardy and cumulative disadvantage hypotheses both suggest that the effect of being minorities on health increases over the life course (Dowd & Bengtson 1978; Dannefer 2003). In contrast, the age-as-leveler and persistent health inequality hypotheses posit that ethnic inequalities in health should decrease or remain stable as people get older (Ferraro & Farmer, 1996a). Moreover, there is evidence that socioeconomic disparities in health diminish after early old age (House et al., 2005), suggesting potential decreases in ethnic differences in depressive symptoms in late life. Empirical evidence for these competing hypotheses has been largely based on studies of physical health measures (Ferraro & Farmer, 1996b; Kelley-Moore & Ferraro, 2004; Mendes de Leon, Barnes, Bienias, Skarupski, & Evans, 2005). Only a few longitudinal studies have examined this issue for depressive symptoms. Based on these longitudinal analyses, there is some evidence that changes in depressive symptoms over time among black/non-white elders were more moderate than those among whites (George & Lynch, 2003; Klein et al. 2008), supporting the notion that there are decreases in ethnic differences in depressive symptoms in late life.
We are unaware of any research comparing Hispanics and blacks in the trajectory of depressive symptoms. However, given that there is some evidence for diminishing ethnic differences in depressive symptoms in late life and our hypothesis that Hispanics have the highest symptomatology while white Americans have the lowest symptomatology, we further postulate that blacks and Hispanics have more moderate rates of increase in depressive symptoms over time in comparison to whites (H1b) and that Hispanics have a more gradual increase than blacks (H1c).
Hypothesis 2: Adjusting for population heterogeneity (e.g., SES and health status), among individuals age 51 and over, blacks, Hispanics, and whites have comparable levels of depressive symptoms (H2a), but blacks and Hispanics have greater rates of reduction in symptomatology (H2b). Finally, net of SES and health effects, the rate of change in depressive symptoms are more moderate in Hispanics than in blacks (H2c).
The important role of socioeconomic position in influencing depressive symptomatology has been consistently documented (Everson, Siobhan, Lynch, & Kaplan, 2002). Prior research suggests that deteriorating health and increasing impairments in old age are associated with decline in feelings of personal control (Schulz, Heckhausen, & O’Brien, 1994; Shaw & Krause, 2001), which in turn is significantly associated with increased emotional distress (Mirowsky & Ross, 1992; Seligman & Altenor, 1980). Ethnic minorities have disadvantageous SES and shoulder a disproportionate burden of diseases and disability (Centers for Disease Control and Prevention, 2005; Oliver & Muntaner, 2005). The stress and strain from both lower SES and poor health among members of ethnic minority groups may induce higher levels of psychological distress (George & Lynch, 2003).
Evidence from cross-sectional studies supports that after adjustment of SES and health, there is comparable psychological distress among black and Hispanic Americans than whites (Bromberger, Harlow, Avis, Kravitz, & Cordal, 2004). Most longitudinal studies also showed a level of depressive symptoms in blacks/non-whites similar to that among whites after population heterogeneity was controlled (Klein et al., 2008; Lynch & George 2002; Yang, 2007). However, some investigators observed fewer symptoms among blacks (Taylor & Lynch, 2004) or more symptoms among blacks/non-whites (Kim & Durden 2007; Skarupski et al., 2005). Based on the predominant evidence, we hypothesize that blacks, Hispanics, and whites have comparable levels of symptomatology, when their SES and health differentials are controlled (H2a).
There is strong evidence that adjusting for population heterogeneity, depressive symptoms tend to decrease slightly over time in old age (Lynch & George, 2002; Mirowsky & Ross, 1992; Steffens et al., 2005; Yang, 2007). However, ethnic differences in the rate of change in depressive symptoms net of population heterogeneity are less clear. Previous research found that the negative effects of old age on the sense of mastery are stronger in whites than African Americans, suggesting more resilience to psychological distress associated with advancing age among blacks (Jang, Borenstein-Graves, Haley, Small, & Mortimer, 2003). Williams and Lawler (2001) also proposed the hardiness hypothesis positing that minorities may become better off in old age because of surviving a highly selective process. Hence, we hypothesize that adjusting for variations in SES and health, blacks and Hispanics have greater rates of improvement in depressive symptoms compared to white Americans (H2b).
There is no prior research concerning how blacks and Hispanics differ in the rate of change in depressive symptoms and how these differences relate to SES and health status. However, according to the notion of Hispanic paradox, Hispanics, despite their socioeconomic disadvantages, have similar or better health outcomes than non-Hispanic Americans (Markides & Black, 1996). This suggests a smaller health affect of SES among Hispanics. Therefore, we further hypothesize that the rate of reduction in depressive symptoms among Hispanics is more moderate than blacks after adjusting for SES and health differentials (H2c).
METHODS
Data and Design
Data for this study came from the Health and Retirement Study (HRS) which began in 1992 by surveying a national sample of 12,654 persons born in 1931–1941. In 1993, its companion study, the Asset and Health Dynamics among the Oldest Old (AHEAD), was launched with a national sample of 8,222 individuals age 70 and over (i.e., born before 1924). Beginning in 1998, the fourth wave of the HRS was fully integrated with the third wave of the AHEAD. Two additional cohorts, Children of the Depression (CODA) (2,320 persons born in 1924–1930) and War Babies (WB) (2,529 persons born in 1942–1947) were also added to the HRS in 1998. Biennial interviews have been conducted thereafter. As of 2006, these four components of HRS yielded a nationally representative sample of Americans age 51 and over. Spanish version questionnaires have been administered by bilingual interviewers to Spanish-speaking respondents.
For our analysis, baseline was defined as 1995 for AHEAD, 1996 for HRS, and 1998 for CODA and WB. Follow-up data came from 1998 (for AHEAD and HRS cohorts), 2000, 2002, 2004, and 2006. HRS data collected in 1992 and 1994 and AHEAD data in 1993 were excluded because: 1) questions on depressive symptoms and response options were asked differently in 1992 and 1994, and 2) several questions of physical functioning status (a key explanatory variable) were not asked consistently in these earlier years.
A total of 22,185 individuals aged 51 and older completed the baseline interviews. We excluded 734 respondents who reported an ethnic group other than Hispanic, non-Hispanic white, or non-Hispanic black and 2,657 respondents who had zero analytical weights (mostly age-ineligible spouses and respondents living outside the U.S. or institutionalized), and 905 respondents with proxy interviews. Our dynamic specifications required several time-varying covariates, including lagged measures and their changes between two adjacent waves. Therefore, we further excluded 693 individuals who never responded to consecutive interviews between 1995 and 2006, because they had no observations with valid data on lagged covariates and change terms. The final analytical sample consisted of 17,196 individuals contributing to 64,674 observations.
Measures
Depressive symptoms were measured by an abbreviated version of the Center for Epidemiologic Studies Depression (CES-D) scale, which has been shown to be internally consistent with the factor structure of prior versions of the CES-D (Turvey, Wallace, & Herzog, 1999). The scale composed of nine dichotomous items (i.e., yes/no), indicating the respondent’s feelings much of the time over the week prior to the interview (Standardized Cronbach’s alpha = 0.80). These items included: (a) felt depressed, (b) felt that everything was an effort, (c) sleep was restless, (d) felt lonely, (e) felt sad, (f) could not get going, (g) felt happy, (h) enjoyed life, and (i) had a lot of energy. A summary score (score range: 0–9) was constructed such that a higher score reflected more negative affect during the previous week. The CES-D scale has been widely used to study depressive symptoms in white, black, and Hispanic Americans and has demonstrated reasonable reliability and validity (Davidson, Feldman, & Crawford, 1994; Liang, Van Tran, Krause, & Markides, 1989; Radloff, 1977; Swenson, Baxter, Shetterly, Scarbro, & Hamman, 2000).
Several measures of social stratification were included. Age differences were measured by age in 1995. Dummy variables of gender and ethnicity (non-Hispanic white, non-Hispanic black, and Hispanic) were created. Education was indexed by years of schooling, whereas household income was indicated using inflation adjusted 2006 dollars (in $1,000s).
Other covariates included marital status, constructed as a dummy variable (1 = married or living with a partner, and 0 = otherwise), and several measures of health status. In particular, burden of diseases was a count of seven health conditions (i.e., heart disease, cancer, stroke, diabetes, hypertension, lung disease, and arthritis). Self-rated health was a single item rating of the respondent’s health (1 = excellent, 2 = very good, 3 = good, 4 = fair, and 5 = poor). Functional status (score range: 0–11) entailed a count of difficulties with six activities of daily living (ADLs) (i.e., dressing, walking, bathing or showering, eating, getting in or out of bed, and using the toilet) and five instrumental activities of daily living (IADLs) (i.e., preparing hot meals, grocery shopping, making phone calls, taking medications, and managing own money and expenses).
To better reflect the dynamics of depressive symptoms, a number of covariates (i.e., income, marital status, diseases, functional status, and self-rated health) were specified as varying with time. To ensure a clear time sequence between the time-varying covariates and the outcome variable, we used the lagged measure (i.e., value from the last wave of interview) and the change term (i.e., change in the value between two adjacent waves) for each of the time-varying covariates. For instance, marital status was included as a lagged covariate and as the change in status (−1 for dissolutions, 0 for no change, and 1 for the acquisition of a partner). Table 1 presents the descriptive statistics of all variables.
Table 1.
Descriptive statistics of time-varying and time constant covariates
| Time Varying Covariates | 1998 (n=13,139) |
2000 (n=14,999) |
2002 (n=13,185) |
2004 (n=12,139) |
2006 (n=11,212) |
|---|---|---|---|---|---|
| CES-D | 2.09 ± 2.18 | 1.98 ± 2.13 | 1.92 ± 2.15 | 1.86 ± 2.14 | 1.89 ± 2.15 |
| Time since baseline (in years) | 2.36 ± 0.48 | 3.78 ± 1.07 | 5.75 ± 1.06 | 7.70 ± 1.04 | 9.67 ± 1.03 |
| Marriedt-1 | 9,360 (71%) | 10,491 (70%) | 8,790 (67%) | 7,966 (66%) | 7,300 (65%) |
| Δ Marital statust-1,t | −0.02 ± 0.14 | −0.05 ± 0.27 | −0.03 ± 0.21 | −0.02 ± 0.20 | −0.03 ± 0.21 |
| Household incomet-1 | 59.38 ± 83.77 | 62.55 ± 90.61 | 63.39 ± 103.72 | 61.75 ± 90.34 | 73.35 ± 73.51 |
| Δ Household incomet-1,t | −0.32 ± 92.22 | −1.39 ± 88.60 | −3.56 ± 86.73 | 10.15 ± 107.12 | −4.33 ± 93.69 |
| Self-rated healtht-1 | 2.66 ± 1.13 | 2.80 ± 1.13 | 2.70 ± 1.09 | 2.75 ± 1.08 | 2.81 ± 1.08 |
| Δ Self-rated healtht-1,t | 0.25 ± 0.92 | −0.04 ± 0.90 | 0.11 ± 0.88 | 0.11 ± 0.86 | 0.07 ± 0.86 |
| Diseasest-1 | 1.55 ± 1.21 | 1.61 ± 1.24 | 1.69 ± 1.24 | 1.85 ± 1.27 | 1.99 ± 1.28 |
| Δ Diseasest-1,t | 0.20 ± 0.56 | 0.13 ± 0.58 | 0.22 ± 0.58 | 0.18 ± 0.58 | 0.18 ± 0.57 |
| Functional statust-1 | 0.36 ± 1.17 | 0.35 ± 1.20 | 0.35 ± 1.17 | 0.50 ± 1.29 | 0.53 ± 1.35 |
| Δ Functional statust-1,t | 0.12 ± 1.16 | 0.07 ± 1.08 | 0.26 ± 1.19 | 0.14 ± 1.11 | 0.08 ± 1.16 |
| Time Constant Covariates | Total (n=17,196) |
White (n=13,644) |
Black (n=2,340) |
Hispanic (n=1,212) |
P value |
|---|---|---|---|---|---|
| Died (between baseline and 2006) | 4,061 (24%) | 3,207 (24%) | 603 (26%) | 251 (21%) | .0028 |
| Ever attrited (between baseline and 2006) | 1,537 (9%) | 1,132 (8%) | 268 (11%) | 137 (11%) | <.0001 |
| Age (in 1995) | 63.97 ± 10.23 | 64.32 ± 10.06 | 62.80 ± 9.93 | 62.28 ± 9.44 | <.0001 |
| Female | 10,061 (59%) | 7,832 (57%) | 1,506 (64%) | 723 (60%) | <.0001 |
| Education | 12.08 ± 3.27 | 12.64 ± 2.75 | 10.81 ± 3.53 | 8.30 ± 4.62 | <.0001 |
| Baseline marital status | 12,205 (71%) | 10,143 (74%) | 1,217 (52%) | 845 (70%) | <.0001 |
| Baseline self-rated health | 2.67 ± 1.14 | 2.56 ± 1.11 | 3.06 ± 1.14 | 3.15 ± 1.17 | <.0001 |
| Baseline disease | 1.51 ± 1.22 | 1.47 ± 1.21 | 1.77 ± 1.24 | 1.40 ± 1.20 | <.0001 |
| Baseline functional status | 0.35 ± 1.16 | 0.29 ± 1.05 | 0.59 ± 1.51 | 0.56 ± 1.47 | <.0001 |
| Baseline CES-D | 1.71 ± 1.96 | 1.57 ± 1.84 | 2.15 ± 2.16 | 2.46 ± 2.44 | <.0001 |
Note: Statistics are reported as mean ± standard deviation or n (%). Time varying covariates are those associated with repeated observations within individuals. Data based on the 1995–2006 Health and Retirement Study (HRS).
Data Analysis
We used hierarchical linear models (HLM) (Raudenbush & Bryk, 2002) to depict the trajectory of depressive symptoms. Specifically, depressive symptoms (CES-Dit) for individual i at time t are specified in the following level-1 model:
| (1) |
TIMEit represents the number of years since the baseline interview. Xkit (where k = 1, …, K) denotes the kth time-varying covariate for individual i at time t. βk represents the effect of the kth time-varying covariate on an individual’s depressive symptoms. εij is a random error. The intercept (π0i) in our analysis reflects CES-D score for individual i at the beginning of the observation. π1i is the linear rate of change in CES-D for individual i over time. Both linear and quadratic models of changes in CES-D over time were tested (we present Equation 1 as a linear function of time for ease of presentation).
To examine ethnic differences in the changes of depressive symptoms, the parameters of the growth curve for CES-D (i.e., the intercept (π0i) and slope (π1i)) were specified as a function of race/ethnicity and other covariates in the level 2 (or person-level) equation:
| (2) |
Here p equals 0, 1, 2, … for the intercept, linear slope, quadratic slope, etc. Xqi (where q = 1, …, Q) is the qth time constant covariate (e.g., age in 1995 and gender) associated with individual i, and αpq represents the effect of Xq on the pth growth parameter (πp). ζpi is a random effect with mean of zero. No random effects were modeled for βk.
A major challenge confronted by an analyst of longitudinal data derived from HRS is whether to weight the data or not. The HRS involves a national sample of households, augmented by oversamples of African Americans, Hispanics, and Floridians. We chose not to weight the data for several reasons. First, although there is a consensus for weighting data in generating descriptive statistics for a given target population, there is no such agreement in multivariate analyses (Gelman, 2006; Groves, 1989: 279–290). Second, many of the attributes (e.g., race, ethnicity, marital status) upon which unequal selection probabilities in HRS were based were explicitly controlled in our multivariate analyses. When sampling weights are solely a function of independent variables included in the model, unweighted estimates are preferred because they are unbiased, consistent, and have smaller standard errors than weighted estimates (Winship & Radbill, 1994). Third, we undertook multivariate analyses by using unweighted as well as weighted data (by applying weights at the time of survey for the level-1 units and weights in 1998 for the level-2 units) and obtained very similar results. Therefore, only unweighted results are reported here.
Because of our massive sample size (17,196 respondents with over 64,674 observations), there is a concern about the over-abundance of significant results. To offset this, only estimates with a p value less than 0.01 were considered statistically significant.
Mortality, Attrition and Proxy Interview
To minimize the loss of data due to item missing, multiple imputation was undertaken. Three complete data sets were imputed with the NORM software developed by Schafer (1997), and analyses were run on each of these three data sets. Parameter estimates and their standard errors were derived by averaging across three imputations and by adjusting for their variance.
To address the potential non-ignorable missing data problem associated with attrition and mortality, we used a pattern-mixture model approach (Hedeker & Gibbons, 2006). Specifically, individuals were divided into groups depending on their missing data pattern (i.e., those who died during the period of observation, those who dropped out of the study during the period of observation, and those with complete responses throughout the period of observation). Indicators of these groups were then included in the level-2 equation as covariates to assess the effect of the missing data pattern on our outcome measure. Such analysis indicated that missing data pattern, especially mortality during the observation period, was significantly associated with depressive symptoms trajectory. Therefore, growth curve parameter estimates would likely be biased if missing data patterns were not adequately accounted for. To address this issue, we ran separate analyses for individuals with different missing data patterns, and obtained overall coefficient estimates by averaging over the missing data patterns weighted by the sample proportion of each missing data pattern (Hedeker & Gibbons, 1997; 2006). Estimates thus derived reflect the overall population estimates. Results reported in this manuscript reflect these average estimates.
Proxy interviews were conducted in HRS when a respondent was unable to be interviewed. Whereas some health measures were obtained from the proxy informants, CES-D items were not available. We analyzed data by excluding as well as including proxy interviews by applying the multiple imputation approach to impute the missing values on CES-D. The results were remarkably similar. Given that imputation of subjective measures might not be justified and that there might be concerns regarding the validity of proxy responses on health measures, we chose to report only the results without proxy interviews.
RESULTS
Both linear and quadratic models of changes in CES-D over time were tested. In our exploratory analysis, although the estimated quadratic slope was statistically significant, the magnitude was quite small (b = 0.007). The Bayesian Information Criterion (BIC) suggested that a linear model provided slightly better fit to the data compared to the quadratic model (149,210.89 versus 149,218.08). The residual plot also indicated that a linear model was adequate. Therefore, we chose the more parsimonious linear model in our final analysis.
Ethnic Differences in Depressive Symptoms
On average, depressive symptoms increased moderately with time among the older Americans in our sample (intercept b = 1.9783, p<.001; linear slope b = .0253, p<.001; Model 2 in Table 2). Both blacks and Hispanics had more symptoms than whites at the beginning of the observation (b = .6178 and 1.1534, respectively, p<.001, Model 2 in Table 2). Parallel analysis was conducted using blacks as the reference group. Depressive symptoms at baseline were higher among Hispanics than blacks (b = .5356, p<.001, data not shown), lending support to H1a.
Table 2.
Sequential Models for the Trajectory of Depressive Symptoms
| Covariates | Model 1 | Model 2 | Model 3 |
|---|---|---|---|
| Time Varying Covariates | |||
| Marriedt-1 | −0.1281 *** | ||
| Δ Marital statust-1,t | −0.6299 *** | ||
| Household incomet-1 | −0.0002 | ||
| Δ Household incomet-1,t | −0.0003 * | ||
| Self-rated healtht-1 | 0.4895 *** | ||
| Δ Self-rated healtht-1,t | 0.3976 *** | ||
| Diseasest-1 | 0.0463 *** | ||
| Δ Diseasest-1,t | 0.0796 *** | ||
| Functional statust-1 | 0.2254 *** | ||
| Δ Functional statust-1,t | 0.2147 *** | ||
| For Intercept, π0 | |||
| Intercept | 1.9761 *** | 1.9783 *** | 2.1219 *** |
| Non-Hispanic black | 0.6178 *** | −0.0226 | |
| Hispanic | 1.1534 *** | 0.3070 *** | |
| Age (in 1995) | −0.0023 | −0.0093 *** | |
| Female | 0.5545 *** | 0.2812 *** | |
| Education | −0.0169 ** | ||
| Baseline CESD | 0.4283 *** | ||
| For Linear Time slope, π1 | |||
| Intercept | 0.0211 *** | 0.0253 *** | −0.0199 *** |
| Non-Hispanic black | −0.0276 ** | −0.0185 | |
| Hispanic | −0.0728 *** | −0.0641 *** | |
| Age (in 1995) | 0.0021 *** | 0.0008 * | |
| Female | −0.0033 | −0.0075 | |
| Education | −0.0013 | ||
| Baseline CESD | −0.0113 *** | ||
| Random Effect | Variance | Variance | Variance |
| Intercept | 1.5365 *** | 1.4269 *** | 0.6282 *** |
| Linear time slope | 0.0098 *** | 0.0093 *** | 0.0072 *** |
| Level-1, R | 0.9692 | 0.9695 | 0.9391 |
| AIC Fit Index | 149,140.29 | 148,616.57 | 141,466.72 |
| BIC | 149,210.89 | 148,687.17 | 141,537.31 |
AIC = Akaike's information criterion. BIC = Bayesian information criterion.
p<.05,
p<.01,
p<.001.
Consistent with H1b, on average blacks and Hispanics had a smaller rate of increase in CES-D than whites (b = −.0276, p<.01 and b = −.0728, p<.001, respectively, Model 2 in Table 2). Moreover, as hypothesized in H1c, Hispanics had an even more gradual rate of increase in depressive symptoms than blacks over time (b = −.0452, p < .01, data not shown).
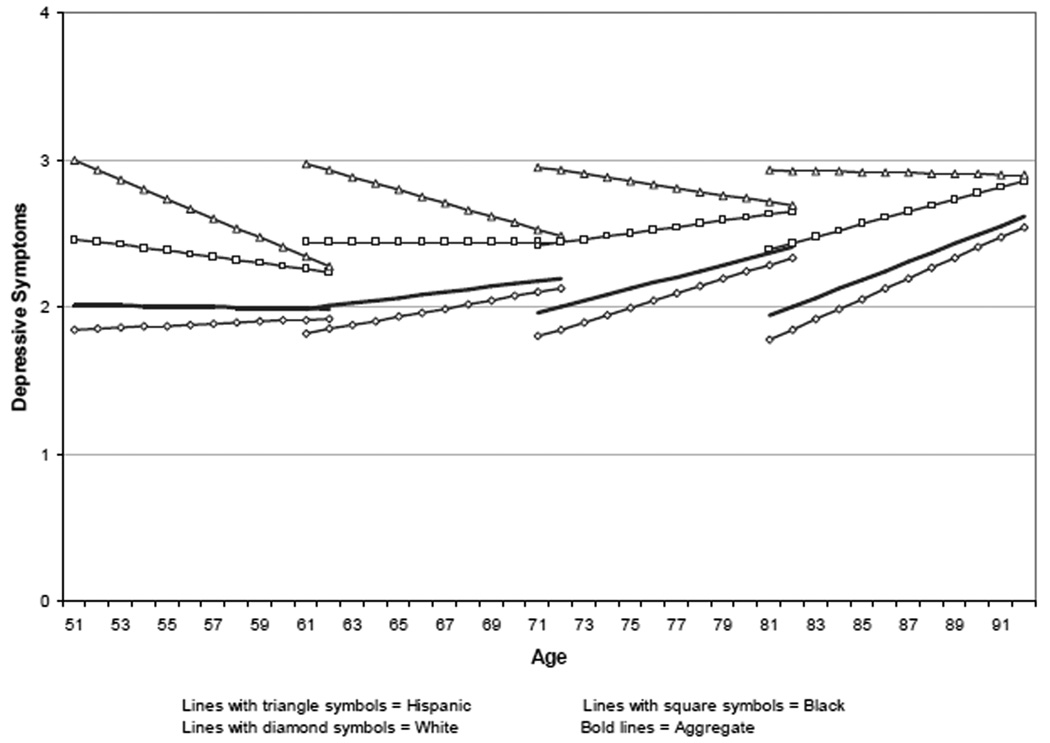
Such ethnic differences in the dynamics of depressive symptom change among middle aged and older Americans are depicted in Figure 1a. To illustrate the trajectory of depressive symptom changes over the 11 years of observation for individuals starting at different ages, we charted the trajectories by age groups. Based on our analysis, ethnic differences in the trajectory of depressive symptoms diminished over time. Relative to white and black Americans, Hispanics had the highest level of depressive symptoms, while blacks had a higher level of depressive symptoms than whites. In general, white Americans had the most rapid rate of increase in depressive symptoms over time, while Hispanics and blacks had significantly lower rate of increase or even reduction in the number of symptoms.
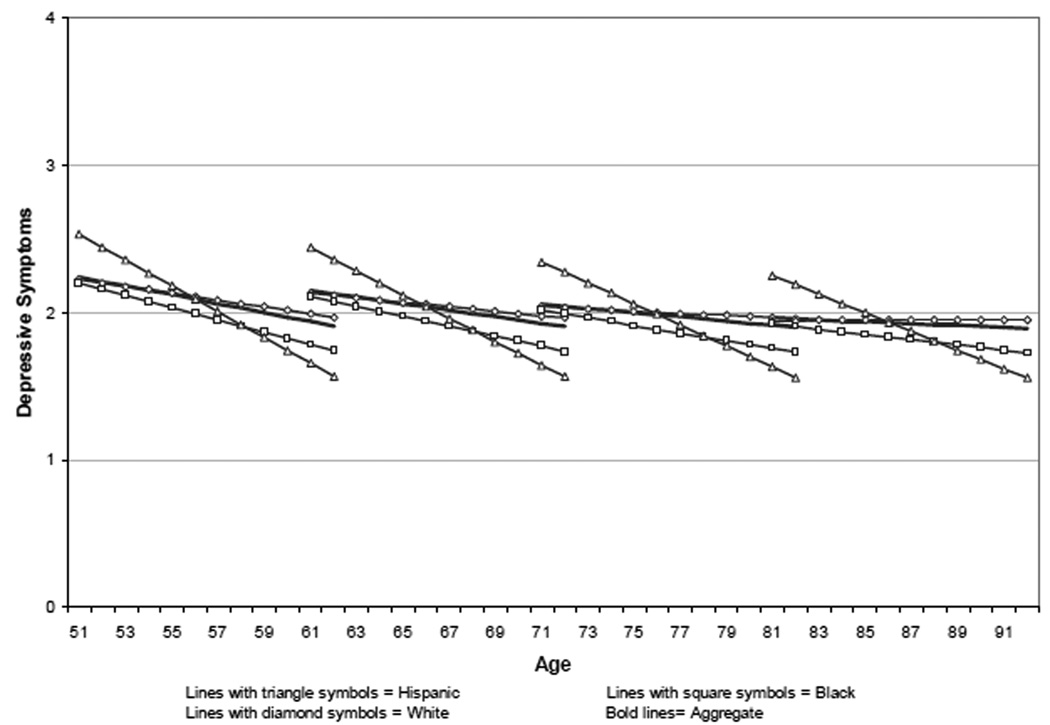
Figure 1. Ethnic Differences in the Trajectory of Depressive Symptoms.
a. Gross ethnic differences (based on Model 2 in Table 2)
b. Net ethnic differences (based on Model 3 in Table 2)
Depressive Symptoms and Population Heterogeneity
After adjusting for SES, marital status, and prior health, depressive symptoms in general decreased moderately over time. Blacks no longer differ from whites in the intercept of the trajectory (b = −.0226, p = .6767, Model 3 in Table 2). Hispanic/white differences in the intercept of depressive symptoms were also reduced substantially; however, Hispanic Americans still showed significantly higher symptomatology than white Americans (b = .3070, p<.001, Model 3 in Table 2). The difference in the level of depressive symptoms between Hispanics and blacks also was reduced considerably, but it remained significant (b = .3296, p<.001, data not shown). These results only provide partial support for H2a, but do suggest that the greater depressive symptoms observed in blacks and Hispanics were largely due to their disadvantageous SES and health.
Ethnic variations in the rate of change in depressive symptoms persisted even when population heterogeneity was controlled. The Hispanic/white difference in linear slope stayed around -.07 (b = −.0641, p<.001, Model 3 in Table 2). However, black/white difference in linear slope did not reach statistical significance (b = −.0185, p = .0644, Model 3 in Table 2). These provide partial support for the hypothesis that net of SES and health effects, blacks and Hispanics had greater rates of reduction in depressive symptoms than whites (H2b). However, contrary to H2c, Hispanic Americans were found to have a more rapid rate of reduction in depressive symptoms than black Americans (b = −.0456, p < .01, data not shown).
After adjusting for heterogeneity in socioeconomic and health status, all ethnic groups in our sample experienced improvement in their symptomatology over time (Figure 1b). Hispanics started with a higher CES-D score, but improved steadily over the 11-year period, ending up at a lower level than whites with the same baseline age. Compared to white Americans, African Americans had a similar number of depressive symptoms at the beginning of the observation and a comparable rate of change over time.
Other Covariates
Net of SES and health effects, baseline age, gender and education were only correlated with the intercept of depressive symptoms (Model 3 in Table 2). Persons who were married at the previous interview or newly married since their last interview had significantly fewer symptoms (Model 3 in Table 2).
Depressive symptoms were significantly correlated with prior health and health changes. Poor self-rated health, more chronic diseases, functional disability, and recent deterioration in these health measures were all associated with elevated symptomatology (Model 3 in Table 2). Individuals with a higher CES-D score at baseline also experienced more symptoms during the follow-up period, but a greater reduction in symptoms over time.
DISCUSSION
A key contribution of the current study lies in its characterization of the trajectory of depressive symptoms for middle aged and older Hispanic Americans. Relative to white and black Americans, Hispanics started with the highest level of symptoms, but experienced more advantageous changes over time. To the best of our knowledge, this is the first study comparing the trajectory of depressive symptoms across Hispanic, black, and white Americans simultaneously. In this regard, our study extends previous research by demonstrating Hispanic/white and Hispanic/black differences in the trajectories of depressive symptoms.
In addition, compared to white Americans, blacks had a higher level of mental distress but experienced a significantly lower rate of increase over time. These findings are consistent with the results from prior studies, where non-whites or blacks were found to have more depressive symptoms (Mirowsky & Kim, 2007; Kim & Durden, 2007) and more moderate rate of changes than white Americans (George & Lynch, 2003; Klein et al., 2008). Furthermore, our finding of diminishing differences in depressive symptoms between blacks and whites, and between Hispanics and whites, provides empirical evidence supporting the age-as-leveler hypothesis.
Why do minorities, particularly Hispanic Americans, have an advantage in the rate of change in depressive symptoms in old age? One possible explanation is that as argued by the age-as-leveler hypothesis, minority persons adopt coping strategies throughout the life course to deal with racial discrimination, and these may help Hispanic and black Americans in dealing with age discrimination (Ferraro & Farmer 1996a). In addition, according to the notion of the Hispanic paradox, Hispanics have similar or better health outcomes than whites, despite their socioeconomic disadvantages (Markides & Black, 1996). This phenomenon may be extended to the dynamic changes in depressive symptoms in old age such that Hispanic Americans experience more moderate rate of increase in symptoms, or even improved symptoms, over time than white and black Americans. Clearly, more research is needed to identify the exact reasons why Hispanics may have an advantage in the rate of change in depressive symptoms as they age.
Depressive symptoms are common among the elderly. Fourteen percent of Americans age 65 and older have clinically relevant depressive symptoms (Federal Interagency Forum on Aging-Related Statistics, 2008). Studies have shown that a high number of depressive symptoms are associated with poor health, impaired functioning, and increased health care cost (Pratt & Brody, 2008) Depressive symptoms also could complicate the course and treatment of other illnesses. Because older adults tend to have multiple illnesses, understanding the various risk-reducing and mediating factors for depressive symptoms among older adults remain an important public health issue (Chapman & Perry, 2008).
According to our analysis, ethnic differences in the trajectory of depressive symptoms are substantially confounded by socioeconomic and health differentials. Adjustment of socioeconomic positions and health conditions reversed the direction of the CES-D growth rate for the overall sample (i.e., changed from a generally increasing trajectory to a decreasing trajectory). Moreover, greater depressive symptoms among Hispanic Americans than white Americans were largely explained by their socioeconomic and health differentials. Racial differences in socioeconomic and health status also fully accounted for the observed black/white differences in depressive symptoms trajectories. Thus, improving SES and health among middle aged and older Americans may lead to a significant reduction in their burden of psychological distress. Nevertheless, our analysis also suggests that SES and health status are less influential in determining the changes in affective functioning of Hispanics relative to whites and blacks, calling for tailored interventions for different ethnic groups in order to improve their psychological well-being. Additional research aimed to identify what factors disproportionately affect Hispanics more than other ethnic groups would prove beneficial in this regard.
Although there are important commonalities in each ethnic group, there is also variation within the subgroup (Williams et al., 2007). For example, there is greater affective distress in Puerto Ricans than Mexican-Americans (Angel & Guarnaccia, 1989; Falcón & Tucker, 2000; Yang, Cazorla-Lancaster, & Jones, 2008) and greater levels of depressive symptoms in Caribbean blacks than U.S.-born African Americans (Cohen, Berment, & Magai, 1997; Lincoln, Chatters, Taylor, & Jackson, 2007). Further studies on diversity within ethnic groups and the role of acculturation would contribute additional knowledge (Williams et al., 2007). Moreover, much is to be learned about the trajectory of psychological well-being among other ethnic groups in the U.S., such as American Indians and Asians, and how black, Hispanic and White Americans differ from these other sub-populations.
In addition, reciprocal linkages could exist between depressive symptoms and health conditions (e.g., ADL/IADL, diseases, and self-rated health). On the one hand, declined health can operate as stressors exerting negative effects on depressive symptomatology; while on the other, elevated depressive symptoms may compromise health through various biological, motivational, and behavioral factors (Cohen & Rodriquez, 1995; Lenze et al., 2001). Future studies of the reciprocal linkages between the trajectory of depressive symptoms and other health measures and potential ethnic differences in such relationships will provide additional insights.
Finally, because respondents of HRS were sampled in mid- and late-life, differential mortality had already altered the representativeness of the original birth cohorts before they were eligible for inclusion. This left truncation may lead to selection bias. If survival is more selective among blacks and Hispanics than whites, more whites with poor physical and affective health might have been included in the HRS panel. This could lead to underestimated ethnic differences in depressive symptoms.
In sum, our research makes an important first step toward characterizing the trajectory of depressive symptoms for middle and old age Hispanics. We identified significant variations in not only the intercept but also the rate of change in depressive symptoms across black, Hispanic and white Americans. The various mediating factors identified in the study, such as education, marital status, and health status, provide opportunities for intervention to reduce ethnic disparities in the affective health of middle aged and older Americans. Further research incorporating additional or more elaborated ethnic groups, and addressing the potential reciprocal linkages between physical and mental health would advance our understanding of ethnic differences in affective functioning.
Acknowledgments
This research was supported by the National Institutes of Health via a pilot grant (Xiao Xu, PI) from the University of Michigan Claude D. Pepper Older Americans Independence Center (5P30AG024824) and the Michigan Institute of Clinical and Health Research (UL1RR024986), and grants R01-AG015124 and R01-AG028116 (Jersey Liang, PI). The Japanese Ministry of Health, Labor and Welfare Longevity Foundation and the Tokyo Metropolitan Institute of Gerontology provided additional support.
References
- Angel R, Guarnaccia PJ. Mind, body, and culture: Somatization among Hispanics. Social Science & Medicine. 1989;18(12):1229–1238. doi: 10.1016/0277-9536(89)90341-9. [DOI] [PubMed] [Google Scholar]
- Angel RJ, Angel JL. Diversity and Aging in the United States. In: Binstock RH, George LK, Cutler S, Hendricks J, Schulz J, editors. Handbook of Aging and the Social Sciences. Burlington, MA: Academic Press; 2006. pp. 94–110. [Google Scholar]
- Bromberger JT, Harlow S, Avis N, Kravitz HM, Cordal A. Racial/ethnic differences in the prevalence of depressive symptoms among middle-aged women: The Study of Women's Health Across the Nation (SWAN) American Journal of Public Health. 2004;94(8):1378–1385. doi: 10.2105/ajph.94.8.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Health disparities experienced by black or African Americans--United States. MMWR. Morbidity and Mortality Weekly Report. 2005;54(1):1–3. [PubMed] [Google Scholar]
- Chapman DP, Perry GS. Depression as a major component of public health for older adults. [Accessed December 10, 2008];Preventing Chronic Disease. 2008 5(1) Available at: http://www.cdc.gov/pcd/issues/2008/jan/07_0150.htm. [PMC free article] [PubMed]
- Cohen CI, Berment F, Magai C. A comparison of US-born African-American and African-Caribbean psychiatric outpatients. Journal of the National medical Association. 1997;89(2):117–123. [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Rodriquez MS. Pathways linking affective disturbances and physical disorders. Health Psychology. 1995;14(5):374–380. doi: 10.1037//0278-6133.14.5.374. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Hayward MD, Seeman T. Race/ethnicity, socioeconomic status, and health. In: Anderson N, Bulatau R, Cohen B, editors. Critical Perspectives on Race and Ethnic Differences in Health and Later Life. Washington, DC: National Academies Press; 2004. [Google Scholar]
- Crimmins EM, Seeman T. Integrating biology into demographic research on health and aging (with a focus on the MacArthur Study of successful aging) In: Finch C, Vaupel J, Kinsella K, editors. Cells and surveys: Should biological measures be included in social science research? Washington, DC: National Academies Press; 2001. pp. 9–41. [PubMed] [Google Scholar]
- Dannefer D. Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. Journal of Gerontology: Social Sciences. 2003;58B(6):S327–S337. doi: 10.1093/geronb/58.6.s327. [DOI] [PubMed] [Google Scholar]
- Davidson H, Feldman PH, Crawford S. Measuring depressive symptoms in the frail elderly. Journal of Gerontology: Psychological Sciences. 1994;49(4):P159–P164. doi: 10.1093/geronj/49.4.p159. [DOI] [PubMed] [Google Scholar]
- Dowd JJ, Bengtson VL. Aging in minority populations: An examination of the double jeopardy hypothesis. Journal of Gerontology. 1978;33(3):427–436. doi: 10.1093/geronj/33.3.427. [DOI] [PubMed] [Google Scholar]
- Everson SA, Siobhan SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. Journal of Psychosomatic Research. 2002;53(4):891–895. doi: 10.1016/s0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- Falcón LM, Tucker KL. Prevalence and correlates of depressive symptoms among Hispanic elders in Massachusetts. Journal of Gerontology: Social Sciences. 2000;55B(1):S108–S116. doi: 10.1093/geronb/55.2.s108. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2008: Key Indicators of Well-Being. [Accessed November 12, 2009];Washington, DC: U.S. Government Printing Office; Federal Interagency Forum on Aging-Related Statistics. 2008 March; Available at: http://www.agingstats.gov/agingstatsdotnet/Main_Site/Data/Data_2008.aspx.
- Ferraro KF, Farmer MM. Double jeopardy, aging as leveler, or persistent health inequality? A longitudinal analysis of white and black Americans. Journal of Gerontology: Social Sciences. 1996a;51B:S319–S328. doi: 10.1093/geronb/51b.6.s319. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Farmer MM. Double jeopardy to health hypothesis for African Americans: Analysis and critique. Journal of Health and Social Behavior. 1996b;37(1):27–43. [PubMed] [Google Scholar]
- Gelman A. Struggle with survey weighting and regression modeling. 2006 Available at: www.stat.columbia.edu/~gelman/ Retrieved 3/29/2007.
- George LK, Lynch SM. Race differences in depressive symptoms: a dynamic perspective on stress exposure and vulnerability. Journal of Health and Social Behavior. 2003;44(3):353–369. [PubMed] [Google Scholar]
- Groves RM. Survey errors and survey costs. New York: Wiley; 1989. [Google Scholar]
- Hedeker D, Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2(1):64–78. [Google Scholar]
- Hedeker D, Gibbons RD. Missing data in longitudinal studies. In: Hedeker D, Gibbons RD, editors. Longitudinal Data Analysis. Hoboken, New Jersey: John Wiley & Sons, Inc; 2006. pp. 279–312. [Google Scholar]
- House JS, Lantz PM, Herd P. Continuity and change in the social stratification of aging and health over the life course: evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans' Changing Lives Study) Journal of Gerontology: Psychological Sciences. 2005;60(2):P15–P26. doi: 10.1093/geronb/60.special_issue_2.s15. [DOI] [PubMed] [Google Scholar]
- Jackson JS, Antonucci TC, Gibson RC. Cultural, racial, and ethnic minority influences on aging. In: Birren JE, Schaie KW, editors. Handbook of the Psychology of Aging. 3rd edition. New York: Academic Press; 1990. pp. 103–123. [Google Scholar]
- Jang Y, Borenstein-Graves A, Haley WE, Small BJ, Mortimer JA. Determinants of a sense of mastery in African American and White older adults. Journal of Gerontology: Social Sciences. 2003;58(4):S221–S224. doi: 10.1093/geronb/58.4.s221. [DOI] [PubMed] [Google Scholar]
- Kelley-Moore JA, Ferraro KF. The black/white disability gap: Persistent inequality in later life? Journal of Gerontology: Social Sciences. 2004;59B(1):S34–S43. doi: 10.1093/geronb/59.1.s34. [DOI] [PubMed] [Google Scholar]
- Kim J, Durden E. Socioeconomic status and age trajectories of health. Social Science & Medicine. 2007;65(12):2489–2502. doi: 10.1016/j.socscimed.2007.07.022. [DOI] [PubMed] [Google Scholar]
- Klein DN, Shankman SA, Rose S. Dysthymic disorder and double depression: prediction of 10-year course trajectories and outcomes. Journal of Psychiatric Research. 2008;42(5):408–415. doi: 10.1016/j.jpsychires.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9(2):113–135. [PubMed] [Google Scholar]
- Liang J, Van Tran T, Krause N, Markides KS. Generational differences in the structure of the CES-D scale in Mexican Americans. Journal of Gerontology: Social Sciences. 1989;44(3):S110–S120. doi: 10.1093/geronj/44.3.s110. [DOI] [PubMed] [Google Scholar]
- Lincoln KD, Chatters LM, Taylor RJ, Jackson JS. Profiles of depressive symptoms among African Americans and Caribbean blacks. Social Science & Medicine. 2007;65(2):200–213. doi: 10.1016/j.socscimed.2007.02.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch SM, George LK. Interlocking trajectories of loss-related events and depressive symptoms among elders. Journal of Gerontology: Social Sciences. 2002;57(2):S117–S125. doi: 10.1093/geronb/57.2.s117. [DOI] [PubMed] [Google Scholar]
- Markides KS, Black SA. Race, ethnicity, and aging: The impact of inequality. In: Binstock RH, George LK, editors. Handbook of Aging and the Social Sciences. 4th edition. San Diego, CA: Academic Press; 1996. pp. 153–170. [Google Scholar]
- Mendes de Leon CF, Barnes LL, Bienios JL, Skarupski KA, Evans DA. Racial disparities in disability: Recent evidence from self-reported and performance-based disability measures in a population-based study of older adults. Journal of Gerontology: Social Sciences. 2005;60B(5):S263–S271. doi: 10.1093/geronb/60.5.s263. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Kim J. Graphing age trajectories: vector graphs, synthetic and virtual cohort projections, and cross-sectional profiles of depression. Sociological Methods & Research. 2007;35(4):497–541. [Google Scholar]
- Mirowsky J, Ross CE. Age and depression. Journal of Health and Social Behavior. 1992;33(3):187–205. discussion 206–212. [PubMed] [Google Scholar]
- Mroczek DK, Spiro A. Change in life satisfaction during adulthood: Findings from the Veterans Affairs Normative Aging Study. Journal of Personality and Social Psychology. 2005;88:189–202. doi: 10.1037/0022-3514.88.1.189. [DOI] [PubMed] [Google Scholar]
- Mui AC. Self-reported depressive symptoms among black and Hispanic frail elders: A sociocultural perspective. Journal of Applied Gerontology. 1993;12(2):170–187. [Google Scholar]
- Oliver MN, Muntaner C. Researching health inequities among African Americans: the imperative to understand social class. International Journal of Health Services. 2005;35(3):485–498. doi: 10.2190/PPQX-47DY-KW0X-78Y8. [DOI] [PubMed] [Google Scholar]
- Pratt LA, Brody DJ. Depression in the United States household population, 2005–2006. National Center for Health Statistics Data Brief. 2008;2008(7):1–8. Available at: http://www.cdc.gov/nchs/data/databriefs/db07.htm. [PubMed]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical Linear Models. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Robert SA, House JS. Socioeconomic Inequalities in Health: An Enduring Sociological Problem. In: Bird CE, Conrad P, M A, editors. Handbook of Medical Sociology. 5th edition. Upper Saddle River, NJ: Prentice Hall; 2000. pp. 79–97. [Google Scholar]
- Schafer JL. Analysis of Incomplete Multivariate Data. London: Chapman and Hall; 1997. [Google Scholar]
- Schulz R, Heckhausen J, O’Brien A. Control and the disablement process in the elderly. Journal of Social Behavior and Personality. 1994;9(5):139–152. [Google Scholar]
- Seligman MEP, Altenor A. Part II: Learned Helplessness. Behaviour Research and Therapy. 1980;18(5):462–473. doi: 10.1016/0005-7967(80)90011-x. [DOI] [PubMed] [Google Scholar]
- Shaw BA, Krause N. Exploring race variations in aging and personal control. Journal of Gerontology: Social Sciences. 2001;56(2):S119–S124. doi: 10.1093/geronb/56.2.s119. [DOI] [PubMed] [Google Scholar]
- Skarupski KA, Mendes de Leon CF, Bienias JL, Barnes LL, Everson-Rose SA, Wilson RS, et al. Black-white differences in depressive symptoms among older adults over time. Journal of Gerontology: Psychological Sciences. 2005;60B(3):P136–P142. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- Steffens DC, Pieper CF, Bosworth HB, MacFall JR, Provenzale JM, Payne ME, et al. Biological and social predictors of long-term geriatric depression outcome. International Psychogeriatrics. 2005;17(1):41–56. doi: 10.1017/s1041610205000979. [DOI] [PubMed] [Google Scholar]
- Swenson CJ, Baxter J, Shetterly SM, Scarbro SL, Hamman RF. Depressive symptoms in Hispanic and Non-Hispanic white rural elderly. American Journal of Epidemiology. 2000;152(11):1028–1055. doi: 10.1093/aje/152.11.1048. [DOI] [PubMed] [Google Scholar]
- Taylor MG, Lynch SM. Trajectories of impairment, social support, and depressive symptoms in later life. Journal of Gerontology: Social Sciences. 2004;59(4):S238–S246. doi: 10.1093/geronb/59.4.s238. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Wallace RB, Herzog R. A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. International Psychogeriatrics. 1999;11(2):139–148. doi: 10.1017/s1041610299005694. [DOI] [PubMed] [Google Scholar]
- Williams DR. Race and health: basic questions, emerging directions. Annals of Epidemiology. 1997;7(5):322–333. doi: 10.1016/s1047-2797(97)00051-3. [DOI] [PubMed] [Google Scholar]
- Williams D, Lawler KA. Stress and illness in low-income women: the roles of hardiness, John Henryism, and race. Women & Health. 2001;32(4):61–75. doi: 10.1300/J013v32n04_04. [DOI] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: results from the National Survey of American Life. Archives of General Psychiatry. 2007;64(3):305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Winship C, Radbill L. Sampling Weights and Regression Analysis. Sociological Methods and Research. 1994;23:230–257. [Google Scholar]
- Yang FM, Cazorla-Lancaster Y, Jones RN. Within-group differences in depression among older Hispanics living in the United States. Journal of Gerontology: Psychological Sciences. 2008;63B(1):P27–P32. doi: 10.1093/geronb/63.1.p27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y. Is old age depressing? Growth trajectories and cohort variations in late-life depression. Journal of Health and Social Behavior. 2007;48(1):16–32. doi: 10.1177/002214650704800102. [DOI] [PubMed] [Google Scholar]