It is well known that polyethylene (PE) wear is the major limiting factor in longevity of primary total hip arthroplasty (THA) [1]. Many studies report that cup loosening due to wear is the most frequent reason for revision in the long term for both cemented and uncemented THA, especially in young and active patients [2–7]. To date, this phenomenon is known to produce osteolysis secondary to particle debris on both the acetabular and femoral sides [3, 8–11]. Ultrahigh molecular weight PE was introduced by Sir John Charnley in the early 1960s. He developed the low-friction arthroplasty (LFA) consisting of cemented fixation with a bearing surface of a 22.25-mm metallic femoral head and an all-PE cup [12]. That type of PE has been used for >40 years and is still the most frequent bearing surface used in total joint replacements.
Conventional PE is sterilized by gamma irradiation in air. This process offers the benefits of molecular cross-linking but can also produce free radicals that, in the presence of air, oxidize [13]. Oxidation decreases resistance of the biomaterial, resulting in degradation and brittle PE, and thus may increase wear [14]. PE wear is multifactorial: among the different factors associated with wear are a patient’s higher activity level, a big femoral-head diameter or thin PE liners, vertical orientation of the acetabular cup, or the use of modular uncemented cups [15, 16]. When PE wear is evaluated on radiographs, penetration of the femoral head into the PE liner is examined. The different radiographic methods of evaluating PE wear include manual [17–20] and digitized methods using two- and three-dimensional techniques [15, 21–23]. All these techniques suffer from different degrees of error and are of limited value, as they have only been validated in a laboratory model but not in vivo studies [24]. Sychterz et al. assessed the time pattern of PE wear on X-rays and reported different findings; they observed that femoral-head penetration into the PE liner is due to two different phenomena: the so-called bedding-in process, which is the result of creep and settling of the liner into the cup; and true wear, which is due to the removal of particles [22, 25]. Bedding-in occurs in the first two postoperative years and true wear over time. These results have recently been confirmed by different authors [26, 27].
At our institution we have also analyzed this PE wear pattern. We performed a study assessing the long-term results of a cylindric PE liner, ACS (DePuy, Warsaw, IN, USA) using two different hemispheric uncemented cups: the Profile and Trilock cups (DePuy) [28]. We observed that 11 hips of the 40 cups implanted had broken their liner (Fig. 1), an already-described complication [29], even though all cups were well fixed at the time of revision and for a minimum follow-up of 14 years. Using a digitized scanner (EPSON), we assessed PE wear by measuring anteroposterior radiographs using the software package AUTOCAD 200 (Sausalito, CA, USA), based on Kim et al.’s bidimensional method [23]. Overall femoral-head penetration rate in hips without liner fracture with reference to the early penetration point was 0.1188 ± 0.070 mm/year. PE liner fractures were associated with higher early femoral-head penetration (P < 0.0001) and a vertical cup position (P = 0.0016). The 14-year survival without cup revision for any reason was 63.9%, 71.8% with no ACS PE liner fracture and 65.3% with no acetabular osteolysis (Fig. 2). In that study, we concluded that despite the catastrophic failure of the system resulting from PE rupture. Bone fixation of these cups in long-term results were good, even though the high rate of acetabular osteolysis necessitates close follow-up of these patients.
Fig. 1.
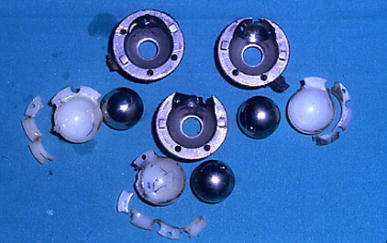
Polyethylene (PE) liner rupture and its deleterious effects
Fig. 2.

Acetabular osteolysis in a well-fixed uncemented hemispherical cup; polyethylene (PE) wear can be observed
In another study, we evaluated two different generations of a cementless cup to assess clinical and radiological results over a minimum follow-up of 10 years [30]. We compared 83 Harris-Galante I and 93 Harris-Galante II hemispherical uncemented cups (Zimmer, Warsaw, IN, USA) with a conventional PE liner sterilized by gamma irradiation in air using 32- and 28-mm femoral-head diameters, respectively. Nine Harris-Galante I cups and two Harris-Galante II cups were revised due to aseptic loosening or PE problems. When we analyzed the lineal PE wear using the above-described method, we observed that the initial PE wear at 6 months after surgery was greater for the first-generation cup, although the mean wear was similar in both cups. Mean femoral-head penetration at 6 week after surgery was 0.15 ± 0.05 mm for the Harris-Galante I cup and 0.12 ± 0.03 for the Harris-Galante II cup (P < 0.001); but mean wear was 0.13 ± 0.23 mm/year for the Harris-Galante I cup and 0.11 ± 0.10 for the Harris-Galante II cup (P = 0.740). The appearance of radiolucent lines and osteolysis was related to a greater initial wear, greater mean wear, and greater wear at the end of follow-up. Most metallic shells in both groups showed stable fixation. The so-called second-generation cups had a lower initial PE wear that resulted in less PE wear at the latest the follow-up, but the overall wear rate was similar in both groups despite the different femoral-head sizes and the improved locking mechanism. In both studies, we confirmed that the most important factor to affect the long-term result of a THA, especially in the uncemented cups, is PE wear rather than bone fixation, which usually is not a problem. We also observed the bedding-in or creep process that occurs when we sequentially analyzed penetration of the femoral head into the PE liner, described by Sychterz and others. Factors that influence PE wear, such as a vertical cup position or thin liner (like the ACS system) are also described, as well as other factors related to the design, such as a locking mechanism of the cup to the PE liner or the femoral-head size not influencing the mean wear but only the initial bedding-in process. This last observation could be examined by the probability that liner thickness and cup settling into the liner as well as PE creep that occur during the first postoperative 2 years are more important for final wear than other factors.
Since the late 1980s, new PEs have been developed to lessen the effects of wear. Different methods of sterilization have also been used to avoid the appearance of free radicals and their oxidation. These methods include gamma radiation in nitrogen, low-oxygen package, ethylene oxide, or plasma gas [31]. Clinical results of these PEs did not improve over conventional PE, and some were even worse [32–34].
New highly cross-linked polyethylenes
During the past decade, different manufacturers have begun to develop new biomaterials in order to decrease PE wear and its use in THA. Not only have new PEs been investigated as alternate bearing surfaces, but metal-on-metal and ceramic-on-ceramic interfaces are being used due to the excellent properties regarding wear [35, 36]. Some surgeons still prefer PE liners because they present some advantages, such as shock absorbers, tolerance to edge loading, forgiveness under malalignment, and relatively low price. Also, they do not at present eliminate the disadvantages of the other bearing surfaces, such as ion release, clearance, potential chromosomal aberrations, placental crossing, squeaking, or ceramic fracture [37–40]. The development of new highly cross-linked polyethylenes (HXLPE) is aimed at improving PE in both cemented and uncemented implants. In order to decrease PE wear, research has attempted to improve wear resistance while maintaining mechanical properties and eliminating the oxidation process [41]. All manufacturers produce HXLPE based on three processes: cross-linking, heat treatment, and sterilization while avoiding exposure to air. Higher cross-linking density is obtained using gamma irradiation or electron beams at a dose between 50 and 100 kGy to increase wear resistance. Heat treatment is aimed at eliminating free radicals that appear after cross-linking; this thermal treatment applies temperature above (remelting) or below (annealing) the melting transition temperature of the polymer (137°C). Both processes produce benefits and disadvantages in the PE. Whereas the remelting process stabilizes, the polymer eliminating all free radicals, on the other hand, it introduces changes in the microstructure that can affect the mechanical properties. These final changes are less important during the annealing process, but it does not completely eliminate them [41]. Clinical studies are now reported in short- and medium-term follow-ups. One of the first was from Sweden. Digas et al. [42, 43] reported better performance regarding femoral-head penetration into conventional and HXLPEs in both cemented and uncemented cups using the RSA (Umea, Sweden) method. These results have been confirmed over time in a further medium-term follow-up study. Different new HXLPEs are also confirming these results in vivo using different radiological methods of measuring femoral-head penetration [44–48] (Table 1). The results have increased the use of larger femoral heads in primary THA, although wear studies have not reported better performance for large femoral heads [49]. Thus, rim cracking has been reported, especially in thin liners and vertical cups [50].
Table 1.
Different clinical studies comparing conventional and highly cross-linked polyethylene
| Hips | Implant | Method | Follow-up (years) | Results of wear (mm/year) | |
|---|---|---|---|---|---|
| Digas et al. [43] | 56 (28/27) |
Cemented Sulene-Durasul |
RSA | 5 | 0.001–0.06 |
| Digas et al. [43] | 23 (11/12) |
Uncemented Trilogy Conventional-Longevity |
RSA | 5 | 0.005–0.06 |
| Manning et al. [44] | 181 (111/70) |
Uncemented Conventional/Longevity |
Martell | 2 | 0.174–0.007 |
| Dorr et al. [45] | 74 (37/37) |
Uncemented InterOp Conventional/Durasul |
Dorr | 5 | 0.065–0.029 |
| Engh et al. [46] | 169 (83/86) |
Uncemented Duraloc Enduron/Marathon |
Martell | 4–7 | 0.19–0.01 |
| Geerdink et al. [47] | 133 (67/66) |
Uncemented ABG II Conventional/Duration |
Martell | 3–6 | 0.12–0.08 |
| Triclot et al. [48] | 102 (53/49) |
Uncemented Fitmore Sulene/Durasul |
Martell | 4–6 | 0.10–0.02 |
| Garcia-Rey et al. [51] | 90 (45/45) |
Uncemented Allofit Sulene/Durasul |
Dorr | 5–7 | 0.038–0.006 |
We published our minimum 5-year follow-up results in a prospective randomized study comparing a nitrogen-sterilized PE (Sulene, Zimmer) and an HXLPE (Durasul, Zimmer) [51]. All hips used the same implant—the Allofit cup (Zimmer) and the Alloclassic femoral stem (Zimmer)—as well as a metallic 28-mm femoral head. Preoperative patient data were similar in both groups in terms of age, gender, weight, activity level, femur type, and diagnosis. We used the Dorr method [20] to assess femoral-head penetration into the PE liner because of the nonspherical shape of the cup and the presence of irregularities of the outer shell. We used digitized X-rays scanned and a software package (AUTOCAD 2000) to make the measurements (Fig. 3). We observed no differences in terms of clinical results or appearance of radiolucents lines or osteolysis, which was zero, between the two groups. The differences we observed were in PE wear: The mean rate of penetration calculated from regression analysis during the first 5 years was 38 μm/year [standard deviation (SD) 2] for the Sulene group and 6 μm/year (SD 1) for the Durasul group (P = 0.00002). The penetration rate for the Durasul group was 15.7% of that of the Sulene group. We concluded that there is a significant reduction in yearly linear femoral-head penetration with the Durasul PE. This study supports the better in vivo behavior of the highly cross-linked PE in primary uncemented total hip replacements (THRs) compared with nitrogen-sterilized PE using the same type of implant in all cases. However, we await the long-term results of these HXLPEs and expect that this excellent wear performance should provide a lower rate of osteolysis in primary THR.
Fig. 3.

Femoral-head penetration using digitized X-rays and the Dorr method
The so-called second-generation HXLPE is being developed. To decrease free radical oxidation and increase the mechanical properties of the polymers, different strategies are being used. The sequential annealing process maintains the mechanical properties of the PE at the same time as it theoretically reduces the production of free radicals. In vitro preliminary results report better performance by this newer HXLPE than with conventional or even first-generation HXLPE [52, 53]. The other strategy is to introduce vitamin E, the antioxidant alpha-tocopherol, into ultra-high-molecular weight PE (UHMWPE) prior to consolidation to help prevent the oxidative degradative reaction. This would avoid the deleterious effect of the melting process that decreases the mechanical properties of PE [54]. Preliminary in vitro results report good wear and improved mechanical and fatigue properties [55].
The orthopedic surgeon must keep in mind that the most important factor limiting primary THA longevity is PE wear. In most cases, with primary osteoarthritis and avascular necrosis without acetabular bone loss, bone fixation is achieved independently regardless of the choice of cemented or uncemented implant. Thus, the bearing surface would seem to be one of the critical aspects. Mid-term results of new highly cross-linked PEs seem to indicate that HXLPE is one of the materials of choice, especially in young and/or active patients with a long life expectancy and who are being considered for a THA.
Conflict of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Harris WH. Wear and periprosthetic osteolysis: the problem. Clin Orthop. 2001;393:66–70. doi: 10.1097/00003086-200112000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Hartofilakidis G, Stamos K, Ioannidis TT. Fifteen years’ experience with Charnley low-friction arthroplasty. Clin Orthop. 1989;246:48–56. [PubMed] [Google Scholar]
- 3.Garcia-Cimbrelo E, Munuera L. Early and late loosening of the acetabular cup after low-friction arthroplasty. J Bone Joint Surg. 1992;74:1119–1129. [PubMed] [Google Scholar]
- 4.Garcia-Cimbrelo E, Cruz-Pardos A, Cordero J, Sanchez-Sotelo J. Low-friction arthroplasty in patients younger than 40 years old: 20- to 25-year results. J Arthroplast. 2000;15:825–832. doi: 10.1054/arth.2000.8097. [DOI] [PubMed] [Google Scholar]
- 5.Eskelinen A, Remes V, Helenius I, Pulkkinen P, Nevalainen J, Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4, 661 primary replacements followed for 0–22 years. Acta Orthop. 2005;76:28–41. doi: 10.1080/00016470510030292. [DOI] [PubMed] [Google Scholar]
- 6.Engh CA, Jr, Culpepper WJ, 2nd, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79:177–184. doi: 10.1302/0301-620X.79B2.7640. [DOI] [PubMed] [Google Scholar]
- 7.Engh CA, Hopper RH, Jr, Engh CA., Jr Long-term porous-coated cup survivorship using spikes, screws, and press-fitting for initial fixation. J Arthroplast. 2004;19:54–60. doi: 10.1016/j.arth.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Hallan G, Lie SA, Havelin LI. High wear rates and extensive osteolysis in 3 types of uncemented total hip arthroplasty: a review of the PCA, the Harris Galante and the Profile/Tri-Lock Plus arthroplasties with a minimum of 12 years median follow-up in 96 hips. Acta Orthop. 2006;77:575–584. doi: 10.1080/17453670610012638. [DOI] [PubMed] [Google Scholar]
- 9.Orishimo KF, Claus AM, Sychterz CJ, Engh CA. Relationship between polyethylene wear and osteolysis in hips with a second-generation porous-coated cementless cup after seven years of follow-up. J Bone Joint Surg Am. 2003;85:1095–1099. doi: 10.2106/00004623-200306000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Cruz-Pardos A, García-Cimbrelo E. The Harris-Galante total hip arthroplasty. A minimum 8-year follow-up. J Arthroplast. 2001;16:586–597. doi: 10.1054/arth.2001.23921. [DOI] [PubMed] [Google Scholar]
- 11.Maloney WJ, Galante JO, Anderson M, Goldberg V, Harris WH, Jacobs J, Kraay M, Lachiewicz P, Rubash HE, Schutzer S, Woolson ST. Fixation, polyethylene wear, and pelvic osteolysis in primary total hip replacement. Clin Orthop. 1999;369:157–164. doi: 10.1097/00003086-199912000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Charnley J. Arhtroplasty of the hip. A new operation. Lancet. 1961;1:1129–1132. doi: 10.1016/S0140-6736(61)92063-3. [DOI] [PubMed] [Google Scholar]
- 13.Hopper RH, Jr, Young AM, Orishimo KF, Engh CA., Jr Effect of terminal sterilization with gas plasma or gamma radiation on wear of polyethylene liners. J Bone Joint Surg Am. 2003;85:464–468. doi: 10.2106/00004623-200303000-00010. [DOI] [PubMed] [Google Scholar]
- 14.McKellop H, Shen FW, Lu B, Campbell P, Salovey R. Effect of sterilization method and other modifications on the wear resistance of acetabular cups made of ultra-high molecular weight polyethylene. A hip-simulator study. J Bone Joint Surg Am. 2000;82:1708–1725. doi: 10.2106/00004623-200012000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Devane PA, Horne JG, Martin K, Coldham G, Krause B. Three-dimensional polyethylene wear of a press-fit titanium prosthesis. Factors influencing generation of polyethylene debris. J Arthroplast. 1997;12:256–266. doi: 10.1016/S0883-5403(97)90021-8. [DOI] [PubMed] [Google Scholar]
- 16.Young AM, Sychterz CJ, Hopper RH, Jr, Engh CA. Effect of acetabular modularity on polyethylene wear and osteolysis in total hip arthroplasty. J Bone Joint Surg Am. 2002;84:58–63. doi: 10.2106/00004623-200201000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Charnley J, Cupic Z. The nine and ten year results of the low-friction arthroplasty of the hip. Clin Orthop. 1973;95:9–25. [PubMed] [Google Scholar]
- 18.Charnley J, Halley DK. Rate of wear in total hip replacement. Clin Orthop. 1975;112:170–179. doi: 10.1097/00003086-197510000-00021. [DOI] [PubMed] [Google Scholar]
- 19.Livermore J, Ilstrup D, Morrey B. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990;72:518–528. [PubMed] [Google Scholar]
- 20.Dorr LD, Wan Z. Ten years of experience with porous acetabular components for revision surgery. Clin Orthop. 1995;319:191–200. [PubMed] [Google Scholar]
- 21.Martell JM, Berdia S. Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am. 1997;79:1635–1641. doi: 10.2106/00004623-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Sychterz CJ, Engh CA, Jr, Shah N, Engh CA., Sr Radiographic evaluation of penetration by the femoral head into the polyethylene liner over time. J Bone Joint Surg Am. 1997;79:1040–1046. doi: 10.2106/00004623-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Kim YH, Kim JS, Cho SH. A comparison of polyethylene wear in hips with cobalt-chrome or zirconia heads. A prospective, randomised study. J Bone Joint Surg Br. 2001;83:742–750. doi: 10.1302/0301-620X.83B5.10941. [DOI] [PubMed] [Google Scholar]
- 24.Wan Z, Boutary M, Dorr LD. Precision and limitation of measuring two-dimensional wear on clinical radiographs. Clin Orthop. 2006;449:267–274. doi: 10.1097/01.blo.0000218758.35181.93. [DOI] [PubMed] [Google Scholar]
- 25.Sychterz CJ, Engh CA, Jr, Yang A, Engh CA. Analysis of temporal wear pattern of porous-coated acetabular components: distinguishing between true wear and so-called bedding-in. J Bone Joint Surg Am. 1999;81:821–830. doi: 10.1302/0301-620X.81B5.9383. [DOI] [PubMed] [Google Scholar]
- 26.McCladen RW, Naudie DD, Yuan X, Bourne RB. Radiographic methods for the assessment of polyethylene wear after total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2323–2334. doi: 10.2106/JBJS.E.00223. [DOI] [PubMed] [Google Scholar]
- 27.Glyn Jones S, McLardy-Smith P, Gill HS, Murray DW. The creep and wear of highly cross-linked polyethylene: a three-year randomised, controlled trial using radiostereometric analysis. J Bone Joint Surg Br. 2008;90(5):556–561. doi: 10.1302/0301-620X.90B5.20545. [DOI] [PubMed] [Google Scholar]
- 28.Garcia-Rey E, Garcia-Cimbrelo E. Long-term results of uncemented acetabular cups with an ACS polyethylene liner. A 14–16-year follow-up study. Int Orthop. 2007;31:205–210. doi: 10.1007/s00264-006-0151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berry DJ, Barnes CL, Scott RD, Cabanela ME, Poss R. Catastrophic failure of the polyethylene liner of uncemented acetabular components. J Bone Joint Surg Br. 1994;76:575–578. [PubMed] [Google Scholar]
- 30.Garcia-Rey E, Garcia-Cimbrelo E. Clinical and radiographic results and wear performance in different generations of a cementless porous-coated acetabular cup. Int Orthop. 2008;32:181–187. doi: 10.1007/s00264-006-0305-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kurtz SM, Muratoglu OK, Evans M, Edidin AA. Advances in the processing, sterilization, and crosslinking of ultra-high molecular weight polyethylene for total joint arthroplasty. Biomaterials. 1999;20:1659–1688. doi: 10.1016/S0142-9612(99)00053-8. [DOI] [PubMed] [Google Scholar]
- 32.Chmell MJ, Poss R, Thomas WH, Sledge CB. Early failure of Hylamer acetabular inserts due to eccentric wear. J Arthroplast. 1996;11(3):351–353. doi: 10.1016/S0883-5403(96)80093-3. [DOI] [PubMed] [Google Scholar]
- 33.Sychterz CJ, Orishimo KF, Engh CA. Sterilization and polyethylene wear: clinical studies to support laboratory data. J Bone Joint Surg Am. 2004;86:1017–1022. [PubMed] [Google Scholar]
- 34.Kurtz SM, Hozack WJ, Purtill JJ, et al. Significance of in vivo degradation for polyethylene in total hip arthroplasty. Clin Orthop. 2006;453:47–57. doi: 10.1097/01.blo.0000246547.18187.0b. [DOI] [PubMed] [Google Scholar]
- 35.Delaunay CP, Bonnomet F, Clavert P, Laffargue P, Migaud H. THA using metal-on-metal articulation in active patients younger than 50 years. Clin Orthop. 2008;466:340–346. doi: 10.1007/s11999-007-0045-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bizot P, Hannouche D, Nizard R, Witvoet J, Sedel L. Hybrid alumina total hip arthroplasty using a press-fit metal-backed socket in patients younger than 55 years. A six- to 11-year evaluation. J Bone Joint Br. 2004;86:190–194. doi: 10.1302/0301-620X.86B2.14026. [DOI] [PubMed] [Google Scholar]
- 37.Clarke MT, Lee PT, Arora A, Villar RN. Levels of metal ions after small- and large-diameter metal-on-metal hip arthroplasty. J Bone Joint Surg Br. 2003;85:913–917. [PubMed] [Google Scholar]
- 38.Ziaee H, Daniel J, Datta AK, Blunt S, McMinn DJ. Transplacental transfer of cobalt and chromium in patients with metal-on-metal hip arthroplasty: a controlled study. J Bone Joint Surg Br. 2007;89:301–305. doi: 10.1302/0301-620X.89B3.18520. [DOI] [PubMed] [Google Scholar]
- 39.Case CP, Langkamer VG, Howell RT, Webb J, Standen G, Palmer M, Kemp A, Learmonth ID. Preliminary observations on possible premalignant changes in bone marrow adjacent to worn total hip arthroplasty implants. Clin Orthop. 1996;329:s269–s279. doi: 10.1097/00003086-199608001-00024. [DOI] [PubMed] [Google Scholar]
- 40.Walter WL, O’toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplast. 2007;22:496–503. doi: 10.1016/j.arth.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 41.Gomez-Barrena E, Puertolas JA, Munuera L, Könttinen YT. Update on UHMWPE research: from the bench to the bedside. Acta Orthop. 2008;79:832–840. doi: 10.1080/17453670810016939. [DOI] [PubMed] [Google Scholar]
- 42.Digas G, Kärrholm J, Thanner J, Malchau H, Herberts P. Highly cross-linked polyethylene in total hip arthroplasty: randomized evaluation of penetration rate in cemented and uncemented sockets using radiostereometric analysis. Clin Orthop. 2004;429:6–16. doi: 10.1097/01.blo.0000150314.70919.e3. [DOI] [PubMed] [Google Scholar]
- 43.Digas G, Kärrholm J, Thanner J, Herberts P. 5-year experience of highly cross-linked polyethylene in cemented and uncemented sockets: two randomized studies using radiostereometric analysis. Acta Orthop. 2007;78:746–754. doi: 10.1080/17453670710014518. [DOI] [PubMed] [Google Scholar]
- 44.Manning DW, Chiang PP, Martell JM, Galante JO, Harris WH. In vivo comparative wear study of traditional and highly cross-linked polyethylene in total hip arthroplasty. J Arthroplast. 2005;20:880–886. doi: 10.1016/j.arth.2005.03.033. [DOI] [PubMed] [Google Scholar]
- 45.Dorr LD, Wan Z, Shahrdar C, Sirianni L, Boutary M, Yun A. Clinical performance of a Durasul highly cross-linked polyethylene acetabular liner for total hip arthroplasty at five years. J Bone Joint Surg Am. 2005;87:1816–1821. doi: 10.2106/JBJS.D.01915. [DOI] [PubMed] [Google Scholar]
- 46.Engh CA, Jr, Stepniewski AS, Ginn SD, Beykirch SE, Sychterz-Terefenko CJ, Hopper RH, Engh CA. A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked marathon and non-cross-linked enduron polyethylene liners. J Arthroplast. 2006;21(Suppl 2):17–25. doi: 10.1016/j.arth.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 47.Geerdink CH, Grimm B, Ramakrishnan R, Rondhuis J, Verburg AJ, Tonino AJ. Crosslinked polyethylene compared to conventional polyethylene in total hip replacement: pre-clinical evaluation, in vitro testing and prospective clinical follow-up study. Acta Orthop. 2006;77:719–725. doi: 10.1080/17453670610012890. [DOI] [PubMed] [Google Scholar]
- 48.Triclot P, Grosjean G, El Masri F, Courpied JP, Hamadouche M. Comparison of the penetration rate of two polyethylene acetabular liners of different levels of cross-linking. A prospective randomised trial. J Bone Joint Surg Br. 2007;89:1439–1445. doi: 10.1302/0301-620X.89B11.19543. [DOI] [PubMed] [Google Scholar]
- 49.Bragdon CR, Greene ME, Freiberg AA, Harris WH, Malchau H. Radiostereometric analysis comparison of wear of highly cross-linked polyethylene against 36- vs 28-mm femoral heads. J Arthroplast. 2007;22:125–129. doi: 10.1016/j.arth.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 50.Tower SS, Currier JH, Currier BH, Lyford KA, Van Citters DW, Mayor MB. Rim cracking of the cross-linked longevity polyethylene acetabular liner after total hip arthroplasty. J Bone Joint Surg Am. 2007;89:2212–2217. doi: 10.2106/JBJS.F.00758. [DOI] [PubMed] [Google Scholar]
- 51.Garcia-Rey E, Garcia-Cimbrelo E, Cruz-Pardos A, Ortega-Chamarro J. New polyethylenes in total hip replacement: a prospective, comparative clinical study of two types of liner. J Bone Joint Surg Br. 2008;90:149–153. doi: 10.1302/0301-620X.90B2.19887. [DOI] [PubMed] [Google Scholar]
- 52.Brach del Prever EM, Bistolfi A, Bracco P, Costa L. UHMWPE for arthroplasty: past or future? J Orthop Traumatol. 2009;10:1–8. doi: 10.1007/s10195-008-0038-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dumbleton JH, D’Antonio JA, Manley MT, Capello WN, Wang A. The basis for a second-generation highly cross-linked UHMWPE. Clin Othop. 2006;453:265–271. doi: 10.1097/01.blo.0000238856.61862.7d. [DOI] [PubMed] [Google Scholar]
- 54.Oral E, Greenbaum ES, Malhi AS, Harris WH, Muratoglu OK. Characterization of irradiated blends of alpha-tocopherol and UHMWPE. Biomaterials. 2005;26:6657–6663. doi: 10.1016/j.biomaterials.2005.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Oral E, Christensen SD, Malhi AS, Wannomae KK, Muratoglu OK. Wear resistance and mechanical properties of highly cross-linked, ultrahigh-molecular weight polyethylene doped with vitamin E. J Arthroplast. 2006;21:580–591. doi: 10.1016/j.arth.2005.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]


