Abstract
Due to shortcomings of the office blood pressure (BP) in individuals with hypertension, including white coat and masked hypertension effects, terminal digit bias and large variability in BP among a small number of readings, the utilization of out-of-office blood pressure measurements has become much more common in clinical practice. The presence of the syndromes of white coat and masked hypertension creates the concern that the office BP measurements are not reflective of an individual patient's true BP values. Home (or self) and ambulatory BP assessments have been used in numerous types of clinical trials and have demonstrated their usefulness as reliable research and clinical tools. In this article, we review the recent literature on the benefits and limitations of home (self) and ambulatory monitoring of the BP in clinical practice, particularly how it relates to diagnosis of patients with various presentations of hypertension and to cardiovascular outcomes with long-term follow-ups of population cohorts.
Keywords: ambulatory blood pressure, home (self) blood pressure, out-of-office blood pressure, white-coat hypertension, masked hypertension, cardiovascular outcomes
Introduction
Traditionally, blood pressure (BP) is measured at the doctor's office and these clinical measurements are used for the diagnosis and followup of patients with hypertension. Because the office BP has been the primary type of measurement used in the major hypertension outcome trials, office (or clinic) BP has been a standard for hypertension management. In individual patients (in contrast to clinical trial populations), the office (or clinic) BP has long been recognized to have reliability and precision concerns including terminal digit bias, variability between readings and visits, and ‘environmental’ effects of the hospital or clinics that have prompted the utilization of out-of-office BP measurements [1, 2].
Terminal digit preference is the tendency to round off readings to a particular number, (in particular, zero). Digit preference/bias is influenced by bias in the observer taking the measurement, previous patient readings or preset cut-offs of cuff inflation and can lead to over- or under-estimation of the actual BP. This problem can be mitigated to some extent by an increased focus on proper measurement techniques in which care is given to terminal digits of BP using cuff deflation at slow rates (e.g, < 4 mmHg/minute).
Even when proper BP measuring technique is followed conscientiously, 2 to 3 BP measurements in the doctor's office are often associated with large variations in the BP values measured in the clinic within a single visit and among several visits. These issues have led clinicians to utilize out-of-office BP technologies with increasing frequency in practice. As will be discussed in this article, a number of prospective studies have shown the usefulness of self and ambulatory BP as reliable research and clinical tools. As a result, physicians have become more familiar with their value and recognize that out-of-office BP measurements are useful means to not only supplement the office BP but oftentimes are superior measurements to predict cardiovascular outcomes in high risk patients with hypertension [1, 3-6].
Self (or home) Blood Pressure Monitoring
Self (or home) monitoring of the BP has attributes that provides additive clinical impact to the office BP readings. Self-monitoring of the BP is relatively inexpensive, allows for multiple readings outside the clinical setting and has been shown to improve patient compliance [3]. Further, self-BP monitoring can provide information that may lead to the diagnosis of white-coat or masked hypertension and helps in assessing response to antihypertensive therapy over time [4].
Types of Blood Pressure Monitoring Devices used for home or self use
While the mercury sphygmomanometer is available from a small number of manufacturers, most patients use either an aneroid sphygmomanometer or a digital, automated oscillometric BP device for self-BP measurements. During the past decade, mercury column BP devices have been banned from many medical facilities due to environmental concerns – hence, the companies manufacturing these devices have curtailed their production dramatically. Mercury column sphygmomanometers are precise devices, but take a good deal of training for patients to become proficient in their use, hence, are not likely to be recommended [5]. Similar to the mercury devices, the aneroid manometer requires the use of a stethoscope and therefore carries many of the training and proficiency concerns noted above. Aneroid manometers are also susceptible to loss of calibration from the wear and tear of daily use and must be checked against a standard every 6 months to ensure its precision for continued use [5].
The electronic oscillometric devices are presently the most popular means for patients to perform self-BP monitoring and use small oscillations in the cuff pressure to determine the patient's BP values. Systolic and diastolic BPs are determined by proprietary algorithms unique to each manufacturer. Because the oscillometric BP devices are electronic and automated, the oscillometric devices are not associated with observer bias or terminal digit preference. They can be used with minimal training by most patients, even those with physical limitations. Unfortunately, a number of digital BP devices available to patients have not undergone rigorous independent validation according to a standard and many of the devices lack accuracy in patients with arrhythmias, obese arm sizes, and during pregnancy [6].
Device Selection / Validation
Proper selection of an independently validated BP monitoring device is critical, since appropriate diagnosis and treatment can only occur in the setting of precise readings. A complete and updated list of validated BP monitoring devices can be found at the British Hypertension Society website – www.bhsoc.org or at www.dableducational.com, a non-profit educational organization that frequently reviews new devices entering into the marketplace. To ensure accuracy and reliability of non-invasive BP monitors, it is advisable that they should be validated by one of the currently accepted protocols. Although the Association for the Advancement of Medical Instrumentation (AAMI) [7] and the British Hypertension Society (BHS) [8] have developed standards for BP monitors, many of the devices available on the market have not undergone independent testing to validate their accuracy. Of those that do undergo evaluation, few meet the standards recommended by either the BHS or the AAMI [9]. While there are several wrist devices that have been validated using the protocol of the BHS, upper arm devices are preferred over any wrist devices. The exception is when upper arm size is large enough to preclude obtaining accurate measurements (typically > 42 cm in diameter). Finger devices have neither been validated nor recommended by any consensus groups.
Technique for Self/Home Blood Pressure Monitoring
Blood pressure should be taken at the same time each day in a comfortable room and position with the patient resting for 5 minutes prior to taking a reading. Measurements should be taken in the seated position with the patient's back supported and the forearm supported at heart level [10]. Patients should be told to avoid caffeine, nicotine, food and exercise for at least 30 to 60 minutes prior to taking a reading and they should not have a full bladder.
Recommendations for the number and frequency of self-BP measurements to best assess diagnostic precision and response to therapy are varied. In the only randomized clinical trial to address this issue, the Treatment of Hypertension Based on Home or Office Blood Pressure Trial (THOP) [11], showed that at least 3 days of readings are necessary to establish an average home BP reading that relates to target organ outcomes. The SMART study [12] concluded that 6 self-BP measurements were required to reduce variability in evaluating a clinical response to drug therapy. When more than 6 self -BP measurements were recorded, the precision (reproducibility) of the average measurement was not improved [12]. Another noteworthy observation by Stergiou et al [13] was that the BP values obtained on the first day of 6 consecutive days of monitoring were significantly higher than the remaining 5 days. The authors suggested excluding the first day BP values in clinical research and practice.
Definition of Normal Self/Home Blood Pressure
There is substantial controversy over the definition of “normal” home BP readings. There are a few studies that have attempted to address this question, hence meta-analyses have been used to address the question. The THOP investigators in Belgium determined that a range of 125/79 –137/89 mmHg (with a mean of 132/85 mmHg) are normotensive [14]. The Didima study population from Greece suggested that BP values of < 137/83 mmHg are consistent with normotension [15]. However, these values are comparatively high relative to normal 24-hour BP average values of 130/80 mmHg or less. Current consensus recommendations support self-BP values of 125/75 mmHg to 130/80 mmHg as normotensive [16-18].
Indications for Home Blood Pressure Monitoring
Self or home BP monitoring has multiple clinical uses including aid in the diagnosis of hypertension, determination of the white coat effect, monitoring of treatment efficacy and improving patient compliance. White coat hypertension is a well-recognized phenomenon that is defined as having persistently elevated office BP readings of > 140/90 with 24-hour average ambulatory BP of < 130/80 mmHg [1, 19, 20]. As ambulatory BP monitoring is the gold standard for the diagnosis of white-coat hypertension, the role of self/home BP monitoring is relegated to a screening procedure that should lead to an ambulatory BP study for confirmation. White coat hypertension, long believed to be a benign condition [21-23] based on cross-sectional studies or short-term prospective cohort analyses of cardiovascular events may have a higher risk than normotensive subjects, especially when considering follow-up event rates of > 10 years. In a 10 year retrospective cohort analysis from Denmark, the cumulative cardiovascular event rate in patients with white-coat hypertension was 18%, whereas in the ‘essential’ hypertension group, the rate was 16%, both significantly higher than the normal subjects (6.8%) [24].
The usefulness of self/home BP monitoring for the diagnosis of white-coat hypertension has been extensively studied. Home monitoring of the BP has an intermediate sensitivity and high specificity for the detection of white-coat hypertension - approximately 65% and 85% respectively [25-27]. These findings confirm the recent recommendations from the American Society of Hypertension position paper by Pickering and White [10], which recommend that self/home BP should be used primarily as a screening tool in the diagnosis of white-coat hypertension.
The syndrome of masked hypertension is generally the opposite concept to white-coat hypertension – in this case the office BP is spuriously low and patients have hypertensive BP values during their activities of routine daily life [28]. The prevalence of masked hypertension in the general population is not well studied but surveys suggest that it is equal in men and women, and more common in patients being treated for hypertension [28-30]. Conservative estimates suggest that masked hypertension occurs in 10-20% of the hypertensive population.
The Self-Measurement of Blood Pressure at Home in the Elderly (SHEAF) study showed that patients with masked hypertension had cardiovascular risk profiles equal to that of uncontrolled hypertensive patients [29], and that home BP readings carry prognostic significance in terms of CV events. Home and ambulatory BP measurements identify equal number of patients with masked hypertension so both have a role in screening for the diagnosis of masked hypertension [30].
Although multiple studies have shown that self-BP measurements carry prognostic importance [11, 17, 31], there are no long-term outcome studies that show an impact on cardiovascular morbidity or mortality when treating versus not treating masked hypertension.
Conclusions for self (home) Blood pressure monitoring in practice
Home BP monitoring has been shown to be of benefit in the diagnosis of hypertension, as a screening tool for the diagnosis of white-coat hypertension and white-coat effect and as an alternative to ambulatory BP monitoring in the diagnosis of masked hypertension.
Recommendations from the American Heart Association [32] convincingly support a role for home BP monitoring in the long-term clinical management of hypertension to supplement the findings of office-based readings. Using home BP measurements to guide anti-hypertensive therapy can lead to less intensive medication therapy, or more appropriate dosing times of anti-hypertensive medications and improved control of the BP [11, 14, 32]. The guidelines for using home BP measurements in clinical practice [32] advocate using a protocol of duplicate pre-dose seated self-BP measurements in both the morning and the evening for 7 consecutive days as an appropriate means to evaluate hypertension control in the treated patient. This procedure performed every 3 months should both enhance BP control and empower patients to more fully participate in their hypertension care, a phenomenon associated with improved compliance [33].
AMBULATORY BLOOD PRESSURE MEASUREMENT
Ambulatory BP monitoring provides comprehensive information for BP and heart rate, through the use of portable non-invasive devices that were introduced in the late 1970s for possible clinical utility. The earliest devices were large (3 kg) and cumbersome and used a microphone with simultaneous electrocardiographic monitoring to identify Korotkoff sounds. Today's ambulatory BP devices are lightweight units (< 0.5 kg) that can be worn either on a belt or shoulder strap that has a rubber air hose that connects to a cuff and bladder assembly worn on the upper arm so that the patient can carry out their usual activities of daily living [1]. Nearly all of these devices utilize an oscillometric measurement method to recognize the initial and maximal arterial wave amplitudes to indirectly compute BP using set algorithms.
Like self-BP measurements, ambulatory BP monitoring eliminates observer bias and can help to identify white coat and masked hypertension. However, the large number of readings taken in the patient's daily environment (including during sleep) provides a superior assessment of the true BP and can be used for diagnosis as well as assessing response to therapy. Additionally, ambulatory BP monitoring provides information about the circadian variability of BP as well as BP behavior during various environmental conditions (work, stress, smoking cigarettes, etc).
Device validation and Technique of Ambulatory BP recordings
A number of technical studies comparing ambulatory BP monitors with intraarterial measurements and mercury column sphygmomanometers have demonstrated that the ambulatory BP devices can provide an accurate, reliable and reproducible assessment of BP in various settings [34]. However, like self BP monitors, ambulatory devices must meet the independent validation criteria proposed by national committees to ensure the reliability of the devices and techniques used for measuring the BP to verify that the systolic and diastolic BP agree within about 5 mmHg of a standard BP measurement [7-10].
When educating patients regarding use of ambulatory BP devices, excessive heavy physical activity during measurements should be discouraged, as it usually interferes with the accuracy of the measurements. It is also beneficial to maintain a diary or log of activities, wake and sleep times, time of medication administration, meals, and any occurrence of symptoms. It is critical to perform the BP study on a typical working weekday in order to obtain the most representative BP values for the individual patients.
The ambulatory monitors have the ability to be programmed for the rate and degree of inflation and deflation and the frequency of BP measurements during the study. The frequency of measurements are variable across laboratories performing ambulatory BP monitoring – we typically use a protocol that requires 80 valid readings be obtained over a 24 hour period that are later separated into awake and sleep periods. New software also allows for analysis of specific time intervals to evaluate the ‘white-coat effect’ period, early morning surge periods, and distinct periods for responses to drug therapy.
Analysis of ambulatory bp monitoring data
Ambulatory BP measurements provide important prognostic information about cardiovascular risk, mortality and progression of hypertensive end organ damage and is a better predictor of risk compared to office blood pressures [21,23,24, 35-41]. For example, in the multicenter Office vs Ambulatory Blood Pressure (OvA) study of 1963 treated hypertensive patients, Clement et al [37] showed that elevated 24 hour BPs were independent risk factors for new cardiovascular events, even after adjustment for office BP and cardiovascular risk factors. In fact, the adjusted relative risk of cardiovascular events associated with a 1-SD increment in BP was 1.34 for 24-hour ambulatory systolic BP, 1.30 for daytime systolic BP, and 1.27 for nighttime systolic BP. Corresponding relative risks of cardiovascular events were lower for diastolic BP.
In contrast to office and self-measured BP, the ambulatory BP provides extensive information on several BP parameters, including the average BP and HR, BP variability, BP load, and the nocturnal change in BP as compared to daytime values. Information from ambulatory BP recordings is provided on 3 aspects of BP behavior: The mean or average blood pressures, blood pressure variability and the circadian rhythm of BP. Clinical guidelines focus on the importance of the mean ambulatory BP for clinical practice as the other 2 types of analysis are still experimental [10, 42].
Numerous studies have shown that mean ambulatory BP averages are lower than clinic blood pressure averages and correlate better with end organ damage [43]. Consensus papers from the American Society of Hypertension [10] and American Heart Association [34] suggests that the upper limits of ‘normal’ ambulatory blood pressure in low risk populations as 130/80 for 24 hr average BP, 135/85 for awake BP and 120/75 for sleep BP [10]. These values are typically lower for high risk groups (Table 1)
Table 1.
Suggested Values for the Upper Limit of Normal Ambulatory Pressure
| Opttimal | Norrmall | Abnormal | |
|---|---|---|---|
| Daytime | < 130/80 | < 135/85 | > 140/90 |
| Niighttime | < 115/65 | < 120/70 | > 125/75 |
| 24-hour | < 125/75 | < 130/80 | > 135/85 |
Mean ambulatory BP is nearly always lower than office based BP due to effects of sleep (BP is reduced in 80% of subjects by 10% or more compared to daytime readings) and the virtual elimination of white coat effect. A small percentage of patients have higher ambulatory values than office values, consistent with masked hypertension discussed previously. Ambulatory BP monitoring has become the gold standard for the diagnosis of white coat and masked hypertension. In the short-term (< 5 years) followup studies, white coat hypertension typically carries similar cardiovascular risk to normal subjects with no antihypertensive therapies but patients with masked hypertension are at greater cardiovascular risk and without more stringent control may have accelerated target organ damage [34,41].
Blood Pressure Variability
Several clinical studies have focused on the variability of BP over time and it is shown to bear a significant relationship to end organ damage [42]. In a 7 year follow up study of 73 patients who underwent 24 hr intraarterial blood pressure monitoring, Frattola and co-workers [42] showed that those with higher BP variability had greater increase in left ventricular mass index on echocardiography, even after controlling for mean office and 24-hour mean BP.
The variability can be measured in different ways including from beat-to-beat changes; which is most accurately accomplished with intra-arterial monitoring since non-invasive intermittent BP measurements are only an estimate of variability. Typically the mean systolic and diastolic blood pressures are calculated for different time periods and are reported along with the standard deviation as an indicator for BP variability. Additionally, using data from awake and sleep times, ambulatory recordings provides an accurate assessment of day to night variability and the degree of ‘dipping’ as discussed below.
Diurnal variation: Dipping, Non-dipping and Nocturnal Hypertension
The nocturnal fall in BP relative to the awake, daytime values is referred to as ‘dipping’ due to the appearance of the curve over 24 hours. Dipping and non-dipping has been arbitrarily calculated as a proportion of > 10% or < 10% (nocturnal reduction relative to diurnal BP) and is the calculated difference between awake and sleep averages divided by the awake average BP. In most studies, the nocturnal decline in BP is between 10 and 20% in general healthy people with normotension or stage I hypertension [1,10]. The etiology of non-dipping (nocturnal decline of < 10%) is complex and may be secondary to a high level of activity during the day, poor quality of sleep, autonomic dysfunction, an activated sympathetic nervous system, and volume expansion due to heart and kidney disease [43,44]. Non-dipping patterns are also associated with decreased arterial compliance, age, obesity, and diabetes mellitus [44]. In some patients the BP may actually be higher during sleep than during awake hours – these patients are referred to as ‘reverse dippers’ or ‘risers’ and have the worst prognoses of the various sub-types of ambulatory BP patterns [10,41]. Some studies have indicated that non-dippers are at greater cardiovascular risk and the non-dipping pattern may be a marker for future cardiovascular events, hence, studies are underway to identify patients in whom more aggressive antihypertensive management might be beneficial. It is estimated that up to 30% of hypertensive patients exhibit a non-dipping profile and have higher nocturnal blood pressures; the incidence increases with age and severity of hypertension [44,45].
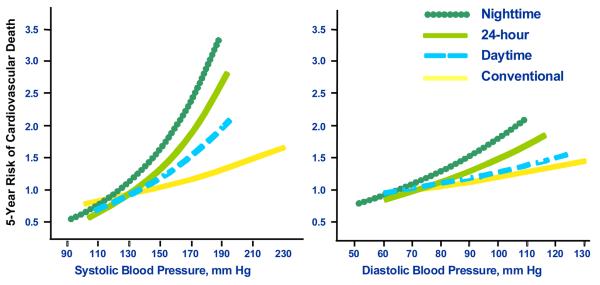
Concern exists regarding the reproducibility of 24-hour BP patterns based on proportional changes relating nighttime values to daytime values. A recent study of more than 600 patients who underwent 48 hour ABPM showed that one out of every five patients changed their profile from dippers to non-dippers or vice-versa when the first and second 24 hr periods were compared [44]. Some investigators have advocated using the absolute values of nocturnal BP rather than the proportional dip in the curve as it is more reproducible and also is strongly associated with cardiovascular outcomes [46,47]. In a prospective study of more than 5000 hypertensive patients, the authors of the Dublin Study concluded that ambulatory BP was superior to clinic BP in predicting cardiovascular mortality and nighttime systolic BP was the most potent predictor of outcome of the various components of the 24 hour period (hazard ratio of 1.21 for 10 mmHg increase in nocturnal SBP versus 1.12 for daytime SBP) [48] (Figure 1). In any event, successful management of hypertension should target both daytime and nocturnal blood pressures and information about circadian profile can aid in a more refined management plan
Figure 1.
Relations among different types of systolic blood pressure (BP) determination and 5-year risk of cardiovascular death. The nocturnal systolic BP is the most predictive BP parameter for cardiovascular mortality [48].
Morning surge of blood pressure
In most patients, there is a moderate and steady increase in BP in the morning hours with a more rapid rise in BP that coincides with awakening. This has been referred to as the ‘morning surge’ and is usually calculated by subtracting the 2 –hour pre-awakening sleep systolic BP from the 2 hour post-awakening SBP [49]. The period of the early morning BP surge is independently associated with increased risk of stroke [50] and cardiac hypertrophy [50]. The early morning increase in BP is related to various physiological changes occurring at that time including increased levels of plasma cortisol, augmented sympathetic nervous system activity and increased activity of the renin-angiotensin-aldosterone (RAAS) system. The morning surge on ABPM may be accompanied by attenuation of antihypertensive therapies. Achieving improved BP control should focus on the duration of action of antihypertensive agents and their times of administration. Whether the morning surge is a marker of increased cardiovascular risk versus whether CV risk can be reduced by targeting the treatment of the morning rise in BP remains to be studied.
Clinical Indications for use of ABPM
Ambulatory BP monitoring is useful in clinical practice along with clinic BP assessments for diagnosis and management of a variety of conditions. It is currently considered the gold standard for the diagnosis of white coat and masked hypertension and is recommended for the evaluation of patients with hypotension with antihypertensive medications, episodic hypertension and autonomic dysfunction, resistant hypertension and those on complex antihypertensive regimens. The ability to get patient initiated readings is particularly useful in symptomatic patients and those with postural hypotension. It also serves as a confirmatory tool when there is discrepancy between clinic and home BPs and to evaluate treatment efficacy in patients. The methodology continues to be invaluable in hypertension research and clinical trials for comparing the effects of different antihypertensive medications [1,10,33]. Ambulatory BP monitoring is helpful in assessing BP control throughout the 24 hour period and can assist in tailoring antihypertensive therapy for individual patients. More frequent dosing intervals, switching to nighttime dosing or a longer acting agent are typical outcomes when results of ambulatory BP monitoring are available to treating physicians [51].
Limitations of ambulatory BP monitoring exist however and includes relatively high cost (coupled with poor reimbursement by insurance companies), limited availability in most medical communities, and lack of physicians' familiarity with interpretation of ABPM data. The ambulatory devices are not as accurate in obese patients with very large arms and current devices are not validated in patients with mid-arm circumferences of greater than 46 cm. Because patient activity, arm movement and arm position can influence BP values, patient education becomes extremely important to have a successful study. Patients with irregular heart rhythms such as atrial fibrillation and patients with stiff arteries such as those on hemodialysis may be impossible to successfully monitor.
Conclusions regarding ambulatory BP monitoring
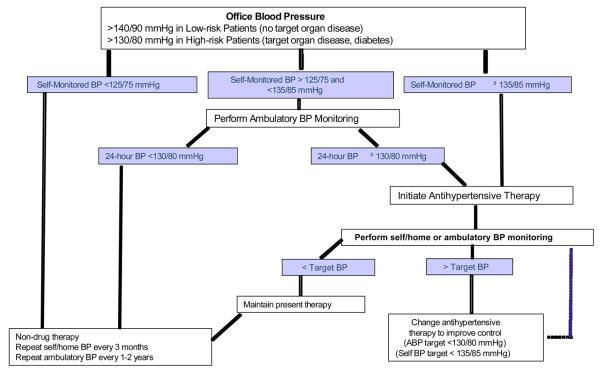
Ambulatory BP monitoring has matured into a valuable tool for the management of patients with hypertension and may lead to improved clinical outcomes especially if patient selection is appropriate and precise guidelines are followed. As physician and patient awareness increases and reimbursement improves, ambulatory BP monitoring should will become a mandatory part of the evaluation of many patients with hypertension (Figure 2).
Figure 2.
Practical use of self/home BP monitoring and ambulatory BP monitoring in clinical practice. Self-BP monitoring should be performed according to strict guidelines prior to clinical decision-making (see text for details). Following antihypertensive therapy, the determination to use self/home BP monitoring versus ambulatory BP monitoring is made according to availability, clinical judgment, and insurance coverage. [10]
References
- 1.White WB. Ambulatory blood pressure monitoring in clinical practice. N Engl J Med. 2003;348:2377–2378. doi: 10.1056/NEJMp030057. [DOI] [PubMed] [Google Scholar]
- 2.Thavarajah S, White WB, Mansoor GA. Terminal digit bias in a specialty hypertension faculty practice. J Hum Hyperten. 2003;17:819–822. doi: 10.1038/sj.jhh.1001625. [DOI] [PubMed] [Google Scholar]
- 3.Yarows SA, Staessen JA. How to use home blood pressure monitors in clinical practice. Am J Hypertens. 2002;15:93–96. doi: 10.1016/s0895-7061(01)02277-4. [DOI] [PubMed] [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560–2571. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 5.O'Brien E, Asmar R, Beilin L, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–848. doi: 10.1097/00004872-200305000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Yarows SA, Julius S, Pickering TG. Home blood pressure monitoring. Arch Intern Med. 2000;160:1251–1257. doi: 10.1001/archinte.160.9.1251. [DOI] [PubMed] [Google Scholar]
- 7.Association for the Advancement of Medical Instrumentation . American National Standard. Electronic or automated sphygmomanometers. AAMI; Arlington, VA: 1993. p. 40. (ANSI/AAMI SP 10-1992). [Google Scholar]
- 8.O'Brien E, Petrie J, Littler WA, et al. The British Hypertension Society Protocol for the evaluation of blood pressure measuring devices. J Hypertens. 1993;11:S43–S63. doi: 10.1097/00004872-199306000-00013. [DOI] [PubMed] [Google Scholar]
- 9.O'Brien E, Waeber B, Parati G, Staessen J, Myers MG. Blood pressure measuring devices: recommendations of the European Society of Hypertension. BMJ. 2001;322:531–536. doi: 10.1136/bmj.322.7285.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10••.Pickering TG, White WB, American Society of Hypertension Writing Group ASH Position Paper: Home and ambulatory blood pressure monitoring. When and how to use self (home) and ambulatory blood pressure monitoring. J Am Soc Hypertens. 2008;2:119–124. doi: 10.1016/j.jash.2008.04.002. [This position paper from the American Society of Hypertension serves as an updated guide for the indications of home and ambulatory blood pressure monitoring and provides a practical guideline for the use of these techniques in clinical decision making] [DOI] [PubMed] [Google Scholar]
- 11.Staessen JA, Den Hond E, Celis H, et al. Antihypertensive treatment based on blood pressure measurement at home or in the physician's office: a randomized controlled trial. JAMA. 2004;291:955–964. doi: 10.1001/jama.291.8.955. [DOI] [PubMed] [Google Scholar]
- 12.Chatellier G, Dutrey-Dupagne C, Vaur L, et al. Home self blood pressure measurement in general practice. The SMART study. Self-measurement for the assessment of the response to trandolapril. Am J Hypertens. 1996;9:644–652. doi: 10.1016/0895-7061(96)00018-0. [DOI] [PubMed] [Google Scholar]
- 13.Stergiou GS, Skeva II, Zourbaki AS, Mountokalakis TD. Self-monitoring of blood pressure at home: how many measurements are needed? J Hypertens. 1998;16:725–731. doi: 10.1097/00004872-199816060-00002. [DOI] [PubMed] [Google Scholar]
- 14.Celis H, Den Hond E, Staessen JA. Self-measurement of blood pressure at home in the management of hypertension. Clin Med Res. 2005;3:19–26. doi: 10.3121/cmr.3.1.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stergiou GS, Thomopoulou GC, Skeva II, Mountokalakis TD. Home blood pressure normalcy: The Didima Study. Am J Hypertens. 2000;13:678–685. doi: 10.1016/s0895-7061(99)00266-6. [DOI] [PubMed] [Google Scholar]
- 16.Ohkubo T, Asayama K, Kikuya M, Metoki H, Hoshi H, et al. How many times should blood pressure be measured at home for better prediction of stroke risk? Ten-year follow-up results from the Ohasama study. J Hypertens. 2004;22:1099–1104. doi: 10.1097/00004872-200406000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Mansoor GA, White WB. Self-measured home blood pressure in predicting ambulatory hypertension. Am J Hypertens. 2004;17:1017–1022. doi: 10.1016/j.amjhyper.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 18.Thijs L, Staessen JA, Celis H, et al. Reference values for self-recorded blood pressure: a meta-analysis of summary data. Arch Intern Med. 1998;158:481–488. doi: 10.1001/archinte.158.5.481. [DOI] [PubMed] [Google Scholar]
- 19.Den Hond E, Celis H, Vandenhoven G, O'Brien E, Staessen J. Determinants of white-coat syndrome assessed by ambulatory blood pressure or self-measured home blood pressure. Blood Press Monit. 2003;8:37–40. doi: 10.1097/00126097-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 20.Stergiou GS, Alamara CV, Skeva II, Mountokalis TD. Diagnostic value of strategy for the detection of white coat hypertension based on ambulatory and home blood pressure monitoring. J Hum Hypertens. 2004;18:85–89. doi: 10.1038/sj.jhh.1001640. [DOI] [PubMed] [Google Scholar]
- 21.Verdecchia P, Porcellati C, Schillaci G, et al. Ambulatory blood pressure. An independent predictor of prognosis in essential hypertension. Hypertension. 1994;24:793–801. doi: 10.1161/01.hyp.24.6.793. [DOI] [PubMed] [Google Scholar]
- 22.Kario K, Shimada K, Schwartz JE, et al. Silent and clincially overt stroke in older Japanese subjects with white-coat and sustained hypertension. J Am Coll Cardiol. 2001;38:238–245. doi: 10.1016/s0735-1097(01)01325-0. [DOI] [PubMed] [Google Scholar]
- 23.Khattar RS, Senior R, Lahiri A. Cardiovascular outcome in white-coat versus sustained mild hypertension. Circulation. 1998;98:1892–1897. doi: 10.1161/01.cir.98.18.1892. [DOI] [PubMed] [Google Scholar]
- 24.Gustavsen PH, Høegholm A, Bank LE, Kristensen KS. White coat hypertension is a cardiovascular risk factor: a 10-year follow-up study. J Human Hypertens. 2003;17:811–817. doi: 10.1038/sj.jhh.1001643. [DOI] [PubMed] [Google Scholar]
- 25.Parati G, Stergiou GS. Self measured and ambulatory blood pressure in assessing the ‘white-coat’ phenomenon. J Hypertens. 2003;21:677–682. doi: 10.1097/00004872-200304000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Stergiou GS, Zourbaki AS, Skeva II, Mountokalakis TD. White coat effect detected using self-monitoring of blood pressure at home: comparison with ambulatory blood pressure. Am J Hypertens. 1998;11:820–827. doi: 10.1016/s0895-7061(98)00038-7. [DOI] [PubMed] [Google Scholar]
- 27.Stergiou GS, Skeva II, Baibas NM, et al. Diagnosis of hypertension using home or ambulatory blood pressure monitoring: comparison with conventional strategy based on repeated clinic blood pressure measurements. J Hypertens. 2000;18:1745–1751. doi: 10.1097/00004872-200018120-00007. [DOI] [PubMed] [Google Scholar]
- 28.Bombelli M, Sega R, Facchetti R, et al. Prevalence and clinical significance of a greater ambulatory versus office blood pressure (‘reversed white coat’ condition) in a general population. J Hypertens. 2005;23:513–520. doi: 10.1097/01.hjh.0000160206.58781.07. [DOI] [PubMed] [Google Scholar]
- 29.Bobrie G, Genès N, Vaur L, et al. Is “isolated home” hypertension as opposed to “isolated office” hypertension a sign of greater cardiovascular risk? Arch Intern Med. 2001;161:2205–2211. doi: 10.1001/archinte.161.18.2205. [DOI] [PubMed] [Google Scholar]
- 30.Stergiou GS, Salgami EV, Tzamouranis DG, Roussais LG. Masked hypertension assessed by ambulatory blood pressure versus home blood pressure monitoring: Is it the same phenomenon? Am J Hypertension. 2005;18:772–778. doi: 10.1016/j.amjhyper.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 31.Ohkubo T, Imai Y, Tsuji I, et al. Home blood pressure measurement has a stronger predictive power for mortality than does screening blood pressure measurement: a population-based observation in Ohasama, Japan. J Hypertens. 1998;16:971–975. doi: 10.1097/00004872-199816070-00010. [DOI] [PubMed] [Google Scholar]
- 32••.Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society of Hypertension and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52:10–29. doi: 10.1161/HYPERTENSIONAHA.107.189010. [The first consensus paper on the utility of home blood pressure monitoring in clinical practice; the paper strongly advocates a protocol for assessing self-BP measurement for management of hypertension in treated individuals.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pickering TG, Hall JE, Appel LJ, et al. Recommendations for Blood Pressure Measurement in Humans and Experimental Animals: Part 1: Blood Pressure Measurement in Humans: A Statement for Professionals From the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation. 2005;111:697–716. doi: 10.1161/01.CIR.0000154900.76284.F6. [DOI] [PubMed] [Google Scholar]
- 34.Hansen TW, Jeppesen J, Rasmussen S, Ibsen H, Torp-Pedersen C. Ambulatory blood pressure and mortality: a population-based study. Hypertension. 2005;45:499–504. doi: 10.1161/01.HYP.0000160402.39597.3b. [DOI] [PubMed] [Google Scholar]
- 35.Cuspidi C, Meani S, Fusi V, et al. Isolated ambulatory hypertension and changes in target organ damage in treated hypertensive patients. J Hum Hypertens. 2005;19:471–477. doi: 10.1038/sj.jhh.1001850. [DOI] [PubMed] [Google Scholar]
- 36.Björklund K, Lind L, Zethelius B, Andrén B, Lithell H. Isolated ambulatory hypertension predicts cardiovascular morbidity in elderly men. Circulation. 2003;107:1297–30. doi: 10.1161/01.cir.0000054622.45012.12. [DOI] [PubMed] [Google Scholar]
- 37.Clement DL, De Buyzere ML, De Bacquer DA, et al. Prognostic value of ambulatory blood-pressure recordings in patients with treatedhypertension. N Engl J Med. 2003;348:2407–15. doi: 10.1056/NEJMoa022273. [DOI] [PubMed] [Google Scholar]
- 38.Ohkubo T, Imai Y, Tsuji I, et al. Prediction of mortality by ambulatory blood pressure monitoring versus screening blood pressure measurements: a pilot study in Ohasama. J Hypertens. 1997;15:357–364. doi: 10.1097/00004872-199715040-00006. [DOI] [PubMed] [Google Scholar]
- 39.Ohkubo T, Hozawa A, Nagai K, et al. Prediction of stroke by ambulatory blood pressure monitoring versus screening blood pressure measurements in a general population: the Ohasama study. J Hypertens. 2000;18:847–854. doi: 10.1097/00004872-200018070-00005. [DOI] [PubMed] [Google Scholar]
- 40.Sega R, Facchetti R, Bombelli M, et al. Prognostic value of ambulatory and home blood pressures compared with office blood pressure in the general population: follow-up results from the Pressioni Arteriose Monitorate e Loro Associazioni (PAMELA) Study. Circulation. 2005;111:1777–1783. doi: 10.1161/01.CIR.0000160923.04524.5B. [DOI] [PubMed] [Google Scholar]
- 41.Pickering TG, Shimbo D, Haas D. Ambulatory blood-pressure monitoring. N Engl J Med. 2006;354:2368–74. doi: 10.1056/NEJMra060433. [DOI] [PubMed] [Google Scholar]
- 42.Frattola A, Parati G, Cuspidi C, Albini F, Mancia G. Prognostic value of 24-hour blood pressure variability. J Hypertens. 1993;11:1133–1137. doi: 10.1097/00004872-199310000-00019. [DOI] [PubMed] [Google Scholar]
- 43.Sierra A, Redon J, Banegas J, Segura J, Parati G, et al. Spanish Society of Hypertension Ambulatory Blood Pressure Monitoring Registry Investigators Prevalence and factors associated with circadian blood pressure patterns in hypertensive patients. Hypertension. 2009;53:466–472. doi: 10.1161/HYPERTENSIONAHA.108.124008. [DOI] [PubMed] [Google Scholar]
- 44.Hernandez-del Rey R, Martin-Baranerab M, Sobrinoc J, et al. Spanish Society of Hypertension Ambulatory Blood Pressure Monitoring Registry Investigators Reproducibility of the circadian blood pressure pattern in 24-h versus 48-h recordings: the Spanish Ambulatory Blood Pressure Monitoring Registry. J Hypertens. 2007;25:2406–2412. doi: 10.1097/HJH.0b013e3282effed1. [DOI] [PubMed] [Google Scholar]
- 45.Perez-Lloret S, Toblli J, Cardinali DP, Malateste JC, Milei J. Nocturnal hypertension defined by fixed cut-off limits is a better predictor of left ventricular hypertrophy than non-dipping. Int J Cardiol. 2008;127:387–389. doi: 10.1016/j.ijcard.2007.04.027. [DOI] [PubMed] [Google Scholar]
- 46.White WB, LaRocca G. Improving the utility of the nocturnal hypertension definition by using absolute sleep blood pressure rather than the ‘dipping’ proportion. Am J Cardiol. 2003;92:1439–1441. doi: 10.1016/j.amjcard.2003.08.054. [DOI] [PubMed] [Google Scholar]
- 47.Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370:1218–1229. doi: 10.1016/S0140-6736(07)61538-4. [DOI] [PubMed] [Google Scholar]
- 48••.Dolan E, Stanton A, Thijs L, et al. Superiority of Ambulatory Over Clinic Blood Pressure Measurement in Predicting Mortality: The Dublin Outcome Study. Hypertension. 2005;46:156–161. doi: 10.1161/01.HYP.0000170138.56903.7a. [This long term prospective study in more than 5000 patients confirmed the improved outcome predictability of ABPM over clinic BP and highlighted the importance of nocturnal hypertension as the most potent predictor of cardiovascular mortality.] [DOI] [PubMed] [Google Scholar]
- 49.Kario K, Pickering TG, Umeda Y, et al. Morning surge in blood pressure as a predictor of silent and clinical cerebrovascular disease in elderly hypertensives: a prospective study. Circulation. 2003;107:1401–1406. doi: 10.1161/01.cir.0000056521.67546.aa. [DOI] [PubMed] [Google Scholar]
- 50.Kuwajima I, Mitani K, Miyao M, et al. Cardiac implication of the morning surge in blood pressure in elderly hypertensive patients: relation to arising time. Am J Hypertens. 1995;8:29–33. doi: 10.1016/0895-7061(94)00154-4. [DOI] [PubMed] [Google Scholar]
- 51.Grin JM, McCabe EJ, White WB. Management of hypertension after ambulatory blood pressure monitoring. Ann Intern Med. 1993;118:833–837. doi: 10.7326/0003-4819-118-11-199306010-00001. [DOI] [PubMed] [Google Scholar]