Abstract
The purpose of the study was to investigate the effect of upper extremity (UE) weight bearing on UE impairment functional performance of persons with acquired brain injury (BI).
A quasi-experimental design was used to examine a convenience sample of 99 persons with acquired BI and 22 without BI (WBI) living in a community re-entry centre. A computerized force-sensing array pressure map system was used to determine the UE pressure during unilateral and bilateral conditions. Differences between groups were examined using t-tests. Correlations were computed between UE weight bearing and hand function, and functional performance as measured by the Fugl-Meyer scale and functional independence measure (FIM) scale.
The group of people with BI exerted significantly lower UE weight bearing during unilateral conditions as compared with persons WBI [left: t (119) = 2.34, p = 0.021; right: t (119) = 4.79, p = 0.043). UE weight-bearing measures correlated strongly with FIM motor scores with bilateral UE conditions yielded the highest significant correlation (bilateral left r = 0.487, p < 0.001; bilateral right r = 0.469, p < 0.01).
The results indicated that UE weight-bearing pressure differs in unilateral and bilateral conditions, between persons with and WBI and between persons with stroke and traumatic brain injury. These findings may have implications for occupational therapists that use unilateral versus bilateral motor training for rehabilitation.
There is a need to replicate the study design with a randomized and stratified sample of persons with BI.
Keywords: hand impairment, hemiplegia, neuro-rehabilitation
Introduction
Brain injury (BI) can lead to a broad spectrum of symptoms and disabilities. Persons with acquired BI from stroke and traumatic head injury [traumatic brain injury (TBI)] can exhibit motor disorders in which the upper extremities often show common clinical symptoms such as spasticity, decreased muscle strength, incoordination, impaired sensation and ability to bear weight symmetrically (Rosenstein et al., 2008). It has been estimated that 3 months after a stroke, only 20% of patients have full recovery of upper extremity (UE) function and that 30–66% of persons with BI are unable to use their affected UE (Parker et al., 1986; van der Lee et al., 1999). UE weight-bearing activities are a common clinical practice for the rehabilitation of persons with BI (Kinghorn and Roberts, 1996).
The incorporation of UE weight-bearing activities is an important and common practice for normalizing muscle tone in children and adults following BI and for glenohumeral joint pathology reduction (Barnes, 1986; Chakerian and Larson, 1993; Brouwer and Ambury, 1994; Kinghorn and Roberts, 1996; Uhl et al., 2003). Repetitive UE weight bearing increases symmetry and facilitation of movement in the affected side in persons with hemiplegia. Knowledge of UE weight bearing can be useful for the rehabilitation of persons with acquired BI. However, there is limited information regarding both objective evaluation and intervention for unilateral and bilateral training. The purpose of this study was to investigate the effect of UE weight bearing with UE impairment functional performance after BI. We hypothesized that persons with BI would exhibit less UE weight-bearing average pressure than persons in the control group. Furthermore, we hypothesized that bilateral UE weight bearing would strongly correlate with functional measures when compared to unilateral trials.
Methods
Participants
A consecutive convenience sample of 99 participants had a diagnosis of BI, and 22 control participants that had no history of BI were studied. All participants in the BI sample were recruited from the centre’s rehabilitation unit, and volunteers in the control sample were recruited by e-mail from facility staff list. The inclusion criteria for the BI sample were as follows: participation in a post-acute rehabilitation centre, presence of unilateral or bilateral UE impairment, ability to comprehend and follow three-step directions and ability to give informed consent. For the control sample, the participants were excluded if they had a history of BI or head contusion. Consent from all participants and Institutional Board approval were obtained from the clinical and educational institutions. Refer to Table 1 for participant demographics.
TABLE 1.
Comparison of the participant demographics and outcome measures
| Participant demographics | ||
|---|---|---|
| Brain injury (n = 99) | Without BI (n = 22) | |
| Age | ||
| Mean ± standard deviation | 42.05 ± 15.97 | 37.05 ± 12.13 |
| Range | 18–83 years | 22–59 years |
| Years of education | ||
| Mean ± standard deviation | 13.13 ± 2.65 | 16.10 ± 2.61 |
| Caucasian | 62 (62.1%) | 13 (59.1%) |
| African American | 10 (10.1%) | 6 (27.3%) |
| Hispanic | 24 (24.2%) | 3 (13.6%) |
| Asian | 3 (3.0%) | |
| Handedness* | ||
| Right | 84 (84.8%) | 19 (86.4%) |
| Left | 10 (10.2%) | 3 (13.6%) |
| Bilateral | 3 (3.0%) | |
| Affected side* | ||
| Right | 32 (32.3%) | |
| Left | 61 (61.6%) | |
| Bilateral | 3 (3.0%) | |
| Type of injury | ||
| Traumatic brain injury | 54 (54.6%) | |
| Aneurysm | 39 (39.4%) | |
| Tumour | 3 (3.0%) | |
| Anoxia | 1 (1.0%) | |
| Other | 1 (1.0%) | |
| Onset of injury | ||
| Less than 3 months ago | 22 (22.2%) | |
| 3–6 Months ago | 25 (25.3%) | |
| 6 Months to 1 year ago | 21 (21.2%) | |
| Greater than 1 year ago | 31 (31.3%) | |
| Functional independence measure (FIM)* | ||
| Motor score | 59.67 ± 20.27 | |
| Cognitive score | 20.33 ± 6.86 | |
| Total score | 80.03 ± 22.86 | |
| Fugl-Meyer upper extremity assessment | ||
| Right | 55.51 ± 16.74 | |
| Left | 48.10 ± 21.57 | |
Missing data for three participants.
Setting
This quasi-experimental study was carried out at a community-based centre located in the southern portion of the United States. Post-acute rehabilitation services offered at the centre included medical, nursing, occupational therapy, physical therapy, speech and language services, psychology, neuropsychology, vocational services and therapeutic recreation. Services provided at the centre were matched to each individual’s needs and abilities.
Outcome measures
Three measures were used in this study: UE weight bearing as measured by the force-sensing array (FSA) pressure map system, Fugl-Meyer UE scale (FM) and functional independence measure (FIM). One was a direct measure of UE pressure exerted by the participants during one- and two-handed pressure tasks. The second instrument measured UE impairment (FM), and the third assessed the participant’s overall functional performance (FIM).
FSA pressure map system
A computerized FSA pressure map system was used to determine the average pressure applied during unilateral UE weight-bearing, and bilateral UE weight-bearing conditions. The FSA system recorded, stored and displayed in topographical form UE pressure schematics representing higher-pressure areas, as well as numeric values representing the measured pressure. The FSA system included a 256-sensor (16 × 16 inches) pressure-sensing mat and an interface to a laptop computer. For each hand, two left and two right quadrant sensors were delineated on the mat for each hand placement, and they were calibrated for a maximum pressure of 100 mm Hg. The sampling rate was 38 frames per second. The manufacturer’s reported accuracy with the interfaces was 90%, and studies have confirmed the accuracy and reliability of this FSA system (Jeffcott et al., 1999; Abreu et al., 2007). The FSA pressure mat was encased in a plastic cover designed for the study to allow for standardized hand placement with a measuring tape attached to the mat cover borders delineating four quadrants. The FSA system was used to measure the average pressure of each UE during unilateral and bilateral conditions within a week after admission.
FM UE scale
The FM is a widely used assessment of UE motor impairment for persons with spasticity and hemiplegia (Fugl-Meyer et al., 1975; Fugl-Meyer, 1980; Stein et al., 2004). Several studies have demonstrated the construct validity, and excellent inter-rater and intra-rater reliability properties of the FM scale (Bohannon and Smith, 1987; Sanford et al., 1993). The FM UE scale is a 3-point ordinal scale (2 points for each item performed completely, 1 point for each item performed partially and 0 for items not performed). The UE scale has a maximum score of 66 points when patients have no apparent motor deficits (Fugl-Meyer, 1980; Sanford et al., 1993). All FM assessments were obtained by a master clinician and member of the research team with extensive experience in BI rehabilitation, within a week after admission.
FIM
The FIM is part of the uniform data system for medical rehabilitation. The FIM is one of the most widely used methods of assessing functional status in persons with a disability [Guide for the Uniform Data Set for Medical Rehabilitation (including the FIM instrument), 1997]. The FIM includes 18 items, each with a maximum score of 7 and a minimum score of 1. Total possible FIM scores range from 18 to 126. The areas examined by the FIM include: self-care, sphincter control, transfers, locomotion, communication and social cognition. These areas are further divided into motor and cognitive domains (Granger et al., 1993, 1995). The FIM is intended to serve as a basic indicator of the severity of disability. The inter-rater reliability of fully credentialed subscriber facilities is reported as ICC = 0.96 for total FIM scores with kappa values from 0.66 to 0.83 for individual items. Several studies have been conducted to examine and support the reliability and validity of the FIM (Hamilton et al., 1994; Ottenbacher et al., 1994). The FIM instrument was administered within 3 days of admission.
Procedures
The same therapist and engineer collected all UE weight-bearing data in a standardized manner. During data collection, the therapist gave all instructions and performed all individual adjustments. Simultaneously, the engineer performed all data collection and computer management tasks. Because of the nature of the UE impairments in the sample, it was not possible to blind either the therapist or engineer during data collection. However, all data analysis was conducted by another researcher who was not involved in the collection process. For data collection, the FSA mat was placed on top of a table measuring 73.7 cm in height, 76.2 cm in width and 152.4 cm in length. Each participant was seated in a standard chair in front of a standard table. The mat was adjusted so that the elbow was flexed at an 80-degree angle. The hands were positioned in prone, 2 inches apart from the centre of each quadrant. The hand alignment was secured by placing three disposable paper markers for each participant’s hand. One marker was posted at the end of the third finger, one marker at the end of the ulna and one at the end of the radius. This allowed for hand repositioning in between trials. After repositioning the individual’s shoulder and elbow, FSA pressure measures were made. Each person was asked to press down on the mat while seated in the chair. The pressing down and relax cycle was performed for 5 s while UE weight bearing was monitored. This cycle was based on qualitative analysis of videotaped performance of five persons with BI. The pressing down cycle was recorded twice for three conditions: (1) unilaterally to the right; (2) unilaterally to the left; and (3) bilaterally. In order to minimize the potential of differences associated to the novelty of the task, only the second trial in each cycle was included in the data analysis. The order of the conditions was counterbalanced to minimize the influence of the confounder. Half of the participants started with the unilateral conditions, and the other half started with the bilateral condition first. For analysis purposes, the three conditions were divided into four average pressure values: (1) right unilateral; (2) right bilateral; (3) left unilateral; and (4) left bilateral. Figure 1 shows the lab set-up with the FSA system and an example of the graphic output.
FIGURE 1.
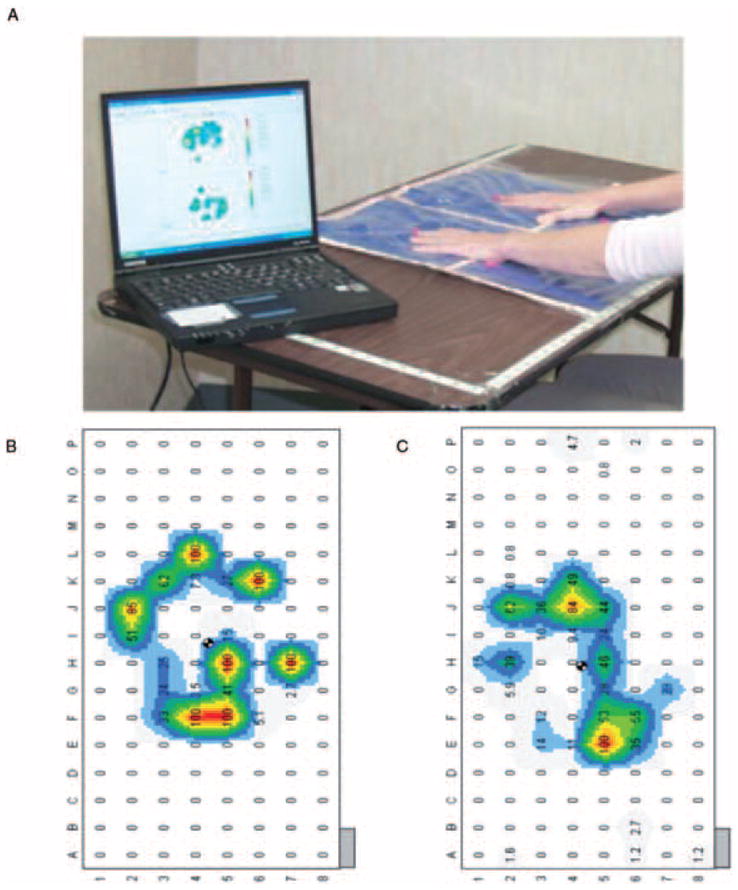
(A) Lab set-up showing bilateral upper extremity weight bearing, (B) left hand during weight bearing for a control participant, (C) left hand during weight bearing for a participant with a brain injury.
Data analysis
Data were examined descriptively for measure of central tendency and variability. Data were also analysed using independent sample t-tests to examine group differences between BI and control participants across conditions. Sub-analyses of TBI and stroke participants were performed using analysis of variance (ANOVA). Pearson’s correlations were used to examine the relationship between UE weight bearing, and FM and FIM scores among the BI participants (SPSS version 15 for Windows statistical software, Chicago, IL).
Results
Of the 99 persons with BI, 54 participants sustained TBI, 39 stroke, 3 brain tumours and 2 with anoxia. The BI sample ranged from 18 to 83 (median age = 43) years old, and the without BI (WBI) group was between 22 and 59 years old (median age = 32), indicating that that with WBI sample was younger than the BI sample. The BI group included 89 right-handed people and 10 left-handed people. Thirty-two participants showed a right hemiplegia or hemi-paresis, 61 participants showed a left hemiplegia or hemiparesis and 2 showed bilateral UE involvement. Similarly, the participants in the WBI group included 19 right-handed people and 3 left-handed people with no history of musculoskeletal injury to their UE and no history of BI.
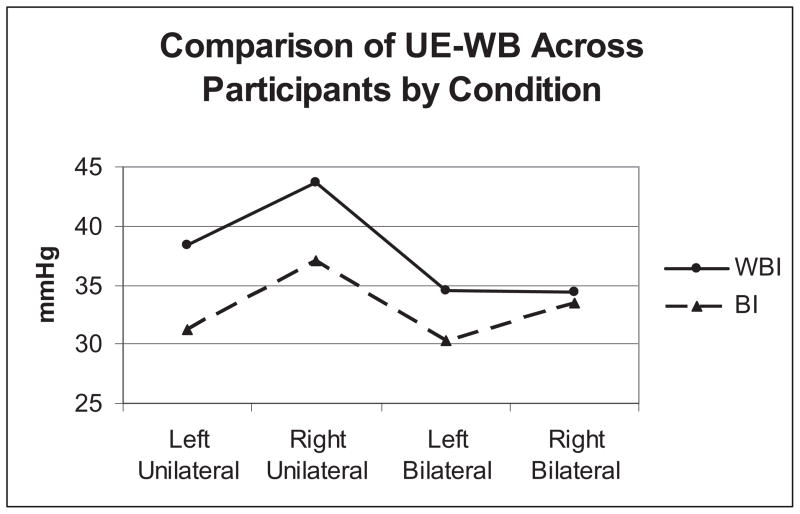
The BI sample produced lower UE weight-bearing pressure in all conditions; however, these differences only reached significance for the unilateral conditions [left: t (119) =2.34, p = 0.021; right t (119) =4.79, p = 0.043). Persons in the WBI group consistently demonstrated higher UE weight-bearing outcomes. Figure 2 shows the UE weight-bearing pressure for all conditions by sample. The difference between BI and WBI noted in the unilateral conditions decreased during the bilateral condition.
FIGURE 2.
Average upper extremity weight bearing (UE-WB) pressure between participants with brain injury (BI) and control participants.
Sub-analyses of the BI group were performed to further explore the potential differences related to: (1) hemiplegic side; (2) the type of BI (stroke and TBI); and (3) the onset of injury. The first sub-analysis examining the hemiplegic side excluded participants with bilateral involvement. We examined the difference within the unilateral and bilateral conditions for the hemiplegic side, and differences between individuals with right and left hemiplegia. The ANOVA showed no significant differences (F = 1.72, p = 0.185), which suggests that the affected side did not differ with respect to UE weight-bearing abilities in either the unilateral or bilateral conditions.
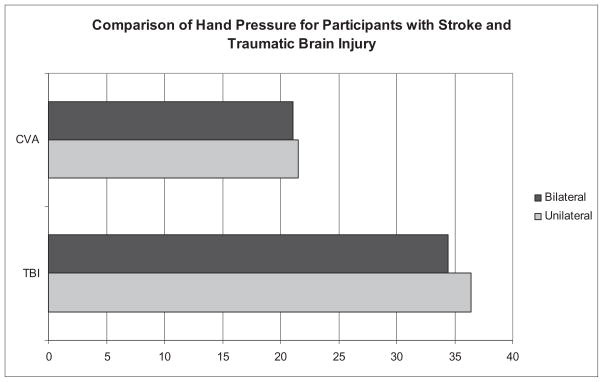
The second sub-analysis examined differences between the type of acquired BI (persons with cerebral vascular accident and persons with TBI) with respect to unilateral and bilateral conditions. The ANOVA yielded significant differences between groups for both unilateral (F = 12.71, p = 0.001) and bilateral (F = 9.76, p = 0.004) conditions. In both unilateral and bilateral UE weight bearing, the TBI sample consistently demonstrated higher amounts of UE weight bearing. Figure 3 shows a comparison of unilateral and bilateral UE weight bearing for individuals with TBI and stroke.
FIGURE 3.
Bilateral and unilateral average hand pressure for participants with stroke and traumatic brain injury.
The third sub-analysis examined the onset of injury with respect to unilateral and bilateral UE weight bearing. There was no significant difference in UE weight bearing with respect to onset of injury, indicating that the length of time since injury was not a contributing factor in the clients’ average UE weight-bearing pressure during unilateral or bilateral conditions (unilateral left F = 0.246, p = 0.864; unilateral right F = 1.641, p = 0.778; bilateral left F = 0.366, p = 0.728; bilateral right F = 1.77, p = 0. 159).
Relationships were examined between UE weight bearing, FIM motor, FIM cognitive, FIM total scores and FM right and left UE. Table 2 shows the results of the correlations. Significant relationships were noted between UE weight bearing and the FM, FIM motor and FIM total in unilateral and bilateral conditions. The UE pressure measures correlated more strongly with the FIM score than with the FM score. Within the FIM scores, the bilateral UE pressure condition consistently showed stronger relationships when compared to the unilateral conditions. These data indicate that up to 23.7% of the variability in the FIM motor scores can be explained by average UE pressure during the bilateral condition (bilateral left r = 0.487, p < 0.001; bilateral right r = 0.469, p < 0.01). In the bilateral conditions, the persons with BI appeared more able to exert UE weight-bearing pressure. In addition, their UE weight-bearing pressure scores were less variable and closer to that of the participants WBI. This finding may, in part, help to explain the increased in functional performance after weight-bearing interventions.
TABLE 2.
Relationships between average hand pressure conditions and rehabilitation outcomes
| Unilateral left | Unilateral right | Bilateral left | Bilateral right | |
|---|---|---|---|---|
| Fugl-Meyer left | 0.413** | 0.033 ns | 0.269** | 0.105 ns |
| Fugl-Meyer right | 0.001 ns | 0.325** | 0.081 ns | 0.370** |
| FIM motor | 0.465** | 0.456** | 0.487** | 0.469** |
| FIM total | 0.418** | 0.458** | 0.459** | 0.478** |
| FIM cognitive | 0.019 ns | 0.192 ns | 0.101 ns | 0.225* |
p < 0.05;
p < 0.01;
ns, p > 0.05.
Discussion
This study indicates that during unilateral and bilateral conditions, persons with BI exert lower amounts of UE pressure than individuals WBI. These findings are similar to those reported in the BI literature (Luke et al., 2004; Lang et al., 2007).
Neither the onset of BI nor the side of the hemiplegia influenced the UE pressure. However, significant differences by group diagnosis were found for both unilateral and bilateral conditions. This finding may indicate that the difference in UE pressure related to diffuse damage associated with TBI rather than the focal injury commonly found following stroke. Further research is needed to characterize these differences.
The examination of the relationship between the two outcome measures at the impairment and functional level as measured by the FM and FIM showed a significant moderate correlation between the FIM and UE pressure.
The action demands of unilateral or bilateral tasks during UE weight bearing include external and internal factors. External factors according to Serrien et al. (2007) arise from the information provided by the environment in which the movement is produced. Therefore, the unilateral or bilateral condition itself is an external factor modifying the UE weight-bearing pressure. Internal factors, on the other hand, refer to the person’s related conditions from his or her central nervous system. For example, the person’s attention affects movement and symmetrical weight bearing of the extremity (Roerdink et al., 2008). When occupational therapists use unilateral and bilateral tasks for interventions with individuals after BI, there is a complex dynamic modulation of skills that needs to be taken into consideration. It is critical to understand how attention is relevant to action, because client’s cognitive resources are recruited in a variety of manner in accordance with the characteristics of the therapeutic task. This study suggests that the use of unilateral or bilateral activities may affect motor ability and functional performance in a different manner. Some studies suggest that training of the affected UE improves bilateral performance (Cunningham et al., 2002; Luft et al., 2004). Other studies suggest that bilateral training alone or in combination with sensory feedback is effective in motor training after BI (Stewart et al., 2006). An important goal for occupational therapists would be to objectively evaluate UE weight-bearing pressure in order to better understand this process. Given the relationship between functional performance and UE weight-bearing pressure, the authors recommend the inclusion of objective UE weight-bearing pressure measures in rehabilitation to aid in understanding the value of bilateral weight bearing and its potential benefit as an intervention.
Other researchers have combined unilateral and bilateral robotic training with good results for UE neurorehabilitation in persons with BI (Lum et al., 2006). Mudie and Matyas (2000) proposed that the theoretical base for this improvement is that bilateral simultaneous movements promote interhemispheric disinhibition likely to allow reorganization by sharing of normal movement commands from the undamaged hemisphere. The authors believe that Mudie and Matyas’s neurophysiological interpretation can partially explain the results of this study.
Limitations
Limitations include lack of randomization, age difference between the control and study participants, mixed diagnosis and impairment level. In addition, the data collection methods used may have affected the results of this study. Further examination is needed to determine how these variables affect UE weight bearing. Despite these methodological limitations, this study can add to the evidence to support UE weight-bearing evaluation and interventions. The results warrant further exploration of the use of UE weight bearing in occupational therapy practice.
FSA technologies have offered innovative rehabilitation applications. Occupational therapy researchers have used FSA pressure mapping systems to provide quantitative. assessments of seated postural control and wheelchair cushion selection (Abreu, 1995; Shechtman et al., 2001; Abreu et al., 2007). As supported in this study, FSA may help in the objective evaluation of UE weight bearing; however, clinicians might also use bathroom scales as a low-cost but less reliable alternative to roughly estimate UE weight-bearing pressure.
Conclusions
The results point to the need for more research on UE weight bearing in persons with BI. The results of the study indicated that the UE weight-bearing pressure is different in unilateral and bilateral conditions, between persons with and WBI and between persons with stroke and TBI. The findings confirmed that persons with BI activated significantly lower pressure UE weight-bearing area during unilateral conditions as compared with persons WBI. UE weight-bearing measures correlated strongly with FIM motor scores. Bilateral UE weight-bearing conditions yielded the highest significant correlation. The findings may have implications for occupational therapists that use unilateral versus bilateral motor training for BI rehabilitation. Further study of UE weight-bearing pressure is warranted with more methodological rigor.
Acknowledgments
Funding from the National Institute of Health, National Institute for Child Health and Human Development and National Institute for Neurological Disorders and Stroke (K12-H0055929), and the Moody Foundation supported this research project.
Contributor Information
TIMOTHY REISTETTER, Department of Occupational Therapy, East Carolina University, Greenville, NC, and Division of Rehabilitation Sciences, University of Texas Medical Branch, Galveston, TX.
BEATRIZ C. ABREU, Division of Rehabilitation Sciences, University of Texas Medical Branch, Galveston, TX, and Transitional Learning Center, Galveston, TX
JANE BEAR-LEHMAN, Department of Occupational Therapy, New York University Steinhardt, New York, NY.
KENNETH J. OTTENBACHER, Division of Rehabilitation Sciences, University of Texas Medical Branch, Galveston, TX
References
- Abreu BC. The effect of environmental regulations on postural control after stroke. American Journal of Occupational Therapy. 1995;49:517–525. doi: 10.5014/ajot.49.6.517. [DOI] [PubMed] [Google Scholar]
- Abreu BC, Heyn P, Reistetter TA, Patterson RM, Buford WL, Jr, Masel B, Ottenbacher KJ. Postural control comparisons of able-bodied horseback riders and riders with brain injury. In: Engel BT, MacKinnon JR, editors. Enhancing Human Occupation Through Hippotherapy: A Guide for Occupational Therapy. Bethesda, MD: American Occupational Therapy Association; 2007. pp. 92–99. [Google Scholar]
- Barnes KJ. Improving prehension skills of children with cerebral palsy: a clinical study. Occupational Therapy Journal of Research. 1986;6:227–239. [Google Scholar]
- Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Physical Therapy. 1987;67:206–207. doi: 10.1093/ptj/67.2.206. [DOI] [PubMed] [Google Scholar]
- Brouwer BJ, Ambury P. Upper extremity weight-bearing effect on corticospinal excitability following stroke. Archives of Physical Medicine and Rehabilitation. 1994;75:861–866. doi: 10.1016/0003-9993(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Chakerian DL, Larson MA. Effects of upper-extremity on hand-opening and prehension patterns in children with cerebral palsy. Developmental Medicine & Child Neurology. 1993;35:216–229. doi: 10.1111/j.1469-8749.1993.tb11626.x. [DOI] [PubMed] [Google Scholar]
- Cunningham CL, Stokykov MEP, Walter CB. Bilateral facilitation of motor control in chronic hemiplegia. Acta Psychologica. 2002;110:321–337. doi: 10.1016/s0001-6918(02)00040-9. [DOI] [PubMed] [Google Scholar]
- Fugl-Meyer AR. Post-stroke hemiplegia assessment of physical properties. Scandinavian Journal of Rehabilitation Medicine. 1980;(Supplement 7):85–93. [PubMed] [Google Scholar]
- Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. I: a method for evaluation of physical performance. Scandinavian Journal of Rehabilitation Medicine. 1975;7:13–31. [PubMed] [Google Scholar]
- Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD. Performance profiles of the functional independence measure. American Journal of Physical Medicine & Rehabilitation. 1993;72:84–89. doi: 10.1097/00002060-199304000-00005. [DOI] [PubMed] [Google Scholar]
- Granger CV, Divan N, Fiedler RC. Functional assessment scales: a study of persons after traumatic brain injury. American Journal of Physical Medicine & Rehabilitation. 1995;74:107–113. [PubMed] [Google Scholar]
- Uniform Data System for Medical Rehabilitation. Guide for the Uniform Data Set for Medical Rehabilitation (Including the FIM instrument). Version 5.1. Buffalo, NY: State University of New York at Buffalo; 1997. [Google Scholar]
- Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level functional independence measure. Scandinavian Journal of Rehabilitation Medicine. 1994;26:115–119. [PubMed] [Google Scholar]
- Jeffcott LB, Holmes MA, Townsend HGG. Validity of saddle pressure measurementsusing force-sensing array technology: preliminary studies. Veterinary Journal. 1999;158:113–119. doi: 10.1053/tvjl.1998.0334. [DOI] [PubMed] [Google Scholar]
- Kinghorn J, Roberts G. The effect of an inhibitive weight-bearing splint on tone and function: a single-case study. American Journal of Occupational Therapy. 1996;50:807–815. doi: 10.5014/ajot.50.10.807. [DOI] [PubMed] [Google Scholar]
- Lang CE, Wagner JM, Edwards DF, Dromerick AW. Upper extremity use in people with hemiparesis in the first few weeks after stroke. Journal of Neurologic Physical Therapy. 2007;31:56–63. doi: 10.1097/NPT.0b013e31806748bd. [DOI] [PubMed] [Google Scholar]
- van der Lee JH, Wagenaar RC, Lankhorst G, Vogelaar TW, Devillé WL, Bouter LM. Forced use of the upper extremity in chronic stroke patients: results from a single-blind randomized clinical trial. Stroke. 1999;30:2369–2375. doi: 10.1161/01.str.30.11.2369. [DOI] [PubMed] [Google Scholar]
- Luft AR, McCombe-Waller S, Whitall J, Forrester LW, Macko R, Sorkin JD. Repetitive bilateral arm training and motor cortex activation in chronic stroke: a randomized controlled trial. Journal of the American Medical Association. 2004;292:1853–1861. doi: 10.1001/jama.292.15.1853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luke C, Dodd KJ, Brock K. Outcomes of the Bobath concept on upper limb recovery following stroke. Clinical Rehabilitation. 2004;18:888–898. doi: 10.1191/0269215504cr793oa. [DOI] [PubMed] [Google Scholar]
- Lum PS, Burgar CG, Van der Loos M, Shor PC, Majmundar M, Yap R. MIME robotic device for upper-limb neurorehabilitation in subacute stroke subjects: a follow-up study. Journal of Rehabilitation Research and Development. 2006;43:631–642. doi: 10.1682/jrrd.2005.02.0044. [DOI] [PubMed] [Google Scholar]
- Mudie MH, Matyas TA. Can simultaneous bilateral movement involve the undamaged hemisphere in reconstruction of neural networks damaged by stroke? Disability and Rehabilitation. 2000;22:23–37. doi: 10.1080/096382800297097. [DOI] [PubMed] [Google Scholar]
- Ottenbacher KJ, Mann WC, Granger CV, Tomita M, Hurren D, Charvat B. Inter-rater agreement and stability of functional assessment in community-based elderly. Archives of Physical Medicine and Rehabilitation. 1994;75:1297–1301. [PubMed] [Google Scholar]
- Parker VM, Wade DT, Langton Hewer R. Loss of arm function after stroke: measurement, frequency, and recovery. International Rehabilitation Medicine. 1986;8:69–73. doi: 10.3109/03790798609166178. [DOI] [PubMed] [Google Scholar]
- Roerdink M, Geurts ACH, de Haart M, Beek PJ. On the relative contribution of the paretic leg to the control of posture after stroke. Neurorehabilitation & Neural Repair. 2008;23(3):267–274. doi: 10.1177/1545968308323928. [DOI] [PubMed] [Google Scholar]
- Rosenstein L, Ridgel AL, Thota A, Samame B, Alberts JL. Effects of combined robotic therapy and repetitive-task practice on upper-extremity function in a patient with chronic stroke. American Journal of Occupational Therapy. 2008;62:28–35. doi: 10.5014/ajot.62.1.28. [DOI] [PubMed] [Google Scholar]
- Sanford J, Moreland J, Swanson LR, Stratford PW, Gowland C. Reliability of the Fugl-Meyer assessment for testing motor performance in patients following stroke. Physical Therapy. 1993;73:447–454. doi: 10.1093/ptj/73.7.447. [DOI] [PubMed] [Google Scholar]
- Serrien DJ, Ivry RB, Swinnen SP. The missing link between action and cognition. Progress in Neurobiology. 2007;82:95–107. doi: 10.1016/j.pneurobio.2007.02.003. [DOI] [PubMed] [Google Scholar]
- Shectman O, Hanson CS, Garrett D, Dunn P. Comparing wheelchair cushions for effectiveness of pressure relief: a pilot study. Occupational Therapy Journal of Research. 2001;21:29–48. [Google Scholar]
- Stein J, Krebs HI, Forontera WR, Fasoli SE, Hughes R, Hogan N. Comparison of two techniques of robot-aided upper limb exercise training after stroke. American Journal of Physical Medicine & Rehabilitation. 2004;82:720–728. doi: 10.1097/01.phm.0000137313.14480.ce. [DOI] [PubMed] [Google Scholar]
- Stewart KC, Cauraugh JH, Summers JJ. Bilateral movement training and stroke rehabilitation: a systematic review and meta-analysis. Journal of the Neurological Sciences. 2006;244:89–95. doi: 10.1016/j.jns.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Stineman MG, Shea JA, Jette A, Tassoni CJ, Ottenbacher KJ, Fielder R, Granger CV. The Functional Independence Measure: Tests of scaling assomptions, structure, and reliability across 20 diverse impairment categories. Archives of Physical Medicine & Rehabilitation. 1996;77:1101–1108. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- Uhl TL, Carver TJ, Mattacola CG, Mair SD, Nitz AJ. Shoulder musculature activation during upper extremity weight-bearing exercise. Journal of Orthopaedic & Sports Physical Therapy. 2003;33:109–117. doi: 10.2519/jospt.2003.33.3.109. [DOI] [PubMed] [Google Scholar]