Abstract
BACKGROUND
Magnetic resonance imaging (MRI) of the knee is often performed in patients who have knee symptoms of unclear cause. When meniscal tears are found, it is commonly assumed that the symptoms are attributable to them. However, there is a paucity of data regarding the prevalence of meniscal damage in the general population and the association of meniscal tears with knee symptoms and with radiographic evidence of osteoarthritis.
METHODS
We studied persons from Framingham, Massachusetts, who were drawn from census-tract data and random-digit telephone dialing. Subjects were 50 to 90 years of age and ambulatory; selection was not made on the basis of knee or other joint problems. We assessed the integrity of the menisci in the right knee on 1.5-tesla MRI scans obtained from 991 subjects (57% of whom were women). Symptoms involving the right knee were evaluated by questionnaire.
RESULTS
The prevalence of a meniscal tear or of meniscal destruction in the right knee as detected on MRI ranged from 19% (95% confidence interval [CI], 15 to 24) among women 50 to 59 years of age to 56% (95% CI, 46 to 66) among men 70 to 90 years of age; prevalences were not materially lower when subjects who had had previous knee surgery were excluded. Among persons with radiographic evidence of osteoarthritis (Kellgren–Lawrence grade 2 or higher, on a scale of 0 to 4, with higher numbers indicating more definite signs of osteoarthritis), the prevalence of a meniscal tear was 63% among those with knee pain, aching, or stiffness on most days and 60% among those without these symptoms. The corresponding prevalences among persons without radiographic evidence of osteoarthritis were 32% and 23%. Sixty-one percent of the subjects who had meniscal tears in their knees had not had any pain, aching, or stiffness during the previous month.
CONCLUSIONS
Incidental meniscal findings on MRI of the knee are common in the general population and increase with increasing age.
The menisci are two semilunar, fibrocartilaginous disks located between the medial and lateral articular surfaces of the femur and tibia in each knee. Their key functions are the transfer of weight and absorption of shock during dynamic movements of the knee, thus protecting the cartilage in the joint.1–3 A meniscal tear is a frequent orthopedic diagnosis, and arthroscopic partial meniscectomy is the most frequent surgical procedure performed by orthopedic surgeons in the United States, with more than 50% of the procedures performed in patients 45 years of age or older.4 People in whom this procedure has been performed are at increased risk for knee osteoarthritis, 5–7 which is one of the most common causes of musculoskeletal disability in developed countries.8,9
Magnetic resonance imaging (MRI) of the knee is widely used to diagnose damage to the menisci, and clinicians often use the findings as a factor in determining whether a person should undergo an arthroscopic meniscectomy. However, there is a paucity of epidemiologic data on the prevalence of meniscal tears in the general population, making it difficult to interpret the diagnostic information provided by MRI among persons who have symptoms that are possibly attributable to tears. We designed this study to determine the prevalence of meniscal damage, including meniscal tears, and the association of meniscal damage with knee osteoarthritis and symptoms in a large sample of middle-aged and elderly men and women who were representative of the general population.
METHODS
STUDY DESIGN AND SUBJECT RECRUITMENT
We recruited subjects from the town of Framingham, Massachusetts. (The study cohort is distinct from the Framingham Heart Study and the Framingham Offspring Study cohorts.) Framingham census-tract data from the year 2000 and random-digit telephone dialing were used to recruit study participants; they were not selected on the basis of having knee or other joint problems. Repeated efforts were made to contact potential subjects by telephone, with a minimum of 15 attempts made over at least a 4-week period before a telephone number was retired from the list of randomly selected numbers. Potential subjects were called at least once each during daytime hours on a weekday, evening hours on a weekday, and weekend hours, although most were called several times during each of these periods. All persons who initially declined to participate were called back in an attempt to reverse their decision. Unless they were adamant at the time of the second refusal, they were also called a third time at least 2 weeks later. To enhance recruitment efforts, community leaders and Framingham senior centers were informed of the study, and flyers were posted in public areas. The institutional review board of Boston University Medical Center approved the study, including our call strategy, and we obtained written informed consent from all participants.
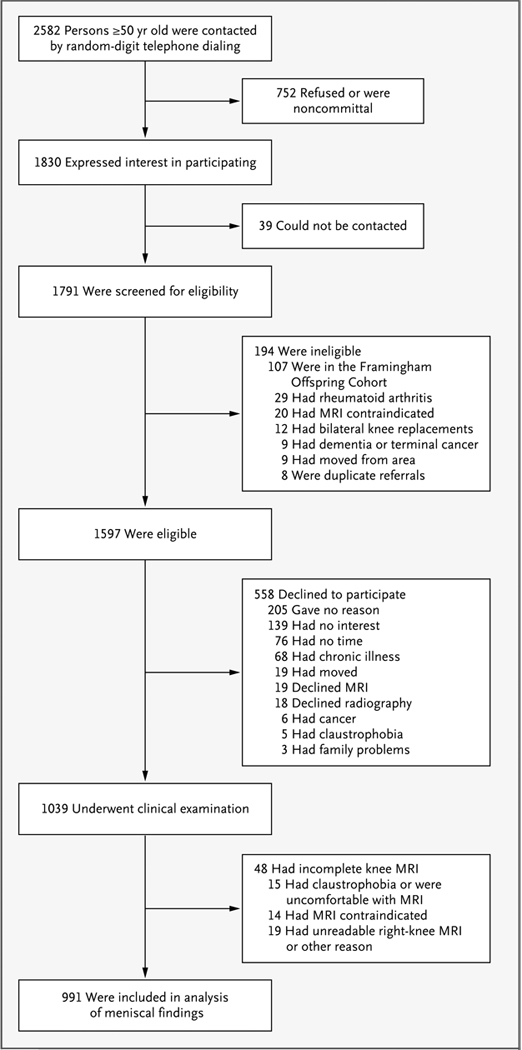
To be included in the study, subjects had to be at least 50 years of age and ambulatory (use of assistive devices such as canes and walkers was allowed), with no plans to move out of the area for at least 5 years. Subjects with a history of bilateral total knee replacement, rheumatoid arthritis,10 dementia, or terminal cancer and those who had contraindications to MRI were excluded. Of 2582 people 50 years of age or older and living in Framingham who were contacted by random-digit dialing, 1830 expressed initial interest in participating in the study. Of these subjects, 1039 were examined during the period from October 2002 to June 2005. We assessed the integrity of the medial and lateral menisci in the right knee in persons who were willing and eligible to undergo MRI and whose scans were readable (991 subjects) (Fig. 1).
Figure 1.
Recruitment and Enrollment of Study Participants from the General Population in Framingham, Massachusetts.
MRI AND GRADING OF MENISCAL INTEGRITY
MRI scans of the knee were obtained with the use of a 1.5-tesla scanner (Siemens) with a phased-array knee coil. Images from three pulse sequences were used in the assessment of the integrity of the menisci: sagittal and coronal fat-saturated, proton-density–weighted, turbo spin–echo images (repetition time, 3610 msec; echo time, 40 msec; slice thickness, 3.5 mm; interslice gap, 0 mm; echo spacing, 13.2 msec; turbo factor, 7; field of view, 140 mm × 140 mm; matrix, 256 × 256) and sagittal T1-weighted spin–echo images (repetition time, 475 msec; echo time, 24 msec; slice thickness, 3.5 mm; interslice gap, 0 mm; field of view, 140 mm × 140 mm; matrix, 256 × 256).
The MRI scans were read by one reader, who had a background in orthopedics; for cases in which the finding was not definitive, confirmation was obtained from a second reviewer, who was a musculoskeletal radiologist. Readings were performed for each of the meniscal segments (the anterior horn, the body, and the posterior horn) for both the medial and lateral menisci. Interob-server agreement (kappa statistic) for the detection of meniscal damage was 0.72. The readers were unaware of the characteristics of the subjects and of the clinical and radiographic data.
We regarded an increased meniscal signal as indicative of a meniscal tear when it communicated with the inferior, superior, or free edge of the meniscal surface (or more than one of those) on at least two consecutive images (or for a radial tear, if it was visible on both the coronal and sagittal images).11,12 Tears were categorized as follows: horizontal, defined as a tear parallel to the tibial plateau separating the meniscus into upper and lower parts; oblique (parrot-beak), defined as a tear oblique to the circumferentially oriented collagen fibers; longitudinal, defined as a vertical tear perpendicular to the tibial plateau and parallel to the orientation of the circumferential fibers; radial, defined as a vertical tear that began in the central free margin and was perpendicular both to the tibial plateau and to the circumferential fiber orientation; complex, defined as multiple tears in more than one configuration; and root, defined as a tear in the posterior or anterior central meniscal attachment.13 The absence of meniscal tissue owing to complete maceration, destruction, or surgical resection was recorded as mensical destruction. In this report, we refer to meniscal damage as a tear or destruction of either segment of the medial or lateral meniscus (see Fig. 1 in the Supplementary Appendix, available with the full text of this article at www.nejm.org).
KNEE RADIOGRAPHY AND GRADING OF IMAGES
Weight-bearing posteroanterior knee radiography with the use of a fixed-flexion protocol14,15 was performed for 963 of the 991 subjects whose MRI scans of the right knee were readable. One musculoskeletal radiologist, who was unaware of the MRI findings and clinical data, graded all radiographs according to the Kellgren–Lawrence scale (intraobserver kappa, 0.83).16,17 Radiographic tibiofemoral osteoarthritis was considered to be present if the Kellgren–Lawrence grade was 2 or higher (on a scale of 0 to 4, with higher numbers indicating more definite signs of osteoarthritis).
QUESTIONNAIRES
At the clinic visit, subjects filled out questionnaires concerning knee-joint symptoms. They were asked, “In the past month, have you had any pain, aching, or stiffness in your knees?” and “On most days, do you have pain, aching, or stiffness in either of your knees?” If either of these questions was answered in the affirmative, we asked additional questions about whether these symptoms were present in the left or right knee or in both knees. For all analyses, we used only information that was specific to the right knee.
The subjects’ weight without shoes was measured with the use of a balance-beam scale, and height was measured with the use of a stadiometer. The body-mass index was calculated as the weight in kilograms divided by the square of the height in meters.
STATISTICAL ANALYSIS
We calculated the prevalence of meniscal findings on MRI and the 95% confidence interval with the use of the modified Wald method.18 Comparisons between groups were made with the use of the chi-square test, the t-test, or one-way analysis of variance, as appropriate. We report prevalence ratios because the odds ratio overestimates the prevalence ratio when the outcome is frequent (as is the case with meniscal tears in this study). We calculated adjusted prevalence ratios using a Cox proportional-hazards model, with a constant time period assigned to all subjects and robust variance estimation.19 All tests were two-tailed, and P values of less than 0.05 were considered to indicate statistical significance. Analyses were performed with Stata/IC 10 for Windows software.
RESULTS
CHARACTERISTICS OF THE STUDY SAMPLE
Of the 991 subjects, 57% were women, and 93% were white. The mean age was 62.3 years (range, 50.1 to 90.5), and the mean body-mass index was 28.5 (range, 16.6 to 55.6) (Table 1). The sample was representative of the Framingham census-tract population, except that the study subjects were slightly younger. (The proportion of persons 70 years of age or older was 14% lower in the study sample than in the census-tract population.)
Table 1.
Characteristics of the Study Sample.*
| Characteristic | Subjects (N = 991) |
|---|---|
| Age — yr | 62.3±8.6 |
| Female sex — no. (%) | 565 (57) |
| White race — no. (%)† | 922 (93) |
| Body-mass index‡ | 28.5±5.6 |
| Current smoker — no./total no. (%) | 106/946 (11) |
| Characteristics of the right knee — no./total no. (%) | |
| Any pain, aching, or stiffness in the previous month | 278/965 (29) |
| Pain, aching, or stiffness on most days | 226/966 (23) |
| Any episode of buckling in the previous 3 months | 64/964 (7) |
| Radiographic evidence of osteoarthritis§ | 171/963 (18) |
| Symptomatic osteoarthritis¶ | 90/942 (10) |
| Previous injury‖ | 139/966 (14) |
| Previous surgery | 56/966 (6) |
Plus–minus values are means ±SD.
Race was self-reported.
The body-mass index is the weight in kilograms divided by the square of the height in meters. Data for the body-mass index were missing for 13 subjects.
Tibiofemoral osteoarthritis was defined as a grade of 2 or higher on the Kellgren–Lawrence scale.
Symptomatic osteoarthritis was defined as knee pain, aching, or stiffness on most days and radiographic evidence of tibiofemoral osteoarthritis as defined by a grade of 2 or higher on the Kellgren–Lawrence scale.
Previous injury was defined as a knee injury leading to a reduced ability to walk for at least 3 days or the use of crutches or a cane.
PREVALENCE OF MENISCAL DAMAGE
In the overall sample, the prevalence of meniscal damage in the right knee (i.e., meniscal tear or destruction) was 35% (95% confidence interval [CI], 32 to 38). Damage to the medial meniscus was more common than damage to the lateral meniscus (prevalence, 28% vs. 12%; P<0.001). The prevalence of a meniscal tear (in isolation or in combination with mensical destruction) in the total sample was 31% (95% CI, 28 to 34); meniscal destruction was present in 10% (95% CI, 8 to 12) (Table 2). After excluding subjects who had had previous knee surgery (56 subjects), the prevalence of meniscal destruction was 8%.
Table 2.
Prevalence of Meniscal Damage in the Right Knee among the 426 Men and 565 Women in the Study Cohort.*
| Meniscal Damage | Medial Meniscus | Lateral Meniscus | Medial or Lateral Meniscus | |||
|---|---|---|---|---|---|---|
| no. | % (95% CI) | no. | % (95% CI) | no. | % (95% CI) | |
| Men | ||||||
| One or more tears without destruction | 121 | 28 (24–33) | 37 | 9 (6–12) | 139 | 33 (28–37) |
| Destruction† | 34 | 8 (6–11) | 9 | 2 (1–4) | 39 | 9 (7–12) |
| Any damage | 155 | 36 (32–41) | 46 | 11 (8–14) | 178 | 42 (37–47) |
| Women | ||||||
| One or more tears without destruction | 71 | 13 (10–16) | 60 | 11 (8–13) | 110 | 19 (16–23) |
| Destruction† | 49 | 9 (7–11) | 17 | 3 (2–5) | 62 | 11 (9–14) |
| Any damage | 120 | 21 (18–25) | 77 | 14 (11–17) | 172 | 30 (27–34) |
Milder meniscal signal abnormalities on MRI that were not considered to be sufficient evidence of a tear were present in 68 men (16%) and 104 women (18%) who otherwise did not have evidence of meniscal tear or destruction.
With persons with previous knee surgery (56 persons) excluded, the prevalence of destruction (of either the medial or lateral meniscus) was 7% among men and 9% among women (a decrease of approximately 2%).
Among the 308 persons with a meniscal tear in their right knee, 66% had a medial tear, 24% had a lateral tear, and 10% had both medial and lateral tears. In the knees with one or more tears in the meniscus, the tear involved the posterior horn of the medial or lateral meniscus in 66% of the cases, the body segment in 62%, and the anterior horn in 11%. Forty percent of the knees with a meniscal tear had a horizontal tear, 37% a complex tear, 12% an oblique tear, 15% a radial tear, 7% a longitudinal tear, and 1% a root tear. (The percentages do not add up to 100% because meniscal tears could involve more than one segment of the meniscus or a knee could have more than one type of meniscal tear.)
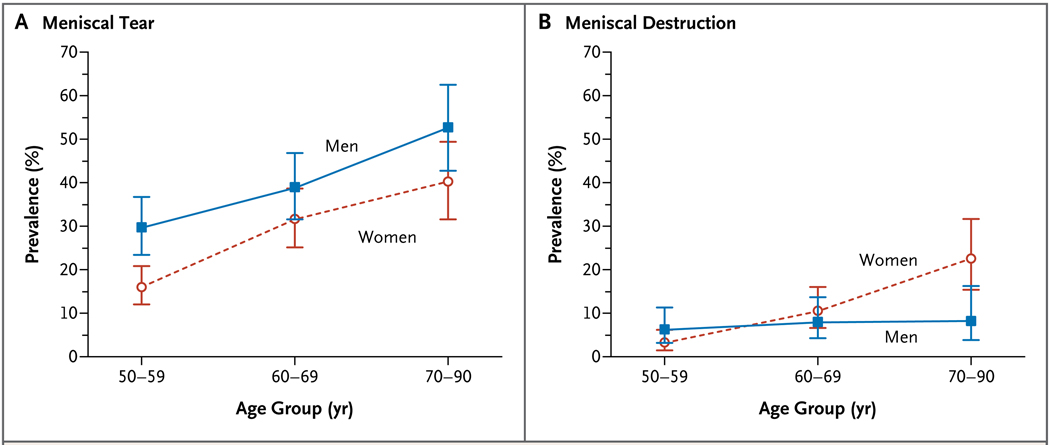
The prevalence of meniscal damage increased with increasing age in both sexes (P<0.001 for trend). Among subjects who were 50 to 59 years of age, the prevalence of a meniscal tear or destruction was 32% (95% CI, 26 to 40) in men and 19% (95% CI, 15 to 24) in women, whereas prevalences were 56% (95% CI, 46 to 66) and 51% (95% CI, 42 to 60), respectively, among those 70 to 90 years of age. Men had a higher prevalence of meniscal tears in all age groups, but women had a higher prevalence of meniscal destruction in the oldest age category (Fig. 2).
Figure 2.
Prevalence of Meniscal Tear or Destruction in the Right Knee among Middle-Aged and Elderly Persons, According to Age Group and Sex.
All persons with previous knee surgery were excluded from the prevalence estimates of meniscal destruction. The I bars denote 95% confidence intervals.
Women with at least one meniscal tear or with meniscal destruction in their right knee had a higher body-mass index than women without meniscal damage (29.9 vs. 27.9, P<0.001), but among men, there was no significant difference in the body-mass index between the group with damage and the group without damage (28.7 and 28.6, respectively; P = 0.83). Demographic and clinical characteristics of persons with no meniscal damage, those with at least one meniscal tear, and those with meniscal destruction are shown in Table 1 in the Supplementary Appendix.
The prevalence of meniscal damage was significantly higher among subjects with radiographic evidence of tibiofemoral osteoarthritis (Kellgren and Lawrence grade 2 or higher) than among those without such evidence (82% vs. 25%, P<0.001), and the prevalence increased with a higher Kellgren and Lawrence grade (P<0.001 for trend). Among persons with radiographic evidence of severe osteoarthritis (Kellgren and Lawrence grade of 3 or 4 in their right knee), 95% had meniscal damage (Table 2 in the Supplementary Appendix).
Although the presence of one or more meniscal tears was more common in persons who had knee pain, aching, or stiffness on most days than in those who did not have these symptoms (45% vs. 26%, P<0.001), this difference was markedly attenuated when radiographic evidence of osteoarthritis was taken into account. In the group of persons with radiographic evidence of osteoarthritis (Kellgren–Lawrence grade 2 or higher), the prevalence of a meniscal tear was 63% among those with knee pain, aching, or stiffness on most days and 60% among those without these symptoms (P = 0.75); the corresponding prevalences in the group without radiographic evidence of osteoarthritis (Kellgren–Lawrence grade 2 or higher) were 32% and 23% (P = 0.02) (Table 3). A majority of the meniscal tears — 180 of 297 (61%) — were in subjects who had not had any pain, aching, or stiffness in the previous month (data on symptoms were missing for 11 subjects). We found no significant differences in the proportions of persons who had symptoms of pain, aching, or stiffness in the knees according to the type of tear or compartment in which the tear occurred or according to whether the tear extended into the peripheral (capsular) third of the meniscus (data not shown).
Table 3.
Prevalence of Meniscal Tears According to the Presence or Absence of Frequent Knee Symptoms and Radiographic Evidence of Osteoarthritis.*
| Meniscal Tears | Frequent Knee Symptoms | Prevalence Ratio† | |||
|---|---|---|---|---|---|
| Yes | No | Unadjusted | Adjusted (95% CI)‡ |
||
| no. (%) | |||||
| Radiographic evidence of osteoarthritis | |||||
| One or more meniscal tears | 57 (63) | 46 (60) | 1.06 | 1.14 (0.90–1.45) | |
| No meniscal tear | 33 (37) | 31 (40) | |||
| No radiographic evidence of osteoarthritis | |||||
| One or more meniscal tears | 41 (32) | 146 (23) | 1.43 | 1.43 (1.08–1.90) | |
| No meniscal tear | 86 (68) | 502 (77) | |||
Frequent knee symptoms were defined as knee pain, aching, or stiffness in the right knee on most days. Radiographic evidence of osteoarthritis was considered present if the Kellgren–Lawrence grade was 2 or higher. Data for 49 of the 991 subjects in the community-based sample were not available (because of missing radiographs, responses to the item in the questionnaire regarding frequent knee symptoms, or both).
The prevalence ratios were calculated as the proportion of subjects with meniscal tears among those with frequent knee symptoms divided by the corresponding proportion among subjects without frequent knee symptoms.
The prevalence ratio is adjusted for age, sex, and body-mass index.
DISCUSSION
We found that meniscal damage in the right knee was common in middle-aged and elderly persons from a suburban community in the United States. The prevalence ranged from 19% among women who were 50 to 59 years old to 56% among men who were 70 to 90 years old and was only minimally lower when persons with previous knee surgery were excluded. The prevalence of meniscal damage increased with increasing age in both sexes. The majority of meniscal tears were found in persons who did not have knee pain, aching, or stiffness.
A high prevalence of meniscal damage (67 to 91%) among patients with symptomatic osteoarthritis of the knee has been reported previously.20–23 In one of these studies, which involved U.S. veterans, most of whom were men, meniscal tears were also noted in 37 of 49 control subjects without knee pain (mean age, 67 years) who were seeking health care for another condition.23 In addition, other reports of MRI findings, including studies of contralateral knees among patients with knee injury, have suggested that a meniscal tear of the knee among persons who do not have symptoms is more common than previously thought.24–28 However, descriptive epidemiologic data on the prevalence of meniscal damage in the general population have been lacking. Our data from a large sample of community-dwelling adults who were not selected on the basis of knee or other joint problems underscore the high prevalence of this condition among older adults, frequently in the absence of symptoms.
Pathological examination must be considered the standard for assessing meniscal integrity. Our prevalence estimates of meniscal damage on MRI are similar to those of degenerative meniscal tears reported in an autopsy study from the 1970s (in which both knees were examined and tears were found in 60 of 100 persons with a mean age of 65 years). However, it is questionable whether that sample was representative of the general population. 29 Furthermore, the sensitivity and specificity of detecting a meniscal tear by MRI are both in the range of 82 to 96%, and our use of the “two-slice touch” rule (requiring increased signal extending to the meniscal surface on at least two images) favors high specificity.11,12
The results of our study suggest that incidental meniscal findings detected on MRI are likely to be frequent in clinical practice. The increased use of MRI for the assessment of knee symptoms may result in considerable confusion, since it may be difficult to discriminate between symptoms associated with a meniscal tear and those associated with another cause; this discrimination may be particularly complicated by the strong association between meniscal damage and the presence of knee osteoarthritis, an association that was seen in this study and in others.23,29,30 Indeed, degenerative meniscal damage appearing as a tear may signal early osteoarthritic disease.31 Other structures or processes related to knee osteoarthritis may be causing the pain, such as synovitis or bone marrow lesions, the latter possibly initiated by altered loading patterns and chronic overloading due to the loss of meniscal function.26,32 Surgical resection of damaged parts of the meniscus is unlikely to reduce pain substantively in patients in whom osteoarthritis is causing or contributing to the symptoms, and evidence is lacking to support the approach of meniscal resection, as compared with nonsurgical treatment, in these patients.33,34
Some limitations of our study should be noted. First, we cannot rule out the possibility of a selection bias in the use of random-digit dialing for recruitment, which may have affected the prevalence estimates, although the prevalence of radiographic evidence of knee osteoarthritis, an important correlate of meniscal damage and knee pain, is similar to that in other community-based samples of this age group from both the United States and Europe.17,35,36 Second, our sample was primarily white, reflecting the population of Framingham; the proportions of other races or ethnic groups were too small to allow for comparisons according to race or ethnic group. Third, funding limitations precluded the reading of MRI scans of both knees, so we focused on the right knee in each person; in a reanalysis of Framingham data sets, we found that right knees had a slightly (2%) higher prevalence of radiographic evidence of osteoarthritis than left knees. Fourth, our prevalence estimates cannot be generalized to younger adults, since the frequency of meniscal damage is age-dependent. Young, physically active adults in whom a meniscal tear is diagnosed are more likely to have sustained tears due to trauma to an otherwise healthy knee, whereas degenerative processes leading to meniscal tears and destruction clearly prevail in middle-aged and elderly persons.37,38 Fifth, we do not have data on catching or locking of the knee, which may be due to dislocation of torn meniscal tissue. Although such symptoms of meniscal damage may remit and recur, they were likely to have been captured by the questions about symptoms that we asked the subjects. In addition, we made no attempt to identify meniscal tears that may have been unstable and therefore associated with an increased risk of mechanical symptoms, since there are no widely accepted or valid criteria for identifying such tears on MRI.39 Finally, our data do not account for the fact that meniscal maceration, destruction, resection, or extrusion may contribute to a narrowing of the joint space as seen on radiographs.40 We wanted to avoid over-diagnosis of osteoarthritis in subjects with this finding and therefore defined osteoarthritis as a grade of 2 or higher (which requires the presence of a definite osteophyte) on the Kellgren–Lawrence scale.
In conclusion, our findings suggest that meniscal damage is common among middle-aged and elderly persons, irrespective of knee symptoms, and often accompanies knee osteoarthritis. Clinicians who order MRI of the knee should take into account the high prevalence of incidental tears when interpreting the results and planning therapy.
Supplementary Material
Acknowledgments
Supported by grants from the National Institutes of Health (AG18393 and AR47785), the Swedish Research Council, the Tegger Foundation, Sweden, and the Arthritis Foundation.
Dr. Guermazi reports holding equity in Synarc, the company that manufactures the frame used for obtaining fixed-flexion knee radiographs. Dr. Gale reports receiving payment from VirtualScopics for radiology readings. No other potential conflict of interest relevant to this article was reported.
We thank Christine McLennan for her critical contribution as project manager for the Framingham Osteoarthritis Community Cohort, the support staff, and all study participants.
REFERENCES
- 1.Kurosawa H, Fukubayashi T, Nakajima H. Load-bearing mode of the knee joint: physical behavior of the knee joint with or without menisci. Clin Orthop Relat Res. 1980;149:283–290. [PubMed] [Google Scholar]
- 2.Shrive NG, O’Connor JJ, Goodfellow JW. Load-bearing in the knee joint. Clin Orthop Relat Res. 1978;131:279–287. [PubMed] [Google Scholar]
- 3.Walker PS, Erkman MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 4.Hall MJ, Lawrence L. Advance data from vital and health statistics. No. 300. Hyattsville, MD: National Center for Health Statistics; 1998. Aug 12, Ambulatory surgery in the United States, 1996. (DHHS publication no. (PHS) 98-1250.) [PubMed] [Google Scholar]
- 5.Englund M, Lohmander LS. Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum. 2004;50:2811–2819. doi: 10.1002/art.20489. [DOI] [PubMed] [Google Scholar]
- 6.Hede A, Larsen E, Sandberg H. Partial versus total meniscectomy: a prospective, randomised study with long-term followup. J Bone Joint Surg Br. 1992;74:118–121. doi: 10.1302/0301-620X.74B1.1732238. [DOI] [PubMed] [Google Scholar]
- 7.Fairbank TJ. Knee joint changes after meniscectomy. J Bone Joint Surg Br. 1948;30:164–170. [PubMed] [Google Scholar]
- 8.Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Arthritis Rheum. 2008;58:26–35. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet. 2006;367:1747–1757. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 10.Karlson EW, Sanchez-Guerrero J, Wright EA, et al. A connective tissue disease screening questionnaire for population studies. Ann Epidemiol. 1995;5:297–302. doi: 10.1016/1047-2797(94)00096-c. [DOI] [PubMed] [Google Scholar]
- 11.Fox MG. MR imaging of the meniscus: review, current trends, and clinical implications. Radiol Clin North Am. 2007;45:1033–1053. doi: 10.1016/j.rcl.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 12.De Smet AA, Tuite MJ. Use of the “two-slice-touch” rule for the MRI diagnosis of meniscal tears. AJR Am J Roentgenol. 2006;187:911–914. doi: 10.2214/AJR.05.1354. [DOI] [PubMed] [Google Scholar]
- 13.Jee WH, McCauley TR, Kim JM, et al. Meniscal tear configurations: categorization with MR imaging. AJR Am J Roentgenol. 2003;180:93–97. doi: 10.2214/ajr.180.1.1800093. [DOI] [PubMed] [Google Scholar]
- 14.Nevitt MC, Peterfy C, Guermazi A, et al. Longitudinal performance evaluation and validation of fixed-flexion radiography of the knee for detection of joint space loss. Arthritis Rheum. 2007;56:1512–1520. doi: 10.1002/art.22557. [DOI] [PubMed] [Google Scholar]
- 15.Kothari M, Guermazi A, von Ingersleben G, et al. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol. 2004;14:1568–1573. doi: 10.1007/s00330-004-2312-6. [DOI] [PubMed] [Google Scholar]
- 16.Kellgren JH, Jeffrey MR, Ball J. Atlas of standard radiographs of arthritis. Vol. 2. Oxford, England: Blackwell Scientific; 1963. The epidemiology of chronic rheumatism. [Google Scholar]
- 17.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly: the Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30:914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 18.Agresti A, Coull BA. Approximate is better than “exact” for interval estimation for binomial proportions. J Am Stat Assoc. 1998;52:119–126. [Google Scholar]
- 19.Lin DY, Wei LJ. The robust interference for the cox proportional hazards model. J Am Stat Assoc. 1989;84:1074–1078. [Google Scholar]
- 20.Englund M, Niu J, Guermazi A, et al. Effect of meniscal damage on the development of frequent knee pain, aching, or stiffness. Arthritis Rheum. 2007;56:4048–4054. doi: 10.1002/art.23071. [DOI] [PubMed] [Google Scholar]
- 21.Kornaat PR, Bloem JL, Ceulemans RY, et al. Osteoarthritis of the knee: association between clinical features and MR imaging findings. Radiology. 2006;239:811–817. doi: 10.1148/radiol.2393050253. [DOI] [PubMed] [Google Scholar]
- 22.Link TM, Steinbach LS, Ghosh S, et al. Osteoarthritis: MR imaging findings in different stages of disease and correlation with clinical findings. Radiology. 2003;226:373–381. doi: 10.1148/radiol.2262012190. [DOI] [PubMed] [Google Scholar]
- 23.Bhattacharyya T, Gale D, Dewire P, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A:4–9. doi: 10.2106/00004623-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Boks SS, Vroegindeweij D, Koes BW, Hunink MM, Bierma-Zeinstra SM. Magnetic resonance imaging abnormalities in symptomatic and contralateral knees: prevalence and associations with traumatic history in general practice. Am J Sports Med. 2006;34:1984–1991. doi: 10.1177/0363546506290189. [DOI] [PubMed] [Google Scholar]
- 25.Ding C, Martel-Pelletier J, Pelletier JP, et al. Meniscal tear as an osteoarthritis risk factor in a largely non-osteoarthritic cohort: a cross-sectional study. J Rheumatol. 2007;34:776–784. [PubMed] [Google Scholar]
- 26.Zanetti M, Pfirrmann CW, Schmid MR, Romero J, Seifert B, Hodler J. Patients with suspected meniscal tears: prevalence of abnormalities seen on MRI of 100 symptomatic and 100 contralateral asymptomatic knees. AJR Am J Roentgenol. 2003;181:635–641. doi: 10.2214/ajr.181.3.1810635. [DOI] [PubMed] [Google Scholar]
- 27.Hayes CW, Jamadar DA, Welch GW, et al. Osteoarthritis of the knee: comparison of MR imaging findings with radiographic severity measurements and pain in middle-aged women. Radiology. 2005;237:998–1007. doi: 10.1148/radiol.2373041989. [DOI] [PubMed] [Google Scholar]
- 28.Beattie KA, Boulos P, Pui M, et al. Abnormalities identified in the knees of asymptomatic volunteers using peripheral magnetic resonance imaging. Osteoarthritis Cartilage. 2005;13:181–186. doi: 10.1016/j.joca.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 29.Noble J, Hamblen DL. The pathology of the degenerate meniscus lesion. J Bone Joint Surg Br. 1975;57:180–186. [PubMed] [Google Scholar]
- 30.Hunter DJ, Zhang YQ, Niu JB, et al. The association of meniscal pathologic changes with cartilage loss in symptomatic knee osteoarthritis. Arthritis Rheum. 2006;54:795–801. doi: 10.1002/art.21724. [DOI] [PubMed] [Google Scholar]
- 31.Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178–2187. doi: 10.1002/art.11088. [DOI] [PubMed] [Google Scholar]
- 32.Felson DT, Chaisson CE, Hill CL, et al. The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med. 2001;134:541–549. doi: 10.7326/0003-4819-134-7-200104030-00007. [DOI] [PubMed] [Google Scholar]
- 33.Howell JR, Handboll HHG. Surgical treatment for meniscal injuries of the knee in adults. Cochrane Database Syst Rev. 2000;2:CD001353. doi: 10.1002/14651858.CD001353. [DOI] [PubMed] [Google Scholar]
- 34.Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81–88. doi: 10.1056/NEJMoa013259. [DOI] [PubMed] [Google Scholar]
- 35.Peat G, McCarney R, Croft P. Knee pain and osteoarthritis in older adults: a review of community burden and current use of primary health care. Ann Rheum Dis. 2001;60:91–97. doi: 10.1136/ard.60.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–180. [PubMed] [Google Scholar]
- 37.Poehling GG, Ruch DS, Chabon SJ. The landscape of meniscal injuries. Clin Sports Med. 1990;9:539–549. [PubMed] [Google Scholar]
- 38.Smillie IS. Injuries of the knee joint. 3rd ed. Edinburgh: E. & S. Livingstone; 1962. Surgical pathology of the menisci; pp. 51–90. [Google Scholar]
- 39.Vande Berg BC, Poilvache P, Duchateau F, et al. Lesions of the menisci of the knee: value of MR imaging criteria for recognition of unstable lesions. AJR Am J Roentgenol. 2001;176:771–776. doi: 10.2214/ajr.176.3.1760771. [DOI] [PubMed] [Google Scholar]
- 40.Hunter DJ, Zhang YQ, Tu X, et al. Change in joint space width: hyaline articular cartilage loss or alteration in meniscus? Arthritis Rheum. 2006;54:2488–2495. doi: 10.1002/art.22016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.