Abstract
Background
The incidence of and outcomes associated with methicillin-resistant Staphylococcus aureus (MRSA) infection in hospitalized children have been incompletely characterized.
Methods
We performed a retrospective, observational study using the Pediatric Health Information System, a database of clinical and financial data from >40 freestanding US children’s hospitals. Using discharge coding data, we characterized S. aureus infections in children <18 years of age who were hospitalized during the period from 1 January 2002 through 31 December 2007.
Results
During this 6-year study period, we identified 57,794 children with S. aureus infection, 29,309 (51%) of whom had MRSA infection. The median age of patients with S. aureus infection was 3.1 years (interquartile range, 0.8–11.2 years), and less than one-third of these patients had complex, chronic medical conditions. Over time, there was a significant increase in cases of MRSA infection (from 6.7 cases per 1000 admissions in 2002 to 21.1 cases per 1000 admissions in 2007; P = .02, by test for trend), whereas the incidence of methicillin-susceptible S. aureus infection remained stable (14.1 cases per 1000 patient-days in 2002 to 14.7 cases per 1000 patient-days in 2007; P = .85, by test for trend). Of the 38,123 patients whose type of infection was identified, 23,280 (61%) had skin and soft-tissue infections. The incidences of skin and soft-tissue infection, pneumonia, osteomyelitis, and bacteremia that were caused by S. aureus increased over time, and these increases were due exclusively to MRSA. The mortality rate for hospitalized children with MRSA infection was 1% (360 of 29,309 children).
Conclusions
There has been a recent increase in the number of hospitalized children with MRSA infection. This increase is largely driven by, but is not limited to, an increase in skin and soft-tissue infections. The mortality rate for hospitalized children with MRSA infection is low.
Staphylococcus aureus causes skin and soft-tissue infection, pneumonia, osteomyelitis, septic arthritis, bacteremia, and other invasive diseases in adults and children [1]. The emergence of methicillin-resistant S. aureus (MRSA) has complicated the treatment of such infections [2, 3]. For many years, cases of MRSA infection were confined to hospitalized patients [4]. However, the recent emergence of community-associated MRSA (CA-MRSA) infections has expanded the realm of MRSA infections to include S. aureus infections with a fundamentally different epidemiology than that of hospital-associated MRSA (HA-MRSA) infections [5]. CA-MRSA infections often occur in individuals without a history of health care exposure and most commonly manifest as skin and soft-tissue infections [6]. In fact, microbiology laboratory data from many urban, tertiary care centers reveal that the majority of community-onset S. aureus skin and soft-tissue infections treated in US emergency departments are caused by MRSA [7]. Likewise, community-onset skin and soft-tissue infections account for the majority of MRSA infections in children [8, 9].
Although many CA-MRSA infections are managed on an outpatient basis, a significant number of CA-MRSA infections in children require hospitalization [10, 11]. Thus, an increase in the rate of MRSA infection in the community should generate an increase in the frequency of hospitalization for MRSA infection. Single-center pediatric studies suggest an increase in the number of hospitalized patients with MRSA infection [11, 12]. However, both the incidence of MRSA infection among children and the practice patterns of physicians may vary by hospital and by region. A recent national study of US emergency departments identified a high rate of hospitalization and mortality due to MRSA infection, but the majority of these patients were older adults with bacteremia [13]. Likewise, other national hospital-based estimates of rates of MRSA infection and associated mortality have included primarily adults and have used indirect strategies to approximate the rates of MRSA infection [14–16]. In this study, our goal was to compare recent trends in the incidence, clinical features, patient characteristics, and outcomes associated with MRSA infection and methicillin-susceptible S. aureus (MSSA) infection in hospitalized children.
METHODS
Study design
We performed a retrospective, observational study to determine the incidence, clinical features, patient characteristics, and outcomes associated with MRSA infection in hospitalized children during a 6-year period from 1 January 2002 through 31 December 2007.
Study population
We used the Pediatric Health Information System, an administrative database managed by the Child Health Corporation of America in Shawnee Mission, Kansas, which contains inpatient data from more than 40 freestanding US children’s hospitals. The Pediatric Health Information System database contains detailed information on each patient’s hospitalization, including demographic characteristics, diagnoses, medications, procedures, and laboratory tests. Member hospitals represent 17 of the 20 major metropolitan areas across the United States, with only 1 children’s hospital representing each city. On the basis of estimates from the National Association of Children’s Hospitals and Related Institutions (Alexandria, VA), 70% of freestanding pediatric acute care hospital admissions in the United States are reported in the Pediatric Health Information System database.
The quality and reliability of the data are maintained by the joint efforts of the Child Health Corporation of America, a data manager (Thomson Healthcare in Durham, NC), and the participating hospitals. Thomson Healthcare is a leading source of healthcare business information and maintains the nation’s largest health care database, which comprises data on more than 22.6 million patients discharged annually from 2900 hospitals, representing 77.5% of all patients discharged. Data from the Pediatric Health Information System are de-identified at the time of submission (before data extraction and analysis) and subjected to a number of reliability and validity checks before being processed into data quality reports. Data are accepted into the database only when classified errors occur in <2% of a hospital’s quarterly data. If a hospital’s quarterly data are unacceptable according to these limits, all of their quarterly data are rejected. However, these data can be resubmitted and reevaluated before inclusion in the database.
Identification of patients with S. aureus infection
Inpatients <18 years of age at admission to a hospital in the Pediatric Health Information System during the period from 1 January 2002 through 31 December 2007 were eligible for our study. Patients admitted to hospitals that did not maintain patient data for the entire study period or that had significant data issues (according to the criteria above) were excluded; thus, patients admitted to 33 hospitals in the Pediatric Health Information System, each of which contributed complete discharge data for all years of the study, were eligible for inclusion. Case status was determined on the basis of the discharge diagnoses that used International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes for S. aureus infection (code 041.11), S. aureus septicemia (code 038.11), or pneumonia due to S. aureus (code 482.41). A case of MRSA infection was determined by the presence of the ICD-9-CM code for methicillin-resistant S. aureus (code V09.0) that was entered into the Pediatric Health Information System database, either alone or in conjunction with an ICD-9-CM code for S. aureus infection (code 041.11), S. aureus septicemia (code 038.11), or pneumonia due to S. aureus (code 482.41). Thus, the presence of any of the aforementioned codes in the patient’s data at patient discharge would classify that patient as exposed to S. aureus infection, followed by a dichotomous secondary classification of MRSA infection or MSSA infection based on the presence of a discharge code for MRSA infection. Medical records that contained multiple S. aureus–related ICD-9-CM codes were counted only once.
For all patients identified as having an S. aureus infection (by use of the aforementioned ICD-9-CM codes), the type of infection was defined by the use of an additional ICD-9-CM code (Appendix, table A1) for skin and soft-tissue infection (cellulitis or abscess), osteomyelitis, myositis, bacteremia, pneumonia, endocarditis, or deep venous thrombosis. A code used to designate the type of infection was present in the medical records of roughly two-thirds of patients with a diagnosis code for S. aureus infection.
APPENDIX Table A1.
Profile of the International Classification of Diseases, Ninth Revision, Clinical Modification codes used to designate types of infection for patients with Staphylococcus aureus infection.
| Type of infection, code(s) | Description |
|---|---|
| Skin and soft-tissue infection | |
| 528.3 | Cellulitis and abscess (of mouth) |
| 681 | Cellulitis and abscess of finger and toe |
| 681.0 and 681.00–681.02 | Finger, unspecified, felon, onychia and paronychia of finger |
| 681.1 and 681.10–681.11 | Toe, unspecified, onychia and paronychia of toe |
| 681.9 | Cellulitis and abscess of unspecified digit |
| 682.0–682.9 | Other cellulitis and abscess |
| Osteomyelitis | |
| 730.00–730.29 | Osteomyelitis, periostitis, and other infections involving bone |
| Myositis | |
| 728.0 | Infective myositis |
| Bacteremia | |
| 790.7 | Bacteremia |
| Pneumonia | |
| 482 | Other bacterial pneumonia |
| 482.4, 482.41, and 482.49 | Pneumonia due to Staphylococcus |
| 482.9 | Bacterial pneumonia unspecified |
| 484 | Pneumonia in infectious diseases classified elsewhere |
| 485 | Bronchopneumonia, organism unspecified |
| 486 | Pneumonia, organism unspecified |
| Endocarditis | |
| 421.0 | Acute and subacute bacterial endocarditis |
| Deep venous thrombosis | |
| 451.1, 451.11, and 451.19 | Phlebitis and thrombophlebitis of deep vessels of lower extremities |
| 453.40 | Venous embolism and thrombosis of unspecified deep vessels of lower extremity |
| 453.41 | Venous embolism and thrombosis of deep vessels of proximal lower extremity |
| 453.42 | Venous embolism and thrombosis of deep vessels of distal lower extremity |
Determination of underlying medical conditions
To assess whether there might be concurrent chronic conditions, we used a previously validated, ICD-9-CM code–based diagnostic classification system for pediatric complex chronic conditions [17]. This nomenclature was developed to identify medical conditions expected to last ≥1 year and likely to require both specialty care and hospitalization at tertiary care center. This classification system divides ICD-9-CM codes into 9 categories of cancerous and noncancerous conditions that require special health services: neuromuscular, cardiovascular, respiratory, renal, gastrointestinal, hematologic or immunologic, metabolic, malignancy, and genetic or other congenital defects, providing a systematic, practical, and validated method to identify children with chronic health conditions.
Statistical analysis
Summary statistics were constructed on the basis of the frequencies and proportions of categorical variables and on the basis of the mean and median values of continuous variables, by use of SAS, version 9.1.3 (SAS Institute). The Wilcoxon rank-sum test for trends and the odds ratios (ORs) and their 95% confidence intervals (CIs) were performed using Stata, version 9 (StataCorp).
RESULTS
Patient characteristics
During the study period from 2002 through 2007, we identified 57,794 inpatients with S. aureus infection from a total of 1,989,233 patients admitted to 33 US children’s hospitals. Of these 57,794 inpatients, 29,309 (51%) received a diagnosis of MRSA infection that was designated with an ICD-9-CM code (table 1). Overall, the majority of patients were male and white. The median age of all children with S. aureus infection was 3.1 years (interquartile range [IQR], 0.8–11.2 years), and 17,373 (30%) of the 57,794 inpatients with S. aureus infection had at least 1 complex chronic condition. Children with MRSA infection were more likely than those with MSSA infection to have skin and soft-tissue infection (47% vs. 33%; OR, 1.75; 95% CI, 1.69–1.81) and to be black (29% vs. 22%; OR, 1.45; 95% CI, 1.39–1.50) but were less likely to have a complex chronic condition (26% vs. 34%; OR, 0.66; 95% CI, 0.64–0.69). Children with MRSA infection and children with MSSA infection were comparable with respect to median age and sex.
Table 1.
Characteristics of patients with Staphylococcus aureus infection in 33 US children’s hospitals during the period from 1 January 2002 through 31 December 2007.
| Characteristic | MRSA infection (n = 29,309) |
MSSA infection (n = 28,485) |
All S. aureus infections (n = 57,794) |
|---|---|---|---|
| Age, median years (IQR) | 2.8 (0.9–11.0) | 3.5 (0.8–11.3) | 3.1 (0.8–11.2) |
| Female sex | 13,777 (47) | 12,714 (45) | 26,491 (46) |
| Race | |||
| White | 17,848 (61) | 18,531 (65) | 36,379 (63) |
| Black | 8416 (29) | 6198 (22) | 14,614 (25) |
| Other | 3045 (10) | 3756 (13) | 6801 (12) |
| Type of infection | |||
| Abscess and cellulitis | 13,740 (47) | 9540 (33) | 23,280 (40) |
| Osteomyelitis | 1757 (6) | 2185 (8) | 3942 (7) |
| Bacteremia | 1514 (5) | 2361 (8) | 3875 (7) |
| Pneumonia | 2856 (10) | 3135 (11) | 5991 (10) |
| Complex chronic conditionsa | |||
| None | 21,750 (74) | 18,671 (66) | 40,421 (70) |
| Any | 7559 (26) | 9814 (34) | 17,373 (30) |
| Cardiovascular | 2182 (7) | 3008 (11) | 5190 (9) |
| Gastrointestinal | 442 (2) | 585 (2) | 1027 (2) |
| Hematologic and/or immunologic | 760 (3) | 990 (4) | 1750 (3) |
| Malignant | 762 (3) | 1553 (5) | 2315 (4) |
| Metabolic | 408 (1) | 595 (2) | 1003 (2) |
| Neuromuscular | 2512 (9) | 2794 (10) | 5306 (9) |
| Renal | 320 (1) | 485 (2) | 805 (1) |
| Respiratory | 1766 (6) | 2225 (8) | 3991 (7) |
| LOS, median days (IQR) | 5 (3–12) | 6 (3–14) | 5 (3–13) |
| Outcome | |||
| Discharged home | 26,867 (92) | 25,000 (88) | 51,867 (90) |
| Died in hospital | 360 (1) | 683 (2) | 1043 (2) |
| Otherb | 2082 (7) | 2802 (10) | 4884 (9) |
NOTE. Data are no. (%) of patients, unless otherwise indicated. IQR, interquartile range; LOS, length of hospital stay; MRSA, methicillin-resistant S. aureus; MSSA, methicillin-susceptible S. aureus.
This classification system divides the International Classification of Diseases, Ninth Revision, Clinical Modification codes into 9 categories of cancerous and noncancerous conditions that require special health services.
Transferred to either short-term care, skilled nursing facility, intermediate care, or home health services or left against medical advice, or data were missing.
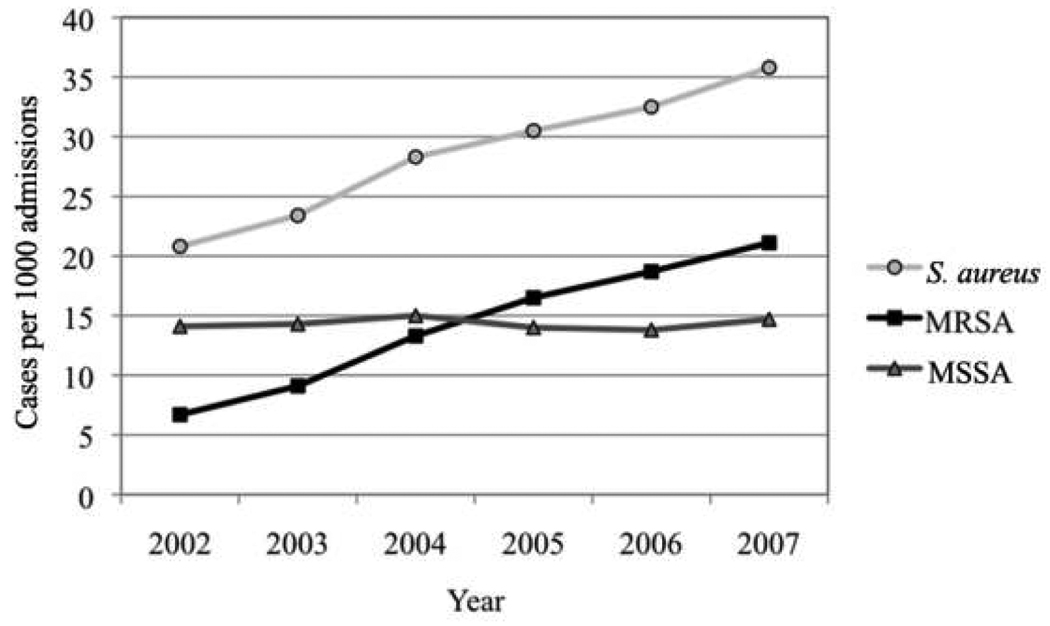
Temporal trends in S. aureus infection
During the course of the study period, there was a significant increase in the overall incidence of S. aureus infection among children (from 20.8 cases per 1000 admissions in 2002 to 35.8 cases per 1000 admission in 2007) and in the incidence of MRSA infection among children (from 6.7 cases per 1000 admissions in 2002 to 21.2 cases per 1000 admission in 2007), whereas the incidence of MSSA infection among children remained stable (from 14.1 cases per 1000 admission in 2002 to 14.7 cases per 1000 admission in 2007) (figure 1). Similar trends were noted when different types of S. aureus infection were analyzed; the incidence of skin and soft-tissue infection, pneumonia, osteomyelitis, and bacteremia that were caused by MRSA increased significantly over time, whereas the incidence of skin and soft-tissue infection, pneumonia, osteomyelitis, and bacteremia that were caused by caused by MSSA remained stable at all of these sites (table 2). Cases of myositis, endocarditis, and deep venous thrombosis that were caused by S. aureus were excluded from the trend analysis, because they each represented ≤1% of all S. aureus infections.
Figure 1.
Rates of all Staphylococcus aureus infections, of methicillin-resistant S. aureus (MRSA) infections, and of methicillin-susceptible S. aureus (MSSA) infections in 33 US children’s hospitals from 2002 to 2007.
Table 2.
Incidences of Staphylococcus aureus infection per 1000 admissions in 33 US children’s hospitals during the period from 1 January 2002 through 31 December 2007, by year and type of infection.
| S. aureus infection | MRSA infection | MSSA infection | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Type of infection | 2002 | 2007 | P | 2002 | 2007 | P | 2002 | 2007 | P |
| All | 20.8 | 35.8 | .02 | 6.7 | 21.1 | .02 | 14.1 | 14.7 | .85 |
| Abscess and cellulitis | 5.9 | 15.9 | .03 | 2.2 | 10.5 | .03 | 3.4 | 5.3 | .09 |
| Osteomyelitis | 1.3 | 2.5 | .03 | 0.3 | 1.4 | .03 | 1.0 | 1.1 | .76 |
| Bacteremia | 1.4 | 2.2 | .04 | 0.4 | 1.0 | .04 | 1.0 | 1.2 | .56 |
| Pneumonia | 2.9 | 3.4 | .09 | 0.9 | 1.9 | .03 | 2.0 | 1.5 | .09 |
NOTE. P value for trend over time; MRSA, methicillin-resistant S. aureus; MSSA, methicillin-susceptible S. aureus.
The predominant type of S. aureus infection was skin and soft-tissue infection. Of the 57,794 children with S. aureus infection, 23,280 (40%) had a skin and soft-tissue infection caused by S. aureus. However, because not all S. aureus infections were further characterized by site of infection, skin and soft-tissue infection accounted for 61% (23,280 of 38,123) of children with S. aureus infection in cases where ICD-9-CM code for site of infection was present. Stratifying S. aureus infections by methicillin resistance, 13,740 (47%) of 29,309 patients with MRSA infection (68% of those with site-of-infection codes) and 9540 (33%) of 28,485 patients with MSSA infection (54% of those with site-of-infection codes) had skin and soft-tissue infections.
Outcomes
The median length of hospital stay was 5 days (IQR, 3–13 days) for all patients with S. aureus infection, 5 days (IQR, 3–12 days) for patients with MRSA infection, and 6 days (IQR, 3–14 days) for patients with MSSA infection. Of the 57,794 children with S. aureus infection, 1043 (2%) died in the hospital, 360 (1%) of whom had MRSA infection and 683 (2%) of whom had MSSA infection (table 1).
DISCUSSION
Prior epidemiological studies that characterized the incidence and implications of MRSA infection have not directly assessed hospitalized children at the national level. By use of active microbiology laboratory surveillance, a 2004–2005 study of 9 US metropolitan areas estimated a relatively high incidence of and a relatively high mortality associated with MRSA infection [13]. Although this was not an inpatient-based study, 92% of the reported patients required hospitalization. However, most were adults with MRSA bacteremia who had either a current or historical association with a health care setting. Of note, the 5–14-year-old age group from this study [13] had a 20-fold lower incidence of MRSA infection than that of the entire cohort, which may indicate a fundamentally different epidemiology of MRSA in hospitalized children. Two additional studies employed a large inpatient database to reveal an increase in MRSA infection during 1999–2000 [16] and during 1999–2005 [14]. By use of this large inpatient database, it was found that the rate of MRSA infection doubled over time (from 4 to 8 cases per 1000 admissions), coincident with a significant increase in rate of skin and soft-tissue infection caused by MRSA during the same period. However, because patient-specific data were not available, the rates of MRSA infection in these analyses were estimated from the data collected from local microbiology laboratory surveillance, and a pediatric age group could not be identified.
To our knowledge, the present study provides the most comprehensive description to date of the epidemiology and burden of MRSA infection among hospitalized children in the United States. We found that MRSA caused more than one-half of all S. aureus infections treated in freestanding children’s hospitals from 2002 through 2007. During the study period, we identified a steady increase in both the overall incidence of S. aureus infection and the incidence of MRSA infection, whereas the incidence of MSSA infection remained stable. Most of these S. aureus infections were skin and soft-tissue infections, and the in-hospital mortality of patients with S. aureus infection—irrespective of methicillin resistance—was low.
Although our analysis did not distinguish between CA-MRSA and HA-MRSA infections, the observed increase in MRSA infections was likely driven by the recent dramatic emergence of CA-MRSA strains that occurred during the study period. The predominance of skin and soft-tissue infections among the cases of MRSA infection in our study is consistent with this hypothesis, because pediatric skin and soft-tissue infections predominantly originate in the community [8, 9]. Furthermore, less than one-third of our MRSA-infected patients had complex chronic conditions [17]. Although complex chronic conditions have not been directly linked to HA-MRSA infection, the relatively frequent hospitalization of children with complex chronic conditions renders them more likely than children without complex chronic conditions to acquire an HA-MRSA infection. Of note, significantly more patients with MRSA infection were black, compared with patients who had MSSA infection. Although the reason for this racial disparity is unclear, it is consistent with previous analyses of CA-MRSA infection [18–20] and colonization [21]. Single-center pediatric studies that documented the impact of the emergence of CA-MRSA infection on the hospitalization of patients also support this hypothesis, confirming both the increased rates of hospitalization over time and the dominance of skin and soft-tissue infection [11, 12]. Although the present study offers only indirect confirmation of this phenomenon, evidence for the influence of CA-MRSA infections on the epidemiology of nosocomial MRSA infections in hospitals is mounting [22–24].
The mortality rate in our study—including all cases of S. aureus infection—was 2%. This rate is at odds with the 6.2%– 8.8% mortality rates calculated for MRSA-infected hospitalized patients in the study by Klein et al. [14] and with the 18% mortality rate that was determined to be the recent national estimate of the MRSA burden by Klevens et al. [13]. As stated above, the majority of these MRSA-infected patients were adults with bacteremia who required hospitalization. In contrast, most of the patients in our study did not have a complex chronic condition or bacteremia; the majority were previously healthy children with skin and soft-tissue infection. Furthermore, because our study captured all-cause mortality, it is likely that the mortality rates attributable to MRSA infection are even lower than those estimated by our analysis. It is interesting to note that the mortality of patients with MRSA infection was lower than that of patients with MSSA infection. This is consistent with CA-MRSA infections being the primary force behind the upsurge in nosocomial MRSA infections; children with CA-MRSA infection are predominantly healthy children with skin and soft-tissue infections, a population with a lower base-line mortality rate than those hospitalized for chronic illnesses (supported by the higher incidence of complex chronic conditions among children with MSSA infection). In other words, the influx of patients with CA-MRSA infection to the hospital may be diluting the previous baseline mortality associated with MRSA infection (and, in effect, relatively inflating the mortality associated with MSSA infection), not because CA-MRSA infection is less virulent, but because it generally infects healthier patients than does HA-MRSA.
Use of the Pediatric Health Information System database offers the unique advantage of national-level, pediatric data. Specifically, the Pediatric Health Information System database contains patient medical records from >40 large, tertiary care children’s hospitals (i.e., >70% of the freestanding children’s hospitals in the United States) that reside in 17 of the 20 major metropolitan areas, each of which is represented by only 1 hospital in the Pediatric Health Information System. This database provides up to 21 diagnosis codes per hospitalization, which is more diagnosis data per patient than any other administrative data set. This large, data-rich, and geographically diverse database, however, may not be generalizable to non–tertiary care, freestanding children’s hospitals. For example, because of referral bias, the Pediatric Health Information System database may overrepresent the true incidence of some medically complicated or severe infections, including those caused by MRSA. Because of this overrepresentation, the low mortality rate observed in this cohort of referral centers is notable.
Despite these advantages, administrative sources of data such as the Pediatric Health Information System are limited with specific regard to the possibility of miscoded or inaccurate information. The accuracy of ICD-9-M codes for diagnosis of either S. aureus or MRSA infection has not been validated for this large population. Although generally specific, ICD-9-CM–based identification may not have ideal sensitivity. For example, when classifying different sites of S. aureus infection, our ICD-9-CM–based approach revealed sites of infection in only two thirds of our cases. However, the reporting of up to 21 discharge diagnosis codes—3-fold more than the national database had used for previous reports of inpatients with S. aureus infection [14, 16]—likely increases our sensitivity relative to the 2 aforementioned studies that used a large inpatient database [14, 16]. Because of the lack of microbiology laboratory data, we have identified patients with MSSA infection as those with an ICD-9-CM code for S. aureus infection but not for MRSA infection in their medical records, taking advantage of the dichotomous nature of S. aureus infections with respect to methicillin resistance. Although it is possible that some cases of MRSA might have been missed (e.g., a diagnosis code for S. aureus infection was entered into the patient’s medical record but an additional diagnosis code for MRSA infection was not), it is unlikely that this would occur differentially by year. In support of this assumption, the overall rate of S. aureus infection increased over time coincident with the increase in the rate of MRSA infection (figure 1); if increased vigilance for properly adding diagnosis codes for MRSA to S. aureus infections over time was the driving force for this increase, the resultant curve would indicate a stable incidence of all S. aureus infections accompanied by a decrease in MSSA infections and an increase in MRSA infections. Furthermore, both the overall incidence of MRSA infection and the distribution of sites of infection from this analysis are consistent with the observations of related studies that used a variety of case definitions and analyses [13, 14, 16]. However, a prospective study to identify patient and infection characteristics supported by patient-specific microbiology laboratory data would be the most reliable method to confirm our findings.
In summary, we have identified a recent increase in MRSA infection among hospitalized children. The predominance of skin and soft-tissue infections, their occurrence in primarily healthy children, the low associated mortality, and the contemporaneous increase in CA-MRSA infections suggest that this increased incidence of MRSA infection in hospitalized children is driven by the recent emergence of CA-MRSA strains.
Acknowledgments
Financial support. The Center for Pediatric Clinical Effectiveness, The Joseph Stokes Jr. Research Institute, and The Children’s Hospital of Philadelphia.
Footnotes
Potential conflicts of interest. All authors: no conflicts.
References
- 1.Lowy FD. Staphylococcus aureus infections. N Engl J Med. 1998;339:520–532. doi: 10.1056/NEJM199808203390806. [DOI] [PubMed] [Google Scholar]
- 2.Daum RS. Clinical practice: skin and soft-tissue infections caused by methicillin-resistant Staphylococcus aureus. N Engl J Med. 2007;357:380–390. doi: 10.1056/NEJMcp070747. (erratum: N Engl J Med 2007; 357:1357) [DOI] [PubMed] [Google Scholar]
- 3.Cosgrove SE, Fowler VG., Jr Management of methicillin-resistant Staphylococcus aureus bacteremia. Clin Infect Dis. 2008;46 Suppl 5:S386–S393. doi: 10.1086/533595. [DOI] [PubMed] [Google Scholar]
- 4.Deurenberg RH, Vink C, Kalenic S, Friedrich AW, Bruggeman CA, Stobberingh EE. The molecular evolution of methicillin-resistant Staphylococcus aureus. Clin Microbiol Infect. 2007;13:222–235. doi: 10.1111/j.1469-0691.2006.01573.x. [DOI] [PubMed] [Google Scholar]
- 5.Boucher HW, Corey GR. Epidemiology of methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008;46 Suppl 5:S344–S349. doi: 10.1086/533590. [DOI] [PubMed] [Google Scholar]
- 6.Stryjewski ME, Chambers HF. Skin and soft-tissue infections caused by community-acquired methicillin-resistant Staphylococcus aureus. Clin Infect Dis. 2008;46 Suppl 5:S368–S377. doi: 10.1086/533593. [DOI] [PubMed] [Google Scholar]
- 7.Moran GJ, Krishnadasan A, Gorwitz RJ, et al. EMERGEncy ID Net Study Group. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355:666–674. doi: 10.1056/NEJMoa055356. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan SL. Implications of methicillin-resistant Staphylococcus aureus as a community-acquired pathogen in pediatric patients. Infect Dis Clin North Am. 2005;19:747–757. doi: 10.1016/j.idc.2005.05.011. [DOI] [PubMed] [Google Scholar]
- 9.Gorwitz RJ. A review of community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infections. Pediatr Infect Dis J. 2008;27:1–7. doi: 10.1097/INF.0b013e31815819bb. [DOI] [PubMed] [Google Scholar]
- 10.McCaskill ML, Mason EO, Jr, Kaplan SL, Hammerman W, Lamberth LB, Hulten KG. Increase of the USA300 clone among community-acquired methicillin-susceptible Staphylococcus aureus causing invasive infections. Pediatr Infect Dis J. 2007;26:1122–1127. doi: 10.1097/INF.0b013e31814536e0. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan SL, Hulten KG, Gonzalez BE, et al. Three-year surveillance of community-acquired Staphylococcus aureus infections in children. Clin Infect Dis. 2005;40:1785–1791. doi: 10.1086/430312. [DOI] [PubMed] [Google Scholar]
- 12.Ochoa TJ, Mohr J, Wanger A, Murphy JR, Heresi GP. Community-associated methicillin-resistant Staphylococcus aureus in pediatric patients. Emerg Infect Dis. 2005;11:966–968. doi: 10.3201/eid1106.050142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klevens RM, Morrison MA, Nadle J, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- 14.Klein E, Smith DL, Laxminarayan R. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999–2005. Emerg Infect Dis. 2007;13:1840–1846. doi: 10.3201/eid1312.070629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarvis WR, Schlosser J, Chinn RY, Tweeten S, Jackson M. National prevalence of methicillin-resistant Staphylococcus aureus in inpatients at US health care facilities, 2006. Am J Infect Control. 2007;35:631–637. doi: 10.1016/j.ajic.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 16.Kuehnert MJ, Hill HA, Kupronis BA, Tokars JI, Solomon SL, Jernigan DB. Methicillin-resistant–Staphylococcus aureus hospitalizations, United States. Emerg Infect Dis. 2005;11:868–872. doi: 10.3201/eid1106.040831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feudtner C, Christakis DA, Connell FA. Pediatric deaths attributable to complex chronic conditions: a population-based study of Washington State, 1980–1997. Pediatrics. 2000;106:205–209. [PubMed] [Google Scholar]
- 18.Skiest DJ, Brown K, Cooper TW, Hoffman-Roberts H, Mussa HR, Elliott AC. Prospective comparison of methicillin-susceptible and methicillin-resistant community-associated Staphylococcus aureus infections in hospitalized patients. J Infect. 2007;54:427–434. doi: 10.1016/j.jinf.2006.09.012. [DOI] [PubMed] [Google Scholar]
- 19.Fridkin SK, Hageman JC, Morrison M, et al. Methicillin-resistant Staphylococcus aureus disease in three communities. N Engl J Med. 2005;352:1436–1444. doi: 10.1056/NEJMoa043252. [DOI] [PubMed] [Google Scholar]
- 20.Sattler CA, Mason EO, Jr, Kaplan SL. Prospective comparison of risk factors and demographic and clinical characteristics of community-acquired, methicillin-resistant versus methicillin-susceptible Staphylococcus aureus infection in children. Pediatr Infect Dis J. 2002;21:910–917. doi: 10.1097/00006454-200210000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Fritz SA, Garbutt J, Elward A, Shannon W, Storch GA. Prevalence of and risk factors for community-acquired methicillin-resistant and methicillin-sensitive Staphylococcus aureus colonization in children seen in a practice-based research network. Pediatrics. 2008;121:1090–1098. doi: 10.1542/peds.2007-2104. [DOI] [PubMed] [Google Scholar]
- 22.Maree CL, Daum RS, Boyle-Vavra S, Matayoshi K, Miller LG. Community-associated methicillin-resistant Staphylococcus aureus isolates causing healthcare-associated infections. Emerg Infect Dis. 2007;13:236–242. doi: 10.3201/eid1302.060781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liu C, Graber CJ, Karr M, et al. A population-based study of the incidence and molecular epidemiology of methicillin-resistant Staphylococcus aureus disease in San Francisco, 2004–2005. Clin Infect Dis. 2008;46:1637–1646. doi: 10.1086/587893. [DOI] [PubMed] [Google Scholar]
- 24.Popovich KJ, Weinstein RA, Hota B. Are community-associated methicillin-resistant Staphylococcus aureus (MRSA) strains replacing traditional nosocomial MRSA strains? Clin Infect Dis. 2008;46:787–794. doi: 10.1086/528716. [DOI] [PubMed] [Google Scholar]