Abstract
Background
The purpose of this secondary analysis was to determine if age affects women’s and men’s exercise adherence after a cardiac event.
Methods
In a convenience sample of 248 adults aged 38–86 having a cardiac event, exercise adherence (exercise three sessions a week) was compared between men and women among three age groups (≤60, 61–70, and >70). Exercise patterns were recorded by heart rate monitors worn during exercise.
Results
No differences were found in adherence between the age groups for women; older men were non-adherent sooner than younger men when controlling for fitness level, pain, comorbidity, self-efficacy, depressed mood, and social support.
Conclusion
Exercise adherence after a cardiac event was higher for younger men compared to older men. At all age groups, less than 37% of the total sample adhered to a three-times-a-week exercise regimen after one year, suggesting that interventions to maintain exercise are needed.
An important component of recovery from a cardiac event is lifestyle modification that includes exercise. Many older adults after a cardiac event participate in an out-patient cardiac rehabilitation programs (CRP) to assist with the adoption of exercise. Out-patient CRPs consist of medically supervised exercise three times a week for 12 weeks (American Association of Cardiovascular and Pulmonary Rehabilitation, 2004). The benefits of adopting a 12-week cardiac rehabilitation exercise program are a 20 to 31% reduction in mortality from heart disease, improved functional capacity (Jolliffe et al., 2000; Jolliffe et al., 2001; Taylor et al., 2004), reduction in cardiac risk factors, improvement in emotional health and quality of life (Wenger et al., 1995), improvement in cognitive function (Gunstad et al., 2005), and improvement in lower extremity function (Dolansky & Moore, 2000). To maintain these benefits, exercise must continue for life. Participants who complete a CRP are given the recommendation to continue to exercise a minimum of three times per week as established during the CRP.
Continuation of the exercise regimen is difficult as only 15% to 50% of the participants continue to exercise 6 months after completion of a CRP (Ades et al., 1999; Bock et al., 1997; Moore et al., 1998). Gender differences exist as women are more vulnerable to not adhering to the exercise regimen compared to men (Moore et al., 2006), even for older adults (Lee, 2005). Although community-based older adults have been reported to be less active than younger adults (Milner, 2008; O'Brien Cousins, 1998), it is not known whether this trend exists for CRP participants. Thus the purpose of this secondary analysis was to determine if age affects women’s and men’s exercise adherence after a cardiac event and completion of a CRP. Understanding differences between young and old adults will assist with the tailoring of interventions to help cardiac patients continue to exercise for life.
Background
As a disease management strategy following hospitalization for a cardiac event, outpatient CRPs offer a comprehensive approach to the integration of healthy lifestyle practices. Although CRP services are not offered under all private insurance plans, CRPs are a covered service for older adults under Medicare. The Centers for Disease Control and Prevention states that participation in a CRP by patients following a cardiac event is a key strategy for reducing further disability (2008). The goals of CRPs are to improve functional capacity, alleviate activity-related symptoms, reduce disability, and modify coronary risk factors in an attempt to reduce subsequent morbidity and mortality (Balady et al., 2000).The focus of CRPs on exercise and the requirement for a cardiac stress test prior to enrollment results in participants who are generally more fit and physically able and motivated to exercise. In addition to being physically able, participants in CRPs are predominately male and have a physician that recommends the use of these services (Ades et al., 1992a; Ades et al., 1992b; Harlan, et al., 1995; Husak et al., 2004; Lieberman et al., 1998).
Factors related to adherence to an exercise program include comorbidity (Ades et al., 1999; O'Brien Cousins, 1998), fitness level (McAuley et al., 1999; Newson & Kemps, 2007), muscle and joint pain (Moore et al., 2003), self-efficacy (McAuley et al., 1993; McAuley, 1993; Clark, 1999; Oman & King, 1998; Bock et al., 1997), depression (Blumenthal et al., 2004; Milani et al., 1993), social support (Lieberman et al., 1998), and race (Crespo et al., 2000). Older cardiac patients are particularly vulnerable to not participate in a CRP as they tend to have decreased physical fitness, reduced muscle strength, and higher levels of depression (Ades, 1999; Ades et al., 2002). In addition, older adults have more comorbidity than younger adults, including a higher incidence of arthritis that may interfere with exercise (Schoenberg et al., 2007). Given that both the trend in community dwelling older adults is to be less physically active and that older adults have more comorbidity, less social support, more disability and depression that is associated with less exercise adherence, it is possible that differences exist in adherence to exercise guidelines between older and younger adults. Thus this secondary analysis addresses the following research questions:
During the year following completion of a CRP, what are the trends in adherence to exercise 3 times a week for men and women for three age groups: ≤60, 61 to 70 and >70?
For women and men, are there differences in adherence to exercise 3 times a week for each of these age groups?
Do these differences remain when controlling for race, comorbidity, physical fitness, pain, self-efficacy, depression and social support?
Methods
Sample
A convenience sample was recruited for a prospective longitudinal intervention study between November 2000 and December 2002 from three Phase II CRP locations in Cleveland, OH (Moore et al., 2006). These individuals started the CRP after a hospitalization for myocardial infarction, cardiac bypass surgery, and/or angioplasty. Individuals were approached as they neared the end of their 12-week out-patient CRP. Every female and minority was approached while every other Caucasian male was approached in order to obtain sufficient numbers of these subpopulations. Regardless of intervention group assigned by the parent study, all participants were included in the current secondary analysis because no differences were found between the intervention and control groups in the outcome variables for this current study.
Exclusion criteria included these criteria for safe exercise after a cardiac event: ejection fraction lower than 30%, a decrease in systolic blood pressure greater than 15 mmHg with exercise, serious arrhythmias at rest or with exercise, or ischemia with exercise indicated by angina and greater than 2 mm ST segment depression on ECG. There were 546 persons who met the study enrollment criteria. Of these, 273 participants were enrolled into the study. This refusal rate is consistent with other cardiac studies (Moore, 1996; Moore & Dolansky, 2001). Fourteen participants dropped prior to assessment of baseline measures, while nine dropped between baseline measurement and completion of CRP. Two individuals were deemed outliers for having reported several hours of walking daily, and were dropped from the analysis to yield a final sample size of 248. Individuals who dropped during the study period after baseline measurements were included in the analysis because the statistics used in the analysis (Kaplan-Meier and Cox regression) appropriately censor these cases.
The sample consisted of 38.3% women and 61.7% men. The mean age of the sample was 62.4 ± 11.1 years with a mean level of education of 14.1± 2.6 years. Eighty-one percent were Caucasian, 17% were African American, and 2% were neither Caucasian nor African American. Cardiac events included hospitalization for a myocardial infarction (51.6%), coronary artery bypass surgery (55.2%), or angioplasty (58.9%). The data were examined for natural break points in age categories and the following were used (≤60, 61–70, and age>70). The demographic information for each age group is shown in Table 1. The mean age for each of the three groups was 51.8 ± 5.4 (age group ≤ 60), 65.5 ± 3.0 (age group 61–70), 76.0 ± 4.5 (age group >70).
Table 1.
Sample Demographic and Predictor Variables by Age Group (N=248)
| ≤60 years old (N=108) N (%) |
61–70 years old (N=73) N (%) |
>70 years old (N=67) N (%) |
||||
|---|---|---|---|---|---|---|
| Female | Male | Female | Male | Female | Male | |
| Race: Caucasian | 21(57) | 65(92) | 21(72) | 33(75) | 26(90) | 35(92) |
| African American | 14(38) | 5(7) | 7(24) | 10(28) | 3(10) | 3(8) |
| Other | 2(5.4) | 1(1.4) | 1(3.4) | 1(2.3) | ||
| Married** includes separated | 18(49) | 58(82) | 18(62) | 34(77) | 13(45) | 31(82) |
| Retired** | 3(8.1) | 6(8.5) | 15(52) | 29(66) | 25(86) | 30(79) |
| Comorbidities | ||||||
| Diabetes | 13(35.1) | 12(16.9) | 8(27.6) | 10(22.7) | 8(27.6) | 9(23.7) |
| Arthritis* | 19(51.4) | 18(25.4) | 21(72.4) | 14(31.80) | 29(69) | 16(42.1) |
| Mean (SD) | Mean (SD) | Mean (SD) | ||||
| Years of school attended | 13.2(1.9) | 15.3(2.5) | 13.6(2.0) | 13.9(3.0) | 13.9(3.0) | 14.3(2.6) |
| Physical Factors | ||||||
| Fitness Six Minute Walk Test (# feet walked)** |
1067(353) | 1338(265) | 1000(279) | 1236(285) | 880(306) | 1026(247) |
| Muscle and joint pain | 1.92(1.0) | 1.46(.77) | 1.83(.97) | 1.57(.76) | 1.86(1.1) | 1.74(.83) |
| Comorbidity (Charlson) ** | 1.46(1.2) | 1.32(1.5) | 1.29(.75) | 1.16(1.2) | 1.97(1.5) | 1.74(1.5) |
| Psychosocial Factors | ||||||
| Self-efficacy for barriers | 66.9(21.7) | 73.7(17.1) | 69.7(22.7) | 76.7(16.6) | 69.7(21.8) | 78.1(17.9) |
| Depressed mood-POMS | 8.0(10.29) | 6.45(8.6) | 4.76(9.9) | 4.39(7.4) | 7.31(9.70) | 3.81(4.9) |
| Social support - Family subscale* |
23.1(10.1) | 23.2(9.6) | 22.7(10.1) | 25.8(9.8) | 20.1(9.36) | 21.0(8.0) |
Significant difference between age groups, p < .05
Significant difference between age groups, p < .01
Measures
Dependent Variable
Exercise sessions were recorded using a portable wristwatch heart rate monitor worn by the participant (Polar Vantage NV) and data were aggregated to determine the number of exercise sessions performed each week. Although adherence to exercise is currently defined by the American Heart Association as minimum of 5– 30 minute sessions per week at a moderate intensity (Haskell et al., 2007), this analysis is based on a more liberal definition of exercising three times a week as recommended by the American Heart Association at the time of subject accrual into the study. A non-adherence event was calculated as occurring the week after the last time a participant did not meet the guideline of three exercise sessions a week. The duration of the individual exercise sessions (N=12,527) ranged from 8 minutes to 62 minutes. Of these 12,527 recorded exercise sessions, 95% were at least 20 minutes in length and 86% were at least 30 minutes in length.
Candidate Predictor Variables
A candidate set of predictor variables were based on Ewart’s conceptual model, Social Problem Solving Model, that describes how component processes interact to influence health behavior (Ewart, 1990). Demographic, physical, and psychosocial variables that were postulated to affect exercise adherence were assessed during the baseline interview (week 6–8 of the CRP). Demographic variables included age, gender and race. Physical variables were fitness, muscle and joint pain, and comorbidity. Fitness was measured by the Six-Minute Walk Test. Muscle and joint pain was measured by the question, “How much muscle or joint pain do you experience while exercising?” Responses range from no discomfort (1) to severe discomfort (4). Comorbidity was assessed using the Charlson Comorbidity Index (Jaeger et al., 1994; Sachdev et al., 2004; Verderber et al., 1999) which measures the impact of comorbid diseases using a weighted scale. The higher the score, the greater the comorbidity.
Psychosocial variables were self-efficacy, depressed mood, and social support. Self-efficacy was measured using the Barriers to Exercise Self-efficacy Scale, which assesses the participant’s perceived confidence to overcome commonly identified barriers to exercise three times weekly for at least 40 minutes over the subsequent two months (McAuley, 1993). Higher scores indicate more self-efficacy to adhere to an exercise program. Depressed mood was measured using the Depression/Dejection scale of the Profile of Mood States (POMS) (McNair et al., 1981). Participants were asked to respond to psychological and emotional responses to stressors in the previous week using a Likert-like scale. Higher scores reflect greater mood disturbance. Social support was measured using the family subscale of the Social Support for Exercise Scale (Sallis et al., 1987); higher scores reflect greater perception of social support from family members.
Procedures and Analysis
Individuals who met study inclusion criteria during weeks 6–8 of their CRP were recruited by trained clinicians. Written informed consent from participants was obtained prior to baseline data collection. The baseline measures included all candidate predictor variables. Each participant was given a heart rate monitor and exercise diary. Participants were directed to return by mail both the monitor and diary each month upon receipt of a new monitor and diary for the next 12 months. Individuals were given exercise prescriptions from their CRP that included a target heart rate and were counseled to exercise at least three times a week for 30 minutes at their target heart rate.
Survival analysis was used to determine the relationships between age group, gender, and time to cessation of exercise. Time was measured in weeks. A non-adherence event was defined as exercising less than three times a week and was recorded as the week after the last week during which the participant exercised fewer than three times. Participants who reported no exercise throughout the study were recorded as having an event at week one. Participants who dropped from the study were censored in the week they dropped if they met the adherence guideline in the last week of participation. Kaplan-Meier (KM) plots of survival distributions were examined by age group for women and men. The log rank test was used to compare differences in the survival distributions. The Cox proportional hazards regression model was used to test the relationship of the candidate predictor variables with adherence to exercise. The confidence interval for significant predictors was set at 95%. Demographic variables (age groups, race), physical variables (fitness, muscle and joint pain, and comorbidity), and psychosocial variables (self-efficacy, depressed mood, and social support) were included in the final model.
Results
The means and standard deviations of the physical and psychosocial variables by gender within age categories are listed in Table 1. The oldest age group had significantly lower scores on the 6-Minute Walk Test, more comorbidity compared to the youngest age group, and less reported family social support. The older groups (61–70 and <70) had significantly more reported arthritis than the younger group. Although not significantly different, men over70 years of age had the highest self efficacy for barriers scores and the younger women had the highest levels of depressed mood.
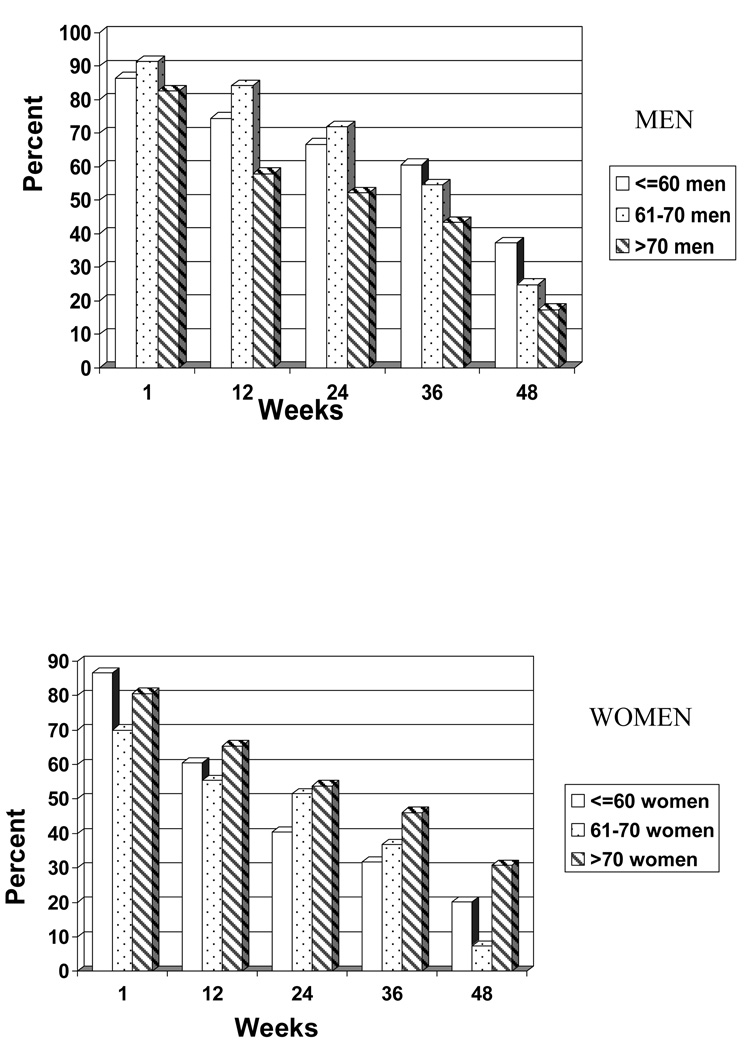
Figure 1 shows the trends in exercise adherence of 3 sessions a week. The percent of women and men that adhered to the guideline at 1, 12, 24, 36 and 48 weeks is displayed. All age groups experienced a downward trend in exercise over time. For the oldest age group (>70), women had higher rates of meeting the exercise guidelines than older men. For both men and women and all age groups, the greatest decline in exercise adherence was between nine and 12 months.
Figure 1.
Percent of Men and Women that Continue to Exercise ≥3 Times a Week by Age Group Over Time
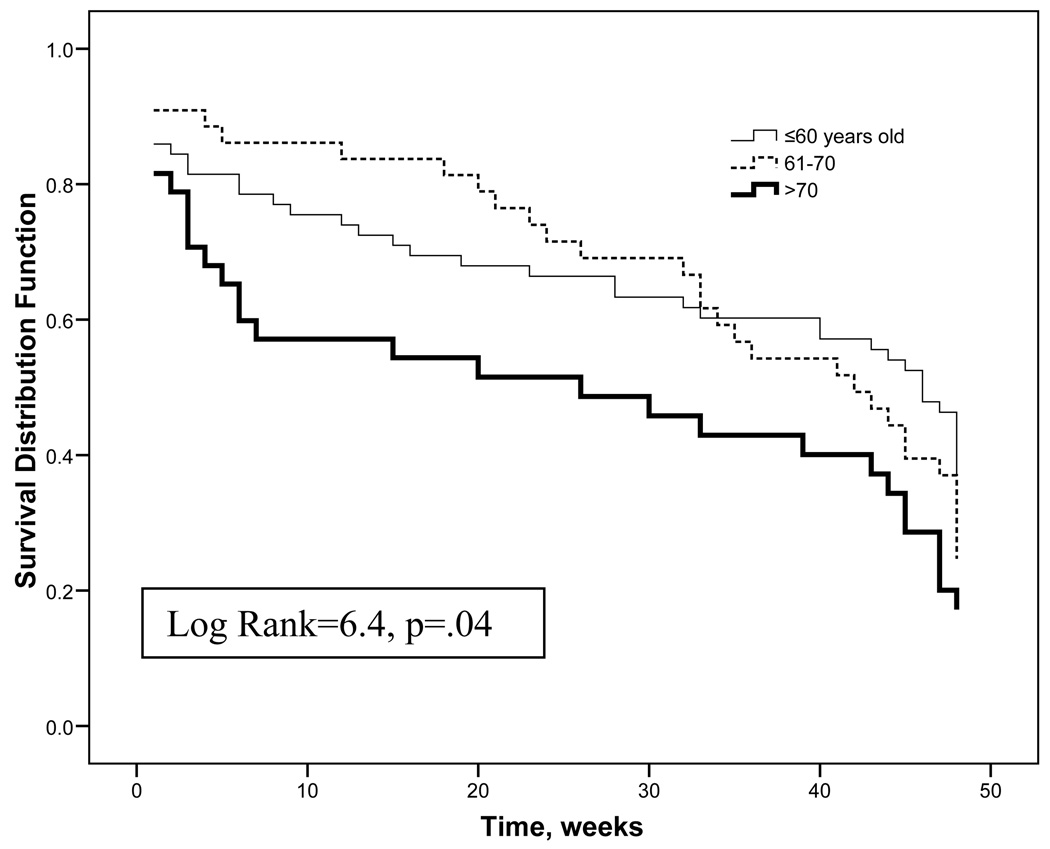
For both men and women, age group comparisons for time to discontinuation of exercise three times a week were examined using KM plots. For women, no significant differences were found among age groups in adherence to exercise in the 48 weeks following a CRP (Log Rank Test = 3.5, p = .18). Significant differences were found for men (Figure 2). Men over 70 years of age stopped exercising sooner than younger men (≤60 X=32.6 weeks; 61–70 X=34.3 weeks; >70 X=24.9 weeks, Log Rank=6.29, p=.04).
Figure 2.
Men only: Time to Discontinuation of Exercise at 3 Times a Week by Age Group
The Cox Proportional Hazards Regression model was used to identify the effect of age while controlling for covariates. The Cox regression results confirm the results of the Kaplan Meir plots. For women, age was not a predictor of exercise; the only significant predictor was race (Wald=11.26, HR=.35, p=.001), indicating that white women continue to exercise after a CRP longer than women of other races. Table 2 displays the Cox regression results for men. Older men were more likely to stop adherence to exercise sooner than younger men even when controlling for all other factors. In addition to age differences in exercise adherence, other covariates were significant (self-efficacy Wald=8.61, HR = .98, p=.003 and depressed mood Wald=11.12, HR 1.04, p=.001). Men with higher self-efficacy were more likely to continue exercise while men reporting a depressed mood were more likely to stop exercise.
Table 2.
Men only: Cox Proportional Hazards Regression Model on the Risk of Discontinuing Adherence to Exercise 3 times a Week Controlling for Covariates
| Variable | Wald χ2 | P value | Hazard Ratio |
95% CI |
|---|---|---|---|---|
| Age | 6.76 | .01 | 1.03 | 1.01 to 1.05 |
| Race | .10 | .76 | .91 | .51 to 1.61 |
| Muscle and joint pain | .68 | .41 | 1.11 | .86 to 1.46 |
| Six-Minute Walk | .20 | .66 | 1.0 | .99 to 1.0 |
| Comorbidity | 1.22 | .27 | .92 | .79 to 1.07 |
| Self-efficacy Barriers | 8.00 | .01 | .98 | .97 to .99 |
| Depressed Mood | 11.08 | .001 | 1.04 | 1.02 to 1.07 |
| Social Support Family | 3.26 | .07 | .98 | .96 to 1.0 |
Hazard ratio is the degree of risk associated with each variable while controlling for all other variables. Ratios less than 1 indicate reduced risk and those above 1 indicate increased risk.
Discussion
Women
The analysis revealed that age group differences in exercise adherence following a cardiac event were gender specific. In contrast to men, age was not a factor in exercise adherence in women. Older women did not exercise less than younger women. Although not statistically significant, there was a trend indicating that older women continued to exercise longer than younger women. This is in contrast to studies of community-dwelling adults in which older women were found to exercise less than younger women (Conn, 1998; Nies & Kershaw, 2002); but consistent with studies of women after a cardiac event and completion of a CRP, in which older women adhered to exercise prescription longer than younger women (Moore et al., 1998). Women having a cardiac event who have completed a CRP may be more functionally fit than older women of the same age in the community and may be more motivated to continue with the exercise routine established during the CRP. In addition, previous studies identified that younger women have more competing work and family obligations than older women and therefore exercise less (Moore et al., 1998).
The only predictor of exercise adherence in women was race. Upon further exploration, it was noted that the age group in which exercise adherence declined the fastest was the youngest group. This group (≤60) had the greatest percentage of African American women (38%). A downward decline in exercise adherence for African American women has been noted in other exercise studies (Crespo et al., 2000; Wilbur et al., 2005). There is a pressing need to understand and develop exercise maintenance strategies that are culturally sensitive and meaningful to African American women.
It was surprising that pain was not related to exercise adherence in women, especially since a large proportion of the women across the age categories reported having arthritis. The measure of pain in this study was investigator developed and it is possible that it did not adequately capture the pain experience for these women. In addition, baseline levels of pain were used as predictors in this study and it is possible that pain scores changed over the course of the year.
Men
Age was a factor in exercise adherence for men. Older men stopped adherence to exercise guidelines sooner than younger men, even when controlling for self-efficacy, depressed mood, comorbidity, physical fitness, and social support. In addition to age, other significant predictors of non-adherence to exercise guidelines were depressed mood and lower self-efficacy. This was consistent with other studies on adherence to exercise after a structured exercise program (Bock et al., 1997; McAuley, 1993). Although there were no significant differences at baseline for self-efficacy among the age groups, at 48 weeks, older men had the lowest level of self-efficacy compared with the other age groups of men. This difference in confidence to exercise among the age categories may indicate that older men had experienced more barriers to exercise compared to younger men. These findings also suggest that screening for depression be done at the completion of a CRP to identify those persons at risk for not adhering to exercise guidelines. Similarly, assessment of self-efficacy to barriers and counseling during a CRP about ways to overcome barriers may help older men to maintain long-term exercise.
Women and Men
There was a downward trend of exercise adherence for all age groups in both men and women over time. At one year, 78% of the participants were not adhering to the exercise guidelines of three sessions a week. This is particularly concerning given that the current guideline recommendation is for exercise five times a week. This low rate of exercise adherence is consistent with other studies that reported that adults have difficulty with maintenance of exercise after completion of a structured exercise program (Bock et al., 1997; McAuley, 1993; Wilbur et al., 2005). More information is needed about the factors influencing maintenance of exercise adherence, as the factors associated with maintenance of exercise are thought to be different than the factors influencing exercise initiation (Rothman, 2000). New models of exercise adherence behavior are needed that explain the underlying mechanisms of transition from exercise initiation to maintenance (Orleans, 2000). The understanding of these CRP transitions (program initiation, program adherence and exercise maintenance) is important, as lifestyle exercise is a dynamic process that requires attention and intervention (Wing, 2000). The CRP environment may be a valuable opportunity to address the dynamic nature of exercise adherence and teach the skills necessary to continue to exercise for life.
Self-efficacy declined over time for both men and women in all age categories. It may be that persons soon after completion of a structured CRP are optimistic and have a unrealistically high confidence regarding their ability to overcome barriers to exercise. As time passes, the reality of the difficulty in adhering to an exercise regimen becomes apparent. This initial overly optimistic outlook has been noted to be a barrier in maintenance in other studies on long-term weight loss in both men and women (Sbrocco et al., 1999).
An unexpected finding of this study was that at 48 weeks following completion of a CRP older women had better adherence to exercise guidelines than older men. This is in contrast to the findings of other studies that demonstrate that women in the general population have lower levels of exercise adherence than men. Participation in a CRP after a cardiac event, therefore, may be especially important for older women as a way to increase lifestyle exercise.
It is interesting to note that although the oldest participants had less fitness and higher comorbidity than the youngest participants, fitness and comorbidity did not contribute to the explanation of non-adherence in men or women. This may be because most people who enter a CRP are generally more physically fit than those who do not participate in a CRP (Dolansky & Moore, 2008). It is also possible that the measurement of physical fitness obtained during the last weeks of a CRP in this study, provided time for all participants to increase their physical fitness levels and thus reduced the differences between age groups.
It is recognized that understanding exercise adherence in this report maybe limitrd by the decision to dichotomize exercise as adherent or not adherent. Further examination of exercise using total amount of exercise and other exercise patterns are reported elsewhere (Moore, et. al., 2006). Another possible limitation of this study is the difficulty of measuring of exercise in field studies. We feel relatively confident in our measure, however, since an objective measure, the Polar Monitor, and two other measures were used to capture lifestyle exercise overtime. Future recommendations include the need for more prospective descriptive studies that examine reasons why people stop adhering to exercise guidelines after completion of a CRP. A National CRP registry that follows participants after a CRP may be a valuable resource for understanding adherence to exercise guidelines. This registry could be web-based and include the tracking of lapses and relapses and collect information related to potential predictors of these situations. Given that only a small percentage of participants adhered to an exercise regimen at one year, intervention studies are needed that consider age and gender issues. Additionally, given the consistent finding in the literature regarding the influence of self-efficacy on exercise, studies that offer booster interventions to enhance self-efficacy to barriers are needed. Other variables to include in studies of exercise adherence are perceived satisfaction with the outcomes of exercise, enjoyment of exercise, and incorporating exercise into daily recreational activities as these factors have been identified as an important in adherence with long-term exercise (Hagberg et al., 2008; Rothman, 2000).
In conclusion, the effect of age on adherence to exercise guidelines after a cardiac event was gender specific. Age was a factor for men but not for women. During the year after participation in a cardiac rehabilitation program, younger men adhered to routine exercise longer than older men. Interventions that impact exercise adherence will assist cardiac patients to continue with exercise for life so that the benefits achieved from participating in a CRP after a cardiac event can be maintained.
Acknowledgements
This study was supported by the NIH, R01-NR04704, Beth Stepanczuk was a Medical Student Training in Aging Research (MSTAR) Program Scholar funded by the American Federation of Aging Research, and Dr. Dolansky was a Multidisciplinary Clinical Research Fellow funded by the KL2RR024990 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR, AFAR or NIH.
Contributor Information
Mary A. Dolansky, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, Ohio.
Beth Stepanczuk, Case Western Reserve University, Cleveland, Ohio.
Jacqueline M. Charvat, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, Ohio.
Shirley M. Moore, Edward J. & Louise Mellen Professor of Nursing, Associate Dean for Research, Frances Payne Bolton School of Nursing, Case Western Reserve University, Cleveland, Ohio.
Reference List
- Ades PA. Cardiac rehabilitation in older coronary patients. Journal of the American Geriatrics Society. 1999;47:98–105. doi: 10.1111/j.1532-5415.1999.tb01909.x. [DOI] [PubMed] [Google Scholar]
- Ades PA, Maloney A, Savage P, Carhart RL., Jr Determinants of physical functioning in coronary patients: response to cardiac rehabilitation. Archives Internal Medicine. 1999;159:2357–2360. doi: 10.1001/archinte.159.19.2357. [DOI] [PubMed] [Google Scholar]
- Ades PA, Savage PD, Tischler MD, Poehlman ET, Dee J, Niggel J. Determinants of disability in older coronary patients. American Heart Journal. 2002;143:151–156. doi: 10.1067/mhj.2002.119379. [DOI] [PubMed] [Google Scholar]
- Ades PA, Waldmann ML, Polk DM, Coflesky JT. Predictors of cardiac rehabilitation participation in older coronary patients. Archives of Internal Medicine. 1992a;152:1033–1035. [PubMed] [Google Scholar]
- Ades PA, Waldmann ML, Polk DM, Coflesky JT. Referral patterns and exercise response in the rehabilitation of female coronary patients aged greater than or equal to 62 years. American Journal of Cardiology. 1992b;69:1422–1425. doi: 10.1016/0002-9149(92)90894-5. [DOI] [PubMed] [Google Scholar]
- American Association of Cardiovascular and Pulmonary Rehabilitation. Guidelines for Cardiac Rehabilitation and Secondary Prevention Programs. 4th ed. Champaign IL: Human Kinetics; 2004. [Google Scholar]
- Balady GJ, Ades PA, Comoss P, Limacher M, Pina IL, Southard D, et al. Core components of cardiac rehabilitation/secondary prevention programs: A statement for healthcare professionals from the American Heart Association and the American Association of Cardiovascular and Pulmonary Rehabilitation Writing Group. Circulation. 2000;102:1069–1073. doi: 10.1161/01.cir.102.9.1069. [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Carney RM, Huber M, Saab PG, Burg MM, et al. Exercise, depression, and mortality after myocardial infarction in the ENRICHD trial. Medicine and Science in Sports Exercise. 2004;36:746–755. doi: 10.1249/01.mss.0000125997.63493.13. [DOI] [PubMed] [Google Scholar]
- Bock BC, Albrecht AE, Traficante RM, Clark MM, Pinto BM, Tilkemeier P, et al. Predictors of exercise adherence following participation in a cardiac rehabilitation program. International Journal of Behavioral Medicine. 1997;4:60–75. doi: 10.1207/s15327558ijbm0401_4. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Receipt of outpatient cardiac rehabilitation among heart attack survivors-United Sates, 2003. MMWR Morbidity and Mortality Weekly Report. 2008;57:89–94. [PubMed] [Google Scholar]
- Clark DO. Physical activity and its correlates among urban primary care patients aged 55 years or older. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1999;54:S41–S48. doi: 10.1093/geronb/54b.1.s41. [DOI] [PubMed] [Google Scholar]
- Conn VS. Older adults and exercise: path analysis of self-efficacy related constructs. Nursing Research. 1998;47:180–189. doi: 10.1097/00006199-199805000-00009. [DOI] [PubMed] [Google Scholar]
- Cresco CJ, Smith E, Andersen RE, Carter-Pokras O, Ainsworth BE. Race/ethnicity, social class and their relation to physical inactivity during leisure time: results from the Third National Health and Nutrition Examination Survey, 1988–1994. American Journal of Preventive Medicine. 2000;18:46–53. doi: 10.1016/s0749-3797(99)00105-1. [DOI] [PubMed] [Google Scholar]
- Dolansky MA, Moore SM. Effect of cardiac rehabilitation on older adults’ lower extremity functioning following CABS. Circulation. 2000;102(18) Supplement II:822. [Google Scholar]
- Dolansky MA, Moore SM. Older adults' use of post-acute and cardiac rehabilitation services after hospitalization for a cardiac event. Rehabilitation Nursing. 2008;33(2):75–83. doi: 10.1002/j.2048-7940.2008.tb00207.x. [DOI] [PubMed] [Google Scholar]
- Ewart CK. A Social Problem-Solving Approach to Behavior Change in Coronary Heart Disease. In: Shumaker SA, editor. The Handbook of Health Behavior Change. New York: Springer; 1990. [Google Scholar]
- Gunstad J, MacGregor KL, Paul RH, Poppas A, Jefferson AL, Todaro JF, et al. Cardiac rehabilitation improves cognitive performance in older adults with cardiovascular disease. Journal of Cardiopulminary Rehabilitation. 2005;25:173–176. doi: 10.1097/00008483-200505000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagberg LA, Lindahl B, Nyberg L, Hellenius ML. Importance of enjoyment when promoting physical exercise. Scandinavian Journal of Medicine and Science in Sports. 2008 doi: 10.1111/j.1600-0838.2008.00844.x. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Medicine and Science in Sports Exercise. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- Harlan WR, III, Sandler SA, Lee KL, Lam LC, Mark DB. Importance of baseline functional and socioeconomic factors for participation in cardiac rehabilitation. American Journal of Cardiology. 1995;76:36–39. doi: 10.1016/s0002-9149(99)80797-8. [DOI] [PubMed] [Google Scholar]
- Husak L, Krumholz HM, Lin ZQ, Kasl SV, Mattera JA, Roumanis SA, et al. Social support as a predictor of participation in cardiac rehabilitation after coronary artery bypass graft surgery. Journal of Cardiopulmonary Rehabilitation. 2004;24:19–26. doi: 10.1097/00008483-200401000-00005. [DOI] [PubMed] [Google Scholar]
- Jaeger AA, Hlatky MA, Paul SM, Gortner SR. Functional capacity after cardiac surgery in elderly patients. Journal of the American College of Cardiology. 1994;24:104–108. doi: 10.1016/0735-1097(94)90548-7. [DOI] [PubMed] [Google Scholar]
- Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane.Database.Syst.Rev. 2000 doi: 10.1002/14651858.CD001800. CD001800. [DOI] [PubMed] [Google Scholar]
- Jolliffe JA, Rees K, Taylor RS, Thompson D, Oldridge N, Ebrahim S. Exercise-based rehabilitation for coronary heart disease. Cochrane Database of Systematic Reviews. 2001 doi: 10.1002/14651858.CD001800. CD001800. [DOI] [PubMed] [Google Scholar]
- Lee YS. Gender differences in physical activity and walking among older adults. Journal of Women and Aging. 2005;17:55–70. doi: 10.1300/J074v17n01_05. [DOI] [PubMed] [Google Scholar]
- Lieberman L, Meana M, Stewart D. Cardiac rehabilitation: gender differences in factors influencing participation. Journal of Womens Health. 1998;7:717–723. doi: 10.1089/jwh.1998.7.717. [DOI] [PubMed] [Google Scholar]
- McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. Journal of Behavioral Medicine. 1993;16:103–113. doi: 10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- McAuley E, Katula J, Mihalko SL, Blissmer B, Duncan TE, Pena M, et al. Mode of physical activity and self-efficacy in older adults: a latent growth curve analysis. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 1999;54:283–292. doi: 10.1093/geronb/54b.5.p283. [DOI] [PubMed] [Google Scholar]
- McAuley E, Lox C, Duncan TE. Long-term maintenance of exercise, self-efficacy, and physiological change in older adults. J.Gerontol. 1993;48:218–224. doi: 10.1093/geronj/48.4.p218. [DOI] [PubMed] [Google Scholar]
- McNair D, Lorr M, Droppleman L. Manual of Profile of Mood State. SanDiego, CA: Educational and Industrial Test Source; 1981. [Google Scholar]
- Milani RV, Littman AB, Lavie CJ. Depressive symptoms predict functional improvement following cardiac rehabilitation and exercise program. Journal of Cardiopulmonary Rehabilitation. 1993;13:406–411. [Google Scholar]
- Milner C. Older Americans 2008: Key Indicators of Well-Being, Federal Interagency Forum on Aging-Related Statistics. Vancouver, British Columbia, Canada: International Council on Active Aging; 2008. [Google Scholar]
- Moore SM. The effects of a discharge information intervention on recovery outcomes following coronary artery bypass surgery. International Journal of Nursing Studies. 1996;33:181–189. doi: 10.1016/0020-7489(95)00054-2. [DOI] [PubMed] [Google Scholar]
- Moore SM, Charvat JM, Gordon NH, Pashkow F, Ribisl P, Roberts BL. Effects of a CHANGE intervention to increase exercise maintenance following cardiac events. Annals of Behavioral Medicine. 2006;31:53–62. doi: 10.1207/s15324796abm3101_9. [DOI] [PubMed] [Google Scholar]
- Moore SM, Dolansky MA. Randomized trial of a home recovery intervention following coronary artery bypass surgery. Research in Nursing and Health. 2001;24:93–104. doi: 10.1002/nur.1012. [DOI] [PubMed] [Google Scholar]
- Moore SM, Dolansky MA, Ruland CM, Pashkow FJ, Blackburn GG. Predictors of women's exercise maintenance after cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation. 2003;23:40–49. doi: 10.1097/00008483-200301000-00008. [DOI] [PubMed] [Google Scholar]
- Moore SM, Ruland CM, Pashkow FJ, Blackburn GG. Women's patterns of exercise following cardiac rehabilitation. Nursing Research. 1998;47:318–324. doi: 10.1097/00006199-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Newson RS, Kemps EB. Factors that promote and prevent exercise engagement in older adults. Journal of Aging and Health. 2007;19:470–481. doi: 10.1177/0898264307300169. [DOI] [PubMed] [Google Scholar]
- Nies MA, Kershaw TC. Psychosocial and environmental influences on physical activity and health outcomes in sedentary women. Journal of Nursing Scholarship. 2002;34:243–249. doi: 10.1111/j.1547-5069.2002.00243.x. [DOI] [PubMed] [Google Scholar]
- O'Brien Cousins S. Exercise, Aging & Health: Overcoming Barriers to an Active Old Age. Philadelphia: Taylor & Francis; 1998. [Google Scholar]
- Oman RF, King AC. Predicting the adoption and maintenance of exercise participation using self-efficacy and previous exercise participation rates. American Journal of Health Promotion. 1998;12:154–161. doi: 10.4278/0890-1171-12.3.154. [DOI] [PubMed] [Google Scholar]
- Orleans CT. Promoting the maintenance of health behavior change: recommendations for the next generation of research and practice. Health Psychol. 2000;19:76–83. doi: 10.1037/0278-6133.19.suppl1.76. [DOI] [PubMed] [Google Scholar]
- Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychology. 2000;19:64–69. doi: 10.1037/0278-6133.19.suppl1.64. [DOI] [PubMed] [Google Scholar]
- Sachdev M, Sun JL, Tsiatis AA, Nelson CL, Mark DB, Jollis JG. The prognostic importance of comorbidity for mortality in patients with stable coronary artery disease. Journal of the American College of Cardiology. 2004;43:576–582. doi: 10.1016/j.jacc.2003.10.031. [DOI] [PubMed] [Google Scholar]
- Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR. The development of scales to measure social support for diet and exercise behaviors. Preventive Medicine. 1987;16:825–836. doi: 10.1016/0091-7435(87)90022-3. [DOI] [PubMed] [Google Scholar]
- Sbrocco T, Nedegaard RC, Stone JM, Lewis EL. Behavioral choice treatment promotes continuing weight loss: preliminary results of a cognitive-behavioral decision-based treatment for obesity. Journal of Consulting and Clinical Psychology. 1999;67:260–266. doi: 10.1037//0022-006x.67.2.260. [DOI] [PubMed] [Google Scholar]
- Schoenberg NE, Kim H, Edwards W, Fleming ST. Burden of Common Multiple-Morbidity Constellations on Out-of-Pocket Medical Expenditures Among Older Adults. The Gerontologist. 2007;47:423–437. doi: 10.1093/geront/47.4.423. [DOI] [PubMed] [Google Scholar]
- Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. American Journal of Medicine. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Verderber A, Castelfranco AM, Nishioka D, Johnson KG. Cardiovascular risk factors and cardiac surgery outcomes in a multiethnic sample of men and women. American Journal of Critical Care. 1999;8:140–148. [PubMed] [Google Scholar]
- Wenger NK, Froelicher ES, Smith LK. Cardiac Rehabilitation. Clinical Practice Guideline #17. Rockville, MD: U.S. Dept of Health & Human Services, Public Health Service, Agency for Health Care Policy & Research and the National Heart, Blood & Lung Institute; 1995. AHCPR # 96-0672. [PubMed] [Google Scholar]
- Wilbur J, Vassalo A, Chandler P, McDevitt J, Miller AM. Midlife women's adherence to home-based walking during maintenance. Nurs.Res. 2005;54:33–40. doi: 10.1097/00006199-200501000-00005. [DOI] [PubMed] [Google Scholar]
- Wing RR. Cross-cutting themes in maintenance of behavior change. Health Psychology. 2000;19:84–88. doi: 10.1037/0278-6133.19.suppl1.84. [DOI] [PubMed] [Google Scholar]