Abstract
What can be done to build effective weight loss solutions for the 1.5 billion people with obesity? It is self-evident that no one good solution exists for people who are overweight or obese, otherwise it would have been applied across the people who need it worldwide. There is, therefore, an urgent need for approaches that will afford weight loss; what is more, such approaches need to be scalable. For that reason, it is attractive to consider electronic platforms as an avenue for scalable weight loss solutions. Such platforms often do not require substantial investments but rather the integration of pre-existing off-the-shelf components. In this article we explore the concepts and design challenges for electronic platforms that precipitate weight loss.
Keywords: accelerometer, energy expenditure, food intake, food storage, physical activity, weight loss
The urgency to address the obesity epidemic is immediate not only because of the health and physical costs associated with obesity, but also because of the unprecedented rates of obesity in children [1].
It is clear that no one good solution exists for obesity [2], otherwise it would have been applied worldwide across the 1.5 billion people who need it. There is, therefore, a pressing need for scalable approaches that will afford weight loss. For that reason, electronic platforms are an attractive avenue for scalable weight loss solutions [3].
This approach is particularly attractive as the last two decades have seen the ubiquitous deployment of desk-based and hand-held electronic devices [4]. Although these electronic devices provide opportunities for weight loss solutions, one needs to recognize that concomitantly, their use has been associated with sedentariness, low energy expenditure and obesity [5].
The goal of this article is to explain how electronic platforms can be deployed for successful weight loss.
Science-based foundation
When considering electronic platforms for weight loss, one needs to identify the conceptual framework around which such platforms will perform; in this case based upon core physiological concepts.
Weight loss cannot occur unless a person enters negative energy balance, whereby energy stores are depleted as a result of energy intake being less than energy expenditure [6]. Thus, there are three core areas that can be addressed with electronics namely energy intake, energy expenditure and energy storage [7–9].
Bearing these core principles in mind, the application of electronic platforms for weight loss can be simplified.
With respect to achieving negative energy balance, electronic devices can be used as sensing technologies, behavior effectors and integration technologies.
Sensing technologies
A variety of sensing approaches can be used to assess and quantify energy intake, energy expenditure and energy storage.
Food intake
Food intake can be assessed either prospectively or retrospectively; the former techniques are more accurate and precise than the latter. However, prospective approaches are more cumbersome, inconvenient and expensive.
Prospective data collection techniques include: the weighed inventory method, where subjects weigh all of their food items for 7 days; the preweighed meal method, where a metabolic kitchen provides subjects with preweighed foods (and measures uneaten food); the premixed liquid formula method, where a subject receives their total energy needs using formulated feeds; the duplicate meal technique, where the subject prepares duplicate meals and stores the duplicate food for analysis; and the standard nonweighed method, where subjects describe the types and quantities of food eaten, usually in notebooks [10,11].
Retrospective assessments are based upon subjects recalling the foods eaten and so the error inherent in recalling the nature and quantity of all foods consumed over a specified period of time is great. Retrospective assessments of dietary intake include: the dietary history method, whereby subjects recall foods eaten, for example, ‘over the last week’; the 24-h recall method where subjects recall, ideally with an interviewer, the food eaten on the previous day [12]; and food frequency assessments, which are invariably conducted using questionnaires [13]. Overall, recall techniques are of limited accuracy and precision as people often cannot accurately recollect either the types or the quantities of foods and beverages consumed [14,15].
Finally, there is an additional source of error in assessing food intake because food tables introduce assessment error compared with chemical analysis, which is the gold standard [16].
Overall, therefore, it can be understood that assessing food intake is problematic. Nonetheless, novel technologies have been deployed/attempted to help assess food intake.
It was an obvious step to deploy such questionnaires to computers and personal digital assistant (PDA) devices [17,18], but this does not overcome the inherent inaccuracies of the approach [19,20]. Other electronic approaches have been used to quantify food intake, for example, the use of cell phones to photograph food intake and the use of automated computer-linked weighing scales [19–21]. These approaches universally do not get over the major hurdles of assessing food intake, which are correctly identifying the nature of the food, correctly identifying the quantity consumed of that food, correctly analyzing the nutritional composition of the food consumed and, finally, ensuring that the data-gathering modality does not interfere with food intake itself.
Other electronic approaches could be used for food intake sensing, such as barcode-reading refrigerators [22,23], self-sensing food vending machines [24], weight sensing and photograph-capturing plates, devices inserted into the mouth to detect chewing and food bolus [25] and systems for cataloging foods stored and removed from storage cupboards [26–28]. There are other broader approaches, such as accessing credit cards to determine food purchase patterns and monitoring a person while attending restaurants [26,29].
Although such new technologies are enticing, there is no evidence to suggest that accuracy and precision improve. In fact, caution is recommended in deploying such approaches until validation studies and an assessment of the sustainability of the methodology have been completed.
Energy expenditure
A person's energy expenditure can be categorized as that associated with either the basal state (basal metabolic rate), food intake consumption and digestion (thermic affect of food), or activity (either exercise or nonexercise activity thermogenesis). Technologies exist for measuring all three components [30], although the emphasis has been on measuring basal metabolic rate and the energy expenditure of activity because the thermic affect of food is small and does not vary greatly between different people [31].
Basal metabolic rate is almost invariably measured using indirect calorimetry, whereby either oxygen intake or carbon dioxide production is measured [30]. The sophistication of the calorimeters ranges from small, cheap, somewhat insensitive or inaccurate hand-held devices through to elaborate, highly accurate and highly precise calorimeters. The former are applicable for broad-based dissemination even to the public and possibly to gyms and offices, for example, while the latter are generally only applicable to the research setting. Most often, basal metabolic rate is predicted to within approximately 10% of the actual value using equations and these are delivered in an electronic format [32].
In the past, daily physical activity has been poorly assessed using questionnaires. The wide availability of accelerometers (ubiquitously micro–electro–mechanical systems [MEMS] technology) [33] has enabled daily physical activity to be measured accurately many times per second for many days [34]. Such devices are revolutionizing the ability of individuals to assess their own daily activity, daily activity patterns and predicted daily activity energy expenditure. Not only are these devices available to researchers but models have been built for broad-based dissemination and self-monitoring. Furthermore, such devices have been integrated into behavioral reminders and linked to computer-based systems for weight loss.
However, often overlooked are the limitations of deploying such technologies outside of the laboratory setting. For example, in one study that included 21 people wearing an accelerometer, 443 h of data were lost from a belt-worn triaxial accelerometer due to technical fault, participant forgetfulness, social stigmatism, unrecordable activity such as swimming, clip breakage, discomfort and fear of damaging the devices [35]. There are also other important caveats: the context of the activity is ill defined, attachment is critical, correct orientation is important, individual validation data are often not obtained, the analysis equations are variable and often not validated (certainly in the free-living state) and many activities cannot theoretically be captured, for example, a belt-worn accelerometer cannot detect arm movement.
Since the 1960s, the doubly labeled water technique has enabled researchers to validate such approaches for measuring total daily energy expenditure [36,37]. This technique involves the consumption of stable isotopes of water and the measurement of urine elimination rates.
As a consequence of reasonable predictive equations of basal metabolic rate and valid equipment for measuring it, as well as the newfound availability of accelerometers plus the capability of validating the approaches, it has become possible to assess energy expenditure accurately, principally as basal metabolic rate predicted from an equation coupled to accelerometer data.
Energy storage
Within the research environment, dual x-ray absorptiometry, MRI and computed tomography (CT) have enabled body composition to be measured accurately and precisely [38–40]. With the development of commercial systems for air displacement plethysmography [41], it has been possible to measure body composition in gyms and offices quite accurately and precisely. The technique of bioimpedance relies on the notion that body fat does not contain water and so the electrical resistance of the body coupled to its weight can enable a determination of fat-free mass-enhanced body composition [42]. Although such devices are commercially available even for the home, bioimpedance does not provide accurate and precise information in general for individuals but is an example of a broadly disseminated technique for measuring body composition.
Finally, there is important literature on the variability associated with individuals self-measuring their body weight [43,44]. This is not only because of the variable accuracy of weighing scales but also because people often weigh themselves with different amounts of clothing at different times of the day and, particularly for premenopausal women, at different times of the month. Nonetheless, the worldwide availability of inexpensive weighing scales that can be connected to computers, demonstrates that it is entirely possible to disseminate worldwide techniques for assessing body composition.
Behavioral effector technologies
Although electronic sensors can be used to assess and measure components of energy balance, electronic platforms can also be used to impact or change the components of energy balance.
Food intake
Simple electronic effectors of food intake include prompts, for example, to change food selections and quantities. These can be delivered through electronic means, namely computers, PDA-like devices and cell phones [22,23]. However, there has been little evidence that these are effective at impacting food choices. Similar electronic platforms can be used to prescribe nutritional intake, for example, as daily menus. Devices could potentially be used to screen shopping [45,46] and make recommendations regarding eating practices as the eater eats (e.g., using an eye camera either attached to a glasses frame or even implanted in the skin or mouth) [47,48].
It would be possible to directly create behavioral cue systems, such as an individual receiving an intra-oral or skin shock when consuming an ill-advised food, or a food container that closes once a certain amount of food has been eaten [49,50]. However, such endeavors require intensive ethical scrutiny, just as with electric shock therapy in psychiatric care and invasive gastric bypass surgery. Although no such device or devices have been formally evaluated to achieve sustained weight loss, their inclusion in a weight loss system is attractive.
Similarly, novel approaches could be invented for positive reinforcement for improved food intake and weight loss [51–53]. For example, an automated fridge detector system identifies that a family has switched to skimmed milk and increased their fruit use by 20%. As a positive reinforcer (i.e., reward), the family then receives coupons for a visit to a gym, for example. In another example, patients were provided with financial incentives for weight loss [53]. Other such positive reinforcement systems could be invented, tested and validated.
Energy expenditure
There has been tremendous interest and effort expended regarding the promoting of physical activity. Accelerometers and step counters are widely available and have been deployed, for example, in people's shoes and on their clothing, to not only measure but also help modulate physical activity and, thus, energy expenditure [33,54,55]. Gaming has been widely publicized and studied as a means for promoting activity, whereby the gaming environment becomes an active one replacing a sedentary one [56]. Games such as Dance Dance Revolution™ and the Wii™ are examples of activity-promoting gaming and games associated with proven increases in energy expenditure compared with traditional sedentary modes [57,58]. Interestingly and importantly, such approaches have yet to be proven to be associated with sustained and long-term changes in weight loss, although for some individuals this clearly does occur [59].
There are several other technologies that can be used to promote daily physical activity, including global positioning system (GPS) activity-promoting systems [60], radiofrequency tagging of physical spaces and self-sensing exercise machines and play equipment. Interestingly, such technologies can be targeted for specific populations, such as the elderly [61,62] or ethnic groups [63].
For example, there has recently been renewed interest in the potential association of brown fat activation with negative energy balance and possibly with weight loss. Therefore, it would be theoretically conceivable that an implantable pump, for example, might deliver either genetic or pharmaceutical materials to activate brown fat (or even change white fat to brown fat), and thus increase energy expenditure and potentially precipitate weight loss [64]. Such devices could be integrated into a cell phone and could be activated by either the patient themselves or their healthcare provider. Any such manipulations would need careful evaluation.
Energy stores
One might think that electronic platforms could not be used to directly modulate energy stores. However, the aforementioned example argues against this. It is conceivable that electronic pumps could be inserted into body fat stores to help deplete them or deliver pharmaceuticals or genetic materials [65–67], impacting the capacity of the adipocyte to store fat and potentially enhancing the release of stored lipid. Essentially, one could contemplate portable real-time liposuction devices that directly impact energy stores.
Integration technologies
One of the greatest difficulties in developing and deploying mass-scalable weight loss solutions – whether they are electronic or not – has been the issue of integration.
In order to design effective integration platforms a crucial physiological notion needs to be born in mind. It is possible to impact body weight by affecting only a single component of the energy balance equation. This is because the end variable (or the outcome) of a weight loss electronic platform is body weight (or body fat). Thus, for example, energy intake could be modulated using the electronic platform and activity neither sensed nor effected. In such a scenario, if body weight remained unchanged, the behavioral effector technology could simply continue to decrease energy intake until weight declined. A similar philosophy can be used with those approaches focused on energy expenditure (especially physical activity). The issue regarding increasing physical activity is slightly more complex because increasing physical activity is principally important at low levels for helping a patient maintain lost weight [68,69]. However, when physical activity increases approximately 2000 kcal/week, this is associated with active weight loss. Such technologies could incorporate this information.
However, the notion of impacting only a single component of the energy balance equation is ill-advised. For example, a system devoted to decreased dietary intake alone will overlook potential compensatory changes in energy expenditure. Similarly, a system focused entirely on physical activity, whereby physical activity is continuously increased until weight loss occurs, may overlook the fact that food intake could increase in response, so that weight loss does not occur. Thus, it is recommended that electronic platforms for weight loss are based upon sound physiological principles, and incorporate both food intake and energetic modulators.
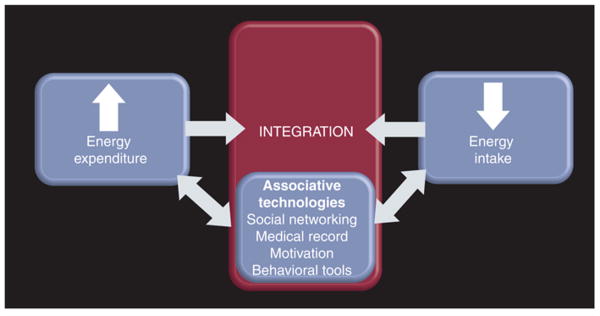
However, the integration element can be afforded greater complexity than only including components of energy balance. For example, data suggest that social networking is important in obesity and so such systems could be integrated into a comprehensive weight loss platform [70]. Similarly, a broad-based electronic platform could integrate knowledge delivery either as informationals (e.g., a video stream about cholesterol management or a real-time yoga lesson streamed to the platform) [71]. Thus, an integrated and widespread electronic platform (Figure 1) affords opportunities beyond adjusting physiological elements to affect weight loss successfully.
Figure 1. Design of the technologies to precipitate weight loss.
Another advantage of such platforms is that the collective human data can be sieved (e.g., favorite activities for a certain age group in a certain region) and also integrated with other commercial entities, such as credit card database mining [29], in order to determine the type of bicycle most popular for people with obesity. Another crucial near-term priority will be integration of such a platform with the medical record [72–76], especially since so many health variables are obesity-linked: diabetes, hyperlipidemia, cardiovascular disease, sleep disorders, degenerative arthritis, cancer and hypertension [77]. Overall, the opportunities for integration are broad once issues such as confidential data transfer and standardized protocols for identification-protection have been devised and agreed upon.
Noting the variable complexity of integrating the electronic components for a mass-scalable weight loss solution, a note of caution is important. Without evaluating such systems in both short- and long-term efficacy trials the efforts will be of little consequence. It will be crucial for national and international success that carefully conducted studies confirm the veracity of the system.
Expert commentary & five-year view
The principal weakness in sensing energy balance is the energy intake component. It is now possible to accurately assess energy expenditure in free living people, and the ability to measure body weight has become a reasonable surrogate for body composition.
The notion of building electronic devices to precipitate weight loss seems attractive, especially noting the scope of the problem and the wide availability of electronics. What is interesting is that the opportunity afforded by the ubiquitous available electronics and a broadening understanding of the social influences on obesity, electronic platforms will need to deliver more than energy balance modulation alone. For example, it is entirely feasible, even today, to incorporate social networking into an energy balance portable electronic device so that a person trying to increase their physical activity can easily and immediately locate a partner for tennis or a ‘walking buddy’. Similarly, a person trying to choose effective recipes to help them reduce fat content can easily browse cookery options on a website streaming to their telephone.
However, the opportunities for portable electronic platforms are far more sophisticated than this. For example, a person can participate in remote yoga classes through the internet, can receive confidential psychological counseling through an electronic webbased counseling services and can even receive physician evaluation and treatment through electronic consultation.
It is anticipated that in the near-term, comprehensive, integrated weight loss platforms can be deployed that not only evaluate energy intake, energy expenditure and energy stores, but will also be able to manipulate these variables, as well as integrate the user with other social, educational and therapeutic opportunities.
As systems are developed, it will be necessary to apply stringent efficacy criteria to quantify and compare success.
With the ubiquitous problem of overweight and obesity across the world, it is important to consider the worldwide availability of portable electronics. Interestingly, such technologies and approaches are potentially of value to the very poor. There has been wide-spread recognition that cell phones, for example, can be used for health promotion in people of low socioeconomic status, such as crop selling in sub-Saharan Africa [78,79]. It is hoped that portable electronic devices can be developed, tested and deployed, and that carefully integrated systems will help end obesity.
Key issues.
1.5 billion people worldwide are overweight or obese.
Weight loss cannot occur unless a person enters negative energy balance, whereby energy stores are depleted as a result of energy intake being less than energy expenditure.
There are three core areas that can be addressed with electronics that would allow for a change in energy balance, namely energy intake, energy expenditure and energy storage.
Electronic devices can be used as sensing technologies, behavioral effector technologies and integration technologies to achieve negative energy balance.
It is recommended that all electronic platforms for weight loss are based upon sound physiological principles and incorporate both food intake and energetic modulators.
Electronic platforms for weight loss cannot be the single solution to weight loss. Assessing covariables, societal factors and other behavioral drivers is mandatory.
Integrated electronic platforms are worthy of research and resource allocation because it is likely that they may assist with weight loss in a scalable cost-effective fashion.
In light of the magnitude of the obesity epidemic and the economic climate, cost-effective, mass–scalable integrated, electronic weight loss solutions must be urgently developed and tested.
Acknowledgments
This paper was supported by grants DK63226, DK66270, DK50456 (Minnesota Obesity Center) and Grant Number 1 UL1 RR024150 from the National Center for Research Resources (NCRR), a component of the NIH, and the NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR, NIH or Mayo Clinic. James A Levine provides gratis scientific advice to Muve Incorporated, in which Mayo Clinic owns equity. The Mayo Clinic and/or James A Levine, may, in future derive royalties from this relationship. Muve Inc. provides wellness solutions to individuals and companies. The technologies and approaches used by Muve are not described in this manuscript.
Footnotes
Financial & competing interest disclosure: The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
No writing assistance was utilized in the production of this manuscript.
- National Center for Research Resources www.ncrr.nih.gov
- Reengineering the Clinical Research Enterprise http://nihroadmap.nih.gov
Contributor Information
Shelly K McCrady-Spitzer, Endocrine Research Unit, Mayo Clinic, Rochester, MN 55905, USA.
James A Levine, Endocrine Research Unit, 5–194 Joseph Mayo Clinic, 200 First Street, SW Rochester, MN 55905, USA, Tel: +1 507 284 7636, Fax:+1 507 255 4828, levine.james@mayo.edu.
References
- 1.James WP. The epidemiology of obesity: the size of the problem. J Intern Med. 2008;263(4):336–352. doi: 10.1111/j.1365-2796.2008.01922.x. [DOI] [PubMed] [Google Scholar]
- 2.Ross R, Bradshaw AJ. The future of obesity reduction: beyond weight loss. Nat Rev Endocrinol. 2009;5(6):319–325. doi: 10.1038/nrendo.2009.78. [DOI] [PubMed] [Google Scholar]
- 3.Finegood DT, Karanfil O, Matteson CL. Getting from analysis to action: framing obesity research, policy and practice with a solution-oriented complex systems lens. Healthc Pap. 2008;9(1):36–41. doi: 10.12927/hcpap.2008.20184. discussion 62–67. [DOI] [PubMed] [Google Scholar]
- 4.Capon AG. The way we live in our cities. Med J Aust. 2007;187(11–12):658–661. doi: 10.5694/j.1326-5377.2007.tb01465.x. [DOI] [PubMed] [Google Scholar]
- 5.McCrady SK, Levine JA. Sedentariness at work: how much do we really sit? Obesity (Silver Spring) 2009;17(11):2103–2105. doi: 10.1038/oby.2009.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Flier JS. Obesity wars: molecular progress confronts an expanding epidemic. Cell. 2004;116(2):337–350. doi: 10.1016/s0092-8674(03)01081-x. [DOI] [PubMed] [Google Scholar]
- 7.Pannemans DL, Westerterp KR. Estimation of energy intake to feed subjects at energy balance as verified with doubly labelled water: a study in the elderly. Eur J Clin Nutr. 1993;47(7):490–496. [PubMed] [Google Scholar]
- 8.Pannemans DL, Westerterp KR. Energy expenditure, physical activity and basal metabolic rate of elderly subjects. Br J Nutr. 1995;73(4):571–581. doi: 10.1079/bjn19950059. [DOI] [PubMed] [Google Scholar]
- 9.Rothwell NJ, Stock MJ. Regulation of energy balance. Annu Rev Nutr. 1981;1:235–256. doi: 10.1146/annurev.nu.01.070181.001315. [DOI] [PubMed] [Google Scholar]
- 10.Marr JW. Dietary survey methods: individual and group aspects. Proc R Soc Med. 1973;66(7):639–641. doi: 10.1177/003591577306600718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marr JW, Heady JA. Within- and between-person variation in dietary surveys: number of days needed to classify individuals. Hum Nutr Appl Nutr. 1986;40(5):347–364. [PubMed] [Google Scholar]
- 12.Weetman AP. Graves' disease. N Engl J Med. 2000;343(17):1236–1248. doi: 10.1056/NEJM200010263431707. [DOI] [PubMed] [Google Scholar]
- 13.Mahabir S, Baer DJ, Giffen C, et al. Calorie intake misreporting by diet record and food frequency questionnaire compared to doubly labeled water among postmenopausal women. Eur J Clin Nutr. 2006;60(4):561–565. doi: 10.1038/sj.ejcn.1602359. [DOI] [PubMed] [Google Scholar]
- 14.Fyfe CL, Stewart J, Murison SD, et al. Evaluating energy intake measurement in free-living subjects: when to record and for how long? Public Health Nutr. 2010;13(2):172–180. doi: 10.1017/S1368980009991443. [DOI] [PubMed] [Google Scholar]
- 15.Schembre S, Greene G, Melanson K. Development and validation of a weightrelated eating questionnaire. Eat Behav. 2009;10(2):119–124. doi: 10.1016/j.eatbeh.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 16.Norgan NG, Durnin JV. The effect of 6 weeks of overfeeding on the body weight, body composition, and energy metabolism of young men. Am J Clin Nutr. 1980;33(5):978–988. doi: 10.1093/ajcn/33.5.978. [DOI] [PubMed] [Google Scholar]
- 17.Fowles ER, Gentry B. The feasibility of personal digital assistants (PDAs) to collect dietary intake data in low-income pregnant women. J Nutr Educ Behav. 2008;40(6):374–377. doi: 10.1016/j.jneb.2007.08.015. [DOI] [PubMed] [Google Scholar]
- 18.Beasley JM, Riley WT, Davis A, Singh J. Evaluation of a PDA-based dietary assessment and intervention program: a randomized controlled trial. J Am Coll Nutr. 2008;27(2):280–286. doi: 10.1080/07315724.2008.10719701. [DOI] [PubMed] [Google Scholar]
- 19.Ngo J, Engelen A, Molag M, Roesle J, Garcia-Segovia P, Serra-Majem L. A review of the use of information and communication technologies for dietary assessment. Br J Nutr. 2009;101(Suppl 2):S102–S112. doi: 10.1017/S0007114509990638. [DOI] [PubMed] [Google Scholar]
- 20.Fukuo W, Yoshiuchi K, Ohashi K, et al. Development of a hand-held personal digital assistant-based food diary with food photographs for Japanese subjects. J Am Diet Assoc. 2009;109(7):1232–1236. doi: 10.1016/j.jada.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 21.Levine JA, Madden AM, Morgan MY. Validation of a computer based system for assessing dietary intake. Br Med J (Clin Res Ed) 1987;295:369–372. doi: 10.1136/bmj.295.6594.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lambert N, Plumb J, Looise B, et al. Using smart card technology to monitor the eating habits of children in a school cafeteria: 3. The nutritional significance of beverage and dessert choices. J Hum Nutr Diet. 2005;18(4):271–279. doi: 10.1111/j.1365-277X.2005.00619.x. [DOI] [PubMed] [Google Scholar]
- 23.Burke LE, Sereika SM, Music E, Warziski M, Styn MA, Stone A. Using instrumented paper diaries to document self-monitoring patterns in weight loss. Contemp Clin Trials. 2008;29(2):182–193. doi: 10.1016/j.cct.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Votruba SB, Blanc S, Schoeller DA. Pattern and cost of weight gain in previously obese women. Am J Physiol Endocrinol Metab. 2002;282(4):E923–E930. doi: 10.1152/ajpendo.00265.2001. [DOI] [PubMed] [Google Scholar]
- 25.Sazonov E, Schuckers S, Lopez-Meyer P, et al. Non-invasive monitoring of chewing and swallowing for objective quantification of ingestive behavior. Physiol Meas. 2008;29(5):525–541. doi: 10.1088/0967-3334/29/5/001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hawkes C. Sales promotions and food consumption. Nutr Rev. 2009;67(6):333–342. doi: 10.1111/j.1753-4887.2009.00206.x. [DOI] [PubMed] [Google Scholar]
- 27.Vucic V, Glibetic M, Novakovic R, et al. Dietary assessment methods used for low-income populations in food consumption surveys: a literature review. Br J Nutr. 2009;101(Suppl 2):S95–S101. doi: 10.1017/S0007114509990626. [DOI] [PubMed] [Google Scholar]
- 28.Roman-Vinas B, Serra-Majem L, Ribas-Barba L, et al. Overview of methods used to evaluate the adequacy of nutrient intakes for individuals and populations. Br J Nutr. 2009;101(Suppl 2):S6–S11. doi: 10.1017/S0007114509990535. [DOI] [PubMed] [Google Scholar]
- 29.Pentland A, Lazer D, Brewer D, Heibeck T. Using reality mining to improve public health and medicine. Stud Health Technol Inform. 2009;149:93–102. [PubMed] [Google Scholar]
- 30.Levine JA. Measurement of energy expenditure. Public Health Nutr. 2005;8(7A):1123–1132. doi: 10.1079/phn2005800. [DOI] [PubMed] [Google Scholar]
- 31.Hill JO, DiGirolamo M, Heymsfield SB. Thermic effect of food after ingested versus tube-delivered meals. Am J Physiol. 1985;248(3 Pt 1):E370–E374. doi: 10.1152/ajpendo.1985.248.3.E370. [DOI] [PubMed] [Google Scholar]
- 32.Cunningham JJ. A reanalysis of the factors influencing basal metabolic rate in normal adults. Am J Clin Nutr. 1980;33(11):2372–2374. doi: 10.1093/ajcn/33.11.2372. [DOI] [PubMed] [Google Scholar]
- 33.Bliley KE, Schwab DJ, Zahn SK, et al. Design of posture and activity detector (PAD) Conf Proc IEEE Eng Med Biol Soc. 2007;2007:2659–2663. doi: 10.1109/IEMBS.2007.4352876. [DOI] [PubMed] [Google Scholar]
- 34.Bonomi AG, Goris AH, Yin B, Westerterp KR. Detection of type, duration, and intensity of physical activity using an accelerometer. Med Sci Sports Exerc. 2009;41(9):1770–1777. doi: 10.1249/MSS.0b013e3181a24536. [DOI] [PubMed] [Google Scholar]
- 35.Perry MA, Hendrick PA, Hale L, et al. Utility of the RT3 triaxial accelerometer in free living: An investigation of adherence and data loss. Appl Ergon. 2010;41(3):469–476. doi: 10.1016/j.apergo.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 36.Lee JS, Lifson N. Measurement of total energy and material balance in rats by means of doubly labeled water. Am J Physiol. 1960;199:238–242. doi: 10.1152/ajplegacy.1960.199.2.238. [DOI] [PubMed] [Google Scholar]
- 37.Schoeller DA, Taylor PB. Precision of the doubly labelled water method using the two-point calculation. Hum Nutr Clin Nutr. 1987;41(3):215–223. [PubMed] [Google Scholar]
- 38.Goran MI, Poehlman ET, Danforth E, Nair KS. Comparison of body composition methods in obese individuals. Basic Life Sci. 1993;60(3):85–86. doi: 10.1007/978-1-4899-1268-8_18. [DOI] [PubMed] [Google Scholar]
- 39.Heymsfield SB, Nunez C, Testolin C, Gallagher D. Anthropometry and methods of body composition measurement for research and field application in the elderly. Eur J Clin Nutr. 2000;54(Suppl 3):S26–S32. doi: 10.1038/sj.ejcn.1601022. [DOI] [PubMed] [Google Scholar]
- 40.Kissebah AH, Krakower GR. Regional adiposity and morbidity. Physiol Rev. 1994;74(4):761–811. doi: 10.1152/physrev.1994.74.4.761. [DOI] [PubMed] [Google Scholar]
- 41.Maddalozzo GF, Cardinal BJ, Snow CA. Concurrent validity of the BOD POD and dual energy x-ray absorptiometry techniques for assessing body composition in young women. J Am Diet Assoc. 2002;102(11):1677–1679. doi: 10.1016/s0002-8223(02)90358-5. [DOI] [PubMed] [Google Scholar]
- 42.Miyatake N, Takenami S, Kawasaki Y, Kunihashi Y, Nishikawa H, Numata T. Clinical evaluation of body fat percentage in 11,833 Japanese measured by air displacement plethysmograph. Intern Med. 2005;44(7):702–705. doi: 10.2169/internalmedicine.44.702. [DOI] [PubMed] [Google Scholar]
- 43.Lee SK. Validity of self-reported weight and height: comparison between immigrant and non-immigrant Mexican Americans in NHANES III. J Immigr Health. 2005;7(2):127–131. doi: 10.1007/s10903-005-2646-4. [DOI] [PubMed] [Google Scholar]
- 44.Dekkers JC, van Wier MF, Hendriksen IJ, Twisk JW, van Mechelen W. Accuracy of self-reported body weight, height and waist circumference in a Dutch overweight working population. BMC Med Res Methodol. 2008;8:69. doi: 10.1186/1471-2288-8-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bhargava A. Socio-economic and behavioural factors are predictors of food use in the National Food Stamp Program Survey. Br J Nutr. 2004;92(3):497–506. doi: 10.1079/bjn20041210. [DOI] [PubMed] [Google Scholar]
- 46.Payette H, Shatenstein B. Determinants of healthy eating in community-dwelling elderly people. Can J Public Health. 2005;96(Suppl 3):S27–35. [PubMed] [Google Scholar]
- 47.Boushey CJ, Kerr DA, Wright J, Lutes KD, Ebert DS, Delp EJ. Use of technology in children's dietary assessment. Eur J Clin Nutr. 2009;63(Suppl 1):S50–S57. doi: 10.1038/ejcn.2008.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martin CK, Han H, Coulon SM, Allen HR, Champagne CM, Anton SD. A novel method to remotely measure food intake of free-living individuals in real time: the remote food photography method. Br J Nutr. 2009;101(3):446–456. doi: 10.1017/S0007114508027438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Levy Y, Levy A, Zangen T, et al. Diagnostic clues for identification of nonorganic vs organic causes of food refusal and poor feeding. J Pediatr Gastroenterol Nutr. 2009;48(3):355–362. doi: 10.1097/mpg.0b013e31818b1936. [DOI] [PubMed] [Google Scholar]
- 50.Yamamoto T. Central mechanisms of roles of taste in reward and eating. Acta Physiol Hung. 2008;95(2):165–186. doi: 10.1556/APhysiol.95.2008.2.2. [DOI] [PubMed] [Google Scholar]
- 51.Heber D. An integrative view of obesity. Am J Clin Nutr. 2009;91(1):280S–283S. doi: 10.3945/ajcn.2009.28473B. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stoeckel LE, Kim J, Weller RE, Cox JE, Cook EW, 3rd, Horwitz B. Effective connectivity of a reward network in obese women. Brain Res Bull. 2009;79(6):388–395. doi: 10.1016/j.brainresbull.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Volpp KG, John LK, Troxel AB, Norton L, Fassbender J, Loewenstein G. Financial incentive-based approaches for weight loss: a randomized trial. JAMA. 2008;300(22):2631–2637. doi: 10.1001/jama.2008.804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chen KY, Acra SA, Majchrzak K, et al. Predicting energy expenditure of physical activity using hip- and wrist-worn accelerometers. Diabetes Technol Ther. 2003;5(6):1023–1033. doi: 10.1089/152091503322641088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Bouten CV, Koekkoek KT, Verduin M, Kodde R, Janssen JD. A triaxial accelerometer and portable data processing unit for the assessment of daily physical activity. IEEE Trans Biomed Eng. 1997;44(3):136–147. doi: 10.1109/10.554760. [DOI] [PubMed] [Google Scholar]
- 56.Mellecker RR, McManus AM, Lanningham-Foster LM, Levine JA. The feasibility of ambulatory screen time in children. Int J Pediatr Obes. 2008;4(2):1–6. doi: 10.1080/17477160802315002. [DOI] [PubMed] [Google Scholar]
- 57.Mellecker RR, McManus AM, Lanningham-Foster LM, Levine JA. The feasibility of ambulatory screen time in children. Int J Pediatr Obes. 2009;4(2):106–111. doi: 10.1080/17477160802315002. [DOI] [PubMed] [Google Scholar]
- 58.Lanningham-Foster L, Foster RC, McCrady SK, Jensen TB, Mitre N, Levine JA. Activity-promoting video games and increased energy expenditure. J Pediatr. 2009;154(6):819–823. doi: 10.1016/j.jpeds.2009.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Inzitari M, Greenlee A, Hess R, Perera S, Studenski SA. Attitudes of postmenopausal women toward interactive video dance for exercise. J Womens Health (Larchmt) 2009;18(8):1239–1243. doi: 10.1089/jwh.2008.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maddison R, Ni Mhurchu C. Global positioning system: a new opportunity in physical activity measurement. Int J Behav Nutr Phys Act. 2009;6:73. doi: 10.1186/1479-5868-6-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Romero-Ortuno R, Cogan L, Cunningham CU, Kenny RA. Do older pedestrians have enough time to cross roads in Dublin? A critique of the Traffic Management Guidelines based on clinical research findings. Age Ageing. 2010;39(1):80–86. doi: 10.1093/ageing/afp206. [DOI] [PubMed] [Google Scholar]
- 62.Elias MF, Snadowsky AM, Rizy EF. Identification of televised symbols as a function of symbol resolution. Percept Mot Skills. 1965;21(1):91–99. doi: 10.2466/pms.1965.21.1.91. [DOI] [PubMed] [Google Scholar]
- 63.Singh GK, Kogan MD, Yu SM. Disparities in obesity and overweight prevalence among US immigrant children and adolescents by generational status. J Community Health. 2009;34(4):271–281. doi: 10.1007/s10900-009-9148-6. [DOI] [PubMed] [Google Scholar]
- 64.Tanzi MC, Fare S. Adipose tissue engineering: state of the art, recent advances and innovative approaches. Expert Rev Med Devices. 2009;6(5):533–551. doi: 10.1586/erd.09.37. [DOI] [PubMed] [Google Scholar]
- 65.Matsushita H, Ishihara A, Mashiko S, et al. Chronic intracerebroventricular infusion of nociceptin/orphanin FQ produces body weight gain by affecting both feeding and energy metabolism in mice. Endocrinology. 2009;150(6):2668–2673. doi: 10.1210/en.2008-1515. [DOI] [PubMed] [Google Scholar]
- 66.Giani JF, Mayer MA, Munoz MC, et al. Chronic infusion of angiotensin-1–7 improves insulin resistance and hypertension induced by a high-fructose diet in rats. Am J Physiol Endocrinol Metab. 2009;296(2):E262–271. doi: 10.1152/ajpendo.90678.2008. [DOI] [PubMed] [Google Scholar]
- 67.Bray DA, Jr, Nguyen J, Craig J, Cohen BE, Collins DR., Jr Efficacy of a local anesthetic pain pump in abdominoplasty. Plast Reconstr Surg. 2007;119(3):1054–1059. doi: 10.1097/01.prs.0000252536.56982.34. [DOI] [PubMed] [Google Scholar]
- 68.Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women? Am J Clin Nutr. 1997;66(3):551–556. doi: 10.1093/ajcn/66.3.551. [DOI] [PubMed] [Google Scholar]
- 69.Saris WH, Blair SN, van Baak MA, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev. 2003;4(2):101–114. doi: 10.1046/j.1467-789x.2003.00101.x. [DOI] [PubMed] [Google Scholar]
- 70.Valente TW, Fujimoto K, Chou CP, Spruijt-Metz D. Adolescent affiliations and adiposity: a social network analysis of friendships and obesity. J Adolesc Health. 2009;45(2):202–204. doi: 10.1016/j.jadohealth.2009.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Lewis JA, Boian RF, Burdea G, Deutsch JE. Remote console for virtual telerehabilitation. Stud Health Technol Inform. 2005;111:294–300. [PubMed] [Google Scholar]
- 72.Glaser J, Foley T. The future of healthcare IT: what can we expect to see? Healthc Financ Manage. 2008;62(11):82–88. [PubMed] [Google Scholar]
- 73.Blake H. Mobile phone technology in chronic disease management. Nurs Stand. 2008;23(12):43–46. doi: 10.7748/ns2008.11.23.12.43.c6728. [DOI] [PubMed] [Google Scholar]
- 74.Page D. Technology: cell phones are quickly becoming cutting-edge medical devices. Hosp Health Netw. 2008;82(8):13. [PubMed] [Google Scholar]
- 75.Lee S, Lee T, Jin G, Hong J. An implementation of wireless medical image transmission system on mobile devices. J Med Syst. 2008;32(6):471–480. doi: 10.1007/s10916-008-9153-9. [DOI] [PubMed] [Google Scholar]
- 76.Sagahyroon A, Raddy H, Ghazy A, Suleman U. Design and implementation of a wearable healthcare monitoring system. Int J Electron Healthc. 2009;5(1):68–86. doi: 10.1504/IJEH.2009.026273. [DOI] [PubMed] [Google Scholar]
- 77.Pi-Sunyer FX. Comorbidities of overweight and obesity: current evidence and research issues. Med Sci Sports Exerc. 1999;31(11 Suppl):S602–S608. doi: 10.1097/00005768-199911001-00019. [DOI] [PubMed] [Google Scholar]
- 78.Puccio JA, Belzer M, Olson J, et al. The use of cell phone reminder calls for assisting HIV-infected adolescents and young adults to adhere to highly active antiretroviral therapy: a pilot study. AIDS Patient Care STDS. 2006;20(6):438–444. doi: 10.1089/apc.2006.20.438. [DOI] [PubMed] [Google Scholar]
- 79.Lehrman S. Dialing in Mobile phones target the world's nonreading poor. Sci Am. 2007;296(5):30–31. [PubMed] [Google Scholar]