Abstract
Mycobacterium ulcerans causes Buruli ulcer, an emerging infectious disease for which antimicrobial therapy has only recently proven to be beneficial. The discovery and development of new drugs against M. ulcerans are severely impeded by its very slow growth. Recombinant bioluminescent strains have proven useful in drug development for other mycobacterial infections, but the ability of such strains to discriminate bacteriostatic from bactericidal activity has not been well demonstrated. We engineered recombinant M. ulcerans strains to express luxAB from Vibrio harveyi. In drug susceptibility tests employing a wide range of antimicrobial agents and concentrations, the relative light unit (RLU) count measured in real time was a reliable surrogate marker for CFU counts available 3 months later, indicating utility for the rapid determination of drug susceptibility and discrimination of bacteriostatic and bactericidal effects. A second important finding of this study is that the addition of subinhibitory concentrations of the ATP-binding cassette transporter inhibitor reserpine increases the susceptibility of M. ulcerans to tetracycline and erythromycin, indicating that drug efflux may explain at least part of the intrinsic resistance of M. ulcerans to these agents.
Mycobacterium ulcerans disease, or Buruli ulcer, is an emerging infectious disease in many humid tropical areas of the world. Presently, it is the third most common mycobacterial disease of humans, after tuberculosis and leprosy (37), but in some swampy areas of central and western Africa, it may be the most prevalent mycobacterial disease. Until recently, it was considered to be unresponsive to antimicrobial therapy and managed primarily by surgical excision with skin grafting. Combination chemotherapy with streptomycin (STR) and rifampin (RIF) for 2 months has demonstrated significant experimental and clinical efficacy against M. ulcerans disease (10, 15). However, STR requires parenteral administration and may cause nephrotoxicity and/or ototoxicity. RIF has relatively weak bactericidal activity against M. ulcerans (7) and may select drug-resistant mutants if used as monotherapy (28). The combination of RIF and clarithromycin (CLR) has shown promise (30), but the emergence of RIF resistance despite the use of this combination was described previously (16). Fluoroquinolones are active against M. ulcerans but are generally contraindicated for children, who represent more than half of the cases (51). Therefore, there is a substantial need to discover and/or develop new drugs to fully enable oral treatment regimens and/or regimens capable of treating M. ulcerans disease in 1 month or less.
A major obstacle for drug discovery and development is the very slow growth rate of M. ulcerans. Indeed, the organism requires up to 3 months of incubation at 32°C to form countable colonies on solid media. In order to accelerate the pace of discovery and development efforts, we sought a real-time method of quantifying viable bacteria following drug exposure. Light production by various luciferase enzymes has been used as a real-time biomarker of bacterial viability for the high-throughput screening of antibiotics and drug susceptibility testing against mycobacteria (4, 5, 12, 17, 22). Bioluminescence produced by a strain of Mycobacterium smegmatis expressing the luxAB genes from the bacterium Vibrio harveyi was 2 orders of magnitude greater than that produced by a comparable strain expressing firefly luciferase (3, 42). Mycobacterial reporter strains expressing luxAB have been used to screen antibiotics and biocides in vitro (3) and evaluate vaccine efficacy (42) in a murine model. Therefore, we sought to develop a reporter strain of M. ulcerans expressing the luxAB genes from V. harveyi. Integrative plasmid vectors in addition to extrachromosomal plasmid vectors were tested in an effort to better ensure plasmid stability and to avoid incompatibility with the giant plasmid of M. ulcerans responsible for the production of the mycolactone toxin (19, 44, 46).
Genome studies have revealed putative drug efflux pumps in most bacteria. The overexpression of such efflux pumps can increase the MICs of multiple antibiotics and may be responsible for intrinsic antibiotic resistance in some species (26). However, the clinical significance of efflux-mediated changes in drug susceptibility among mycobacteria has not been well established. At least 26 putative ATP-binding cassette (ABC) transporters exist in Mycobacterium tuberculosis, and genes encoding ABC transporters occupy 2.5% of the genome (11). Efflux pump inhibitors were recently shown to enhance the killing of intracellular multidrug-resistant M. tuberculosis (1). We blasted all 121 ABC transporter gene products in M. tuberculosis H37Rv against the genome sequence of M. ulcerans Agy99 and found that most of them have homologs in M. ulcerans. Here we used a known inhibitor of ABC transporters (reserpine) to explore the role of ABC efflux transporters in the intrinsic resistance of M. ulcerans to clinically relevant antibiotics.
MATERIALS AND METHODS
Bacterial strains and culture media.
Transformed Escherichia coli DH5α or DH10 isolates were selected on Luria agar containing 25 μg/ml of kanamycin (KAN) (Invitrogen) or 100 μg/ml of hygromycin (HYG) (Roche Diagnostics). Transformed M. smegmatis and M. ulcerans isolates were selected on Middlebrook 7H11 agar (Difco) containing 10% oleic acid-dextrose-catalase complex (OADC) (Difco) and either KAN at 25 μg/ml or HYG at 40 μg/ml. M. ulcerans strains ATCC 19423, Cu001, and 1059 (Table 1) were grown in Dubos broth (Difco) containing Dubos medium albumin and 0.07% Tween 80 for growth and in Middlebrook 7H9 broth (Difco) containing 10% OADC for drug susceptibility testing. When plating suspensions from footpad tissue, selective 7H11 plates were used (50).
TABLE 1.
Bacterial strains, plasmids, and oligonucleotidesa
| Strain, plasmid, or oligonucleotide | Relevant characteristic(s) or sequence (5′-3′)b | Source or reference |
|---|---|---|
| Strains | ||
| M. ulcerans ATCC 19423 | Isolated from Australia | ATCC |
| M. ulcerans Cu001 | Isolated from Côte d'Ivoire | 24 |
| M. ulcerans 1059 | Isolated from Ghana | 53 |
| M. smegmatis mc2155 | Highly transformable derivative of ATCC 607 | 41 |
| Escherichia coli DH5α | F− [φ80dlacZΔM15] Δ(lacZYA-argF)U169 deoR recA1 endA1 hsdR17 glnV44 thi-1 gyrA96 relA | 21 |
| Escherichia coli DH10B | F− [φ80dlacZΔM15] araDJ39 Δ(ara leu)7697 ΔlacX74 galU galK rpsL deoR endA1 nupG recA1 mcrA Δ(mrr hsdRMS mcrBC) | 14 |
| Plasmids | ||
| pCRII | AMPr KANr; 3.9 kb; general-purpose cloning vector | Invitrogen |
| pNBV1 | HYGr; 5.8 kb; E. coli-Mycobacterium shuttle vector | 23 |
| pCK0601 | AMPr HYGr, E Ori, Mycobacterium integrative plasmid | 27 |
| pMH94 | AMPr KANr; 6.2 kb; E Ori; Mycobacterium integrative plasmid | 25 |
| p60LUX | pNBV1 carrying the luxAB gene under the hsp60 promoter | 39 |
| pG13LUX | pNBV1 carrying the luxAB gene under the MuG13 promoter | This study |
| pMOPLUX | pNBV1 carrying the luxAB gene under the mop promoter | This study |
| pTYG13H | pCK0601 carrying the luxAB gene under the MuG13 promoter | This study |
| pTY60H | pCK0601 carrying the luxAB gene under the hsp60 promoter | This study |
| pTY60K | pMH94 carrying the luxAB gene under the hsp60 promoter | This study |
| Oligonucleotides | ||
| G13f | CCTCTAGAGGAATCAGCGCACTGGC (XbaI) | This study |
| G13r | AAGGATCCTCCTCCGCAACACTTCTGCCATT (BamHI) | This study |
| MOPf | TATCTAGACCAGGCTTGACACTTT (XbaI) | This study |
| MOPr | AAGGATCCTCCTCCGAATTGTGAGCG (BamHI) | This study |
| pID | CCCAATACGCAAACCGCCTC | This study |
AMPr, ampicillin resistance; ATCC, American Type Culture Collection.
Restriction enzyme sites are underlined, and the corresponding enzymes are indicated in parentheses. Italics indicate the ribosome-binding site.
Plasmid construction and transformation.
The promoters used were (i) the widely used hsp60 (48) promoter from Mycobacterium bovis BCG, (ii) the Mycobacterium marinum G13 promoter (6) homolog (MuG13) amplified from M. ulcerans ATCC 19423, and (iii) the artificial mycobacterial optimal promoter (MOP) (22), which was modified and amplified from plasmid pMH29. The E. coli-mycobacterium shuttle vectors included extrachromosomal plasmids based on p60LUX (39), a kind gift from Richard L. Friedman (University of Arizona), and integrative plasmids derived from pMH94 (25) and pCK0601 (27) (Table 1).
Primers used to amplify promoters MuG13 and MOP were G13f-G13r and MOPf-MOPr, respectively (Table 1). Genomic DNA of M. ulcerans was isolated as described previously by Stinear et al. (43). The amplified MuG13 promoter was cut with XbaI and BamHI and ligated into plasmid p60LUX cut with the same enzymes to form plasmid pG13LUX. The plasmid was verified by PCR using the following primer pairs: G13f-G13r and pID (whose sequence is between oriC and the hsp60 promoter in p60LUX [39])-G13r. Similarly, the amplified MOP was inserted into p60LUX to form plasmid pMOPLUX, and it was verified by PCR using primer pairs MOPf-MOPr and pID-MOPr. The PCR products of the MuG13 promoter and MOP amplified with pID plus the corresponding reverse primers using p60LUX and pMOPLUX as templates were then sequenced. Plasmids p60LUX and pG13LUX were cut with XbaI and KpnI to obtain the fragments hsp60-luxAB and MuG13-luxAB, and they were inserted into pCK0601 cut with the same enzymes to form plasmids pTY60H and pTYG13H (H indicates HYG resistance), respectively. A fragment containing hsp60-luxAB was cut from pTY60H with KpnI and NdeI and was inserted into pHM94 cut with the same enzymes to obtain pTY60K (K indicates KAN resistance).
M. smegmatis was transformed by an electroporation method (41). M. ulcerans was transformed by the electroporation method with some modifications. We transformed M. ulcerans using not only broth culture but also suspensions of infected footpad tissue and of colonies. The mixture of the plasmid and the competent M. ulcerans cells was incubated at 37°C for 10 min before electroporation transformation was performed at room temperature (52).
Antimicrobial agents.
Moxifloxacin (MXF), linezolid (LZD), and clarithromycin (CLR) were kindly provided by Bayer, Pfizer, and Abbott, respectively. Rifampin (RIF), streptomycin (STR), isoniazid (INH), tetracycline (TET), erythromycin (ERY), and reserpine (RES) were purchased from Sigma.
Determination of MICs with 7H11 agar.
Serial dilutions of drugs were prepared and added to Middlebrook 7H11 agar with 10% OADC. M. ulcerans was grown to an optical density at 600 nm (OD600) of 0.3 to 0.7, and a series of dilutions was plated. Plates were inoculated with 0.5-ml aliquots and incubated at 32°C for 90 days before colony counting. The MIC was defined as the lowest drug concentration that inhibited at least 99% of the bacterial growth observed for drug-free control plates. Each assay was performed in duplicate.
Comparison of light production by different recombinant strains.
Individual colonies were used to inoculate broth, and the OD600 was monitored until it reached 0.15 to 0.35. Light production was measured by removing 200-μl aliquots into 1.5 ml polystyrene tubes (USA Scientific), adding 20 μl of 1% decyl aldehyde substrate in ethanol, and measuring the amount of light produced in 4 s by using a TD20/20 luminometer (Turner BioSystems). Bioluminescence was expressed as the number of relative light units (RLU)/ml detected.
Drug susceptibility testing of broth cultures using RLU and CFU as endpoints.
Serial 2-fold dilutions of drug-containing solutions and M. ulcerans broth cultures (OD600 of 0.3 to 0.7) were prepared as described above for MIC detection. Aliquots were removed for CFU counts and RLU assays after 0, 7, and/or 14 days of incubation. Plates were incubated at 32°C for 90 days before the CFU were counted. Bioluminescence assays for the recombinant ATCC 19423(pTY60H) strain were performed as described above. For the recombinant ATCC 19423(pTY60K) strain and the recombinant 1059(pTY60K) strain, the assays were performed with 250-μl aliquots and 25 μl of substrate per tube, and light production was measured by using a 20/20n luminometer (Turner BioSystems). The TD20/20 luminometer provides an RLU value 1,000 times lower than that provided by the 20/20n version. For uniformity in this study, we defined 1 RLU as 1 unit in the 20/20n luminometer, equivalent to 0.001 units in the TD20/20 luminometer. In these experiments, the MIC and MIClux were defined as the lowest drug concentrations that prevented an increase in the CFU and RLU values, respectively, compared to the baseline (day 0) values.
Effect of efflux inhibitors on drug susceptibility.
The recombinant ATCC 19423(pTY60H) strain was used for drug susceptibility testing, as described above. Susceptibility to RES was tested by using doubling RES concentrations from 0.31 to 10 μg/ml. In experiments to determine the effect of RES on the susceptibility to other antibiotics, 2.5 μg/ml of RES was used. After 14 days of incubation, duplicate aliquots from each tube were removed for RLU and CFU determinations as described above.
RESULTS
Construction of plasmids and transformation.
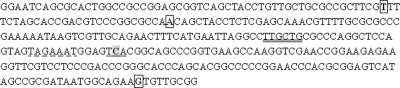
The MICs of KAN and HYG were ≤5 μg/ml and ≤12.5 μg/ml, respectively, for both M. ulcerans strains 19423 and Cu001. The promoter MuG13 was amplified successfully from both M. ulcerans ATCC 19423 and M. ulcerans Cu001 with a single ∼300-bp band. No band was amplified from negative control M. tuberculosis H37Rv genomic DNA. E. coli colonies containing pG13LUX candidates with the MuG13 promoter from M. ulcerans ATCC 19423 were verified with primer pairs pID-G13r and G13f-G13r, producing a ∼1-kb band and a ∼300-bp band, respectively. The ∼1-kb band amplified with Pfu enzyme was sequenced (Fig. 1). Small differences were observed in the G13 promoter sequences between strain ATCC 19423, the genome-sequenced strain M. ulcerans Agy99 and the closest relative, M. marinum M. This finding is consistent with the findings of a comparative genomic analysis (47), which found that M. ulcerans and M. marinum have >98% nucleotide sequence identity and genome-wide synteny. The differing base pairs among the three G13 promoters are outside the functional region, so the promoter is relatively conserved. The MOP was amplified successfully with a single ∼80-bp band, but we did not obtain E. coli transformants containing pMOPLUX. However, we successfully transformed M. smegmatis directly with the ligation product of pMOPLUX. All 15 randomly selected colonies were positively identified by primers MOPf-MOPr (a single ∼80-bp band) and pID-MOPr (a single ∼300-bp band). Two isolates were selected for plasmid extraction and verified by PCR using pID-MOPr. The sequence of the PCR product was the same as expected (22). Furthermore, E. coli could not be transformed with purified plasmid pMOPLUX from M. smegmatis, suggesting that pMOPLUX is toxic to E. coli but not to M. smegmatis.
FIG. 1.
MuG13 sequence from M. ulcerans ATCC 19423. The boxed T and A indicate the sites that differ between the M. ulcerans ATCC 19423 and the M. marinum G13 promoters. The boxed T and G indicate the sites that differ between the M. ulcerans ATCC 19423 and M. ulcerans Agy99 G13 promoters. The double-underlined sequence TTGCTG and the dash-underlined sequence TAGAAAT are potential −35 and −10 regions, respectively. The underlined shaded C is believed to be the start site of transcription.
All target plasmids (p60LUX, pMOPLUX, pG13LUX, pTY60H, and pTYG13H) and the control plasmids (pNBV1 [23] and pCK0601) were transformed into M. ulcerans ATCC 19423 and Cu001 successfully. The recombinant M. ulcerans strains were verified by the detection of RLU directly by using individual-colony suspensions. The E. coli strains containing p60LUX, pG13LUX, pTY60H, and pTYG13H and M. smegmatis containing pMOPLUX were bioluminescent (Fig. 2). A late-log-phase broth culture of E. coli containing the target plasmids emitted >5,000 RLU/ml in the absence of exogenous substrate, indicating that the LuxAB reaction occurs constitutively at a low level. The G13 promoter, the hsp60 promoter, and the MOP are all functional in E. coli, which is in agreement with data from previous reports (6, 22, 40). Each of the plasmids was stable in M. ulcerans. No loss of resistance markers or luciferase activity was observed during our experiments.
FIG. 2.
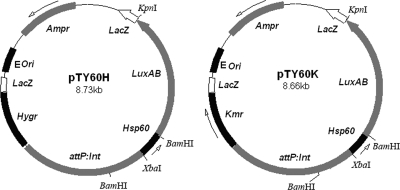
Integrative plasmids pTY60H and pTY60K.
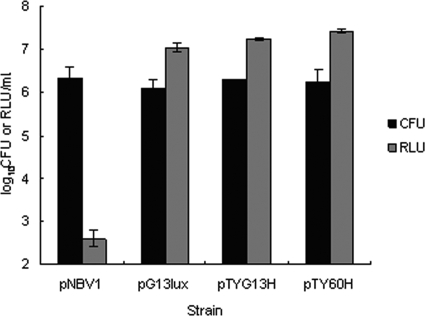
Comparison of light production by different recombinant strains.
ATCC 19423 strains transformed with pG13LUX, pTYG13H, or pTY60H produced comparable amounts of RLU per CFU (Fig. 3). As expected, the control transformed with pNBV1 produced only background luminescence. The similarity of luminescence intensities between strains containing different types of plasmids (extrachromosomal and integrative) with the same or different promoters upstream of luxAB differs from data from a previous report involving M. smegmatis (42). We later confirmed that all recombinant M. ulcerans strains (whether from Cu001 or from ATCC 19423) transformed with p60LUX, pMOPLUX, pG13LUX, pTY60H, or pTYG13H gave similar RLU/CFU ratios at similar OD values (data not shown). Recombinant M. ulcerans ATCC 19423 strains containing the integrative plasmids pTY60H and pTY60K (Fig. 2) were selected for initial drug susceptibility studies. Because the parental strain ATCC 19423 was later found to be attenuated in its ability to cause footpad swelling in mice (data not shown), we transformed a mouse-passaged isolate of M. ulcerans 1059 with pTY60K for subsequent in vitro experiments in order to have consistency between the present in vitro experiments and future in vivo experiments.
FIG. 3.
CFU and RLU results from recombinant M. ulcerans ATCC 19423 strains transformed with different luxAB-containing plasmids. pNBV1 is the empty control plasmid.
MICs of selected antimicrobial agents for recombinant luminescent strains and their parents.
The MIC of each drug for the recombinant M. ulcerans strains was within 1 dilution of the MIC for the corresponding wild-type M. ulcerans parent (Tables 2 and 3), indicating that genetic transformation did not alter the intrinsic drug susceptibility of the recombinant M. ulcerans strains. The single exception was that the MIC of rifampin for recombinant M. ulcerans strain 1059(pTY60K) was 2 dilutions higher than that for the parental strain, but this may well be a chance result. It is also notable that the susceptibilities of ATCC 19423 and 1059 to MXF differ markedly, with the former being highly susceptible to MXF and the latter appearing to be resistant to MXF, exemplifying the susceptibility range previously observed by Ji et al. (24).
TABLE 2.
MICs of selected antibiotics for wild-type parent strain ATCC 19423 or recombinant M. ulcerans strain ATCC 19423(pTY60H) determined on 7H11 agar
| Drug | MIC (μg/ml) for: |
|
|---|---|---|
| Wild-type M. ulcerans | Recombinant M. ulcerans | |
| RIF | 0.5 | 0.5 |
| STR | 0.25 | 0.25 |
| MXF | ≤0.016 | 0.03 |
| TET | 10 | 5 |
| ERY | >16 | >16 |
TABLE 3.
MIC of selected antibiotics for wild-type parent strain 1059 or recombinant M. ulcerans strain 1059(pTY60K) determined on 7H11 agar
| Drug | MIC (μg/ml) for: |
|
|---|---|---|
| Wild-type M. ulcerans | Recombinant M. ulcerans | |
| RIF | 0.13 | 0.5 |
| STR | 0.25 | 0.25 |
| MXF | >0.5 | >0.5 |
| LZD | 1 | 1 |
| CLR | 0.25 | 0.25 |
| INH | >40 | >40 |
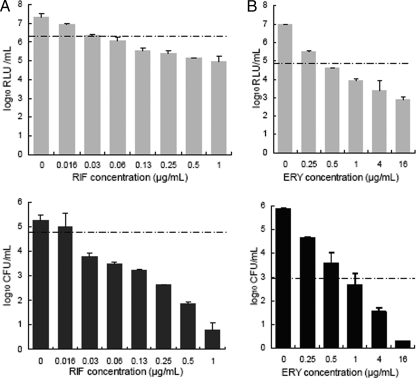
Correlation of RLU and CFU counts during susceptibility testing in broth medium.
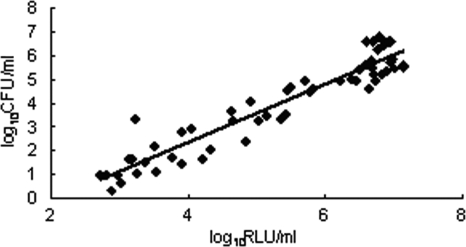
As depicted in Tables 4, 5, and 6, the MIClux in broth determined by using the real-time luminescence method was similar to the MIC defined from CFU counts available 3 months later. Moreover, the occurrence and extent of bacteriostatic or bactericidal activity observed at each concentration, as indicated by CFU counts, were generally well represented by RLU counts until the luminescence reached the background level of approximately 2.7 log10 RLU/ml (see examples in Fig. 4). These results indicate that the measurement of luminescence is a suitable surrogate marker for the discrimination of bacteriostatic and bactericidal drug effects. The RLU and CFU correlated very well, with r2 values of 0.95 for all drugs tested (Fig. 5).
TABLE 4.
MIC and MIClux of selected antibiotics for recombinant M. ulcerans strain ATCC 19423(pTY60H) determined in 7H9 broth after 14 days of incubation
| Drug | MIC (μg/ml) determined according to CFU counts | MIClux (μg/ml) determined according to RLU counts |
|---|---|---|
| RIF | ≤0.03 | ≤0.03 |
| STR | 1 | 1 |
| MXF | ≤0.03 | ≤0.03 |
| TET | 2.5 | 2.5 |
| ERY | 1 | 0.5 |
TABLE 5.
MIC and MIClux of selected antibiotics for recombinant M. ulcerans strain 1059(pTY60K) determined in 7H9 broth after 14 days of incubation
| Drug | MIC (μg/ml) determined according to CFU counts | MIClux (μg/ml) determined according to RLU counts |
|---|---|---|
| RIF | 0.03 | 0.06 |
| STR | 0.13 | 0.13 |
| MXF | >0.25 | >0.25 |
| LZD | 4 | 2 |
| CLR | 0.25 | 0.13 |
| INH | >40 | >40 |
TABLE 6.
MIC and MIClux of selected antibiotics for recombinant M. ulcerans strain ATCC 19423(pTY60K) determined in 7H9 broth after 7 days of incubation
| Drug | MIC (μg/ml) determined according to CFU counts (μg/ml) | MIClux(μg/ml) determined according to RLU counts |
|---|---|---|
| RIF | ≤0.016 | 0.03 |
| STR | 0.25 | 0.5 |
| MXF | 0.03 | 0.03 |
| LZD | 1 | 1 |
| CLR | 0.03 | 0.13 |
| INH | >40 | >40 |
FIG. 4.
Drug susceptibility testing of RIF and ERY against recombinant M. ulcerans strains, comparing CFU and RLU as endpoints. (A) Concentration-ranging activity of RIF against recombinant M. ulcerans 1059(pTY60K) after 7 days of incubation. (B) Concentration-ranging activity of ERY against recombinant M. ulcerans ATCC 19423(pTY60H) after 14 days of incubation. Dotted horizontal lines indicate the values at the onset of drug exposure.
FIG. 5.
Correlation of RLU and CFU counts after drug exposure. The correlation coefficient (r2 value) of log10 RLU and log10 CFU in all CFU-positive tubes from experiments with recombinant M. ulcerans strain ATCC 19423(pTY60H) (including RIF, MFX, ERY, STR, and TET) is 0.95.
Role of efflux in the intrinsic antibiotic resistance of M. ulcerans.
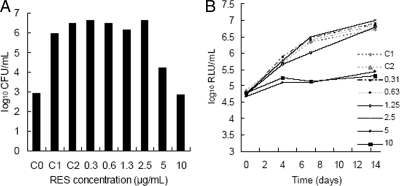
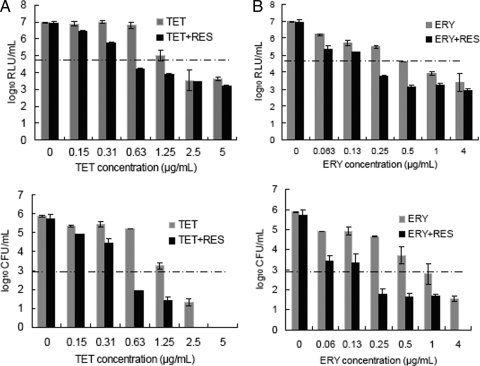
As shown in Fig. 6, 2.5 μg/ml was the highest concentration of RES that had no effect on the growth of recombinant M. ulcerans ATCC 19423(pTY60H). Therefore, this was the concentration of RES used in the subsequent experiments. The addition of RES did not increase susceptibility to STR, RIF, or MXF. Based on CFU counts, the MIC of TET was 1.25 μg/ml alone and 0.625 μg/ml in combination with RES (Fig. 7A). The MIC of ERY was 1 μg/ml alone and 0.25 μg/ml in combination with RES (Fig. 7B). Again, RLU counts correlated well with CFU counts until the background level of approximately 2.7 log10 RLU/ml was reached (Fig. 7A and B). Therefore, it is evident that the addition of RES increased the effect of TET by at least 2-fold and that of ERY by at least 4-fold.
FIG. 6.
Susceptibility of recombinant M. ulcerans ATCC 19423(pTY60H) to RES. (A) CFU counts before (C0) and after (all remaining bars) exposure to the indicated treatments for 14 days. (B) Serial RLU results measured over 14 days of exposure to the indicated RES concentration. C1 and C2 are RES-free controls with water and dimethyl sulfoxide (DMSO), respectively.
FIG. 7.
Increased susceptibility of recombinant M. ulcerans ATCC 19423(pTY60H) to TET (A) and ERY (B) in the presence of RES at 2.5 μg/ml. Dotted horizontal lines indicate the values at the onset of drug exposure. The duration of drug exposure was 14 days.
DISCUSSION
In this report, we demonstrate the feasibility of engineering recombinant bioluminescent M. ulcerans strains expressing luxAB and the utility of such strains for the rapid evaluation of antimycobacterial drug effects in vitro. The recombinant M. ulcerans strains grow normally and have the same drug susceptibility as that of the parental strains. Because of the excellent correlation between RLU and CFU counts, RLU counts provided a reliable surrogate marker enabling the real-time determination of bacteriostatic and bactericidal effects that would ordinarily require 3 months to ascertain with CFU counts. With appropriate equipment, such strains would be suitable for high-throughput screening, as 200 μl broth culture per well and 4 to 7 days of incubation were sufficient to discriminate active compounds from drug-free controls. Hence, recombinant luminescent strains have the potential to accelerate the pace of the discovery and development of drugs that may improve the treatment of this emerging pathogen. Because our bioluminescence-based method requires the genetic transformation of the test organism, other more convenient methods may be developed for evaluating the drug susceptibilities of clinical isolates or a large panel of strains.
For most drugs, the MIC determined by RLU and CFU counts with broth cultures corresponded closely with the MIC determined by conventional agar-based methods. For RIF however, the MIC determined by CFU counts in broth was 4 dilutions lower than the MIC determined by the agar method. Potential explanations for this finding include the instability of RIF in agar media incubated for 3 months and possible microbial adaptation and growth during prolonged incubation with drug concentrations that may initially be bacteriostatic. A greater discrepancy was seen in the evaluation of ERY activity against strain ATCC 19423, for which the MIC was determined to be >16 μg/ml on agar, while the MIC was determined to be 1 μg/ml in broth. Two previously published studies (13, 36) reported the MICs of CLR for this strain to be 0.5 and 1.25 at pH 6.6 and 6.8 on agar and in the Bactec system, respectively, which are similar to the MIC values in broth observed here (Tables 4 and 6). To the best of our knowledge, the MIC of ERY for this or any other strain of M. ulcerans has not been reported. Possible reasons for the discrepancy between the observed MICs of ERY include an instability of ERY in the agar medium and inducible resistance that may become more evident with prolonged incubation. The potential for efflux-mediated resistance will be discussed below. An inducible endoribosomal methylase enzyme is another possibility, but this mechanism would also be expected to have a strong effect on susceptibility to CLR, which was not observed in our study or by others (13, 36). Furthermore, a BLAST search of the fully sequenced M. ulcerans Agy99 genome did not reveal a gene homologous to Rv1988 (9), which encodes ErmMT, the inducible endoribosomal methylase of the M. tuberculosis complex (2).
Several important observations may inform future efforts to engineer recombinant strains of this unusual mycobacterium. First, the pAL5000-derived extrachromosomal plasmid pNBV1 (23) is compatible with the giant plasmid pMU001 (44, 46) of M. ulcerans and can exist stably in M. ulcerans. Unlike the predicted RepA proteins from many other mycobacterial plasmids, which are highly homologous to the repA gene product of pMU001 (44, 46), that of pAL5000 appears to be unrelated (18, 34, 46). The successful transformation of M. ulcerans indicates that pAL5000-derived vectors, which have been used extensively with other mycobacteria, will likely prove useful in other efforts to transform M. ulcerans.
Second, site-specific recombination mediated by mycobacteriophage L5 integrase is feasible for the integration of genetic material into the M. ulcerans chromosome. This finding followed a sequence analysis that confirmed that identical 63-bp fragments (GCTCAATGGTAGAGCCCTAGTCTTCCAAACTAGCTACGCGGGTTCGATTCCCGTCGCCCGCTC) containing both the 43-bp core sequence of the attB site (in boldface type) (25) and the 29-bp fragment (in italics) (33) necessary and sufficient for attB function exist in M. smegmatis, M. ulcerans Agy99, M. marinum M, M. tuberculosis H37Rv, and M. avium 104. Furthermore, the protein sequences of the necessary mycobacterial integration host factor (mIHF) in M. ulcerans Agy99 and M. marinum M are almost identical to those in M. smegmatis and M. tuberculosis H37Rv (32) (data not shown).
Third, we were unable to transform E. coli with luxAB under the control of the strong artificial MOP. It was previously reported that the superoxide radical by-product of the luxAB reaction is toxic for E. coli (20), especially for strains deficient in superoxide dismutase (SOD). We overcame this obstacle by transforming pMOPLUX directly into M. smegmatis and M. ulcerans, which, we speculate, have highly expressed SOD like M. tuberculosis (49, 54). Despite this, it is possible that efforts to further enhance the expression of luxAB in mycobacteria to increase assay sensitivity could have negative effects on viability. In fact, our finding that different recombinant M. ulcerans strains containing single-copy integrative plasmids or multicopy extrachromosomal plasmids (8) with luxAB under different promoters produced similar RLU/CFU ratios suggests that the luxAB copy number and the strength of the promoters do not determine the magnitude of bioluminescence in the recombinant M. ulcerans strains. This is different from previous findings using M. smegmatis in which those authors found that the extrachromosomal plasmid gave higher RLU/CFU ratios (42).
Finally, we successfully transformed M. ulcerans in suspensions of tissue from infected mouse footpads as well as colonies scraped from agar plates. The obvious advantages of such a technique are (i) a more rapid manipulation of slow-growing mycobacteria and (ii) the avoidance of repeated in vitro passage that can result in a loss of virulence or other genetic changes. This is particularly important for M. ulcerans because the giant plasmid responsible for virulence is unstable (45).
Drug efflux is increasingly being recognized as a mechanism of intrinsic bacterial resistance to antibiotics. Despite its intrinsic resistance to a variety of antibiotic classes, M. ulcerans has not previously been shown to harbor drug transporters associated with reduced drug susceptibility. Here we show that the exposure of M. ulcerans to RES, an inhibitor of ABC transporters, results in 2-fold increases in TET activity and 4-fold or greater increases in ERY activity, suggesting an inhibition of as-yet-uncharacterized pumps for which TET and ERY are substrates. These data are consistent with previously reported observations that most ABC transporters in other mycobacterial species are susceptible to RES (31, 35, 38). A BLAST search did reveal a gene in M. ulcerans Agy99 encoding a putative macrolide ABC transporter ATP-binding protein with 91% amino acid identity to its homolog (Rv1473) in M. tuberculosis H37Rv (26). Our results provide preliminary data that ABC transporters contribute to the intrinsic resistance of M. ulcerans to TET and ERY. The direct antimicrobial effect of reserpine alone and its enhancement of the activity of TET and ERY suggest that targeting efflux mechanisms in drug development may result in new antimycobacterial drugs that also enhance the action of existing agents against M. ulcerans (26).
Acknowledgments
This work was supported by grants from the Raoul Follereau Foundation and the National Institute of Allergy and Infectious Diseases (grant R01 AI-082612).
We thank Richard L. Friedman at the University of Arizona for providing us with plasmid p60LUX as a gift. We acknowledge the enthusiastic support and the kind gift of M. ulcerans strain 1059 from Pamela L. C. Small at the University of Tennessee. Finally, we thank Baohong Ji at the Pitie-Salpetriere School of Medicine, Paris, France, for providing us with strain Cu001.
Footnotes
Published ahead of print on 26 April 2010.
REFERENCES
- 1.Amaral, L., M. Martins, and M. Viveiros. 2007. Enhanced killing of intracellular multidrug-resistant Mycobacterium tuberculosis by compounds that affect the activity of efflux pumps. J. Antimicrob. Chemother. 59:1237-1246. [DOI] [PubMed] [Google Scholar]
- 2.Andini, N., and K. A. Nash. 2006. Intrinsic macrolide resistance of the Mycobacterium tuberculosis complex is inducible. Antimicrob. Agents Chemother. 50:2560-2562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andrew, P. W., and I. S. Roberts. 1993. Construction of a bioluminescent mycobacterium and its use for assay of antimycobacterial agents. J. Clin. Microbiol. 31:2251-2254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arain, T. M., A. E. Resconi, M. J. Hickey, and C. K. Stover. 1996. Bioluminescence screening in vitro (Bio-Siv) assays for high-volume antimycobacterial drug discovery. Antimicrob. Agents Chemother. 40:1536-1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arain, T. M., A. E. Resconi, D. C. Singh, and C. K. Stover. 1996. Reporter gene technology to assess activity of antimycobacterial agents in macrophages. Antimicrob. Agents Chemother. 40:1542-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barker, L. P., S. F. Porcella, R. G. Wyatt, and P. L. Small. 1999. The Mycobacterium marinum G13 promoter is a strong sigma 70-like promoter that is expressed in Escherichia coli and mycobacteria species. FEMS Microbiol. Lett. 175:79-85. [DOI] [PubMed] [Google Scholar]
- 7.Bentoucha, A., J. Robert, H. Dega, N. Lounis, V. Jarlier, and J. Grosset. 2001. Activities of new macrolides and fluoroquinolones against Mycobacterium ulcerans infection in mice. Antimicrob. Agents Chemother. 45:3109-3112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bourn, W. R., Y. Jansen, H. Stutz, R. M. Warren, A. L. Williamson, and P. D. van Helden. 2007. Creation and characterisation of a high-copy-number version of the pAL5000 mycobacterial replicon. Tuberculosis (Edinb.) 87:481-488. [DOI] [PubMed] [Google Scholar]
- 9.Buriánková, K., F. Doucet-Populaire, O. Dorson, A. Gondran, J. C. Ghnassia, J. Weiser, and J. L. Pernodet. 2004. Molecular basis of intrinsic macrolide resistance in the Mycobacterium tuberculosis complex. Antimicrob. Agents Chemother. 48:143-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chauty, A., M. F. Ardant, A. Adeye, H. Euverte, A. Guèdèenon, C. Johnson, J. Aubry, E. Nuermberger, and J. Grosset. 2007. Promising clinical efficacy of streptomycin-rifampin combination for treatment of Buruli ulcer (Mycobacterium ulcerans disease). Antimicrob. Agents Chemother. 51:4029-4035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choudhuri, B. S., S. Bhakta, R. Barik, J. Basu, M. Kundu, and P. Chakrabarti. 2002. Overexpression and functional characterization of an ABC (ATP-binding cassette) transporter encoded by the genes drrA and drrB of Mycobacterium tuberculosis. Biochem. J. 367:279-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cooksey, R. C., J. T. Crawford, W. R. Jacobs, Jr., and T. M. Shinnick. 1993. A rapid method for screening antimicrobial agents for activities against a strain of Mycobacterium tuberculosis expressing firefly luciferase. Antimicrob. Agents Chemother. 37:1348-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dossou, A. D., G. E. Sopoh, C. R. Johnson, Y. T. Barogui, D. Affolabi, S. Y. Anagonou, T. Zohoun, F. Portaels, and K. Asiedu. 2008. Management of Mycobacterium ulcerans infection in a pregnant woman in Benin using rifampicin and clarithromycin. Med. J. Aust. 189:532-533. [DOI] [PubMed] [Google Scholar]
- 14.Durfee, T., R. Nelson, S. Baldwin, G. Plunkett III, V. Burland, B. Mau, J. F. Petrosino, X. Qin, D. M. Muzny, M. Ayele, R. A. Gibbs, B. Csörgo, G. Pósfai, G. M. Weinstock, and F. R. Blattner. 2008. The complete genome sequence of Escherichia coli DH10B: insights into the biology of a laboratory workhorse. J. Bacteriol. 190:2597-2606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Etuaful, S., B. Carbonnelle, J. Grosset, S. Lucas, C. Horsfield, R. Phillips, M. Evans, D. Ofori-Adjei, E. Klustse, J. Owusu-Boateng, G. K. Amedofu, P. Awuah, E. Ampadu, G. Amofah, K. Asiedu, and M. Wansbrough-Jones. 2005. Efficacy of the combination rifampin-streptomycin in preventing growth of Mycobacterium ulcerans in early lesions of Buruli ulcer in humans. Antimicrob. Agents Chemother. 49:3182-3186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Faber, W. R., L. M. Arias-Bouda, J. E. Zeegelaar, A. H. Kolk, P. A. Fonteyne, J. Toonstra, and F. Portaels. 2000. First reported case of Mycobacterium ulcerans infection in a patient from China. Trans. R. Soc. Trop. Med. Hyg. 94:277-279. [DOI] [PubMed] [Google Scholar]
- 17.Galluzzi, L., and M. Karp. 2006. Whole cell strategies based on lux genes for high throughput applications toward new antimicrobials. Comb. Chem. High Throughput Screen. 9:501-514. [DOI] [PubMed] [Google Scholar]
- 18.Gavigan, J. A., J. A. Aínsa, E. Pérez, I. Otal, and C. Martín. 1997. Isolation by genetic labeling of a new mycobacterial plasmid, pJAZ38, from Mycobacterium fortuitum. J. Bacteriol. 179:4115-4122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.George, K. M., D. Chatterjee, G. Gunawardana, D. Welty, J. Hayman, R. Lee, and P. L. Small. 1999. Mycolactone: a polyketide toxin from Mycobacterium ulcerans required for virulence. Science 283:854-857. [DOI] [PubMed] [Google Scholar]
- 20.González-Flecha, B., and B. Demple. 1994. Intracellular generation of superoxide as a by-product of Vibrio harveyi luciferase expressed in Escherichia coli. J. Bacteriol. 176:2293-2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanahan, D. 1983. Studies on transformation of Escherichia coli with plasmids. J. Mol. Biol. 166:557-580. [DOI] [PubMed] [Google Scholar]
- 22.Hickey, M. J., T. M. Arain, R. M. Shawar, D. J. Humble, M. H. Langhorne, J. N. Morgenroth, and C. K. Stover. 1996. Luciferase in vivo expression technology: use of recombinant mycobacterial reporter strains to evaluate antimycobacterial activity in mice. Antimicrob. Agents Chemother. 40:400-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Howard, N. S., J. E. Gomez, C. Ko, and W. R. Bishai. 1995. Color selection with a hygromycin-resistance-based Escherichia coli-mycobacterial shuttle vector. Gene 166:181-182. [DOI] [PubMed] [Google Scholar]
- 24.Ji, B., S. Lefrançois, J. Robert, A. Chauffour, C. Truffot, and V. Jarlier. 2006. In vitro and in vivo activities of rifampin, streptomycin, amikacin, moxifloxacin, R207910, linezolid, and PA-824 against Mycobacterium ulcerans. Antimicrob. Agents Chemother. 50:1921-1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee, M. H., L. Pascopella, W. R. Jacobs, Jr., and G. F. Hatfull. 1991. Site-specific integration of mycobacteriophage L5: integration-proficient vectors for Mycobacterium smegmatis, Mycobacterium tuberculosis, and bacille Calmette-Guerin. Proc. Natl. Acad. Sci. U. S. A. 88:3111-3115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li, X. Z., and H. Nikaido. 2009. Efflux-mediated drug resistance in bacteria: an update. Drugs 69:1555-1623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Manabe, Y. C., C. L. Hatem, A. K. Kesavan, J. Durack, and J. R. Murphy. 2005. Both Corynebacterium diphtheriae DtxR(E175K) and Mycobacterium tuberculosis IdeR(D177K) are dominant positive repressors of IdeR-regulated genes in M. tuberculosis. Infect. Immun. 73:5988-5994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Marsollier, L., N. Honoré, P. Legras, A. L. Manceau, H. Kouakou, B. Carbonnelle, and S. T. Cole. 2003. Isolation of three Mycobacterium ulcerans strains resistant to rifampin after experimental chemotherapy of mice. Antimicrob. Agents Chemother. 47:1228-1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reference deleted.
- 30.Nienhuis, W. A., Y. Stienstra, W. A. Thompson, P. C. Awuah, K. M. Abass, W. Tuah, N. Y. Awua-Boateng, E. O. Ampadu, V. Siegmund, J. P. Schouten, O. Adjei, G. Bretzel, and T. S. van der Werf. 2010. Antimicrobial treatment for early, limited Mycobacterium ulcerans infection: a randomised controlled trial. Lancet 375:664-672. [DOI] [PubMed] [Google Scholar]
- 31.Pasca, M. R., P. Guglierame, F. Arcesi, M. Bellinzoni, E. De Rossi, and G. Riccardi. 2004. Rv2686c-Rv2687c-Rv2688c, an ABC fluoroquinolone efflux pump in Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 48:3175-3178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pedulla, M. L., M. H. Lee, D. C. Lever, and G. F. Hatfull. 1996. A novel host factor for integration of mycobacteriophage L5. Proc. Natl. Acad. Sci. U. S. A. 93:15411-15416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peña, C. E., J. E. Stoner, and G. F. Hatfull. 1996. Positions of strand exchange in mycobacteriophage L5 integration and characterization of the attB site. J. Bacteriol. 178:5533-5536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Picardeau, M., C. Le Dantec, and V. Vincent. 2000. Analysis of the internal replication region of a mycobacterial linear plasmid. Microbiology 146:305-313. [DOI] [PubMed] [Google Scholar]
- 35.Piddock, L. J., K. J. Williams, and V. Ricci. 2000. Accumulation of rifampicin by Mycobacterium aurum, Mycobacterium smegmatis and Mycobacterium tuberculosis. J. Antimicrob. Chemother. 45:159-165. [DOI] [PubMed] [Google Scholar]
- 36.Portaels, F., H. Traore, K. De Ridder, and W. M. Meyers. 1998. In vitro susceptibility of Mycobacterium ulcerans to clarithromycin. Antimicrob. Agents Chemother. 42:2070-2073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Portaels, F., M. T. Silva, and W. M. Meyers. 2009. Buruli ulcer. Clin. Dermatol. 27:291-305. [DOI] [PubMed] [Google Scholar]
- 38.Ramón-García, S., C. Martín, J. A. Aínsa, and E. De Rossi. 2006. Characterization of tetracycline resistance mediated by the efflux pump Tap from Mycobacterium fortuitum. J. Antimicrob. Chemother. 57:252-259. [DOI] [PubMed] [Google Scholar]
- 39.Roberts, E. A., A. Clark, and R. L. Friedman. 2005. Bacterial luciferase is naturally destabilized in Mycobacterium tuberculosis and can be used to monitor changes in gene expression. FEMS. Microbiol. Lett. 243:243-249. [DOI] [PubMed] [Google Scholar]
- 40.Rubin, E. J., B. J. Akerley, V. N. Novik, D. J. Lampe, R. N. Husson, and J. J. Mekalanos. 1999. In vivo transposition of mariner-based elements in enteric bacteria and mycobacteria. Proc. Natl. Acad. Sci. U. S. A. 96:1645-1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Snapper, S. B., R. E. Melton, S. Mustafa, T. Kieser, and W. R. Jacobs, Jr. 1990. Isolation and characterization of efficient plasmid transformation mutants of Mycobacterium smegmatis. Mol. Microbiol. 4:1911-1919. [DOI] [PubMed] [Google Scholar]
- 42.Snewin, V. A., M. P. Gares, P. O. Gaora, Z. Hasan, I. N. Brown, and D. B. Young. 1999. Assessment of immunity to mycobacterial infection with luciferase reporter constructs. Infect. Immun. 67:4586-4593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stinear, T., B. C. Ross, J. K. Davies, L. Marino, R. M. Robins-Browne, F. Oppedisano, A. Sievers, and P. D. Johnson. 1999. Identification and characterization of IS2404 and IS2606: two distinct repeated sequences for detection of Mycobacterium ulcerans by PCR. J. Clin. Microbiol. 37:1018-1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stinear, T. P., A. Mve-Obiang, P. L. Small, W. Frigui, M. J. Pryor, R. Brosch, G. A. Jenkin, P. D. Johnson, J. K. Davies, R. E. Lee, S. Adusumilli, T. Garnier, S. F. Haydock, P. F. Leadlay, and S. T. Cole. 2004. Giant plasmid-encoded polyketide synthases produce the macrolide toxin of Mycobacterium ulcerans. Proc. Natl. Acad. Sci. U. S. A. 101:1345-1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stinear, T. P., H. Hong, W. Frigui, M. J. Pryor, R. Brosch, T. Garnier, P. F. Leadlay, and S. T. Cole. 2005. Common evolutionary origin for the unstable virulence plasmid pMUM found in geographically diverse strains of Mycobacterium ulcerans. J. Bacteriol. 187:1668-1676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stinear, T. P., M. J. Pryor, J. L. Porter, and S. T. Cole. 2005. Functional analysis and annotation of the virulence plasmid pMUM001 from Mycobacterium ulcerans. Microbiology 151:683-692. [DOI] [PubMed] [Google Scholar]
- 47.Stinear, T. P., T. Seemann, S. Pidot, W. Frigui, G. Reysset, T. Garnier, G. Meurice, D. Simon, C. Bouchier, L. Ma, M. Tichit, J. L. Porter, J. Ryan, P. D. Johnson, J. K. Davies, G. A. Jenkin, P. L. Small, L. M. Jones, F. Tekaia, F. Laval, M. Daffé, J. Parkhill, and S. T. Cole. 2007. Reductive evolution and niche adaptation inferred from the genome of Mycobacterium ulcerans, the causative agent of Buruli ulcer. Genome. Res. 17:192-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stover, C. K., V. F. de la Cruz, T. R. Fuerst, J. E. Burlein, L. A. Benson, L. T. Bennett, G. P. Bansal, J. F. Young, M. H. Lee, G. F. Hatfull, S. B. Snapper, R. G. Barletta, W. R. Jacobs, Jr., and B. R. Bloom. 1991. New use of BCG for recombinant vaccines. Nature 351:456-460. [DOI] [PubMed] [Google Scholar]
- 49.Tullius, M. V., G. Harth, and M. A. Horwitz. 2001. High extracellular levels of Mycobacterium tuberculosis glutamine synthetase and superoxide dismutase in actively growing cultures are due to high expression and extracellular stability rather than to a protein-specific export mechanism. Infect. Immun. 69:6348-6363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tyagi, S., E. Nuermberger, T. Yoshimatsu, K. Williams, I. Rosenthal, N. Lounis, W. Bishai, and J. Grosset. 2005. Bactericidal activity of the nitroimidazopyran PA-824 in a murine model of tuberculosis. Antimicrob. Agents Chemother. 49:2289-2293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wansbrough-Jones, M., and R. Phillips. 2006. Buruli ulcer: emerging from obscurity. Lancet 367:1849-1858. [DOI] [PubMed] [Google Scholar]
- 52.Wards, B. J., and D. M. Collins. 1996. Electroporation at elevated temperatures substantially improves transformation efficiency of slow-growing mycobacteria. FEMS Microbiol. Lett. 145:101-105. [DOI] [PubMed] [Google Scholar]
- 53.Williamson, H. R., M. E. Benbow, K. D. Nguyen, D. C. Beachboard, R. K. Kimbirauskas, M. D. McIntosh, C. Quaye, E. O. Ampadu, D. Boakye, R. W. Merritt, and P. L. Small. 2008. Distribution of Mycobacterium ulcerans in Buruli ulcer endemic and non-endemic aquatic sites in Ghana. PLoS Negl. Trop. Dis. 2:e205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Zhang, Y., R. Lathigra, T. Garbe, D. Catty, and D. Young. 1991. Genetic analysis of superoxide dismutase, the 23 kilodalton antigen of Mycobacterium tuberculosis. Mol. Microbiol. 5:381-391. [DOI] [PubMed] [Google Scholar]