Abstract
H2 influenza viruses have not circulated in humans since 1968, and therefore a large segment of the population would likely be susceptible to infection should H2 influenza viruses reemerge. The development of an H2 pandemic influenza virus vaccine candidate should therefore be considered a priority in pandemic influenza preparedness planning. We selected a group of geographically and temporally diverse wild-type H2 influenza viruses and evaluated the kinetics of replication and compared the ability of these viruses to induce a broadly cross-reactive antibody response in mice and ferrets. In both mice and ferrets, A/Japan/305/1957 (H2N2), A/mallard/NY/1978 (H2N2), and A/swine/MO/2006 (H2N3) elicited the broadest cross-reactive antibody responses against heterologous H2 influenza viruses as measured by hemagglutination inhibition and microneutralization assays. These data suggested that these three viruses may be suitable candidates for development as live attenuated H2 pandemic influenza virus vaccines.
Influenza pandemics occur when a novel influenza virus enters a population with little preexisting immunity (36). During the pandemics of the last century, novel influenza viruses were introduced either directly from an avian reservoir (34) or were the result of reassortment between contemporaneously circulating human, avian, and swine influenza viruses (5, 29, 36). Due to the lack of preexisting immunity to the novel virus, morbidity and mortality rates are typically higher than in epidemics caused by seasonal influenza viruses (4).
Although pandemic preparedness planning has largely focused on the highly pathogenic H5 and H7 avian influenza virus subtypes, the recent emergence of the 2009 pandemic H1N1 viruses underscores the need to consider other influenza virus subtypes as well. Of the 16 hemagglutinin (HA) influenza A virus subtypes that have been identified to date, H1, H2, and H3 have been known to cause influenza pandemics (7, 27), suggesting that these viruses are capable of sustained transmission and can cause disease in humans. While the H1 and H3 subtypes have cocirculated in humans since 1977, H2 influenza viruses have not circulated in humans since 1968 (36) and therefore a large segment of the population would likely be susceptible to infection should H2 influenza viruses reemerge. The 1957 H2 pandemic virus was a reassortant that derived the HA, neuraminidase (NA), and PB1 genes from an avian virus and the remaining gene segments from the circulating H1N1 virus (15, 30). As H2 subtype viruses continue to circulate in avian reservoirs worldwide (12, 17, 18, 22, 33), they remain a potential pandemic threat. The development of an H2 influenza virus vaccine candidate should therefore be considered a priority in future pandemic influenza preparedness planning.
Given the low likelihood that a previously selected vaccine virus will exactly match the pandemic virus, the ability to elicit a broadly cross-reactive antibody response to antigenically distinct viruses within a subtype is an important consideration in the selection of a pandemic influenza vaccine candidate. Previous studies have examined the ability of inactivated H2 influenza viruses to provide cross-protection against mouse-adapted variants of reassortant human viruses and an avian H2 influenza virus from 1978 (9, 14). Given the potential for live attenuated influenza virus vaccines to confer a great breadth of heterologous cross-protection (1, 2, 6, 35), we recently conducted a study evaluating cold-adapted A/Ann Arbor/6/1960 (AA CA), an H2 influenza virus used as the backbone of the seasonal live attenuated influenza A virus vaccine currently licensed in the United States (3). However, as H2 influenza virus continues to circulate widely and appear in migratory birds (10, 24, 26), in poultry markets (20), and in swine (21), with evidence of interregional gene transmission (19, 22), a more extensive evaluation of recent isolates may be warranted in the selection of a potential H2 pandemic vaccine candidate.
H2 influenza viruses fall into three main lineages: a human lineage, a North American avian lineage, and a Eurasian avian lineage (29). In addition to viruses whose replicative ability in mammals has previously been established (11, 21, 23, 25), we selected a group of geographically and temporally diverse H2 influenza viruses from each lineage. We evaluated the kinetics of replication of each of these viruses in mice and ferrets and compared the abilities of these viruses to induce a broadly cross-reactive antibody response to determine which of these viruses would be suitable for further development as an H2 pandemic influenza vaccine candidate.
MATERIALS AND METHODS
Selection of viruses.
The H2 influenza viruses included in this study are listed in Table 1. Viruses were generously provided by Robert G. Webster, St. Jude Children's Research Hospital, Memphis, TN (A/mallard/Alberta/149/2002 [H2N4], A/chicken/NY/29878/1991 [H2N2], A/mallard/Potsdam/178-3/1983 [H2N2], A/pintail/Praimoric/695/1976 [H2N3], A/Berkeley/1/1968 [H2N2], A/Berlin/3/1964 [H2N2], and A/Krasnodar/101/1959 [H2N2]); Hiroshi Kida and Yoshiro Sakoda, Hokkaido University, Hokkaido, Japan (A/ruddy shelduck/Mongolia/28/2006 [H2N2], A/duck/Hokkaido/W259/2005 [H2N5], A/tern/Australia/1/2004 [H2N5], and A/duck/Hokkaido/107/2001 [H2N2]); Adolfo Garcia-Sastre, Mt. Sinai School of Medicine, New York, NY; and Juergen Richt, ARS-USDA, Ames, IA (A/Swine/MO/4296424/2006 [H2N3]).
TABLE 1.
H2 influenza viruses used in this study
| Virus | Subtype | Abbreviation |
|---|---|---|
| A/Japan/305/1957 | H2N2 | Jap/57 |
| A/Krasnodar/101/1959 | H2N2 | Kras/59 |
| A/Ann Arbor/6/1960 | H2N2 | AA/6/60 |
| A/Berlin/3/1964 | H2N2 | Berlin/64 |
| A/Berkeley/1/1968 | H2N2 | Berk/68 |
| A/pintail/Praimoric/695/1976 | H2N3 | pin/Prai/76 |
| A/mallard/New York/6750/1978 | H2N2 | mal/NY/78 |
| A/mallard/Potsdam/178-3/1983 | H2N2 | mal/Pots/83 |
| A/chicken/New York/29878/1991 | H2N2 | ck/NY/91 |
| A/duck/Hokkaido/107/2001 | H2N2 | dk/Hok/01 |
| A/mallard/Alberta/149/2002 | H2N4 | mal/Alb/02 |
| A/tern/Australia/1/2004 | H2N5 | tern/Aus/04 |
| A/duck/Hokkaido/W259/2006 | H2N5 | dk/Hok/05 |
| A/ruddy shelduck/Mongolia/28/2006 | H2N2 | dk/Mng/06 |
| A/swine/MO/4296424/2006 | H2N3 | sw/MO/06 |
Wild-type (WT) virus stocks were propagated in the allantoic cavities of 9- to 11-day-old specific-pathogen-free embryonated hen's eggs (Charles River Laboratories, Franklin, CT) at 37°C. Fifty percent tissue culture infective dose (TCID50) titers were determined in Madin-Darby canine kidney (MDCK) cells (ATCC, Manassas, VA). The cold-adapted A/Ann Arbor/6/60 (AA CA) virus was obtained from MedImmune. Fifty percent egg infective dose titers were determined in 9- to 11-day-old specific-pathogen-free embryonated eggs (Charles River Laboratories, Franklin, CT). Viral titers were calculated using the Reed and Muench method (28). All experiments were conducted in biosafety level 3 containment laboratories at the National Institutes of Health (NIH) approved for use by the Centers for Disease Control and Prevention.
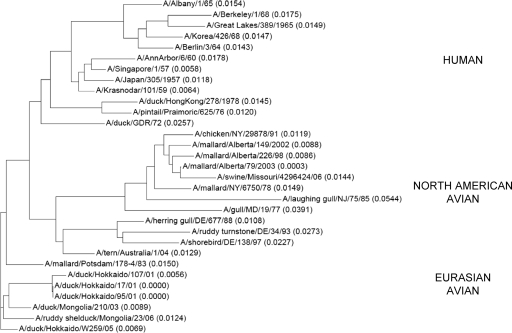
The HA genes of the 14 H2 viruses were obtained either from GenBank or by sequencing. Phylogenetic analysis was performed by a nonrooted neighbor-joining method using Vector NTI (Invitrogen). The phylogenetic distance from the nearest branch point is provided in parentheses for each sequence (see Fig. 1).
FIG. 1.
Phylogenetic analysis of HA1 amino acid sequences of human and avian H2 influenza virus isolates. The predicted HA1 (340 amino acids, including the signal peptides) sequences of 9 human and 22 avian isolates were used in the alignment and analyzed using Vector NTI. The phylogenetic tree was built using a nonrooted neighbor-joining method. The phylogenetic distance of each sequence from the nearest node was measured and is shown in parentheses.
Animals.
Four- to 6-week-old female BALB/c mice (Taconic Farms, Inc., Germantown, NY) were used in all mouse experiments. Ten- to 12-week-old ferrets (Triple F Farms, Sayre, PA) were used in the ferret studies. Animal experiments were approved by the NIH Animal Care and Use Committee.
Evaluation of viral replication in mice and ferrets.
In order to evaluate the kinetics of viral replication, groups of 20 4- to 6-week-old BALB/c mice were lightly anesthetized with isoflurane and intranasally inoculated with 50 μl containing 105 TCID50s of each of the 14 WT viruses. On days 1, 2, 3, 4, and 7 following inoculation, lungs, nasal turbinates, brains, and spleens were harvested from four mice in each group, weighed, and homogenized in L-15 medium (Invitrogen-GIBCO) containing an antibiotic-antimycotic mixture (penicillin, streptomycin, and amphotericin B; Invitrogen-GIBCO) to make 5% (wt/vol) (nasal turbinates, spleens) or 10% (wt/vol) (lungs, brains) tissue homogenates. Tissue homogenates were clarified by centrifugation and titrated in 24- and 96-well tissue culture plates containing MDCK cell monolayers. Viral titers were calculated using the Reed and Muench method (28) and expressed as log10 TCID50s per gram of tissue.
Once the H2 influenza viruses that elicited a cross-reactive antibody response against the greatest number of heterologous H2 viruses were established, we evaluated the replication kinetics of these selected viruses in ferrets in order to confirm that these viruses could be evaluated as potential vaccine candidates. Groups of three 10- to 12-week-old ferrets were lightly anesthetized with isoflurane and intranasally inoculated with 200 μl containing 107 TCID50s of Jap/57, mal/NY/78, and sw/MO/06 viruses. On day 3 following inoculation, the left lower lobe of the lung and the nasal turbinates were harvested and homogenized as described above; a 10% (wt/vol) tissue homogenate was utilized for both lung and nasal turbinate preparations.
Generation of antisera in mice and ferrets. (i) Mice.
Postinfection antiserum was generated in mice against each of the 14 WT H2 influenza viruses and the AA CA virus. Groups of five 4- to 6-week-old BALB/c mice were lightly anesthetized and intranasally inoculated with 50 μl containing 105 TCID50s of each of the WT H2 influenza viruses, except for the sw/MO/06 and AA CA viruses, and monitored for signs of morbidity and mortality for 14 days. Based on the observed lethality of the sw/MO/06 virus, two groups of five 4- to 6-week-old BALB/c mice were lightly anesthetized and intranasally inoculated with 50 μl containing 102 or 103 TCID50s of sw/MO/06. One group of mice received 106 TCID50s of the AA CA virus/50 μl. All of the mice were bled before administration of virus and at days 28, 43, and 56 postinfection (p.i.).
(ii) Ferrets.
Postinfection antiserum was generated in 10- to 12-week-old ferrets that were seronegative for antibodies to seasonal H3N2 and H1N1 influenza viruses. One ferret was used for each virus; each animal was lightly anesthetized with isoflurane and subsequently inoculated intranasally with 200 μl containing 107 TCID50s of one of the 14 WT viruses or the A/Ann Arbor/6/60 WT (AA WT) virus; the animals were monitored for signs of morbidity and mortality. All ferrets were bled before administration of virus, and serum was collected at days 14, 21, and 29 p.i.; the titer was determined at each time point. Three animals that achieved a hemagglutination inhibition (HAI) titer of ≥320 prior to day 39 were sacrificed; all other animals were sacrificed on day 39. Given the low HAI titers of the majority of the sera, we used an Amicon Ultra-15 Centrifugal Filter Device (Millipore, Billerica, MA) to concentrate the sera from each of the ferrets 2-fold. The concentrated ferret serum was also utilized in the microneutralization assays.
Evaluation of the cross-reactivity of antibody against homologous and heterologous H2 viruses. (i) HAI assays.
Antibody titers in postinfection mouse and ferret sera were determined by HAI assays. Sera were treated overnight with receptor-destroying enzyme (Denka Seiken Co., Ltd., Tokyo, Japan) and subsequently tested by standard methods using 4 HA units of virus and a 0.5% suspension of turkey erythrocytes or a 1% suspension of horse erythrocytes, as previously described (16, 31). HAI titers were recorded as the reciprocal of the highest dilution of serum that completely inhibited agglutination of erythrocytes by 4 HA units of the virus. The assessment of antigenic relatedness between influenza viruses is currently assessed using ferret antisera in HAI assays (16). A cross-reactive antibody response was defined as a <4-fold difference between the homologous HAI titer and the titer generated against a heterologous H2 influenza virus.
(ii) Neutralizing antibody assays.
Neutralizing antibody titers in pre- and postinfection sera were determined in a virus neutralization assay. Due to the low volume of serum collected from each individual mouse, sera from each group of mice were pooled for the neutralization assays. Serial 2-fold dilutions of heat-inactivated serum were prepared starting from a 1:10 or 1:20 dilution. Equal volumes of serum and virus were mixed and incubated for 60 min at room temperature. The residual infectivity of the virus-serum mixture was determined in MDCK cells in four replicates for each dilution. Neutralizing antibody titers were log2 transformed and defined as the reciprocal of the highest dilution of serum that completely neutralized the infectivity of 100 TCID50s of the virus as determined by the absence of a cytopathic effect at day 4.
RESULTS
Selection of viruses.
Based on phylogenetic analysis of the HA genes, three lineages of the H2 influenza virus subtype were identified: human, Eurasian avian, and North American avian (Fig. 1). Viruses were selected from each lineage to maximize temporal and geographic diversity. Six viruses were chosen from the human lineage, four viruses from the North American avian lineage, and five viruses from the Eurasian avian lineage. The HA amino acid sequence identities ranged from 86 to 99% (Table 2). The lowest sequence identity was seen in the comparison of Berk/68 with the avian viruses.
TABLE 2.
HA-1 amino acid sequence identity
| Virus | % Identity with: |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jap/57 | Kras/59 | Berlin/64 | AA/6/60 | Berk/68 | dk/Hok/ 05 | mal/Pots/ 83 | dk/ Mong/06 | pin/ Prai/76 | dk/ Hok/01 | mal/ Alb/02 | mal/ NY/78 | tern/ Aus/04 | sw/ MO/06 | ck/ NY/91 | |
| Jap/57 | 100 | ||||||||||||||
| Kras/59 | 99 | 100 | |||||||||||||
| Berlin/64 | 97 | 96 | 100 | ||||||||||||
| AA/6/60 | 96 | 96 | 95 | 100 | |||||||||||
| Berk/68 | 93 | 93 | 97 | 92 | 100 | ||||||||||
| dk/Hok/05 | 96 | 96 | 94 | 94 | 90 | 100 | |||||||||
| mal/Pots/83 | 96 | 96 | 94 | 94 | 90 | 98 | 100 | ||||||||
| dk/Mong/06 | 95 | 96 | 94 | 93 | 90 | 98 | 98 | 100 | |||||||
| pin/Prai/76 | 94 | 95 | 93 | 94 | 90 | 94 | 94 | 95 | 100 | ||||||
| dk/Hok/01 | 93 | 94 | 90 | 92 | 89 | 97 | 95 | 96 | 92 | 100 | |||||
| mal/Alb/02 | 93 | 93 | 91 | 89 | 86 | 93 | 93 | 94 | 93 | 89 | 100 | ||||
| mal/NY/78 | 93 | 93 | 91 | 90 | 86 | 93 | 94 | 94 | 93 | 89 | 98 | 100 | |||
| tern/Aus/04 | 92 | 93 | 89 | 90 | 88 | 97 | 95 | 96 | 92 | 96 | 91 | 92 | 100 | ||
| sw/MO/06 | 92 | 92 | 90 | 88 | 86 | 93 | 92 | 93 | 92 | 88 | 98 | 98 | 90 | 100 | |
| ck/NY/91 | 91 | 91 | 88 | 89 | 86 | 91 | 91 | 91 | 91 | 90 | 98 | 97 | 92 | 97 | 100 |
Replication kinetics in the respiratory tracts of mice.
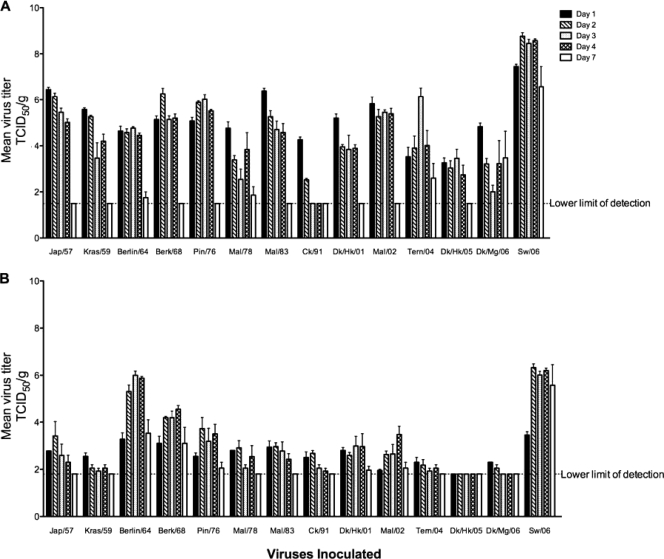
The kinetics of replication of each of the 14 WT viruses in mice are summarized in Fig. 2. All 14 viruses replicated in the lower respiratory tracts of mice, with peak replication in the lungs by day 3 that declined by day 7. Peak viral titers in the lower respiratory tract ranged from 103.5 TCID50s/g (dk/Hok/05) to 108.8 TCID50s/g (sw/MO/06). With the exception of sw/MO/06, dk/Mg/06, and tern/Aus/04, a significant amount of virus was not detected in the lower respiratory tract on day 7.
FIG. 2.
Levels of replication of H2 influenza viruses in the respiratory tracts of mice. Levels of replication of H2 influenza viruses in the lungs (A) and nasal turbinates (B) of mice following intranasal inoculation of the viruses indicated on days 1, 2, 3, 4, and 7 p.i. Virus titers are expressed as mean log10 TCID50s/g of tissue ± the standard error.
All viruses except dk/Hok/05 were detected in the upper respiratory tracts of mice. All viruses showed peak replication in the nasal turbinates by day 4 and were close to the limit of detection by day 7. For each of the 13 viruses that were detected in the upper respiratory tract, peak viral titers ranged from 102.6 TCID50s/g (Kras/59) to 106.3 TCID50s/g (sw/MO/06). Three viruses, sw/MO/06, Berlin/64, and Berk/68, were still detected in the nasal turbinates on day 7 p.i.
Lethality of H2 viruses for mice.
The sw/MO/06 virus was lethal for mice. Two of the four mice inoculated with 50 μl containing 105 TCID50s/ml sw/MO/06 that were to be sacrificed on day 7 p.i. succumbed by day 5 p.i. From a separate evaluation of lethality of sw/MO/06 virus in mice, the 50% lethal dose of sw/MO/06 was determined to be 102.5 TCID50s (data not shown).
Replication kinetics of selected H2 influenza viruses in the respiratory tracts of ferrets.
Both the Jap/57 and sw/MO/06 viruses replicated well, and both were detected in the respiratory tracts of all ferrets. Jap/57 replicated to mean titers of 107 TCID50s/g in the upper respiratory tract and 105.9 TCID50s/g in the lower respiratory tract; sw/MO/06 replicated to mean titers of 107.5 TCID50s/g in the upper respiratory tract and 105.9 TCID50s/g in the lower respiratory tract. The mal/NY/78 virus was not detected in the lower respiratory tract but replicated to a mean titer of 105.9 TCID50s/g in the upper respiratory tract.
Cross-reactive antibodies to homologous and heterologous H2 influenza viruses in ferrets and mice. (i) Ferrets.
Homologous HAI titers from postinfection ferret sera were determined using both turkey and horse erythrocyte suspensions. Postinfection sera generated from animals inoculated with human influenza viruses AA WT, Berlin/64, and Kras/59 did not bind in an HAI using horse erythrocytes, presumably because these viruses have a preference for sialic acid receptors containing N-acetylneuraminic acid α2,6-galactose (SA α2,6Gal) linkages. Among the other viruses, a 2- to 4-fold higher titer was observed when horse erythrocytes were used instead of turkey erythrocytes. Horse erythrocytes were therefore used for the cross-HAI assays (Table 3). Jap/57, mal/NY/78, dk/Hok/05, and sw/MO/06 elicited a cross-reactive antibody response against the greatest number of heterologous H2 viruses. Due to the lack of binding to horse erythrocytes, postinfection sera generated from ferrets inoculated with AA WT, Berlin/64, and Kras/59 were not tested in the cross-HAI assay.
TABLE 3.
Cross-reactivity of postinfection ferret sera against selected H2 viruses in an HAI assaya
| Virus | Ferret antiserum titer in HAI assay |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jap/57b | Kras/59 | AA/6/60 | Berlin/64 | Berk/68 | pin/Prai/76 | mal/NY/78 | mal/Pot/ 83b | ck/NY/91 | dk/ Hok/01 | mal/Alb/02 | tern/Aus/04 | dk/ Hok/05 | dk/Mng/ 06b | sw/MO/ 06b | H2 reference serumc | |
| Jap/57 | 2,560 | 320 | 40 | 320 | 160 | 1,280 | 640 | 640 | 160 | 320 | 320 | 320 | 640 | 1,280 | 320 | 3,840 |
| Kras/59 | NDd | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| AA/6/60 | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| Berlin/64 | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND | ND |
| Berk/68 | 640 | 80 | 20 | 1,280 | 2,560 | 40 | 40 | 80 | 80 | 80 | 40 | 40 | 40 | 1,280 | 320 | 960 |
| pin/Prai/76 | 1,280 | 1,280 | 10 | 1,280 | 20 | 1,280 | 640 | 320 | 160 | 320 | 320 | 320 | 320 | 2,560 | 5,120 | 3,840 |
| mal/NY/78 | 1,280 | 80 | 20 | 80 | 40 | 160 | 640 | 640 | 160 | 160 | 160 | 640 | 320 | 640 | 1,280 | 2,560 |
| mal/Pots/83 | 1,280 | 320 | 20 | 320 | 40 | 160 | 640 | 1,280 | 160 | 640 | 320 | 320 | 640 | 320 | 1,280 | 2,560 |
| ck/NY/91 | 640 | 80 | 16 | 80 | 20 | 80 | 640 | 320 | 640 | 80 | 160 | 160 | 320 | 320 | 640 | 1,920 |
| dk/Hok/01 | 1,280 | 160 | 16 | 160 | 80 | 1,280 | 1,280 | 320 | 320 | 1,280 | 160 | 640 | 1,280 | 2,560 | 2,560 | 7,680 |
| mal/Alb/02 | 640 | 80 | 10 | 20 | 10 | 320 | 320 | 320 | 160 | 320 | 1,280 | 640 | 320 | 320 | 1,280 | 2,560 |
| tern/Aus/04 | 2,560 | 320 | 20 | 180 | 320 | 640 | 2,560 | 640 | 320 | 640 | 320 | 2,560 | 640 | 1,280 | 2,560 | 3,840 |
| dk/Hok/05 | 640 | 80 | 20 | 40 | 80 | 160 | 640 | 320 | 160 | 160 | 160 | 320 | 640 | 320 | 640 | 5,120 |
| dk/Mng/06 | 2,560 | 320 | 32 | 160 | 80 | 640 | 1,280 | 320 | 320 | 640 | 320 | 1,280 | 640 | 2,560 | 2,560 | 5,120 |
| sw/MO/06 | 1,260 | 160 | 16 | 20 | 40 | 640 | 640 | 320 | 640 | 640 | 320 | 320 | 640 | 640 | 2,560 | 5,120 |
Homologous titers are in bold; 4-fold-or-greater differences in titer are underlined. The lower limit of detection was assigned a value of 10. One percent horse erythrocytes were used. Ferret antisera were generated against the viruses indicated.
Antiserum with cross-neutralizing antibody to the greatest number of heterologous H2 subtype influenza viruses.
Hyperimmune goat antiserum against A/Singapore/1/57 (H2N2) was used as the reference antiserum.
ND, not done.
In addition, cross-reactivity was determined with microneutralization assays using all 14 H2 influenza viruses (Table 4). Prior studies have considered a neutralizing antibody titer that was 4-fold lower than the homologous neutralizing antibody response to be indicative of (i) a significant lack of cross-reactivity or (ii) an antigenic difference (8). In general, we noted a variable degree of concordance (58%) between the viruses that were assessed by both cross-HAI and cross-neutralization assays (summarized in Table 5). However, the Jap/57, mal/NY/78, and sw/MO/06 viruses, which were among the viruses that elicited a cross-reactive antibody response against the greatest number of heterologous H2 viruses, also demonstrated a high degree of concordance (>67%) in both assays. In contrast to the results of the HAI assay, the dk/Hok/05 virus did not appear to elicit a broadly cross-reactive neutralizing antibody response to a large number of heterologous H2 influenza viruses.
TABLE 4.
Cross-reactivity of postinfection ferret sera against selected H2 viruses in a neutralization assaya
| Virus | Ferret antiserum titer in neutralization assay |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jap/57b | Kras/59 | AA/6/60 | Berlin/64 | Berk/68 | pin/Prai/76 | mal/NY/78b | mal/Pot/83b | ck/NY/91b | dk/Hok/01b | mal/Alb/02 | tern/Aus/04 | dk/ Hok/05 | dk/ Mng/06 | sw/MO/06b | |
| Jap/57 | 403 | 113 | 10 | 32 | 20 | 160 | 254 | 226 | 80 | 160 | 254 | 254 | 806 | 640 | 1,280 |
| Kras/59 | 905 | 160 | 40 | 40 | 10 | 127 | 806 | 403 | 10 | 160 | 254 | 40 | 160 | 640 | 1,575 |
| AA/6/60 | 640 | 80 | 160 | 57 | 60 | 202 | 320 | 202 | 63 | 80 | 113 | 453 | 226 | 202 | 806 |
| Berlin/64 | 226 | 10 | 160 | 113 | 10 | 403 | 320 | 320 | 10 | 320 | 226 | 226 | 160 | 28 | 463 |
| Berk/68 | 101 | 40 | 63 | 226 | 1,016 | 10 | 32 | 28 | 10 | 25 | 10 | 40 | 25 | 50 | 127 |
| pin/Prai/76 | 1,613 | 10 | 40 | 10 | 10 | 806 | 640 | 254 | 160 | 113 | 254 | 453 | 508 | 508 | 1,613 |
| mal/NY/78 | 640 | 101 | 40 | 28 | 10 | 226 | 905 | 640 | 127 | 113 | 226 | 160 | 508 | 254 | 1,810 |
| mal/Pots/83 | 806 | 80 | 57 | 28 | 20 | 100 | 508 | 453 | 101 | 160 | 113 | 160 | 640 | 403 | 1,280 |
| ck/NY/91 | 453 | 57 | 32 | 10 | 80 | 160 | 403 | 160 | 905 | 113 | 254 | 226 | 453 | 160 | 1,810 |
| dk/Hok/01 | 905 | 101 | 57 | 16 | 25 | 198 | 453 | 202 | 101 | 320 | 226 | 226 | 451 | 226 | 1,810 |
| mal/Alb/02 | 1,016 | 40 | 25 | 28 | 20 | 202 | 640 | 226 | 320 | 320 | 254 | 226 | 508 | 403 | 1,280 |
| tern/Aus/04 | 905 | 101 | 57 | 25 | 10 | 226 | 508 | 403 | 101 | 226 | 226 | 905 | 508 | 403 | 1,016 |
| dk/Hok/05 | 6,451 | 226 | 32 | 127 | 101 | 202 | 3,225 | 905 | 403 | 320 | 226 | 453 | 4,064 | 806 | 5,120 |
| dk/Mng/06 | 1,611 | 127 | 57 | 63 | 28 | 453 | 806 | 403 | 254 | 226 | 202 | 806 | 505 | 640 | 1,280 |
| sw/MO/06 | 1,280 | 80 | 10 | 28 | 16 | 160 | 1,280 | 254 | 202 | 127 | 202 | 111 | 1,280 | 403 | 2,032 |
Homologous titers are in bold; 4-fold-or-greater differences in titer are underlined. The lower limit of detection was assigned a value of 10. Ferret antisera were generated against the viruses indicated.
Antiserum with cross-neutralizing antibody to the greatest number of heterologous H2 subtype influenza viruses.
TABLE 5.
Concordance of results from neutralization and HAI assays using postinfection ferret antiseraa
| Virus | Concordance with ferret antiserum against: |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jap/57b | Kras/59 | AA/6/60 | Berlin/64 | Berk/68 | pin/Prai/76 | mal/NY/78b | mal/Pot/83 | ck/NY/91 | dk/ Hok/01 | mal/Alb/02 | tern/Aus/04 | dk/ Hok/05 | dk/ Mng/06 | sw/MO/06b | |
| A/Jap/57 | + | + | + | + | + | − | + | + | + | − | − | − | − | + | − |
| A/Kras/59 | NAc | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| A/AA/6/60 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| A/Berlin/64 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| A/Berk/68 | − | − | + | + | + | + | + | + | + | + | + | + | + | − | + |
| A/pin/Prai/76 | + | − | − | − | + | + | + | − | + | − | − | − | − | + | + |
| A/mal/NY/78 | + | + | − | − | + | − | + | + | + | − | − | + | − | − | + |
| A/mal/Pots/83 | + | + | + | − | + | + | + | + | + | + | − | + | − | + | + |
| A/ck/NY/91 | − | + | − | − | + | + | + | − | + | − | − | + | − | + | − |
| A/dk/Hok/01 | + | + | + | − | + | − | + | − | + | + | − | + | − | + | + |
| A/mal/Alb/02 | − | − | − | − | + | − | + | − | − | − | + | + | − | − | + |
| A/tern/Aus/04 | + | + | + | − | + | + | + | + | − | + | − | + | − | + | + |
| A/dk/Hok/05 | + | + | − | + | + | − | + | − | − | − | − | − | + | − | − |
| A/dk/Mng/06 | + | + | + | + | + | + | + | − | + | + | − | + | − | + | + |
| A/sw/MO/06 | + | + | − | − | + | − | + | − | − | + | − | + | + | + | + |
A plus sign indicates concordant results; a minus sign indicates discordant results. No HAI data were available for Kras/59, AA/6/60, and Berlin/64, as 1% horse erythrocytes were used in the HAI assay. Ferret antisera were generated against the viruses indicated.
Antiserum with cross-neutralizing antibody detected by both assays to the greatest number of heterologous H2 subtype influenza viruses.
NA, HAI data not available.
(ii) Mice.
In mice, antigenic cross-reactivity among the selected viruses was assessed using titers from a microneutralization assay; these results are summarized in Table 6. An HAI assay was not performed with mouse sera, given that a larger volume of mouse sera would have been required for the HAI assay than for the microneutralization assay. The Jap/57, Kras/59, mal/NY/78, mal/Pots/83, and sw/MO/06 viruses elicited the most broadly cross-reactive antibodies against heterologous H2 influenza viruses. The concordance between the cross-neutralization titers using postinfection sera from mice and ferrets is displayed in Table 7; overall, approximately 70% concordance was noted between the ferret and mouse neutralization assay results. Of the H2 viruses studied, Jap/57, mal/NY/78, and sw/MO/06 elicited a cross-reactive antibody response against the greatest number of heterologous H2 influenza viruses in both mice and ferrets.
TABLE 6.
Cross-reactivity of postinfection mouse sera against selected H2 viruses in a neutralization assaya
| Virus | Titer of mouse serum in neutralization assay |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jap/57b | Kras/59b | AA/6/ 60 | Berlin/64 | Berk/68 | pin/Prai/ 76 | mal/NY/ 78b | mal/Pot/ 83b | ck/ NY/91 | dk/ Hok/01 | mal/ Alb/02 | tern/ Aus/04 | dk/ Hok/05 | dk/ Mng/06 | sw/MO/ 06b | |
| Jap/57 | 320 | 32 | 20 | 226 | 40 | 28 | 202 | 202 | 113 | 80 | 226 | 10 | 10 | 20 | 381 |
| Kras/59 | 254 | 80 | 20 | 40 | 10 | 32 | 254 | 226 | 10 | 80 | 101 | 40 | 320 | 254 | 453 |
| AA/6/60 | 101 | 80 | 50 | 113 | 453 | 10 | 40 | 32 | 10 | 10 | 10 | 16 | 40 | 10 | 16 |
| Berlin/64 | 32 | 320 | 16 | 202 | 40 | 10 | 10 | 16 | 20 | 16 | 28 | 28 | 10 | 57 | 10 |
| Berk/68 | 20 | 320 | 10 | 226 | 453 | 10 | 10 | 10 | 10 | 10 | 16 | 10 | 10 | 25 | 10 |
| pin/Prai/76 | 160 | 80 | 10 | 40 | 10 | 57 | 113 | 63 | 10 | 57 | 80 | 10 | 320 | 254 | 453 |
| mal/NY/78 | 202 | 320 | 10 | 10 | 10 | 20 | 226 | 127 | 10 | 80 | 254 | 10 | 453 | 32 | 202 |
| mal/Pots/83 | 254 | 160 | 10 | 16 | 10 | 25 | 202 | 113 | 10 | 50 | 50 | 10 | 202 | 63 | 226 |
| ck/NY/91 | 127 | 127 | 10 | 28 | 10 | 40 | 160 | 113 | 226 | 50 | 226 | 20 | 226 | 63 | 806 |
| dk/Hok/01 | 160 | 127 | 10 | 32 | 10 | 16 | 202 | 113 | 101 | 113 | 101 | 10 | 135 | 63 | 640 |
| mal/Alb/02 | 202 | 63 | 10 | 16 | 10 | 28 | 160 | 101 | 10 | 32 | 254 | 10 | 67 | 127 | 508 |
| tern/Aus/04 | 101 | 63 | 10 | 16 | 10 | 10 | 63 | 32 | 10 | 20 | 63 | 113 | 67 | 127 | 50 |
| dk/Hok/05 | 805 | 113 | 25 | 127 | 16 | 50 | 453 | 113 | 16 | 202 | 226 | 226 | 160 | 226 | 1,280 |
| dk/Mng/06 | 320 | 320 | 10 | 63 | 20 | 50 | 226 | 160 | 202 | 101 | 160 | 10 | 320 | 2,032 | 640 |
| sw/MO/06 | 160 | 127 | 10 | 16 | 16 | 25 | 127 | 101 | 28 | 101 | 101 | 10 | 160 | 113 | 806 |
Homologous titers are in bold; 4-fold-or-greater differences in titer are underlined. The lower limit of detection was assigned a value of 10. Mouse antisera were generated against the viruses indicated.
Antiserum with cross-neutralizing antibody to the greatest number of heterologous H2 subtype influenza viruses.
TABLE 7.
Concordance of neutralization titers between mouse and ferret antiseraa
| Virus | Concordance with antiserum against: |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jap/57b | Kras/59 | AA/6/60 | Berlin/64 | Berk/68 | pin/Prai/76 | mal/NY/ 78b | mal/ Pot/83 | ck/ NY/91 | dk/ Hok/01 | mal/Alb/02 | tern/Aus/04 | dk/ Hok/05 | dk/ Mng/06 | sw/MO/ 06b | |
| Jap/57 | + | + | + | + | + | − | + | + | − | + | + | − | + | − | + |
| Kras/59 | + | + | − | − | + | − | + | + | + | + | + | − | − | − | + |
| AA/6/60 | + | + | + | + | − | − | − | + | + | + | − | − | + | − | − |
| Berlin/64 | − | − | − | + | + | − | − | − | + | − | − | − | + | + | + |
| Berk/68 | − | − | + | + | + | + | − | + | + | + | + | + | + | + | + |
| pin/Prai/76 | + | − | − | + | + | + | + | + | + | + | + | − | − | − | + |
| mal/NY/78 | + | + | − | + | + | + | + | + | + | + | + | + | − | − | + |
| mal/Pots/83 | + | + | + | + | + | − | + | + | + | + | − | + | − | + | + |
| ck/NY/91 | + | + | − | + | + | − | + | + | + | + | + | + | − | + | + |
| dk/Hok/01 | + | + | + | + | + | − | + | + | − | + | + | + | − | − | + |
| mal/Alb/02 | + | − | − | + | + | + | + | + | − | + | + | + | − | − | + |
| tern/Aus/04 | + | + | + | + | + | − | + | + | + | − | − | + | − | − | − |
| dk/Hok/05 | − | + | − | − | + | + | + | + | − | + | + | + | + | − | + |
| dk/Mng/06 | + | + | + | − | + | + | + | + | + | + | + | − | − | + | + |
| sw/MO/06 | + | + | − | + | + | + | + | + | + | + | + | + | + | − | + |
A plus sign indicates concordant results; a minus sign indicates discordant results. Antisera were generated against the viruses indicated.
Antiserum with cross-neutralizing antibody detected by all assays to the greatest number of heterologous H2 subtype influenza viruses.
DISCUSSION
The potential for an H2 influenza pandemic exists because the number of individuals susceptible to H2 influenza virus increases as more time elapses since the last circulation of this subtype in humans and because H2 influenza viruses continue to circulate in avian reservoirs. Thus, developing an H2 influenza virus vaccine candidate should remain a priority in pandemic influenza preparedness planning. Given the potential advantage of broader heterologous immunity conferred by live attenuated influenza virus vaccines (1, 2, 6, 35), we selected a number of H2 influenza viruses as potential live attenuated H2 pandemic influenza vaccine candidates.
The ability of the virus to replicate in the respiratory tract is an essential feature in the preclinical evaluation of a live attenuated vaccine candidate. Therefore, we first evaluated the ability of each of the selected H2 viruses to replicate in the mouse respiratory tract. The replication kinetics of the H2 influenza viruses were comparable to the replication kinetics of the H6 and H7 influenza viruses noted in mice (8, 13). Similar to the replication kinetics of the other influenza virus subtypes, the majority of the H2 influenza viruses replicated to peak titers by day 4 and declined by day 7 in both the upper and lower respiratory tracts. Without prior host adaptation, nearly all of the H2 influenza viruses replicated well in the upper and lower respiratory tracts of mice and therefore all 14 viruses were included in our assessment of immunogenicity and cross-reactivity.
As it is unlikely that any vaccine seed virus prepared ahead of a pandemic will exactly match the pandemic virus, the ideal seed virus for a pandemic vaccine would elicit broadly cross-reactive antibodies against as many antigenically distinct viruses within a subtype as possible. We carried out a study to identify which H2 influenza viruses would elicit the most broadly cross-reactive antibody response against heterologous H2 viruses. As the AA CA virus is the backbone of the live attenuated seasonal influenza vaccine currently licensed in the United States and thus would be an ideal H2 pandemic vaccine candidate, it was included in the viruses that were selected. Although the AA CA virus did not induce antibodies that were as broadly cross-reactive as other H2 influenza viruses that were evaluated, the AA CA virus elicited antibodies that were cross-reactive in neutralization assays in both ferrets and mice against viruses such as Berlin/64 and Berk/68 that could potentially reemerge.
We utilized both HAI and virus neutralization assays to determine which viruses were able to elicit the most broadly cross-reactive antibody responses against heterologous viruses. We observed that an HAI assay alone was not sufficient to determine cross-reactivity among the entire group of H2 influenza viruses because avian and human influenza viruses have different sialic acid binding preferences. Although the HAI assay using ferret antisera has been the standard in the assessment of antigenic relatedness of seasonal influenza vaccines, discrepant results obtained with turkey and horse erythrocytes have been noted (13, 31, 32). Specifically, we observed that several avian viruses, which often preferentially bind sialic acids containing N-acetylneuraminic acid α2,3-galactose (SA α2,3Gal) linkages, agglutinated horse erythrocytes but did not agglutinate turkey erythrocytes, which contain both SA α2,3Gal and SA α2,6 Gal linkages. As reported by Joseph et al. (13), we noted that among the avian viruses that agglutinated both turkey and horse erythrocytes, the titers achieved were 2- to 5-fold higher with horse erythrocytes than with turkey erythrocytes. In contrast, several human H2 viruses, which preferentially bind SA α2,6Gal linkages, did not agglutinate horse erythrocytes, which exclusively bear SA α2,3Gal linkages. We thus also conducted cross-neutralization assays to examine antibody cross-reactivity among all selected viruses.
In previous studies, variable concordance between HAI and neutralization assays and between mouse and ferret antisera have been noted (8, 13, 32), suggesting that both assays and animal models are needed to comprehensively assess antigenic relatedness among a group of influenza viruses. Similarly, in this study, we noted a variable degree of concordance between the use of ferret and mouse antisera in HAI and neutralization assays. In ferrets, although variable concordance existed among the viruses that were assessed by both HAI and neutralization assay, a significant degree of concordance was observed among Jap/57, mal/NY/78, and sw/MO/06, the viruses that elicited the most broadly cross-reactive antibody against heterologous H2 influenza viruses, as measured by both assays. A similarly high degree of concordance was noted in the cross-neutralization assays—Jap/57, mal/NY/78, and sw/MO/06 elicited the broadest cross-reactive antibody response against heterologous H2 influenza viruses in mice, as well as ferrets. Therefore, we conclude that these three viruses are suitable candidates for the development of live attenuated vaccines to protect against H2 influenza virus subtypes. Given the recent isolation of sw/MO/06 and features of the virus that suggest it is capable of sustained transmission in mammals without prior adaptation (21), this virus may be the most rational candidate to further evaluate in additional preclinical studies.
Acknowledgments
This work was supported by the Intramural Research Program of the NIH and the National Institute of Allergy and Infectious Diseases (NIAID). This research was performed as part of a cooperative research and development agreement between the Laboratory of Infectious Diseases, NIAID, and MedImmune.
H.J. and G.K. are employees of MedImmune, the manufacturer of seasonal live attenuated influenza virus vaccine.
We thank Jadon Jackson for his outstanding technical support. We also thank Robert Webster, Hiroshi Kida, Yoshiro Sakoda, Adolfo García-Sastre, and Juergen Richt for providing WT viruses. We thank Dan Ye and Bin Lu for sequence analysis.
Footnotes
Published ahead of print on 26 May 2010.
REFERENCES
- 1.Armerding, D., H. Rossiter, I. Ghazzouli, and E. Liehl. 1982. Evaluation of live and inactivated influenza A virus vaccines in a mouse model. J. Infect. Dis. 145:320-330. [DOI] [PubMed] [Google Scholar]
- 2.Belshe, R. B., K. L. Nichol, S. B. Black, H. Shinefield, J. Cordova, R. Walker, C. Hessel, I. Cho, and P. M. Mendelman. 2004. Safety, efficacy, and effectiveness of live, attenuated, cold-adapted influenza vaccine in an indicated population aged 5-49 years. Clin. Infect. Dis. 39:920-927. [DOI] [PubMed] [Google Scholar]
- 3.Chen, G. L., E. W. Lamirande, H. Jin, G. Kemble, and K. Subbarao. 2010. Safety, immunogenicity, and efficacy of a cold-adapted A/Ann Arbor/6/60 (H2N2) vaccine in mice and ferrets. Virology 398:109-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cox, N. J., and K. Subbarao. 2000. Global epidemiology of influenza: past and present. Annu. Rev. Med. 51:407-421. [DOI] [PubMed] [Google Scholar]
- 5.Dawood, F. S., S. Jain, L. Finelli, M. W. Shaw, S. Lindstrom, R. J. Garten, L. V. Gubareva, X. Xu, C. B. Bridges, and T. M. Uyeki. 2009. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N. Engl. J. Med. 360:2605-2615. [DOI] [PubMed] [Google Scholar]
- 6.Delem, A. 1977. Protective efficacy of RIT 4025, a live attenuated influenza vaccine strain, and evaluation of heterotypic immunity to influenza A viruses in ferrets. J. Hyg. (Lond.) 79:203-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dowdle, W. R. 1999. Influenza A virus recycling revisited. Bull. World Health Organ. 77:820-828. [PMC free article] [PubMed] [Google Scholar]
- 8.Gillim-Ross, L., C. Santos, Z. Chen, A. Aspelund, C. F. Yang, D. Ye, H. Jin, G. Kemble, and K. Subbarao. 2008. Avian influenza h6 viruses productively infect and cause illness in mice and ferrets. J. Virol. 82:10854-10863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Govorkova, E. A., and A. Smirnov Yu. 1997. Cross-protection of mice immunized with different influenza A (H2) strains and challenged with viruses of the same HA subtype. Acta Virol. 41:251-257. [PubMed] [Google Scholar]
- 10.Hatchette, T. F., D. Walker, C. Johnson, A. Baker, S. P. Pryor, and R. G. Webster. 2004. Influenza A viruses in feral Canadian ducks: extensive reassortment in nature. J. Gen. Virol. 85:2327-2337. [DOI] [PubMed] [Google Scholar]
- 11.Hinshaw, V. S., R. G. Webster, B. C. Easterday, and W. J. Bean, Jr. 1981. Replication of avian influenza A viruses in mammals. Infect. Immun. 34:354-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jonassen, C. M., and K. Handeland. 2007. Avian influenza virus screening in wild waterfowl in Norway, 2005. Avian Dis. 51:425-428. [DOI] [PubMed] [Google Scholar]
- 13.Joseph, T., J. McAuliffe, B. Lu, H. Jin, G. Kemble, and K. Subbarao. 2007. Evaluation of replication and pathogenicity of avian influenza A H7 subtype viruses in a mouse model. J. Virol. 81:10558-10566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaverin, N. V., Y. A. Smirnov, E. A. Govorkova, I. A. Rudneva, A. K. Gitelman, A. S. Lipatov, N. L. Varich, S. S. Yamnikova, N. V. Makarova, R. G. Webster, and D. K. Lvov. 2000. Cross-protection and reassortment studies with avian H2 influenza viruses. Arch. Virol. 145:1059-1066. [DOI] [PubMed] [Google Scholar]
- 15.Kawaoka, Y., S. Krauss, and R. G. Webster. 1989. Avian-to-human transmission of the PB1 gene of influenza A viruses in the 1957 and 1968 pandemics. J. Virol. 63:4603-4608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kendal, A. P., M. S. Pereira, and J. J. Skehel. 1982. Concepts and procedures for laboratory-based influenza surveillance. World Health Organization, Geneva, Switzerland.
- 17.Kishida, N., Y. Sakoda, M. Shiromoto, G. R. Bai, N. Isoda, A. Takada, G. Laver, and H. Kida. 2008. H2N5 influenza virus isolates from terns in Australia: genetic reassortants between those of the Eurasian and American lineages. Virus Genes 37:16-21. [DOI] [PubMed] [Google Scholar]
- 18.Krauss, S., C. A. Obert, J. Franks, D. Walker, K. Jones, P. Seiler, L. Niles, S. P. Pryor, J. C. Obenauer, C. W. Naeve, L. Widjaja, R. J. Webby, and R. G. Webster. 2007. Influenza in migratory birds and evidence of limited intercontinental virus exchange. PLoS Pathog. 3:e167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu, J. H., K. Okazaki, G. R. Bai, W. M. Shi, A. Mweene, and H. Kida. 2004. Interregional transmission of the internal protein genes of H2 influenza virus in migratory ducks from North America to Eurasia. Virus Genes 29:81-86. [DOI] [PubMed] [Google Scholar]
- 20.Liu, M., S. He, D. Walker, N. Zhou, D. R. Perez, B. Mo, F. Li, X. Huang, R. G. Webster, and R. J. Webby. 2003. The influenza virus gene pool in a poultry market in South Central China. Virology 305:267-275. [DOI] [PubMed] [Google Scholar]
- 21.Ma, W., A. L. Vincent, M. R. Gramer, C. B. Brockwell, K. M. Lager, B. H. Janke, P. C. Gauger, D. P. Patnayak, R. J. Webby, and J. A. Richt. 2007. Identification of H2N3 influenza A viruses from swine in the United States. Proc. Natl. Acad. Sci. U. S. A. 104:20949-20954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Makarova, N. V., N. V. Kaverin, S. Krauss, D. Senne, and R. G. Webster. 1999. Transmission of Eurasian avian H2 influenza virus to shorebirds in North America. J. Gen. Virol. 80(Pt. 12):3167-3171. [DOI] [PubMed] [Google Scholar]
- 23.Monto, A. S., and F. Olazabal, Jr. 1966. Asian influenza in the Panama Canal zone: isolation of a virus variant and protective effect of a vaccine containing A2/Japan/305/57. Am. J. Epidemiol. 83:101-112. [DOI] [PubMed] [Google Scholar]
- 24.Munster, V. J., C. Baas, P. Lexmond, J. Waldenstrom, A. Wallensten, T. Fransson, G. F. Rimmelzwaan, W. E. Beyer, M. Schutten, B. Olsen, A. D. Osterhaus, and R. A. Fouchier. 2007. Spatial, temporal, and species variation in prevalence of influenza A viruses in wild migratory birds. PLoS Pathog. 3:e61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Murphy, B. R., V. S. Hinshaw, D. L. Sly, W. T. London, N. T. Hosier, F. T. Wood, R. G. Webster, and R. M. Chanock. 1982. Virulence of avian influenza A viruses for squirrel monkeys. Infect. Immun. 37:1119-1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Okazaki, K., A. Takada, T. Ito, M. Imai, H. Takakuwa, M. Hatta, H. Ozaki, T. Tanizaki, T. Nagano, A. Ninomiya, V. A. Demenev, M. M. Tyaptirganov, T. D. Karatayeva, S. S. Yamnikova, D. K. Lvov, and H. Kida. 2000. Precursor genes of future pandemic influenza viruses are perpetuated in ducks nesting in Siberia. Arch. Virol. 145:885-893. [DOI] [PubMed] [Google Scholar]
- 27.Potter, C. W. 1998. Chronicle of influenza pandemics, p. 3-18. In K. Nicholson, R. G. Webster, and A. J. Hay (ed.), Textbook of influenza. Blackwell Science, Oxford, United Kingdom.
- 28.Reed, L. J., and H. Muench. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 29.Schäfer, J. R., Y. Kawaoka, W. J. Bean, J. Süss, D. Senne, and R. G. Webster. 1993. Origin of the pandemic 1957 H2 influenza A virus and the persistence of its possible progenitors in the avian reservoir. Virology 194:781-788. [DOI] [PubMed] [Google Scholar]
- 30.Scholtissek, C., W. Rohde, V. Von Hoyningen, and R. Rott. 1978. On the origin of the human influenza virus subtypes H2N2 and H3N2. Virology 87:13-20. [DOI] [PubMed] [Google Scholar]
- 31.Stephenson, I., J. M. Wood, K. G. Nicholson, and M. C. Zambon. 2003. Sialic acid receptor specificity on erythrocytes affects detection of antibody to avian influenza haemagglutinin. J. Med. Virol. 70:391-398. [DOI] [PubMed] [Google Scholar]
- 32.Suguitan, A. L., Jr., J. McAuliffe, K. L. Mills, H. Jin, G. Duke, B. Lu, C. J. Luke, B. Murphy, D. E. Swayne, G. Kemble, and K. Subbarao. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3:e360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Süss, J., J. Schäfer, H. Sinnecker, and R. G. Webster. 1994. Influenza virus subtypes in aquatic birds of eastern Germany. Arch. Virol. 135:101-114. [DOI] [PubMed] [Google Scholar]
- 34.Taubenberger, J. K., J. V. Hultin, and D. M. Morens. 2007. Discovery and characterization of the 1918 pandemic influenza virus in historical context. Antivir. Ther. 12:581-591. [PMC free article] [PubMed] [Google Scholar]
- 35.Treanor, J. J., K. Kotloff, R. F. Betts, R. Belshe, F. Newman, D. Iacuzio, J. Wittes, and M. Bryant. 1999. Evaluation of trivalent, live, cold-adapted (CAIV-T) and inactivated (TIV) influenza vaccines in prevention of virus infection and illness following challenge of adults with wild-type influenza A (H1N1), A (H3N2), and B viruses. Vaccine 18:899-906. [DOI] [PubMed] [Google Scholar]
- 36.Wright, P. F., G. Neumann, and Y. Kawaoka. 2007. Orthomyxoviruses, p. 1691-1740. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA.