Abstract
Background
Communication of children’s weight status and targeted counseling by pediatricians may change parental perceptions or child dietary and physical activity (PA) behaviors.
Purpose
To determine whether accuracy of parental perception of children’s weight status and reports of related behaviors changed following a brief pediatrics resident intervention.
Methods
Parents (N=115) of children ages 4–12 years enrolled in Medicaid completed baseline questionnaires about prior communication of weight status and/or body mass index (BMI) with providers, perceptions of their children’s weight, and children s dietary and PA behaviors, and children were weighed and measured. Trained residents used a toolkit to communicate weight status to parents (via color-coded BMI charts) and counseled about mutually chosen healthy behaviors. Questionnaires were repeated at one and three months, and measurements were repeated for children with BMI≥85%.
Results
At baseline, 42% of parents of overweight children believed they were at healthy weight. Most (n=96; 83%) parents completed one-month, and 56% completed three month follow up questionnaires. Improvements in fruit and vegetable consumption, sweet drinks, unhealthy snacks, frequency of restaurant food, lower-fat milk, and screen time, occurred among both overweight and healthy weight children. There were also increases in discussions with providers about weight/BMI and parental accuracy of overweight assessment.
Conclusions
Parent accuracy of weight status and short term childhood dietary and PA behavior changes improved following resident pediatrician use of a toolkit to support communication of weight status and counseling. Further research needs to determine whether accurate parental perception motivates improved behavior change or healthier BMI trajectories.
Keywords: childhood obesity, childhood overweight, BMI, physical activity, nutrition, counseling
In the United States (US), as many as 32% of children and adolescents are overweight or obese using current expert panel definitions,1–3 increasing their likelihood of developing many health problems, including type 2 diabetes, dyslipidemia, hypertension, and depression,4 and of becoming obese adults.5 Studies are ongoing to determine the most effective obesity treatment strategies, and to determine which children are at greatest risk for adult obesity and related health problems. However, growing evidence and national policy statements suggest pediatricians should at least recommend to parents behavioral changes to promote healthy weight that carry no or minimal harm, such as limiting television, limiting sweetened drinks, and increasing physical activity, particularly for higher-risk children.3,6 Helping young children actually achieve these healthier behaviors could be promoted through effective counseling by the pediatrician and motivation by the parents.
One of the barriers to improving behaviors may be that both providers and parents under-identify overweight and obesity in children, and thus do not realize a need for behavior change. Parents fail to recognize when their children, particularly young children, are overweight or obese.7–12 Some also do not perceive associated health risks.10 While we do not know if or how parental recognition of overweight matters, preliminary evidence suggests that parental perception of the child as overweight or obese relates to a greater readiness to make positive weight-related behavioral changes.13
At the same time, pediatric providers consistently under-diagnose weight problems, failing to document obesity for the majority in the overweight category.14 They also infrequently use recommended Centers for Disease Control and Prevention (CDC) age- and gender-specific Body Mass Index (BMI= kg/m2) charts, designed to screen for unhealthy weight status.15–17 This low identification may be because pediatricians have low self-efficacy in managing obesity and report that poor patient and parent motivation,18,19 lack of parental perception of the problem, and lack of patient education tools contribute to their counseling difficulties.20 Pediatricians also report a desire for better counseling tools to guide patients toward lifestyle modification and better tools to communicate weight problems to their patients.20
Given the multitude of tasks required of primary care pediatricians, effective brief strategies for targeted counseling and weight status communication are essential. Yet, only a few studies report on whether such interventions change dietary or physical activity (PA) behaviors in school age children or parental perceptions of obesity,21–24 and those that do usually focus only on overweight23 or older children.24 We designed an intervention to help pediatrics residents prevent and treat obesity and overweight in children, including young children, that encouraged communication between providers and parents regarding children’s weight status using color-coded BMI charts and incorporating an easy-to-use assessment of dietary and PA behaviors and counseling tips. We examined its effects on parents’ reported discussions of weight status with providers and accuracy of understanding their children’s weight status as well as parent-reported dietary and PA behavior change.
METHODS
Study Design and Participants
A pre-test, post-test study was conducted over a 16-month period to measure the effects of a provider “toolkit” aimed at preventing and treating childhood obesity in a pediatric primary care setting. Children 4 to 12 years of age were consecutively recruited at the University of North Carolina Child and Adolescent General Clinic if they were being seen in the clinic for a well child visit or a minor illness, were insured by North Carolina Medicaid or the State Children’s Health Insurance Program (Health Choice), and had English-speaking parents or caregivers. This study was approved by the University of North Carolina at Chapel Hill School of Medicine Institutional Review Board (protocol # 04-HPDP-771).
Intervention, Study Instruments, and Measurement
Pediatric resident physicians were invited to attend a “Healthy Weight” noon conference training session. The one-hour clinician training session included a review of the epidemic of childhood overweight and instruction on how to deliver patient- and parent-focused interventions using the “Healthy Weight” toolkit. This toolkit included color-coded BMI charts and a nutrition- and activity-focused “Starting the Conversation” (STC) assessment and counseling instrument. Training was required for study participation.
Color-coded body mass index (BMI) charts were used to plot the child’s BMI according to age and gender-specific norms set by the CDC.25 As described elsewhere,26,27 we color-coded the charts according to a stop light motif (red, yellow & green) based on the child’s weight status to facilitate identification by the pediatrician and communication of BMI status with parents. Children were classified into measured BMI weight categories as follows according to their sex and age: < 5th percentile, 5th–<85th percentile, 85th–<95th percentile, and ≥95th percentile. For most analyses, we collapsed 85th–<95th percentile, and ≥95th percentile into one category due to small numbers in the 85-<95 percentile group. For simplicity, particularly given the changing terminology around childhood weight categories, we refer to all of these children (≥85th percentile) as “overweight.”
Parents were asked to rate their child’s weight using then standard terminology describing the same four categories: “underweight,” “healthy weight,” “at risk for overweight,” and “overweight.” In order to determine accuracy of weight perceptions, parental responses were dichotomized by collapsing “at risk for overweight” with “overweight” because our goal was to help parents identify any non-healthy weight status, and then compared to the collapsed categories of ≥85th percentile based on BMI as measured in the clinic. Thus, we classified parental reports as: accurately reported, reported their child was thinner than he or she actually was, or reported child was heavier than he or she actually was.
The “Starting the Conversation” (STC) nutrition and physical activity (PA) assessment and counseling instrument (from now on referred to as the “STC instrument”) was designed for use by primary care providers and is composed of evidence-based rapid assessment questions with a section for physicians to provide tailored counseling messages. The STC instrument includes questions assessing current dietary and physical activity behaviors. Five dietary behavior questions are intended to measure behaviors that are likely to help to promote healthy weight: (1) number of servings of fruits and vegetables per day; (2) number of sugary drinks and fruit juice per day; (3) number of snacks like cakes, cookies, ice cream, candy, and chips per day; (4) frequency of eating food purchased away from home; and (5) type of milk that the child drinks most often. Five PA behavior questions ask parents to quantify: (1) hours of active play per day; (2) days per week the child plays outdoors; (3) hours of “screen time” (TV, video, computer games) the child gets each day; (4) involvement in sports teams and community groups; and (5) family activities per week. Respondents chose from three response categories (four for milk type) specific to each behavior (e.g., one or fewer servings, 2–3 servings, >3 servings). While our STC instrument was designed prior to release of the most recent AAP Policy Statement on Prevention of Pediatric Overweight and Obesity, the questions we used covered many similar behaviors, and were developed based on previous research of behaviors related to weight status, face validity, and other research of assessment of weight-related behaviors (i.e. use of outdoor playtime as a surrogate for physical activity).28 The complete toolkit has been previously described.27
Study Procedures
Electronic and manual patient visit schedules in the University of North Carolina Child and Adolescent General Clinic were reviewed several times per week to identify potentially eligible study participants. All parents of eligible children were approached by study research assistants in the patient examination rooms prior to the physicians’ assessments. The RA described the research study expectations for the parents and children. Caregivers, primarily female (92%), then completed the baseline STC instrument (described above) and a baseline parent survey inquiring about the weight-related, nutrition, and physical activity information received from their primary care physician at the last clinic visit, and their own assessment of their children’s weight status. The patient’s weight and height were measured in clinic using standardized equipment (Tronix Scale and Ayrton Stadiometer Model S100) and plotted on the color-coded BMI chart by the RA. Prior to the clinician-patient encounter, the research assistant met with the resident physician for approximately one minute to review the STC instrument responses and BMI color-coded chart
During the clinician-patient-parent encounter, the precise method of using the toolkit was left to the discretion of the resident pediatrician. Generally, the resident reviewed the patient’s BMI with the parent and explained the child’s weight status using the color-coded BMI chart. The resident physician also used the completed STC instrument to identify dietary and physical activity behaviors that could put the child at risk for overweight, reviewed the responses with the parent, provided positive feedback for healthy behaviors, gave advice for 1–2 mutually chosen healthy behavior changes, circled recommended behavior changes, and gave a copy of the STC instrument with circled recommended behavior changes to the parent. One copy of the STC instrument was included in the medical record so that the clinician could monitor patient behavior changes from one visit to another. The intervention was designed to take 2–3 minutes of discussion between parents and residents.
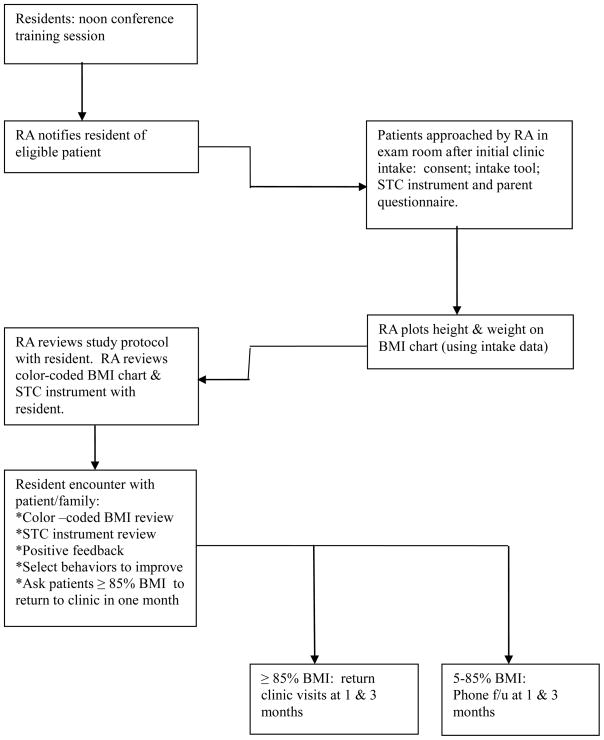
The STC instrument and parent survey were repeated approximately one month and three months after the parent and child received the clinic-based counseling intervention. Follow-up occurred by telephone for those at healthy weight (BMI<85%) at baseline and in person at the clinic during a follow-up visit to check in with the family and reinforce counseling for those identified as overweight (BMI≥85%). Figure 1 documents the study procedures in flow chart format.
Figure 1.
Study procedures.
Statistical Analysis
We hypothesized that parental reports of dietary and PA behaviors, as measured by the STC instrument, would improve following the intervention. The analyses in this report use baseline, one-month, and three-month follow-up data, and focus on pre-intervention to post-intervention changes for the five dietary questions and the five PA questions on the STC instrument. We examined differences in these ordinal responses using Wilcoxon signed-rank tests. Dichotomous differences, such as those between overweight and healthy weight children, are examined using t-tests or chi-squared tests, as appropriate. All analyses were performed using Stata 10.0 (College Park, TX).
RESULTS
Study Sample and Patient Characteristics
Of 52 potentially eligible pediatric resident physicians, 49 (94%) enrolled in the study, participated in patient enrollment and/or follow-up, and completed the post-test survey. Of the 115 children age 4 to 12 years who enrolled in this study, 96 completed the one-month follow-up questionnaires either by telephone or in person depending on BMI weight category, for an 83% completion rate at 1 month and 64 completed the 3-month follow-up, for a 56% completion rate at 3 months (60 completed 3-month follow-up of nutrition and PA behaviors). There were no significant differences between those who did and did not complete either follow-up interview, in terms of age, gender, race, ethnicity, actual weight status, or parent-perceived weight status. Additionally, the only significant differences in baseline behaviors between those who did and did not complete one-month follow-up were that those not returning were more likely to report fewer than two days of family activity per week and more likely to report eating out more than once per week. There were no baseline differences in behaviors between those who did and did not complete 3-month follow-up.
At follow-up the children’s average age was 7.6 years, and 47% were male (Table 1). More than 90% of study participants were non-Hispanic, and 65% were black/African American. Because all participants were insured by North Carolina’s Medicaid or State Children’s Health Insurance Program, all families had household incomes under 200% of the federal poverty guidelines. Use of the toolkit by the resident physician (BMI charts and STC instrument) required, on average, two to three minutes per study participant encounter and were generally regarded alternative approaches for discussing topics that are routine components of the well-child visit rather than additional responsibilities.
Table 1.
Demographic characteristics of the sample at baseline and each follow-up. P-values from McNemar’s exact test non-significant for all variables.
| Baseline (n=115) | 1-month (n=96) | 3-month (n=64) | |
|---|---|---|---|
| Child Age (years) | 7.5 | 7.6 | 7.6 |
| Child Sex | |||
| Male | 50.4 | 46.9 | 51.6 |
| Parent Sex | |||
| Female | 92.2 | 92.7 | 95.2 |
| Child Ethnicity | |||
| Hispanic | 7.8 | 9.4 | 10.9 |
| Non-Hispanic | 92.2 | 90.6 | 89.1 |
| Child Race | |||
| White | 20.9 | 22.9 | 23.4 |
| African American | 66.1 | 64.6 | 60.9 |
| Other | 13.0 | 12.5 | 15.6 |
| Language preference | |||
| English | 95.7 | 94.8 | 95.3 |
| Other | 4.3 | 5.2 | 4.7 |
Reported Dietary Behavior Changes
Significant differences in a healthy direction emerged at one-month follow-up for reported consumption of fruits and vegetables, sweet drinks, unhealthy snacks, and lower-fat milk consumption for all children (Table 2). Even larger differences in a healthy direction were seen at three-month follow-up, including improvements in consumption of fruits and vegetables, sweet drinks, unhealthy snacks, restaurant food, and lower-fat milk. Similar differences are noted when examining only overweight and obese children (data not shown).
Table 2.
Percent reporting diet and exercise behaviors.
| Children seen at one-month follow-up (n=94) | Children seen at three-month follow-up (n=60) | |||||
|---|---|---|---|---|---|---|
| Baseline | 1 Month | p | Baseline | 3 Month | P | |
| Servings fruits or vegetables each day | ||||||
| Less than 3 | 44.7* | 37.2 | 0.022 | 43.3* | 33.3 | 0.011 |
| 3–4 | 45.7 | 45.7 | 50.0 | 50.0 | ||
| 5 or more | 9.6 | 17.0 | 6.7 | 16.7 | ||
| Sugary drinks per day | ||||||
| 1 or fewer | 29.8** | 44.7 | 0.001 | 25.0** | 50.0 | 0.002 |
| 2 | 26.6 | 24.5 | 35.0 | 23.3 | ||
| More than 2 | 43.6 | 30.9 | 40.0 | 26.7 | ||
| Snacks per day | ||||||
| 1 or fewer | 53.2* | 64.9 | 0.031 | 46.7** | 73.3 | 0.001 |
| 2–3 | 40.4 | 33.0 | 43.3 | 23.3 | ||
| More than 3 | 6.4 | 2.1 | 10.0 | 3.3 | ||
| Times eating out per week | ||||||
| 1 or fewer | 54.8 | 66.7 | 0.101 | 46.6** | 67.2 | 0.007 |
| 2–3 | 35.5 | 21.5 | 39.7 | 22.4 | ||
| More than 3 | 9.7 | 11.8 | 13.8 | 10.3 | ||
| Usual milk type | ||||||
| Skim or 1% | 11.7** | 18.1 | 0.001 | 11.7** | 25.0 | 0.004 |
| 2% | 28.7 | 36.2 | 31.7 | 31.7 | ||
| Whole | 53.2 | 39.4 | 51.7 | 36.7 | ||
| None | 6.4 | 6.4 | 5.0 | 6.7 | ||
| Hours of active play per day | ||||||
| Fewer than 1 | 6.4 | 8.5 | 0.531 | 6.7 | 8.3 | 0.889 |
| 1–2 | 31.9 | 33.0 | 30.0 | 28.3 | ||
| More than 2 | 61.7 | 58.5 | 63.3 | 63.3 | ||
| Days per week plays outside | ||||||
| 0–2 | 13.8 | 13.8 | 0.399 | 13.3 | 11.7 | 0.835 |
| 3–4 | 31.9 | 25.5 | 28.3 | 36.7 | ||
| 5 or more | 54.3 | 60.6 | 58.3 | 51.7 | ||
| Hours of screen time per day | ||||||
| 0–2 | 48.9** | 61.7 | 0.003 | 45.0** | 66.7 | 0.001 |
| 3 | 22.3 | 20.2 | 21.7 | 18.3 | ||
| More than 3 | 28.7 | 18.1 | 33.3 | 15.0 | ||
| Involved in sports teams or community groups | ||||||
| Rarely/never | 52.2 | 47.8 | 0.131 | 46.6 | 43.1 | 0.093 |
| Once a week | 23.9 | 20.7 | 27.6 | 12.1 | ||
| More than once a week | 23.9 | 31.5 | 25.9 | 44.8 | ||
| Days per week family or community activities | ||||||
| Less than 2 | 32.3 | 30.1 | 0.285 | 35.6 | 32.2 | 0.262 |
| 2–3 | 47.3 | 41.9 | 39.0 | 33.9 | ||
| More than 3 | 32.6 | 28.0 | 25.4 | 33.9 | ||
p<0.01,
p<0.05; Wilcoxon signed-rank test
Overall, between one-fifth and one-half of children reported behavior improvements from baseline to both 1-month and 3-month follow-up (Table 3). Overweight children were significantly more likely than healthy weight children to report drinking a lower fat milk at both follow-up periods and also more likely to report improvements (decreases) in the frequency of eating restaurant meals at 3-month follow-up.
Table 3.
Percent of children showing improvement in diet and physical activity behaviors, by weight status at baseline.
| Time 1 to Time 2 (n=94) | Time 1 to Time 3 (n=60) | |||||
|---|---|---|---|---|---|---|
| Overweight | Healthy Weight | p | Overweight | Healthy Weight | p | |
| Servings fruits or vegetables each day | 21.7 | 27.1 | 0.547 | 23.3 | 26.7 | 0.766 |
| Sugary drinks per day | 43.5 | 31.3 | 0.220 | 50.0 | 36.7 | 0.297 |
| Snacks per day | 28.3 | 25.0 | 0.721 | 40.0 | 30.0 | 0.417 |
| Times eating out per week | 30.4 | 17.0 | 0.128 | 46.7* | 21.4 | 0.043 |
| Lower Fat Milk | 32.6* | 12.5 | 0.019 | 36.7* | 13.3 | 0.037 |
| Hours of active play per day | 13.0 | 12.5 | 0.937 | 10.0 | 23.3 | 0.166 |
| Days per week plays outside | 30.4 | 14.6 | 0.065 | 26.7 | 33.3 | 0.573 |
| Hours of screen time per day | 39.1 | 20.8 | 0.052 | 43.3 | 36.7 | 0.598 |
| Involved in sports teams or community groups | 19.6 | 28.3 | 0.328 | 26.7 | 32.1 | 0.647 |
| Days per week family or community activities | 26.7 | 31.3 | 0.627 | 31.0 | 26.7 | 0.711 |
p<0.05, chi-squared test comparing overweight and healthy weight children.
Reported Physical Activity Behavior Changes
Screen time improved with more parents reporting that their children engaged in 2 hours or less of screen time per day at one-month follow-up than at baseline (62% versus 49%; p < 0.01) (Table 2) and at 3-month follow-up compared to baseline (67% vs. 45%, p<0.01). There were no significant differences in other activities measured. As with dietary findings, similar results were seen when examining only overweight or obese children. There were also no significant differences by weight status in the proportion of children reporting improvements in physical activity (Table 3).
Weight-based Communication Changes
A significantly greater percentage of parents of healthy weight children reported discussions of weight (68.6% vs. 39.2%, p<0.001) and BMI (52.9% vs. 9.8%, p<0.001) with their physician at one-month follow-up. Additionally, a greater percentage of parents of overweight children reporting discussions of weight (86.4% vs. 68.2%, p=0.031) and of BMI (71.1% vs. 36.8%; p=0.002) at one-month follow-up. These questions were not asked at the 3 month time period.
Accuracy of weight perceptions
At baseline, 100% of parents of healthy weight children correctly perceived their child’s weight; only 56.5% of parents of overweight children did (p<0.001, t-test). At the one-month follow-up, 100% of parents of healthy weight children and 68.9% of parents of overweight children had an accurate perception of their child’s weight (p<0.001, t-test). The changes from baseline to follow-up were not significant (p=0.200, t-test). At 3-month follow-up, 74.1% of parents of overweight children had an accurate perception of their child’s weight, a statistically significant improvement from baseline (p<0.05, t-test).
Weight changes
At one-month follow-up, all of the 46 children who were above the 85th percentile for BMI were measured again. Of these, 39 of the subjects remained in the same weight category as baseline. Of the 7 who changed weight categories, three shifted from overweight (85th–95th percentile) to obese (>95th percentile) and four improved—three from obese to overweight and one from overweight to healthy weight (<85th percentile). These changes were not statistically significant (p=0.706, Wilcoxon signed-rank test). At three-month follow-up, all of the 30 children who were above the 85th percentile at baseline were measured again, with 23 remaining in the same weight category. Of those who changed weight categories, two who were in the overweight category became obese, while two more improved to become healthy weight. Three obese children improved their weight status—two to overweight and one to healthy weight. These changes were not significant (p=0.246, Wilcoxon signed-rank test).
Discussion
In our study, we were able to show that important short term dietary and physical activity behavior changes were reported by parents of children ages 4–12 following a relatively easy-to-implement intervention in a single pediatrics continuity clinic. Confirming prior research,7,11,12 many parents of children in this age group whose BMI’s are ≥85% perceive their children as at a healthy weight. Our intervention resulted in an improvement in the rate of parents correctly identifying their child’s weight status. Though not as simple as weight alone, BMI flags risk for overweight and obesity better than traditional growth charting;16 and our findings confirm previous research that simple modifications like color-coding the BMI chart may facilitate documentation, discussion, and understanding of BMI.26,29,30 However, based on published literature, ours may be the first intervention to change parental recognition of overweight through a simple clinic-based intervention.
Providers who use BMI may be more likely to recognize mild overweight at an earlier age, when treatment may require less significant behavior change. These providers may also more likely to provide nutrition and activity counseling for overweight children. Also, we know from prior study that parents perceive doctors’ nonchalance about overweight at early ages as a barrier to changing health habits.31 Importantly, in our study which focused on communicating BMI status and providing targeted behavior counseling, there were significant short-term (three-month) improvements in reported dietary and physical activity behaviors. Our study suggests that the clinical setting can be an effective site to address at least short term behavior changes to improve obesity and echoes recent research demonstrating that physicians’ assessment of parental confidence and readiness to change is associated with parental confidence to make changes.32
One of the most important strengths of our study is that it was a real-life, brief, and user-friendly intervention that could be implemented in most pediatrics clinics, especially ones that had electronic medical records and a system for handing out questionnaires in the waiting room. The population was also heterogeneous, suggesting that diverse populations could similarly benefit. While studies have shown that brief interventions similar to ours in pediatric providers’ offices have demonstrated feasibility30,33 and improved parental confidence, and others show chart evidence of provider improvements in counseling rates, documentation of overweight,29,33,34 or confidence,23,24 there are few reports that assess parent perception or child behavior outcomes.
Two important studies that did assess behavior outcomes showed that a primary care intervention did not produce any significant differences in child behavior.22,35 One possible reason we were able to demonstrate improvements in behaviors was our focus on recognition of weight status by parents. We do not know specifically if improved parental accuracy of weight status translates into greater understanding of the need to follow behavioral prescriptions with respect to nutrition and physical activity or weight trajectories, and our sample was too small to assess this association. However, this area deserves further research as a possible mechanism for improving the effectiveness of clinic-based obesity interventions.
Our study had several limitations. The changes reported are only short term, and our sample size was relatively small, derived from the willing English-speaking families at just one clinic, so generalizability is limited. However, our clinic is diverse; and this was reflected in the demographics of our sample as well. Small sample size also limited the ability to fully assess the relationship between improved weight status understanding and behavior change. This small sample size is mostly attributed to the relatively infrequent occurrence of parents scheduling and bringing their four to 12 year olds to clinic for well-child visits in this population. Attrition (particularly from one month to three month follow up) also limits our interpretability. However, the limitation of attrition is mitigated by the fact that demographics were similar between groups that did and did not complete the study; and the only differences in behaviors were at the one month follow up. Interestingly, these differences reflected the fact that busier families likely followed up less often as they were more likely to report fewer than two days of family activity per week and more likely to report eating out more than once per week. Another limitation is that our STC instrument has not been previously validated, though the questions are based on previous research. Importantly, the changes seen in reported behaviors could easily be the result of social desirability or reporting bias; and we do not have objective measures of diet or physical activity before and after implementation of the tool. Also, parent report of discussions of weight or BMI with the physician may not accurately reflect whether or not they occurred. Our results were only assessed at one and three months following the intervention, so we can not attest to sustainability. Longer follow-up periods would also allow for greater tracking of changes in children’s weight status and how behavior changes affect weight trajectories long-term. Finally, the lack of a control group definitely limits the ability to assess whether changes seen were related to the intervention, and thus causality can not be determined. This should be remedied in future research.
Treatment plans cannot address unidentified problems. Whether BMI screening and communication to parents of young children and changed understanding of children’s weight status helps parents adopt recommended behavior changes or changes pediatricians’ management has not been adequately investigated and is an area ripe for future research. For families who do not change behaviors with such a simple intervention, more intensive counseling may be necessary, such as a motivational interviewing approach that has shown promise.21 Also, more research might be needed to find out which parent and practitioner characteristics are associated with lack of change in order to improve dynamic communication.
Still, ours is one of the first studies to report short-term healthy weight behavior adoption following brief provider counseling. Given the evidence that television reduction is associated with body mass index reduction36,37 and the importance of sweetened beverages toward total daily energy intake,38 it is encouraging that parents in our study reported improvement in these areas. Our finding of improved reports of discussion of BMI following use of color-coded BMI charts adds to the growing body of research on this potentially important tool. Future research is needed to determine whether tools like this and our “Starting the Conversation” assessment and counseling instrument might impact sustainable and important behavior change and weight status for children in our increasingly “obesogenic” world.
Acknowledgments
The authors would like to thank Kori Flower, MD, MPH, Gina Chung, EdM, Lisa Pullen-Davis, PhD, MSPH, and especially Karah Daniels, MA, and Joanne Propst Finkle, RN, JD, for their research ideas, help, and support throughout various stages of this project. We thank Cynthia Bulik, PhD, and Suzanne Lazorick, MD, MPH, for their thoughtful comments and reviews of manuscript drafts.
Funding Sources: This project was supported by Dr. Perrin’s NIH K23 career development award (5K23 HD051817), Dr. Ammerman’s R01 (5 R01 HD050981-02), Dr. Skinner’s Building Interdisciplinary Careers in Women’s Health (BIRCWH) award (K12-HD01441), and AccessCare.
Footnotes
Conflicts of interest: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Eliana M. Perrin, UNC Chapel Hill, School of Medicine, Department of Pediatrics, Division of General Pediatrics and Adolescent Medicine, Chapel Hill, North Carolina.
Julie C. Jacobson Vann, UNC Chapel Hill, School of Nursing, Health Care Systems, Chapel Hill, North Carolina.
John T. Benjamin, UNC Chapel Hill, Department of Pediatrics, Chapel Hill, North Carolina (retired).
Asheley Cockrell Skinner, UNC School of Medicine, Department of Pediatrics, Division of General Pediatrics and Adolescent Medicine, Chapel Hill, North Carolina.
Steven Wegner, AccessCare, Morrisville, North Carolina.
Alice S. Ammerman, UNC Chapel Hill, Center for Health Promotion Disease Prevention and Department of Nutrition, Chapel Hill, North Carolina.
References
- 1.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA. 2010;3030 (3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 2.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 3.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120 (Suppl 4):S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 4.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3 Pt 2):518–525. [PubMed] [Google Scholar]
- 5.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 6.Whitaker RC. Obesity prevention in pediatric primary care: four behaviors to target. Arch Pediatr Adolesc Med. 2003;157(8):725–7. doi: 10.1001/archpedi.157.8.725. [DOI] [PubMed] [Google Scholar]
- 7.Parry LL, Netuveli G, Parry J, Saxena S. A systematic review of parental perception of overweight status in children. J Ambul Care Manage. 2008;31(3):253–268. doi: 10.1097/01.JAC.0000324671.29272.04. [DOI] [PubMed] [Google Scholar]
- 8.Huang JS, Becerra K, Oda T, et al. Parental ability to discriminate the weight status of children: results of a survey. Pediatrics. 2007;120(1):e112–9. doi: 10.1542/peds.2006-2143. [DOI] [PubMed] [Google Scholar]
- 9.Baughcum AE, Chamberlin LA, Deeks CM, Powers SW, Whitaker RC. Maternal perceptions of overweight preschool children. Pediatrics. 2000;106(6):1380–6. doi: 10.1542/peds.106.6.1380. [DOI] [PubMed] [Google Scholar]
- 10.Jain A, Sherman SN, Chamberlin DL, Carter Y, Powers SW, Whitaker RC. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics. 2001;107(5):1138–46. doi: 10.1542/peds.107.5.1138. [DOI] [PubMed] [Google Scholar]
- 11.Maynard LM, Galuska DA, Blanck HM, Serdula MK. Maternal perceptions of weight status of children. Pediatrics. 2003;111(5 Part 2):1226–31. [PubMed] [Google Scholar]
- 12.Jeffery AN, Voss LD, Metcalf BS, Alba S, Wilkin TJ. Parents’ awareness of overweight in themselves and their children: cross sectional study within a cohort (EarlyBird 21) BMJ. 2005;330(7481):23–4. doi: 10.1136/bmj.38315.451539.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rhee KE, De Lago CW, Arscott-Mills T, Mehta SD, Davis RK. Factors associated with parental readiness to make changes for overweight children. Pediatrics. 2005;116(1):e94–101. doi: 10.1542/peds.2004-2479. [DOI] [PubMed] [Google Scholar]
- 14.Hamilton JL, James FW, Bazargan M. Provider practice, overweight and associated risk variables among children from a multi-ethnic underserved community. J Natl Med Assoc. 2003;95(6):441–8. [PMC free article] [PubMed] [Google Scholar]
- 15.Barlow SE, Dietz WH, Klish WJ, Trowbridge FL. Medical evaluation of overweight children and adolescents: reports from pediatricians, pediatric nurse practitioners, and registered dietitians. Pediatrics. 2002;110(1 Pt 2):222–228. [PubMed] [Google Scholar]
- 16.Perrin EM, Flower KB, Ammerman AS. Body mass index charts: useful yet underused. J Pediatr. 2004;144(4):455–460. doi: 10.1016/j.jpeds.2004.01.047. [DOI] [PubMed] [Google Scholar]
- 17.Dorsey KB, Wells C, Krumholz HM, Concato JC. Diagnosis, evaluation, and treatment of childhood obesity in pediatric practice. Arch Pediatr Adolesc Med. 2005;159(7):632–638. doi: 10.1001/archpedi.159.7.632. [DOI] [PubMed] [Google Scholar]
- 18.Story MT, Neumark-Stzainer DR, Sherwood NE, et al. Management of child and adolescent obesity: attitudes, barriers, skills, and training needs among health care professionals. Pediatrics. 2002;110(1 Pt 2):210–214. [PubMed] [Google Scholar]
- 19.Kolagotla L, Adams W. Ambulatory management of childhood obesity. Obes Res. 2004;12(2):275–283. doi: 10.1038/oby.2004.35. [DOI] [PubMed] [Google Scholar]
- 20.Perrin EM, Flower KB, Garrett J, Ammerman AS. Preventing and treating obesity: pediatricians’ self-efficacy, barriers, resources, and advocacy. Ambul Pediatr. 2005;5(3):150–156. doi: 10.1367/A04-104R.1. [DOI] [PubMed] [Google Scholar]
- 21.Schwartz RP, Hamre R, Dietz WH, et al. Office-based motivational interviewing to prevent childhood obesity: a feasibility study. Arch Pediatr Adolesc Med. 2007;161(5):495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 22.McCallum Z, Wake M, Gerner B, et al. Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int J Obes (Lond) 2007;31(4):630–636. doi: 10.1038/sj.ijo.0803509. [DOI] [PubMed] [Google Scholar]
- 23.Gonzalez JL, Gilmer L. Obesity prevention in pediatrics: A pilot pediatric resident curriculum intervention on nutrition and obesity education and counseling. J Natl Med Assoc. 2006;98(9):1483–1488. [PMC free article] [PubMed] [Google Scholar]
- 24.Patrick K, Sallis JF, Prochaska JJ, et al. A multicomponent program for nutrition and physical activity change in primary care: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2001;155(8):940–946. doi: 10.1001/archpedi.155.8.940. [DOI] [PubMed] [Google Scholar]
- 25.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC Growth Charts for the United States: methods and development. Vital Health Stat 11. 2002;(246):1–190. [PubMed] [Google Scholar]
- 26.Oettinger MD, Finkle JP, Esserman D, et al. Color-coding improves parental understanding of body mass index charting. Acad Pediatr. 2009;9(5):330–338. doi: 10.1016/j.acap.2009.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perrin EM, Finkle JP, Benjamin JT. Obesity prevention and the primary care pediatrician’s office. Curr Opin Pediatr. 2007;19(3):354–361. doi: 10.1097/MOP.0b013e328151c3e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burdette HL, Whitaker RC, Daniels SR. Parental report of outdoor playtime as a measure of physical activity in preschool-aged children. Arch Pediatr Adolesc Med. 2004;158(4):353–7. doi: 10.1001/archpedi.158.4.353. [DOI] [PubMed] [Google Scholar]
- 29.Gilbert MJ, Fleming MF. Use of enhanced body mass index charts during the pediatric health supervision visit increases physician recognition of overweight patients. Clin Pediatr (Phila) 2007;46(8):689–697. doi: 10.1177/0009922807300744. [DOI] [PubMed] [Google Scholar]
- 30.Wald ER, Ewing L, Cluss P, Goldstrohm S, Cipriani L, Colborn K. Establishing a family-based intervention for overweight children in pediatric practice. Ann Fam Med. 2005;3 (Suppl 2):S45–7. doi: 10.1370/afm.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Borra ST, Kelly L, Shirreffs MB, Neville K, Geiger CJ. Developing health messages: qualitative studies with children, parents, and teachers help identify communications opportunities for healthful lifestyles and the prevention of obesity. J Am Diet Assoc. 2003;103(6):721–8. doi: 10.1053/jada.2003.50140. [DOI] [PubMed] [Google Scholar]
- 32.Taveras EM, Mitchell K, Gortmaker SL. Parental confidence in making overweight-related behavior changes. Pediatrics. 2009;124(1):151–158. doi: 10.1542/peds.2008-2892. [DOI] [PubMed] [Google Scholar]
- 33.Ariza AJ, Laslo KM, Thomson JS, Seshadri R, Binns HJ. Pediatric Practice Research Group. Promoting growth interpretation and lifestyle counseling in primary care. J Pediatr. 2009;154(4):596–601. e1. doi: 10.1016/j.jpeds.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 34.Dunlop AL, Leroy Z, Trowbridge FL, Kibbe DL. Improving providers’ assessment and management of childhood overweight: results of an intervention. Ambul Pediatr. 2007;7(6):453–457. doi: 10.1016/j.ambp.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 35.Wake M, Baur LA, Gerner B, et al. Outcomes and costs of primary care surveillance and intervention for overweight or obese children: the LEAP 2 randomised controlled trial. BMJ. 2009;339:b3308. doi: 10.1136/bmj.b3308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282(16):1561–7. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 37.Danner FW. A national longitudinal study of the association between hours of TV viewing and the trajectory of BMI growth among US children. J Pediatr Psychol. 2008;33(10):1100–1107. doi: 10.1093/jpepsy/jsn034. [DOI] [PubMed] [Google Scholar]
- 38.Wang YC, Ludwig DS, Sonneville K, Gortmaker SL. Impact of change in sweetened caloric beverage consumption on energy intake among children and adolescents. Arch Pediatr Adolesc Med. 2009;163(4):336–343. doi: 10.1001/archpediatrics.2009.23. [DOI] [PubMed] [Google Scholar]