Abstract
We evaluated the effluent quality of an urban wastewater treatment facility in South Africa and its impact on the receiving watershed for a period of 12 months. The prevalence and antimicrobial susceptibility of potential Listeria pathogens (L. ivanovii and L. innocua) and the physicochemical quality of the treated wastewater effluent was assessed, with a view to ascertain the potential health and environmental hazards of the discharged effluent. Total listerial density varied between 2.9 × 100 and 1.2 × 105 cfu/mL; free living Listeria species were more prevalent (84%), compared to Listeria species attached to planktons (59–75%). The treated effluent quality fell short of recommended standards for turbidity, dissolved oxygen, chemical oxygen demand, nitrite, phosphate and Listeria density; while pH, temperature, total dissolved solids and nitrate contents were compliant with target quality limits after treatment. The Listeria isolates (23) were sensitive to three (15%) of the 20 test antibiotics, and showed varying (4.5–91%) levels of resistance to 17 antibiotics. Of seven resistance gene markers assayed, only sulII genes were detected in five (22%) Listeria strains. The study demonstrates a potential negative impact of the wastewater effluent on the receiving environment and suggests a serious public health implication for those who depend on the receiving watershed for drinking and other purposes.
Keywords: water quality, Listeria pathogens, health/environmental impact, receiving watershed
1. Introduction
Listeria is an emerging pathogen commonly associated with foodborne infections. Although seven species are recognized namely L. monocytogenes, L. ivanovii, L. innocua, L. seeligeri, L. welshimeri, L. grayii and L. murrayi, only two (L. monocytogenes and L. ivanovii) are pathogenic; the former is responsible for disease in both humans and animals, while the latter causes diseases mostly in ruminants but also in other animals [1,2]. There are reports, however, of L. seeligeri and L. ivanovii causing illnesses in humans [3,4], and L. innocua is occasionally associated with encephalitis in ruminants [5]. Other species are generally regarded as non-pathogenic [2].
The bacterium has been implicated in several foodborne outbreaks in the developed world [6,7] with little information on the existence of the pathogen in developing countries [6]. Although food is reported to be the major route of transmission of the pathogen, previous studies [8–13] indicated that Listeria is capable of surviving conventional wastewater treatment process even after disinfection; thus suggesting that wastewater may be significant in the epidemiology of the pathogen. This has serious public health implications for developing countries such as South Africa where a larger percentage of the population depend on surface water bodies that may be negatively impacted by untreated or inadequately treated wastewater for drinking and other purposes [14–16]. The existence of bacteria as free-living or attached cells was previously observed [17–19] to influence their capacity to resist disinfection and enhance resistance to antimicrobial therapy. Listerial resistance to antimicrobial therapy was also reported [20,21] to be mediated by certain resistance genes that encodes proteins which function in ways that inhibit or reduce the effects of antimicrobials on the pathogen.
Listeria infections have the highest (up to 50%) mortality rate amongst foodborne pathogens [6], making the South African public particularly vulnerable in the event of an outbreak due to the high HIV/AIDS prevalence level and rate of drug and alcohol abuse in the country [22]. The potential severity of listeriosis outbreak on the public health notwithstanding, there is dearth of information on the prevalence of this pathogen in South Africa. More worrisome is the fact that globally, Listeria is not considered a waterborne pathogen in spite of reports in the literature [8–13,21] suggesting that the pathogen is well established in the water supply chain.
The etiology of many waterborne outbreaks in South Africa is not known [23]; this may be due to the religious focus on traditional waterborne pathogens by investigators. The dire need to preserve the public health however calls for the investigation of emerging waterborne pathogens that were hitherto not investigated or overlooked notwithstanding their potentials to survive and distribute within the water supply chain. The current study was therefore carried out to investigate the effluent quality (Listeria pathogens and physicochemical) of a typical urban wastewater treatment facility in South Africa and its impact on the receiving watershed; with emphasis on the potential public health and environmental hazards associated with the use of such waters.
2. Materials and Methods
2.1. Description of Sampling Site
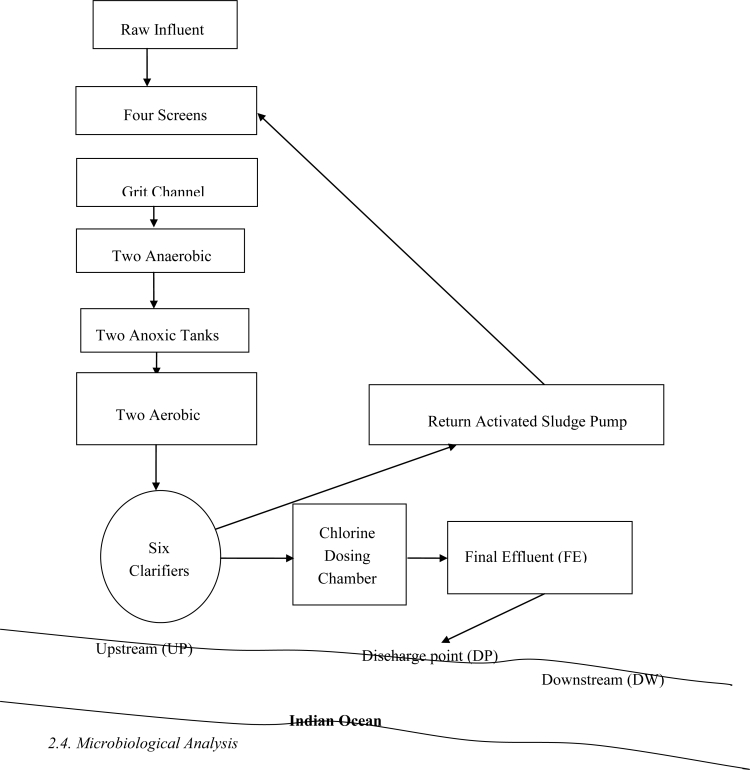
The wastewater treatment plant (Figure 1) is located in East London, a large and highly populated urban community in the Eastern Cape Province of South Africa, with the geographical coordinates: 32.97°S and 27.87°E. The plant receives municipal domestic sewage and a heavy industrial effluent and comprise of four screens, a grit channel, two anaerobic and two anoxic tanks and two aerobic tanks (each equipped with three vertically mounted mechanical aerators). The plant has six sedimentation tanks with the return activated sludge (RAS) pumped from the bottom of the clarifiers via the screens with raw sewage to the aeration tanks. Chlorine contact is carried out by means of a water pressure operated, wall mounted, gas chlorinator in a baffled reinforced concrete contact tank and the final effluent is discharged into the Indian Ocean. The average daily inflow of raw sewage during the study period was 32,000 m3/day, while the plant has a built in capacity of 40,000 m3/day.
Figure 1.
Schematic representation of the study area.
2.2. Sample Collection
Wastewater samples were collected on a monthly basis from the final effluent (FE), discharge point (DP), five hundred meters (500 m) upstream (UP) and five hundred meters (500 m) downstream (DW) of the discharge point between August 2007 and July 2008. Aqueous effluent samples were collected in duplicates in sterile one liter Nalgene bottles and transported in cooler boxes containing ice packs to the Applied and Environmental Microbiology Research Group (AEMREG) laboratory at the University of Fort Hare, Alice, South Africa for analyses. Sample bottles for the final effluents contained 0.1% sodium thiosulphate (3% solution) to neutralize the effect of the chlorine residual on the microflora. Processing of samples was done within 6 hours of sample collection.
2.3. Sample Processing
Samples were processed according to the descriptions of Maugeri et al. [24] with modifications. Briefly, samples (one liter in duplicates) were filtered in the laboratory through 180-, 60- and 20-μm pore size nylon nets (Millipore Corp., Ireland) respectively; the water that flowed through the 20-μm pore size nylon nets was collected in clean sterile containers for planktonic (free-living) Listeria cells analyses. To obtain a final volume corresponding to 40× of the original sample, trapped planktons on the nets and adhering bacteria were resuspended in 25 mL of sterile phosphate-buffered saline (PBS). To detach adhering bacteria from the planktons, 12.5 g of sterile 0.1 mm glass beads (Biospec Products Inc., Bartlesville, OK 74005, USA) was weighed into the bacteria-plankton suspension, vortexed at high speed for 30 s and centrifuged at 3,000× g for 10 min at ambient temperature using the Beckman Model TJ-6 centrifuge. The glass beads were allowed to settle to the bottom of the centrifuge tube and the supernatant was used for plankton-associated Listeria analyses. Henceforth in this paper, plankton of sizes ≥ 180 μm, ≥ 60 μm ≤ 180 μm, and ≥ 20 μm ≤ 60 μm, shall simply be represented as 180 μm, 60 μm and 20 μm, respectively.
2.4. Microbiological Analysis
The isolation of Listeria species were done according to the description of Hitchins [25] with modifications. Briefly, aliquots of samples containing free-living and plankton-associated bacteria were directly inoculated onto Listeria chromogenic agar (LCA agar) (Pronadisa® Madrid, Spain) following standard spread plate technique and incubated for 24–48 h at 35 °C. Typical Listeria colonies appear blue-green on LCA agar plates while pathogenic Listeria species (Listeria monocytogenes and L. ivanovii) were surrounded by an opaque halo in addition to their blue-green color. Total Listeria counts were recorded and presumptive Listeria pathogens were isolated from the treated (chlorinated) effluent samples, purified and stored on nutrient agar slants at 4 °C for further analyses. The presumptive Listeria pathogens were further confirmed by standard cultural characteristics and biochemical reactions [25] and using the API Listeria kits (10 300, bioMerieux, South Africa). Listeria monocytogenes (ATCC 19115) and Staphylococcus aureus (ATCC 25923) were used as positive and negative controls, respectively.
2.5. Physicochemical Analyses
All field meters and equipment were checked and appropriately calibrated according to the manufacturers’ instructions. pH, temperature, total dissolve solid (TDS), and dissolved oxygen (DO), were all determined on site using the multi-parameter ion specific meter (Hanna-BDH laboratory supplies). Turbidity and the concentrations of free chlorine residual in the final effluent samples were also determined on site using a microprocessor turbidity meter (HACH Company, model 2100P) and an ion-specific meter (Hanna Instruments, HI 93711) respectively. The concentrations of orthophosphate as P (PO4), nitrate (NO3), nitrite (NO2), and chemical oxygen demand (COD) were determined in the laboratory by the standard photometric method [26] using the spectroquant NOVA 60 photometer (Merck Pty Ltd). Samples for COD analyses were digested with a thermoreactor model TR 300 (Merck Pty Ltd) prior to analysis using the spectroquant NOVA 60 photometer.
2.6. Antimicrobial Agents
Twenty antibiotics commonly used as therapy in human and veterinary listeriosis were employed in the antibiogram assay. The paper disks containing the antibiotics were obtained from Mast Diagnostics (Merseyside, United Kingdom) and includes: Amikacin (30 μg), Ciprofloxacin (5 μg), Aztreonam (30 μg), Linezolid (30 μg), Chloramphenicol (30 μg), Imipenem (10 μg), Ceftriaxone (30 μg), Meropenem (10 μg), Cephalothin (30 μg), Ertapenem (10 μg), Erythromycin (15 μg), Gatifloxacin (5 μg), Gentamicin (10 μg), Moxifloxacin (5 μg), Ampicillin (25 μg), Streptomycin (25 μg), Penicillin G (10 μg), Tetracycline (30 μg), Trimethoprim (5 μg), and Sulphamethoxazole (25 μg).
2.7. Antibiotic Susceptibility Test
The antibiotic susceptibility test was performed and interpreted based on the disk diffusion method as described by the Clinical and Laboratory Standard Institute [27], using Mueller Hinton agar plates (Biolab, Merck, South Africa). The inhibition zone diameters (IZD) were interpreted according to CLSI standards for staphylococci due to lack of specific standards for Listeria species [28]. Interpretative standard for Linezolid was still under investigation for staphylococci at the time of this report, thus standard for Enterococcus species was applied for this antimicrobial agent.
2.8. Bacterial DNA Extraction and Amplification of Antimicrobial Resistance Genes
DNA was isolated from pure cultures of the selected Listeria strains by the boiling method as described elsewhere [29]. Based on the in vitro antimicrobial susceptibility profile of the Listeria isolates, seven antimicrobial resistance genes including those encoding penicillin binding protein (penA); dihydropteroate synthetase type I (sulI); dihydropteroate synthetase type II (sulII); adenine methylase (ermA); erythromycin resistance methylase (ermB); erythromycin esterase type II (ereB); and β-lactamase-ampicillin resistance gene (ampC); were selected for screening. Oligonucleotide sequences and predicted amplicon sizes for the different antimicrobial resistance genes are listed in Table 1. Presence of antimicrobial resistance genes in the Listeria species were all determined by PCR technique according to the description of Srinivasan et al. [21].
Table 1.
Primers used for resistance genes detection in the Listeria isolates from chlorinated waste water effluents.
| Gene | Primer | Nucleotide sequence | Amplicon size | Reference |
|---|---|---|---|---|
| penA | PenA-F | ATCGAACAGGCGACGATGTC | 500 | [21] |
| PenA-R | GATTAAGACGGTGTTTTACGG | |||
| ampC | AmpC-F | TTCTATCAAMACTGGCARCC | 550 | ” |
| AmpC-R | CCYTTTTATGTACCCAYGA | |||
| ermB | ErmB-F | GAAAAGGTACTCAACCAAATA | 639 | ” |
| ErmB-R | AGTAACGGTACTTAAATTGTTTAC | |||
| ereA | EreA-F | AACACCCTGAACCCAAGGGACG | 420 | ” |
| EreA-R | CTTCACATCCGGATTCGCTCGA | |||
| ereB | EreB-F | AGAAATGGAGGTTCATACTTACCA | 546 | ” |
| EreB-R | CATATAATCATCACCAATGGCA | |||
| su1I | Su1I-F | GTGACGGTGTTCGGCATTCT | 779 | ” |
| Su1I-R | TCCGAGAAGGTGATTGCGCT | |||
| su1II | Su1II-F | CGGCATCGTCAACATAACCT | 721 | ” |
| Su1II-R | TGTGCGGATGAAGTCAGCTC |
2.9. Statistical Analyses
Calculation of means and standard deviations were performed using Microsoft Excel Office 2007 version. Correlations (paired T-test) and test of significance (one-way ANOVA) were performed using SPSS 17.0 version for Windows program (SPSS, Inc.). All tests of significance and correlations were considered statistically significant at P values of < 0.05 or < 0.01.
3. Results
3.1. Abundance of Listeria
Total Listeria counts ranged from 2.9 × 100 to 1.2 × 105 cfu/mL (Table 2). The lowest count was observed during summer in the month of November 2007 at DW while the highest count was observed at the DP, also in the summer month of December 2007. Abundance of free-living Listeria species varied between 0 and 2.4×103 cfu/mL, with the highest count recorded at FE and DW in April 2008. Listeria species associated with plankton of sizes 180 μm, 60 μm, and 20 μm, were observed at population densities of 0 to 1.95 × 103 cfu/mL, 0 to 1.8 × 102 cfu/mL and 0 to 1.15 × 105 cfu/mL, respectively. The highest counts for the plankton-associated Listeria species were all observed at the DP in December 2007, June 2008 and December 2007 for 180 μm, 60 μm, and 20 μm categories, respectively. Listerial abundance did not vary significantly with season either as free-living or plankton-associated entities. The population of free-living Listeria species in the FE samples varied significantly (P < 0.05) with those of large (180 μm) and medium sized (60 μm) planktons but not with small (20 μm) planktons. Listeria density did not vary significantly with the size of the planktons to which they attach at DP and DW. There was, however, significant difference (P < 0.05) in listerial density between free-living Listeria populations and plankton-attached species of all categories at the UP sampling site.
Table 2.
Population density and distribution of the Listeria species in the treated effluents and its receiving watershed.
| Net Sampling pore Sites sizes | Listeriadensity (cfu/mL) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Spring | Summer | Autumn | Winter | ||||||||||
| Aug. 2007 | Sep. 2007 | Oct. 2007 | Nov. 2007 | Dec. 2007 | Jan. 2008 | Feb. 2008 | Mar. 2008 | Apr. 2008 | May 2008 | Jun. 2008 | Jul. 2008 | ||
| FE | 180 μm | 1.5×100 | 3.5×100 | ND | 4.0×100 | 8.6×101 | 2.5× 101 | 7.6×100 | 3.5×101 | 1.1×101 | 2.7×101 | 4.3×101 | 1.8×01 |
| 60 μm | 2.9×100 | 2.4×100 | ND | 0.0 | 1.0×101 | 1.6 ×101 | 3.0×100 | 1.4×101 | 8.1×100 | 1.0×101 | 3.8×101 | 1.2×101 | |
| 20 μm | 6.3×102 | 7.1×100 | ND | 0.0 | 3.0×102 | 1.2×101 | 9.3×100 | 3.9×100 | 9.4×100 | 1.2×101 | 9.3×101 | 1.1×100 | |
| Free | 2.6×102 | 3.0 ×102 | ND | 1.6×102 | 2.4× 102 | 2.3× 102 | 2.8×102 | 9.5×102 | 2.4×103 | 2.0×101 | 4.5×102 | 2.5×101 | |
| Total | 8.8×102 | 3.3×102 | ND | 1.7×102 | 6.3×102 | 2.8×102 | 2.95×102 | 1.0×103 | 2.4×103 | 6.9×101 | 6.2×102 | 5.7×101 | |
| DP | 180 μm | 3.9×100 | 2.1×100 | ND | 3.0×100 | 1.95×103 | 9.9×100 | 1.5×100 | 2.1×101 | 0.0 | 1.0×101 | 1.8×102 | 0.0 |
| 60 μm | 3.5×100 | 0.0 | ND | 0.0 | 1.9×101 | 2.2×101 | 3.8×100 | 3.5×100 | 7.6×100 | 7.0×100 | 1.8×102 | 0.0 | |
| 20 μm | 2.8×100 | 1.1×100 | ND | 0.0 | 1.2×105 | 6.3×100 | 6.1×100 | 4.7×101 | 6.7×101 | 1.6×101 | 6.9×101 | 0.0 | |
| Free | 5.7×102 | 2.1×102 | ND | 1.5×101 | 4.0×102 | 8.0×101 | 2.1×102 | 3.4×102 | 3.5×101 | 1.5×102 | 8.5×101 | 5.0×100 | |
| Total | 5.8×102 | 2.1×102 | ND | 1.98×101 | 1.2×105 | 1.2×102 | 2.2×102 | 4.1×102 | 1.1×102 | 1.8×102 | 5.1×102 | 5.0×100 | |
| DW | 180 μm | 0.0 | 1.1×100 | ND | 2.9×100 | 0.0 | 2.1×101 | 1.1×100 | 2.9×100 | 0.0 | 4.3×100 | 2.6×101 | 0.0 |
| 60 μm | 0.0 | 0.0 | ND | 0.0 | 0.0 | 1.5×101 | 0.0 | 0.0 | 0.0 | 6.9×100 | 3.0×101 | 0.0 | |
| 20 μm | 0.0 | 0.0 | ND | 0.0 | 0.0 | 1.2×101 | 1.6×100 | 9.6×100 | 0.0 | 1.96×101 | 1.8×101 | 0.0 | |
| Free | 3.5×101 | 3.5×101 | ND | 0.0 | 0.0 | 0.0 | 5.0×101 | 1.6×102 | 2.4×103 | 0.0 | 1.5×101 | 5.0×100 | |
| Total | 3.5×101 | 3.6×101 | ND | 2.9×100 | 0.0 | 4.8×101 | 7.8×100 | 1.7×102 | 2.4×103 | 3.1×101 | 8.9×101 | 5.0×100 | |
| UP | 180 μm | 0.0 | 0.0 | ND | 3.5×100 | 0.0 | 2.5×101 | 1.0×100 | 4.4×100 | 0.0 | 4.3×100 | 9.9×100 | 0.0 |
| 60 μm | 0.0 | 0.0 | ND | 0.0 | 0.0 | 8.9×100 | 2.0×100 | 1.1×100 | 0.0 | 2.7×101 | 2.4×101 | 0.0 | |
| 20 μm | 0.0 | 0.0 | ND | 3.6×103 | 0.0 | 7.6×100 | 1.5×100 | 2.4×100 | 0.0 | 1.7×101 | 3.1×101 | 0.0 | |
| Free | 1.5×101 | 5.0×100 | ND | 1.2×102 | 0.0 | 3.5×101 | 1.0×101 | 1.3×102 | 9.0×101 | 0.0 | 0.0 | 5.0×100 | |
| Total | 1.5×101 | 5.0×100 | ND | 1.2×102 | 0.0 | 7.6×101 | 1.5×101 | 1.4×102 | 9.0×101 | 4.8×101 | 6.5×101 | 5.0×100 | |
Legend: FE = treated final effluent, DP = discharge point, DW = 500 m downstream discharge point, UP = 500 m upstream discharge point; ND= not determined.
There was significant (P < 0.01) positive correlation between Listeria populations attached to large (180 μm) planktons and those attached to small (20 μm) planktons. Significant correlation was, however, not observed for other treatments with respect to listerio-plankton association.
Table 2 also shows the prevalence of Listeria during this study. Listeria species were isolated throughout the year from the treated effluents and the receiving watershed. Thirty-seven (84%) of all 44 samples (in duplicate) were positive for free-living Listeria species. Free-living Listeria species were isolated all year round except in DW (summer and early winter: May, 2008) and in UP (December 2007; May and June 2008). Seventy-five percent of all samples were positive for Listeria species associated with large (180 μm) plankton. Of these, Listeria was isolated from FE (11 samples), DP (nine samples), DW (seven samples) and UP (six samples). Twenty-six (59%) of all 44 samples were positive for Listeria species associated with medium-sized (60 μm) planktons, which were isolated from FE (10 samples), DP (eight samples), DW (three samples) and UP (five samples). Listeria species associated with small (20 μm) planktons were isolated in 30 (68%) of the 44 samples. FE samples were positive for this Listeria species in 10 samples, DP in nine samples, DW in five samples and UP in six samples.
3.2. Physicochemical Analyses
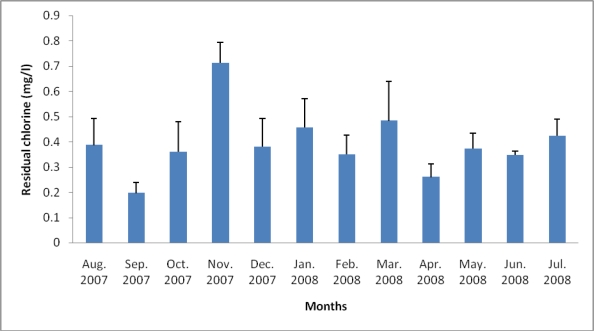
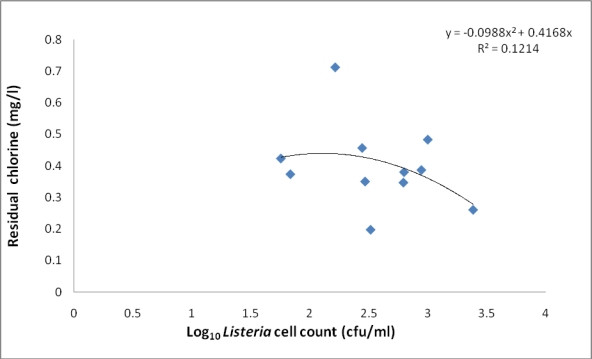
Table 3 shows the range and annual mean values of some wastewater quality parameters before and after treatment of the wastewater under study. Significant differences was observed between raw sewage and treated effluent in terms of turbidity, DO, and PO4 (P < 0.01) and for nitrate (P < 0.05). There was, however, no significant difference between treated and untreated wastewater for pH, temperature, TDS, COD, and NO2. Figure 2 shows the free chlorine residual (CR) of the final effluents during the 12 month study period. Chlorine residual ranged between 0.197 mg/L (September, 2007) and 0.71 mg/L (November, 2007). The relationship between residual chlorine and total Listeria count did not follow any defined trend (Figure 3).
Table 3.
Some physicochemical qualities of the raw wastewater and treated final effluent.
| Parameter | Raw wastewater | Treated effluent | Recommended target limits | ||
|---|---|---|---|---|---|
| Range | Mean±SD | Range | Mean±SD | ||
| pH | 4.97–7.75 | 7.1 ± 0.44 | 6.7–7.7 | 7.1 ± 0.28 | 6–9a |
| Temperature (° C) | 18–26 | 23 ± 2.3 | 18–26 | 22 ± 2.45 | ≤ 25 a |
| Turbidity (NTU) | 86–1,000 | 573 ± 369 | 2.16–16 | 6.09 ± 3.64 | 0–1 a; ≤ 5b |
| TDS (mg/l) | 311–907 | 452 ± 153 | 289–743 | 398 ± 110 | 0–450 a |
| DO (mg/l) | 0.14–7.32 | 1.76 ± 1.78 | 2.38–6.78 | 4.46 ± 0.94 | ≥ 5c |
| COD (mg/l) | 40–2,404 | 489 ± 701 | 4–960 | 143 ± 271 | 30d |
| NO3 (mg/l) | 0.026–5.1 | 3.17 ± 1.32 | 0.25–6.95 | 4.56 ± 2.53 | 6a; 1–5d |
| NO2 (mg/l) | 0.07–3.5 | 0.53 ± 0.93 | 0.07–6.95 | 0.88 ± 1.84 | 0–6a; <0.5e |
| PO4 (mg/l) | 1.33–5.91 | 3.78 ± 1.26 | 0.05–0.73 | 0.34 ± 0.16 | 0.005e |
Legend:
Target limit for domestic water uses in South Africa [30];
Target limit for effluent to be discharged into surface waters [31];
Target limit for the support of aquatic life [32];
Target limit for effluent to be discharged into the environment [33];
Target limit that would reduce eutrophication in aquatic ecosystems [34].
Figure 2.
Chlorine residual regime of the treated effluents during the 12 month study period.
Figure 3.
Scatter plot of the relationship between listerial density (total Listeria count) and chlorine residual. Total listerial density was not determined for the final effluent in the month of October; hence the listerial density for that month is not reflected in the figure.
3.4. Antibiogram and Resistance Gene Detection
Fifty-one presumptive Listeria pathogens were isolated from the final effluents following their morphological characteristics on LCA plates. Of the 51 isolates, 27 (53%) were confirmed to be L. ivanovii; 1 (2%) was L. innocua and the identity of the remaining 23 (45%) isolates were indeterminate by API test. Twenty-three (22 L. ivanovii and 1 L. innocua) of the 28 confirmed Listeria isolates were tested for phenotypic antibiotic susceptibility and the result is shown in Table 4. All 23 Listeria species were sensitive to three (15%) of the 20 test antibiotics including amikacin (aminoglycosides), meropenem, and ertapenem (carbapenems). Eight (35%) of the 23 Listeria isolates were moderately sensitive to moxifloxacin, cephalothin, gatifloxacin, ciprofloxacin and ceftriaxone; three strains showed moderate sensitivity to moxifloxacin, two to gatifloxacin, while the other three were each moderately sensitive to cephalothin, ciprofloxacin, and ceftriaxone. The test isolates showed resistance to 17 (85%) of the 20 antibiotics at percentages ranging from 4.5% to 91% (Table 4). Multiple antibiotic resistances was observed in 22 (95.7%) of the isolates in combinations ranging from four to 10 antibiotics; while one isolate showed resistance to a single antibiotic (aztreonam) (Table 5). Of the seven antimicrobial genes assayed in this study, only sulII genes were detected in five (22%) strains of Listeria ivanovii (Table 6).
Table 4.
In vitro antibiotic susceptibility profile of the Listeria strains isolated from the effluents.
| Antibiotics | Number of isolates (%) | ||
|---|---|---|---|
| Susceptible | Intermediate | Resistant | |
| Amikacin (30 μg) | 23(100) | 0(0) | 0(0) |
| Gentamycin(10 μg) | 19(83) | 0(0) | 4(17) |
| Streptomycin(25 μg) | (15)65 | 0(0) | 8(35) |
| Chloramphenicol(30 μg) | 20(87) | 0(0) | 3(13) |
| Tetracyclin(30 μg) | 19(83) | 0(0) | 4(17) |
| Ciprofloxacin(5 μg) | 21(91) | 1(4.5) | 1(4.5) |
| Gatifloxacin(5 μg) | 19(83) | 2(8.5) | 2(8.5) |
| Moxifloxacin(5 μg) | 17(74) | 3(13) | 3(13) |
| Imipenem(10 μg) | 19(83) | 0(0) | 4(17) |
| Meropenem(10 μg) | 23(100) | 0(0) | 0(0) |
| Ertapenem(10 μg) | 23(100) | 0(0) | 0(0) |
| Ampicillin(30 μg) | 3(13) | 0(0) | 20(87) |
| Penicillin G(10 μg) | 1(4.5) | 1(4.5) | 21(91) |
| Linezolid(30 μg) | 18(78) | 0(0) | 5(22) |
| Aztreonam(30 μg) | 21(91) | 0(0) | 2(9) |
| Erythromycin(15 μg) | 4(17) | 0(0) | 19(83) |
| Cephalothin(30 μg) | 17(74) | 1(4) | 5(22) |
| Ceftriaxone(30 μg) | 21(91) | 1(4.5) | 1(4.5) |
| Sulphamethoxazole (25 μg) | 8(35) | 0(0) | 15(65) |
| Trimethoprim(5 μg) | 17(74) | 0(0) | 6(26) |
Table 5.
Multiple antibiotic resistances of Listeria strains isolated from the chlorinated effluents.
| Antibiotics | Number of isolates involved | Percentage (%) |
|---|---|---|
| E, SMX, LZD, PG, AP | 7a | 31 |
| E, LZD, PG, AP | 2b | 8.7 |
| KF, E, SMX, LZD, PG, AP | 2b | 8.7 |
| E, TM, LZD, MFX, PG, AP | 1b | 4.3 |
| E, LZD, MFX, PG, AP | 1b | 4.3 |
| C, KF, E, S, T, SMX, LZD, GAT, PG, AP | 1b | 4.3 |
| E, S, T, SMX, LZD, MFX, PG, AP | 1b | 4.3 |
| KF, E, S, SMX, TM, LZD, PG, AP | 1b | 4.3 |
| CRO, KF, E, S, SMX, LZD, PG, AP, | 1b | 4.3 |
| E, S, SMX, LZD, PG | 1b | 4.3 |
| C, E, GM, S, SMX, TM, IMI, PG | 1b | 4.3 |
| GM, TM, IMI, AP | 1b | 4.3 |
| ATM, C, GM, S, T, TM, CIP, IMI, PG, AP | 1b | 4.3 |
| GM, S, T, TM, LZD, IMI, PG, AP | 1b | 4.3 |
| Total | 22 | 95.7 |
Legend: ATM = Aztreonam; E = Erythromycin; AP = Ampicillin; LZD = Linezolid; PG = Penicillin G; KF = Cephalothin; SMX = Sulphamethoxazole; TM = Trimethoprim; MFX = Moxifloxacin; C = Chloramphenicol; S = Streptomycin; GAT = Gatifloxacin; CRO = Ceftriaxone; IMI = Imipenem; GM = Gentamycin; T = Tetracycline; CIP = Ciprofloxacin.
One strain of L. innocua and six strains of L. ivanovii;
Strains of L. Ivanovii.
Table 6.
Occurrence of antimicrobial resistance genes in Listeria strains isolated from the final effluents.
| Antibiotic resistance gene markers | Proportion of Listeria pathogens carrying the resistance genes |
|---|---|
| penA | 0(0) |
| ampC | 0(0) |
| ermB | 0(0) |
| ereA | 0(0) |
| ereB | 0(0) |
| su1I | 0(0) |
| su1II | 5(22%) |
4. Discussion
The relative abundance of free-living Listeria species found during this study and across all sampled sites is consistent with reports elsewhere [13,35]. There are no recommended standards specific for Listeria pathogens in water and wastewater samples in South Africa for obvious reasons; thus the fecal coliforms standard (0 cfu/100 ml) for domestic water uses [30] was applied in this report. Based on this standard, the water quality across the studied water system and throughout the year (Table 2) fell short of acceptable target limits for domestic applications, thus disqualifying the waters for use in drinking and other domestic purposes. Listeria abundance did not vary significantly with season, either as free-living or plankton-associated species, consistent with the observation of Murrel et al. [36], but contrary to our previous report [13]. The significant positive correlation observed between Listeria species attached to large (180 μm) planktons and those attached to small (20 μm) planktons suggests that the two groups of Listeria species may occupy the same niche in the ecosystem; this is contrary to our previous report [13], where Listeria species attached to large (180 μm) planktons negatively correlated with those attached to small (20 μm) planktons. The lack of significant correlations between and among other treatments in this study suggests that free-living Listeria species and Listeria species attached to medium-sized (60 μm) planktons occupy separate niches in the water system, different from those occupied by Listeria species attached to large (180 μm) and small (20 μm) planktons. The observation is consistent with those of Maugeri et al. [24] who reported lack of significant correlation between free-living bacteria and plankton associated bacterial populations in a marine coastal zone in Italy. However, another study [37] reported a negative correlation between planktonic Vibrio cells and sessile populations.
Listeria species were isolated from all sampled sites and throughout the year during this study, suggesting a 100% prevalence of the pathogen in the water system. Consistent with observations in a previous study [13], free-living Listeria species were most prevalent (84%) both in treated effluent and the receiving watershed; followed by Listeria cells associated with planktons of sizes 180 μm (75%), 20 μm (68%), and 60 μm (59%), respectively. Corroborating this observation, Maugeri et al. [24] reported higher prevalence for free-living bacteria compared to their plankton-associated counterparts. Listeria species were generally more prevalent in the treated effluents (FE), both as free-living and/or plankton-associated cells, compared to the receiving watershed (Table 2). The observation could be as a result of higher nutrient levels in the wastewater effluents compared to the receiving watershed, in agreement with previous reports [10,11,38]. Consistent with the observation of this study, high prevalence of Listeria species has been reported in water systems impacted by wastewater effluents in Iraq [8,9], Poland [10] France [11], the United Kingdom [12] and rural South Africa [13]. Watkins and Sleath [12] reported 100% prevalence of Listeria species in sewage, river water, and trade effluent at densities (7.0 × 102 to >1.8 × 104 Most Probable Number (MPN)/mL), slightly higher than those observed in this study. The sewage effluent reported by Watkins and colleague, however, only underwent primary treatment unlike ours that was disinfected by chlorination, which could account for the differences. Al-Ghazali and Al-Azawi [8,9] also reported 100% prevalence in treated wastewater effluent in Iraq but at lower densities of <3 to 28 MPN/mL, and Paillard et al. [11] reported 84.4% prevalence of Listeria species in treated wastewater in France at densities ranging from <0.3 to 21 MPN/ml, while Odjadjare and Okoh [13] recorded 100% prevalence in a rural water system in South Africa at densities ranging from 1.0 × 101 to 1.1 × 104 cfu/mL. Contrary to the observation of this study, lower prevalence has been reported for Listeria species in a variety of surface water systems. Frances et al. [39] reported the isolation of Listeria species from 21% of freshwater samples collected from sites in Cheshire and North Wales; while Lyautey et al. [40] reported 64% for surface waters of the South Nation River Watershed in Ontario, Canada. These observations were consistent with expectations for surface waters that were not impacted by wastewater effluent in agreement with a report elsewhere [38].
The significant variation observed between raw and treated sewage for most physicochemical parameters (Table 3) is an indication that the wastewater treatment process remarkably improved the quality of the raw wastewater influent. However, despite the improvement on raw sewage quality, the treated effluent did not measure up to the desired target quality for turbidity, DO, COD, and NO2 with respect to domestic applications [30] and PO4 with reference to preserving the integrity of the aquatic ecosystem [34]. This suggests that the wastewater effluent has a potential negative impact on the environment and public health. The effluent quality was, however, acceptable in terms of pH, temperature, TDS, and NO3 (Table 3).
The chlorine residual (Figure 2) generally fell within acceptable target limits (0.3–0.6 mg/L) for domestic water at the point of use [41], except in September and November 2007, and indicates that the water is safe for domestic applications with reference to chlorine residual. The scatter plot (Figure 3) indicates that the relationship between chlorine residual and listerial density did not follow any particular trend. This observation suggests that factors other than chlorine disinfection affected the abundance of Listeria species during this study; some of these factors may also be responsible for the inability of chlorine to adequately eliminate the pathogens from the wastewater even at relatively high doses. LeChevallier et al. [42] observed attachment of bacteria to planktons and/or other suspended particles as a factor which enhanced resistance of bacteria to chlorine disinfection while Obi et al. [41] reported other factors to include contact time, temperature, and pH. This suggests that turbidity (which is a measure of suspended particles including planktons) could be a factor in the ineffectiveness of chlorine disinfection during this study; turbidity fell short of recommended target limits throughout the study (Table 3). Attachment of Listeria species to plankton may, however, not be a significant factor in the bacterial survival of chlorine disinfection in this study, as free-living Listeria species were more abundant compared to their plankton attached counterparts even after chlorine disinfection in agreement with the observation of our study elsewhere [13]. The reason for this observation is not clear.
Previous studies on the antimicrobial susceptibility profiles of Listeria species focused mainly on clinical and/or food isolates with little information in the literature on antibiotic susceptibility profiles for Listeria strains isolated from chlorinated municipal wastewater effluent. All 23 Listeria species tested in this study were sensitive to three (15%) of the 20 test antibiotics including amikacin (aminoglycosides), meropenem, and ertapenem (carbapenems) (Table 4); suggesting that these antibiotics may be the best therapy in the event of listeriosis outbreak in South Africa. Consistent with the observation of this study, Hansen et al. [43] reported complete sensitivity of 106 Listeria species isolated from humans to meropenem, while Safdar and Armstrong [44] observed 100% sensitivity to amikacin and Odjadjare and Okoh [13] reported complete sensitivity to the three antibiotics by all 14 Listeria species isolated from chlorinated wastewater effluent in a previous study.
Listeria strains in this study showed resistance to at least one of 17 antibiotics at percentages ranging from 4.5%–91% (Table 4), and particularly high levels for penicillin G (91%), ampicillin (87%), erythromycin (83%), and sulphamethoxazole (65%). Contrary to the observation of this study, Listeria species were generally reported to be susceptible to penicillin G [45], ampicillin [46], erythromycin [28,44], and sulphamethoxazole [13,43]. Conversely, considerable resistance has been reported in the literature for Listeria species against the penicillins (penicillin G and ampicillin) [21], erythromycin [13,47], and sulphamethoxazole [46]. The high resistance observed for penicillin G, ampicillin and sulphamethoxazole could be of serious public health concern as penicillin G and ampicillin are reported to be the antibiotics of choice in the treatment of listeriosis [28,43]; while sulphamethoxazole, usually in combination with trimethoprim, is considered second choice therapy, especially for patients who are allergic to the penicillins [46]. The observation generally indicated that municipal wastewater effluent could be a significant source of highly resistant strains of Listeria pathogens in the South African aquatic milieu.
The physicochemical quality of the wastewater effluent may be a factor in the level of resistance observed in this study, as it is widely reported [48–50] that conventional wastewater treatment plants lack the capacity to effectively remove antibiotics and a number of other chemicals from wastewater, thereby increasing the chances of bacterial pathogens resident in such wastewater effluent to develop resistance to common antibiotics due to selective pressure. Although we did not attempt to assay for residual antibiotics in the treated effluents in the course of this study, lack of capacity to remove some chemicals from the wastewater during the treatment process is evident in Table 3. The table shows that the treated effluent fell short of recommended standard quality for critical parameters such as turbidity, DO, COD, NO2, and PO4 and suggests a possible influence on the listerial resistance.
Twenty-two (95.7%) of the 23 test isolates in this study showed multiple antibiotic resistance in combinations ranging from four to 10 antibiotics (Table 5). Similar observations have been reported elsewhere [13,21]. On the contrary Conter et al. [28] reported more resistance to single antibiotics than multiple resistance amongst 120 Listeria isolates tested against 19 antibiotics; while Arslan and Ozdemir [51] reported resistance to single antibiotics with no record of multiple antibiotic resistance amongst 47 strains of Listeria species isolated from white cheese and tested against 13 antibiotics. Multiple drug resistance in Listeria species have been attributed to antimicrobial selective pressure and gene transfer mechanism between and among Listeria species and close relatives of the bacteria such as Enterococcus, Streptococcus and Staphylococcus species [44]. Donlan and Costerton [52] also reported the acquisition of inherent resistance to antimicrobial agents due to bacterial attachment to surfaces; suggesting that attachment to plankton at one point or the other may have enhanced the multiple resistances of our listerial strains to several test antibiotics.
Although the penicillins (penicillin G and ampicillin) and erythromycin showed the highest phenotypic resistance during this study, the genes responsible for resistance to these antibiotics were not detected in our Listeria isolates (Table 6). In a similar report, Srinivasan et al. [21] observed high level (92%) of phenotypic resistance to ampicillin but failed to detect the genes responsible for ampicillin resistance in all of their 38 Listeria isolates. Consistent with the observation of this study, Davis and Jackson [20] could not detect penA genes (responsible for penicillin resistance) in Listeria strains isolated from various sources; while Srinivasan et al. [21] reported their inability to detect genes responsible for erythromycin resistance in 38 Listeria isolates from dairy farms in spite of observed phenotypic resistance to the antibiotic. Contrary to the observation of this study, Srinivasan et al. [21] reported the detection of penA genes in 37% of their Listeria isolates while Roberts et al. [53] reported the detection of erythromycin resistance genes in Listeria species isolated from food samples. To the best of our knowledge, this is the first report on the detection of dihydropteroate synthetase type II (sulII) resistance gene markers in Listeria species (Table 6). Previous attempt by other workers [20,21] did not detect the genes in Listeria species. The percentage of Listeria isolates that harbored this gene was, however, relatively small (22%) compared to the high (65%) level of phenotypic resistance observed for the antibiotic (sulphametoxazole) in this study. The observations generally suggests that the presence of antimicrobial resistance genes in bacterial isolates do not always correlate with phenotypic antibiotic resistance, and indicates that other mechanisms such as decreased outer membrane permeability, activation of efflux pump, or mutation in a ribosomal protein may have contributed to the antimicrobial resistance phenotypes observed in this study [21].
5. Conclusions
The current study demonstrated that the activated sludge treatment process was ineffective in removing Listeria pathogens and other contaminants from the municipal wastewater prior to discharge into the receiving watershed; thereby posing serious threat to the integrity of the receiving environment and its ability to support life; as well as endangering the public health of the people who depend on this all important water resource for drinking and other purposes. Therefore, it is imperative that the relevant monitoring agencies take proactive steps aimed at curtailing an impending listeriosis outbreak in South Africa in the interest of the public health.
Acknowledgments
We are grateful to the National Research Foundation (NRF) for funding this research under the focus area program.
References
- 1.Roberts AJ, Wiedmann M. Pathogen, host and environmental factors contributing to the pathogenesis of listeriosis. Cell. Mol. Life Sci. 2003;60:904–918. doi: 10.1007/s00018-003-2225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brugere-Picoux O. Ovine listeriosis. Small Ruminant Res. 2008;76:12–20. [Google Scholar]
- 3.Cummins AJ, Fielding AK, McLauchlin J. Listeria ivanovii infection in a patient with AIDS. J. Infect. 1994;28:89–91. doi: 10.1016/s0163-4453(94)94347-8. [DOI] [PubMed] [Google Scholar]
- 4.Cocolin L, Rantsiou K, Iacumin L, Cantoni C, Comi G. Direct identification in food samples of Listeria spp. and Listeria monocytogenes by molecular methods. Appl. Environ. Microbiol. 2002;68:6273–6282. doi: 10.1128/AEM.68.12.6273-6282.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker JK, Morgan JH, McLauchlin J, Grant KA, Shallcross JA. Listeria ivanovii isolated from a case of ovine meningoencephalitis. Vet. Microbiol. 1994;59:193–202. doi: 10.1016/0378-1135(94)90023-x. [DOI] [PubMed] [Google Scholar]
- 6.Rocourt J, Jacquet Ch, Reilly A. Epidemiology of human listeriosis and seafoods. Int. J. Food Microbiol. 2000;62:197–209. doi: 10.1016/s0168-1605(00)00336-6. [DOI] [PubMed] [Google Scholar]
- 7.Siegman-Igra Y, Levin R, Weinberger M, Golan Y, Schwartz D, Samra Z, Konigsberger H, Yinnon A, Rahav G, Keller N, Basharat N, Karpuch J, Finkelstein R, Alkan M, Landau Z, Novikov J, Hassin D, Rudnicki C, Kitzes R, Ovadia S, Shimoni Z, Lang R, Shohat T. Listeria monocytogenes infection in Israel and review of cases worldwide. Emerging Infect. Dis. 2002;8:305–310. doi: 10.3201/eid0803.010195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al-Ghazali MR, Al-Azawi KS. Detection and enumeration of Listeria monocytogenes in a sewage treatment plant in Iraq. J. Appl. Bacteriol. 1986;60:251–254. doi: 10.1111/j.1365-2672.1986.tb01080.x. [DOI] [PubMed] [Google Scholar]
- 9.Al-Ghazali MR, Al-Azawi KS. Effects of sewage treatment on the removal of Listeria monocytogenes. J. Appl. Bacteriol. 1988;65:203–208. doi: 10.1111/j.1365-2672.1988.tb01886.x. [DOI] [PubMed] [Google Scholar]
- 10.Czeszejko K, Boguslawska-Was E, Dabrowski W, Kaban S, Umanski R.Prevalence of Listeria monocytogenes in municipal and industrial sewage Electron J Pol Agric Univ Environ Dev 20036; Available online: http://www.ejpau.media.pl (accessed 4 November 2008). [Google Scholar]
- 11.Paillard D, Dubois V, Thiebaut R, Nathier F, Hoogland E, Caumette P, Quentin C. Occurrence of Listeria spp. in effluents of French urban wastewater treatment plants. Appl. Environ. Microbiol. 2005;71:7562–7566. doi: 10.1128/AEM.71.11.7562-7566.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Watkins J, Sleath KP. Isolation and enumeration of Listeria monocytogenes from sewage, sewage sludge, and river water. J. Appl. Bacteriol. 1981;50:1–9. doi: 10.1111/j.1365-2672.1981.tb00865.x. [DOI] [PubMed] [Google Scholar]
- 13.Odjadjare EEO, Okoh AI. Prevalence and distribution of Listeria pathogens in the final effluents of a rural wastewater treatment facility in the Eastern Cape Province of South Africa. World J. Microbiol. Biotechnol. 2010;26:297–307. [Google Scholar]
- 14.Mackintosh G, Colvin C. Failure of rural schemes in South Africa to provide potable water. Environ. Geol. 2003;44:101–105. [Google Scholar]
- 15.Okoh AI, Odjadjare EE, Igbinosa EO, Osode AN. Wastewater treatment plants as a source of pathogens in receiving watersheds. Afr. J. Biotechnol. 2007;6:2932–2944. [Google Scholar]
- 16.Venter SN. Microbial water quality in the 21st century. SA Water bull. 2001;27:16–17. [Google Scholar]
- 17.Djordjevic D, Wiedmann M, McLandsborough LA. Microtitre assay for assessment of Listeria monocytogenes biofilm formation. Appl. Environ. Microbiol. 2002;68:2950–2958. doi: 10.1128/AEM.68.6.2950-2958.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lunden JM, Miettinen MK, Autio TJ, Korkeala H. Persistent Listeria monocytogenes strains show enhanced adherence to food contact surface after short contact times. J. Food Prot. 2000;63:1204–1207. doi: 10.4315/0362-028x-63.9.1204. [DOI] [PubMed] [Google Scholar]
- 19.Mafu A, Roy D, Goulet J, Magny P. Attachment of Listeria monocytogenes to stainless steel, glass, polypropylene and rubber surfaces after short contact times. J. Food Prot. 1990;53:742–746. doi: 10.4315/0362-028X-53.9.742. [DOI] [PubMed] [Google Scholar]
- 20.Davis JA, Jackson CR. Comparative antimicrobial susceptibility of Listeria monocytogenes, L. innocua, and L. welshimeri. Microb. Drug Res. 2009;15:28–32. doi: 10.1089/mdr.2009.0863. [DOI] [PubMed] [Google Scholar]
- 21.Srinivasan V, Nam HM, Nguyen LT, Tamilselvam B, Murinda SE, Oliver SP. Prevalence of antimicrobial resistance genes in Listeria monocytogenes isolated from dairy farms. Foodborne Pathog. Dis. 2005;2:201–211. doi: 10.1089/fpd.2005.2.201. [DOI] [PubMed] [Google Scholar]
- 22.Obi CL, Onabolu B, Momba MNB, Igumbor JO, Ramalivahna J, Bossong PO, van Rensburg EJ, Lukoto M, Green E, Mulaudzi TB. The interesting cross-paths of HIV/AIDS and water in Southern Africa with special reference to South Africa. Water SA. 2006;32:323–343. [Google Scholar]
- 23.Daily Dispatch. Report highlights cholera risk profile. Thursday January 30, 2003; Available online: http://www.dispatch.co.za/2003/01/30/easterncape/BCHOLERA.HTM (accessed on 12 September 2008).
- 24.Maugeri TL, Carbon M, Fera MT, Irrera GP, Gugliandolo C. Distribution of potentially pathogenic bacteria as free-living and plankton associated in a marine coastal zone. J. Appl. Microbiol. 2004;97:354–361. doi: 10.1111/j.1365-2672.2004.02303.x. [DOI] [PubMed] [Google Scholar]
- 25.Hitchins AD.Detection and enumeration of Listeria monocytogenes in foods Bacteriological Analytical Manual US Food and Drug Administration; Madison, WI, USA: 2001; Available online: http://www.cfsan.fda.gov/∼ebam/bam-toc.html (accessed on 4 November 2008). [Google Scholar]
- 26.DWAF . Analytical Methods Manual, TR 151. Department of Water Affairs and Forestry; Pretoria, South Africa: 1992. [Google Scholar]
- 27.CLSI Performance Standards for Antimicrobial Susceptibility Testing; Fifteenth Informational Supplement, M100-S15, vol. 251Clinical and Laboratory Standards Institute; Wayne, PA, USA: 2005163 [Google Scholar]
- 28.Conter M, Paludi D, Zanardi E, Ghidini S, Vergara A, Ianieri A. Characterization of antimicrobial resistance of foodborne Listeria monocytogenes. Int. J. Food Microbiol. 2009;128:497–500. doi: 10.1016/j.ijfoodmicro.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 29.Naravaneni R, Jamil K. Rapid detection of food-borne pathogens by using molecular techniques. J. Med. Microbiol. 2005;54:51–54. doi: 10.1099/jmm.0.45687-0. [DOI] [PubMed] [Google Scholar]
- 30.DWAF . South African Water Quality Guidelines: Domestic Use. 2nd ed. Vol. 2 Department of Water Affairs and Forestry; Pretoria, South Africa: 1996. [Google Scholar]
- 31.WHO Rolling Revision of the WHO Guidelines for Drinking-Water Quality, Draft for Review and Comments Nitrates and Nitrites in Drinking-Water World Health Organization; (WHO/SDE/WSH/04.08/56), 2004 [Google Scholar]
- 32.Fatoki SO, Gogwana P, Ogunfowokan AO. Pollution assessment in the Keiskamma River and in the impoundment downstream. Water SA. 2003;29:183–187. [Google Scholar]
- 33.SA Government Gazette Requirements for the Purification of Wastewater or Effluent; Gazette No. 9225, Regulation 991, 1984
- 34.DWAF . South African Water Quality Guidelines: Aquatic Ecosystems. 1st ed. Vol. 7 Department of Water Affairs and Forestry; Pretoria, South Africa: 1996. [Google Scholar]
- 35.Venkateswaran K, Takai T, Navarro IM, Nakano H, Hashimoto H, Siebeling RJ. Ecology of Vibrio cholerae non-01 and Salmonella spp. and role of zooplankton in their seasonal distribution in Fukuyama coastal waters, Japan. Appl. Environ. Microbiol. 1989;55:1591–1598. doi: 10.1128/aem.55.6.1591-1598.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Murrell MC, Hollibaugh JT, Silver MW, Wong PS. Bacterioplankton dynamics in Northern San Francisco Bay: role of particle association and seasonal freshwater flow. Limnol. Oceanogr. 1999;44:295–308. [Google Scholar]
- 37.Hsieh JL, Fries JS, Noble RT. Vibrio and phytoplankton dynamics during the summer of 2004 in a eutrophying estuary. Ecol. Appl. 2007;17:S102–S109. [Google Scholar]
- 38.Dijkstra RG. The occurrence of Listeria monocytogenes in surface waters of canals and lakes, in ditches of one big polder and in the effluents and canals of a sewage treatment plant. Zentralbl. Bakteriol. Mikrobiol. Hyg. B. 1982;176:202–205. [PubMed] [Google Scholar]
- 39.Frances N, Hornby H, Hunter PR. The isolation of Listeria species from freshwater sites in Cheshire and North Wales. Epidemiol. Infect. 1991;107:235–238. doi: 10.1017/s0950268800048858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lyautey E, Lapen DR, Wilkes G, McCleary K, Pagotto F, Tyler K, Hartmann A, Piveteau P, Rieu A, Robertson WJ, Medeiros DT, Edge TA, Gannon V, Topp E. Distribution and characteristics of Listeria monocytogenes isolates from surface waters of the South Nation River Watershed, Ontario, Canada. Appl. Environ. Microbiol. 2007;73:5401–5410. doi: 10.1128/AEM.00354-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Obi CL, Igumbor JO, Momba MNB, Samie A. Interplay of factors involving chlorine dose, turbidity, flow capacity and pH on microbial quality of drinking water in small treatment plants. Water SA. 2008;34:565–572. [Google Scholar]
- 42.LeChevallier MW, Cawthan CD, Lee RG. Factors promoting survival of bacteria in chlorinated water supplies. Appl. Environ. Microbiol. 1988;54:649–654. doi: 10.1128/aem.54.3.649-654.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hansen JM, Gerna-Smidt P, Bruun B. Antibiotic susceptibility of Listeria monocytogenes in Denmark 1958–2001. Acta Pathol. Microbiol. Immunol. Scand. 2005;113:31–36. doi: 10.1111/j.1600-0463.2005.apm1130105.x. [DOI] [PubMed] [Google Scholar]
- 44.Safdar A, Armstrong D. Antimicrobial activities against 84 Listeria monocytogenes isolates from patients with systemic listeriosis at a comprehensive cancer center (1955–1997) J. Clin. Microbiol. 2003;41:483–485. doi: 10.1128/JCM.41.1.483-485.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abuin CMF, Fernandez EJQ, Sampayo CF, Otero JTR, Rodriguez LD, Cepeda S. Susceptibilities of Listeria species isolated from food to nine antimicrobial agents. Antimicrob. Agents Chemother. 1994;38:1655–1657. doi: 10.1128/aac.38.7.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhang Y, Yeh E, Hall G, Cripe J, Bhagwat AA, Meng J. Characterization of Listeria monocytogenes isolated from retail foods. Int. J. Food Microbiol. 2007;113:47–53. doi: 10.1016/j.ijfoodmicro.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 47.Aureli P, Ferrrini AM, Mannoni V, Hodzic S, Wedell-Weergaard C, Oliva B. Susceptibility of Listeria monocytogenes isolated from food in Italy to antibiotics. Int. J. Food Microbiol. 2003;83:325–330. doi: 10.1016/s0168-1605(02)00381-1. [DOI] [PubMed] [Google Scholar]
- 48.Giger W, Alder AC, Golet EM, Kohler HE, McArdell CS, Molnar E, Siegrist H, Suter MJ-F. Occurrence and fate of antibiotics as trace contaminants in wastewaters, sewage sludges, and surface waters. Chimia. 2003;57:485–491. [Google Scholar]
- 49.Kummerer K. Significance of antibiotics in the environment. J. Antimicrob. Chemother. 2003;52:5–7. doi: 10.1093/jac/dkg293. [DOI] [PubMed] [Google Scholar]
- 50.Volkmann H, Schwartz T, Bischoff P, Kirchen S, Obst U. Detection of clinically relevant antibiotic-resistance genes in municipal wastewater using real-time PCR (TaqMan) J. Microbol. Methods. 2004;56:277–286. doi: 10.1016/j.mimet.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 51.Arslan S, Ozdemir F. Prevalence and antimicrobial resistance of Listeria spp. in homemade white cheese. Food Control. 2008;19:360–363. [Google Scholar]
- 52.Donlan RM, Costerton JW. Biofilms: survival mechanism of clinically relevant microorganisms. Clin. Microbiol. Rev. 2002;15:167–193. doi: 10.1128/CMR.15.2.167-193.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roberts CM, Facinelli B, Giovanetti E, Varaldo PE. Transferable erythromycin in Listeria spp. isolated from food. Appl. Environ. Microbiol. 1996;62:269–270. doi: 10.1128/aem.62.1.269-270.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]