Abstract
Purpose of Review
Surgeons have long been striving to develop new surgical procedures to improve functional outcomes for a variety of hand and wrist deformities resulting from rheumatoid arthritis (RA). The purpose of this review is to assess the latest surgical outcomes related to hand and wrist surgery in the patient with RA.
Recent Findings
There is a lack of outcomes studies in RA hand and wrist surgery to justify many of the surgical procedures proposed for the treatment of the rheumatoid hand. However, advances made by the silicone metacarpophalangeal arthroplasty (SMPA) Group regarding hand reconstruction for RA patients have improved patient care for this widely used procedure. Prophylactic versus therapeutic procedures are also discussed.
Summary
Rheumatoid hand is one of the earliest presentations of RA, and the progression of rheumatoid hand disease can be unpredictable. There are a number of surgical treatments for the rheumatoid hand and careful sequential planning of the surgical procedures can maintain patients’ hand function and in many cases, should enhance outcomes of the rheumatoid hand by correcting existing deformities. An early introduction to a hand surgeon can inform patients of available options and allow longitudinal assessment of structural and functional changes that could be treatable by future surgical interventions.
Keywords: Rheumatoid arthritis, outcomes, reconstruction, hand, wrist
Introduction
Treatment of the rheumatoid hand has been mired in controversy. For years, surgeons have been devising new surgical procedures to improve functional outcomes for a variety of hand and wrist deformities resulting from rheumatoid arthritis (RA). However, surgeons often lament that RA patients are sent for hand surgery consultations too little and too late. Prior studies have shown that one reason for the lack of referral for hand surgery evaluation is the paucity of collaborative working relationships between rheumatologists and hand surgeons.[1, 2] The lack of clinical interactions has been shown to affect the quality of care due to specialists not receiving a timely referral for consultation.[2] Another concern is the lack of outcomes studies in RA hand surgery to justify many of the surgical procedures proposed for the treatment of the rheumatoid hand. The lack of outcomes studies is related to the complexity of many rheumatoid hand conditions and the difficulty in designing clinical trials for the rheumatoid hand because of patient preferences regarding treatment options as well as the many hurdles inherent in multi-center clinical trials for surgical diseases.
Outcomes
An extensive review of several rheumatoid hand surgery procedures found that surgical management is still not standardized.[3] Available studies are mostly of low quality, consisting of case studies rather than randomized controlled trials, containing patients with heterogeneous diagnoses and disease severity, and assessing patients at inconsistent time intervals and with varying outcomes measures. These research design deficiencies were highlighted in a systematic review of patient outcomes after silicone metacarpophalangeal joint arthroplasty (SMPA).[4] It is difficult to compare the outcomes of a particular procedure when the available studies are so heterogeneous. These sentiments are echoed by rheumatologists; in a national survey, only 19% of rheumatologists felt that high quality information was available for surgical options and outcomes for the rheumatoid hand.[1] Although there are large variations in the rates of rheumatoid hand surgery performed in the US,[5, 6] there are also large variations in the rates of rheumatoid hand surgery performed around the world.[7] Economically privileged countries such as the United States, France, and Japan tend to have aggressive surgical approaches to correcting rheumatoid hand deformities as opposed to a country with an emerging economy such as China.[7] Family support, which is usually more available in Asian countries, also seems to play a role in discouraging surgery for the RA hand.
Because of the lack of evidence for most rheumatoid hand surgical procedures, the SMPA Group has set out to determine the outcomes of the widely used SMPA procedure (Figure 1). The SMPA Group has published their short-term study findings (up to 1 year) in several manuscripts.[8**,9,10,11**,12*,13**,14*] At 1-year, the outcomes of the two groups—surgical versus medically-treated only—were compared.[8**] The surgical group consisted of patients who chose to undergo SMPA, whereas the control group consisted of patients who were managed only medically. Both groups were eligible to undergo the SMPA procedure based on strict hand deformity eligibility criteria. The surgical group and medical group were statistically similar in terms of age, race, education, and income. The patient-assessed outcomes questionnaire results using the Michigan Hand Outcomes Questionnaire showed significant improvement in the surgical group, but no change in the medical group despite worse baseline function in the surgical group. Ulnar deviation and extensor lag improved significantly in the surgical group, but biomechanical measures showed no significant improvement. The medical group’s function did not deteriorate during the 1-year follow-up interval. This study was consistent with previous findings of surgical patients that showed improvement in ulnar drift, extensor lag, and health-related quality of life, but no improvement in other standard functional measures (such as grip and pinch strength).[9, 15–17]
Figure 1.
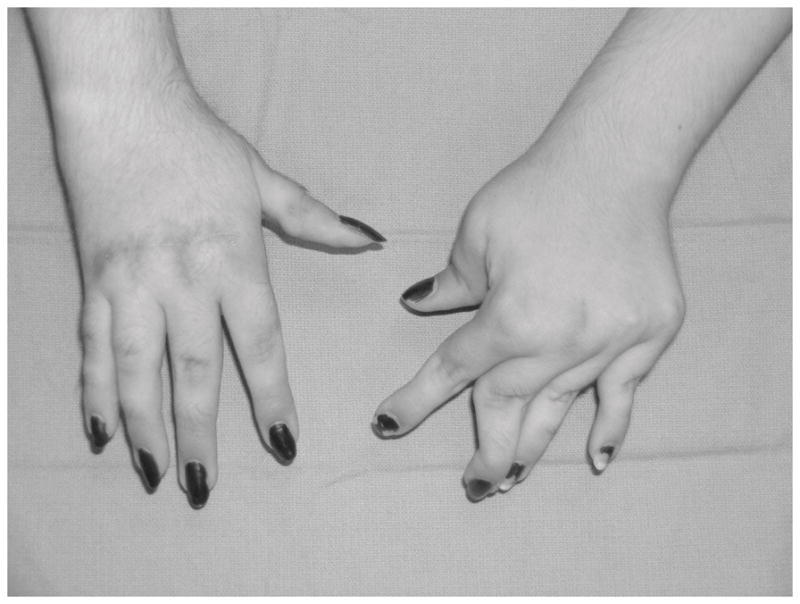
Silicone arthroplasty in the right hand. Note the well aligned fingers when compared to the unoperated hand.
The SMPA Group set out to determine if more severe metacarpophalangeal (MCP) joint deformity resulted in worse outcomes following SMPA. One year postoperatively, 70 surgical group patients were analyzed by categorizing them into two groups: those with more MCP joint deformity and those with less MCP joint deformity.[13**] There were no significant differences between these two groups in terms of grip/pinch strength, ability to perform activities of daily living, or outcomes questionnaire scores. Patients in the more deformed group did have significantly more extensor lag and ulnar drift compared to the less deformed group. This study showed that surgical reconstruction is beneficial for all RA patients with MCP joint deformity, regardless of the degree of deformity.
Popular surgical belief indicates that after SMPA, the ulnar fingers will have less improvement than the radial fingers, marked with greater ulnar drift, extension lag, and less MCP joint arc of motion. However, 1-year after surgery, the SMPA Group found that the opposite was true; for both ulnar drift and extension lag, the largest improvement was seen in the little finger and the smallest improvement in the index finger. The largest improvement in MCP joint arc of motion was seen in the two ulnar fingers.[11**]
It is unknown if hand function in RA patients with MCP joint deformity will remain the same or decline over longer follow-up periods, whether they undergo SMPA reconstruction or not. The SMPA Group will follow these two groups of patients for 3 years and possibly longer.
Prophylactic versus Therapeutic Surgical Procedures
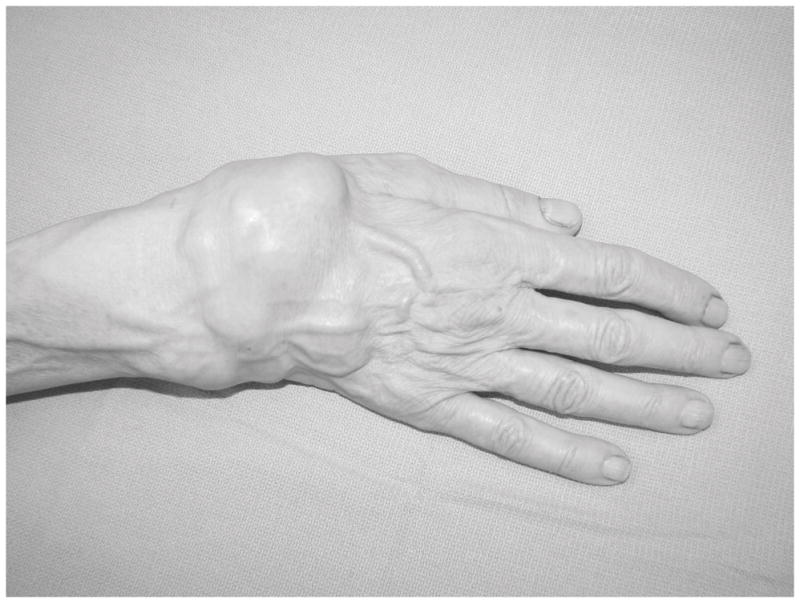
Rheumatoid hand interventions can be categorized into prophylactic and therapeutic surgical procedures. Prophylactic procedures include the removal of inflammatory synovial tissue before synovial hypertrophy stretches the ligamentous support around joints, which can cause a tendon imbalance, or before synovial tissue invades into tendons, causing tendon rupture, or before it destroys the articular cartilage. This prophylactic procedure is tenosynovectomy in which hypertrophic synovial tissues are removed from the extensor or flexor tendons or sometimes from wrist joints or finger joints (Figure 2). Distal ulna excision also can be considered a prophylactic procedure because a dorsally displaced, eroded distal ulna can cause attritional rupture of the extensor tendons (Figure 3), and the altered biomechanics of the distal radio-ulnar joint can affect pronation and supination motions. Therapeutic surgical treatment is proposed for patients who have intractable pain due to arthritic wear of the joint or rupture of the extensor tendons. Additional surgical procedures for destroyed joints are either joint replacement surgery (arthroplasty) or joint fusion (arthrodesis). However, for cases involving tendon rupture, tendon transfer procedures to restore finger motion are excellent solutions for restoring function.
Figure 2.
Diffuse synovitis that is classic for a patient with rheumatoid arthritis. This patient will require synovectomy to prevent tendon ruptures and progressive wrist joint destruction.
Figure 3.

Extensor tendon rupture of the left ring and little fingers.
Prophylactic Surgical Procedures
With the introduction of newer RA medications, proliferation of the synovial tissue is under much better control and surgeons have observed that the rate of rheumatoid hand surgery has been decreasing. Many active rheumatoid hand surgery programs are seeing fewer patients requiring synovectomy procedures, and the severe hand and wrist deformities seen in the past are not encountered as frequently today. However, in other regions of the world where medical resources are limited and rationed, costly disease-modifying drugs or biologic medications are not readily available and the incidence of hand surgery has not seen a general decline. The SMPA Group found that RA patients in the United States are more likely to take biologic medications (p<0.001), steroids (p=0.02), and Cox-2 inhibitors (p=0.02) than RA patients with similar disease severity in the United Kingdom.[12*]
Performing outcomes research on these prophylactic procedures is difficult because patients need to be followed for a prolonged period of time in order to observe whether the prophylactic procedures have avoided certain complications resulting from untreated synovitis. It is generally accepted that if a patient has persistent dorsal synovitis of the extensor mechanism for greater than 3 months despite optimal medical management, then consultation with a hand surgeon is necessary to consider the extensor tenosynovectomy procedure. However, there has not been sufficient evidence to demonstrate that synovectomy can effectively decrease the incidence of tendon ruptures. Furthermore, it is intriguing to consider whether the often performed excision of hypertrophic synovial tissues in the small joints of the hand or the wrist may retard the destruction of the articular cartilage. Again, prospective long-term studies are not available to support joint synovectomy as an effective adjunctive procedure to medical treatment. However, it is known that synovitis can stretch the support ligaments around the joints and lead to joint instability and finger deformities. Henceforth, for effective prevention of secondary deformities of the rheumatoid hand, optimal medical treatment is certainly advocated and if synovitis persists for 3 to 6 months despite optimal medical treatment, then surgical removal of the synovial tissue theoretically should prevent destruction of the support ligaments and potentially decrease the inflammatory response within the joints that would eventually lead to joint destruction. For a patient who has instability of the distal radio-ulnar joint and crepitus over the dorsal extensor tendons from rubbing of the extensor tendons over the eroded head of the ulna, surgical consultation is advised to consider surgical procedures to prevent eventual attritional rupture of the extensor tendons. Excision of the distal ulna is a common surgical procedure for the rheumatoid wrist and removing the offending distal ulna as a cause of tendon irritation can prevent tendon ruptures that may be more difficult to repair than to prevent.
For the wrist, prophylactic open synovectomy of the wrist joint has not been shown to be an effective treatment. Because of the complexity of the wrist joint and the multiple compartments within the wrist, complete synovectomy is impossible to achieve. With the recent advances in wrist arthroscopic assisted synovectomy, persistent wrist synovitis may be treated effectively by using the shaver through portals in the wrist for effective debridement.
Therapeutic Procedures
Once the joints are destroyed or the tendons are ruptured, then therapeutic options should be considered. For example, when the little finger extensor tendon is ruptured, the surgeon can suture the distal end of the ruptured tendon to the ring finger, thereby using the ring finger extensor tendon to power the little finger. There are many strategies available for treating tendon ruptures using tendon transfer procedures, and these procedures should carefully consider the biomechanical properties of available tendons to replace the function of the ruptured tendons.
For destroyed joints, the choices are either arthroplasty or arthrodesis. Because the destruction of the joints is often accompanied by ligamentous instability, from the hand surgeon’s perspective there are certain joints that should have arthrodesis and certain joints that should have arthroplasty. For example, stability of the thumb is of utmost importance because the thumb usually functions as a post for grip. Therefore, the thumb interphalangeal (IP) joint and the MCP joint are often fused to provide stability, whereas the thumb carpometacarpal joint is often treated with arthroplasty in order to maintain the motion of the thumb. For the fingers, the distal IP joint should be treated with fusion because the tip of the finger requires stability and injudicious arthroplasty procedure of this joint can lead to instability and disastrous outcomes. As previously described, for the MCP joint, arthroplasty procedures are most appropriate. In the rheumatoid proximal IP joint, the inherent lack of ligament support in RA as well as tendon imbalances make the arthroplasty procedure a difficult option. The arthroplasty procedure using implants requires stability of the ligaments to support the joints and without sufficiently good ligamentous support, fusion is often the best choice for the proximal IP joint.
The wrist joint is an area of great interest among hand surgeons. Hand surgeons often want to strive to maintain wrist motion and when the wrist is destroyed, a variety of limited joint fusion procedures can be proposed for the wrist in order to maintain some motion and at the same time alleviate pain.[18–22] However, for RA patients with severe painful wrist destruction, the options are either wrist arthrodesis or arthroplasty. Arthrodesis is a time honored procedure in order to fuse the wrist and provide a stable platform for patients to use their hands more effectively. Although wrist fusion will rob the patient of motion of the wrist, many of these patients do not have much motion of their arthritic wrist joints, and they usually have accommodated and can tolerate the wrist fusion rather well. Interestingly, the appearance of wrist destruction on x-ray is not an indication for surgery because paradoxically, many patients with severe changes on the x-ray may not have much pain and can function remarkably well. An experienced hand surgeon will want to understand the patient’s expectations and motivations for seeking hand surgery consultation. If a patient is still able to accommodate with a markedly destroyed wrist, I will often defer surgery until the pain becomes more incapacitating or the wrist deformity progressively affects the hand function. The surgeon should carefully weigh both the advantages and disadvantages of surgical treatment in order to provide the most appropriate treatment options for the patient.
Wrist arthroplasty has become an increasingly active area of research in hand surgery (Figures 4 and 5). Research to design new wrist implants to avoid wrist fusion is progressing rapidly and our recent studies have shown that arthroplasty is slightly more preferred by patients, hand surgeons, and rheumatologists compared to arthrodesis and that both procedures are cost-effective.[23] Wrist arthroplasty is not without complications.[24**] Rheumatoid patients undergoing the wrist arthroplasty procedure may have a higher incidence of failure because of the lack of integration of the wrist implant in RA patients with marginal bone stock. However, patients and surgeons do prefer the wrist arthroplasty procedure in an effort to maintain some wrist motion. Better implant materials and design should make this technology much more predictable and suitable to maintain function of the rheumatoid wrist.
Figure 4.

Pre-operative x-ray of a patient requiring wrist arthroplasty for treatment of a painful RA wrist.
Figure 5.

Post-operative x-ray of wrist arthroplasty. Please note the good bone stock in this RA patient that can support the wrist implant components.
Conclusion
Although the incidence of severe rheumatoid hand condition is decreasing in the United States, rheumatoid hand is one of the earliest presentations of RA, and the progression of rheumatoid hand disease can be unpredictable. In early consultation with a hand surgeon, RA patients should be carefully assessed for suitability of surgical treatment and informed of available options. Surgical consultation does not equate to planning surgery, but can be an early introduction to the hand surgeon who may be of service to the patient in the future. There are a number of surgical treatments for the rheumatoid hand and careful sequential planning of the surgical procedures can maintain patients’ hand function and in many cases, should enhance outcomes of the rheumatoid hand by correcting existing deformities. Prospective outcomes studies are underway in order to assess the effectiveness of a number of common hand surgical procedures in order to derive high-level evidence regarding the use of these surgical treatments. A collaborative relationship between rheumatologists and hand surgeons to derive these outcomes data is critical, as demonstrated by the SMPA Group studies that result from the collaboration between rheumatologists and hand surgeons at each center to conjointly devise the study protocol for understanding the outcomes of the SMPA procedure. Additional efforts are underway for the evaluation of the surgical treatment of wrist diseases in rheumatoid hands. Until the cure for RA is found, hand surgeons will continue to be valuable partners of rheumatologists to aid in the team effort directed at the rehabilitation of RA patients.
Acknowledgments
Supported in part by a grant from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01 AR047328) and a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
References
- 1.Alderman AK, Chung KC, Kim HM, et al. Effectiveness of rheumatoid hand surgery: contrasting perceptions of hand surgeons and rheumatologists. J Hand Surg. 2003;28A:3–11. doi: 10.1053/jhsu.2003.50034. [DOI] [PubMed] [Google Scholar]
- 2.Alderman AK, Ubel PA, Kim HM, et al. Surgical management of the rheumatoid hand: consensus and controversy among rheumatologists and hand surgeons. J Rheumatol. 2003;30:1464–1472. [PubMed] [Google Scholar]
- 3.Ghattas L, Mascella F, Pomponio G. Hand surgery in rheumatoid arthritis: state of the art and suggestions for research. Rheumatology. 2005;44:834–845. doi: 10.1093/rheumatology/keh608. [DOI] [PubMed] [Google Scholar]
- 4.Chung KC, Kowalski CP, Myra Kim H, Kazmers IS. Patient outcomes following Swanson silastic metacarpophalangeal joint arthroplasty in the rheumatoid hand: a systematic overview. J Rheumatol. 2000;27:1395–1402. [PubMed] [Google Scholar]
- 5.Alderman AK, Chung KC, DeMonner S, et al. Large area variations in the surgical management of the rheumatoid hand. Surg Forum. 2001;LII:479–481. [Google Scholar]
- 6.Alderman AK, Chung KC, Demonner S, et al. The rheumatoid hand: a predictable disease with unpredictable surgical practice patterns. Arthritis Rheum. 2002;47:537–542. doi: 10.1002/art.10662. [DOI] [PubMed] [Google Scholar]
- 7.Kotsis SV, Chung KC. A qualitative assessment of rheumatoid hand surgery in various regions of the world. J Hand Surg. 2005;30A:649–657. doi: 10.1016/j.jhsa.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 8**.Chung KC, Burns PB, Wilgis EF, et al. A multicenter clinical trial in rheumatoid arthritis comparing silicone metacarpophalangeal joint arthroplasty with medical treatment. J Hand Surg. 2009;34A:815–823. doi: 10.1016/j.jhsa.2009.01.018. This is the first study to include a medically-treated control group. It also assesses patients prospectively at designated time intervals with standardized patient-assessed outcomes questionnaires and biomechanical measures. This is the largest cohort of RA patients enrolled with strict eligibility criteria for hand deformity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg. 2004;29A:646–653. doi: 10.1016/j.jhsa.2004.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chung KC, Kotsis SV, Kim HM, et al. Reasons why rheumatoid arthritis patients seek surgical treatment for hand deformities. J Hand Surg. 2006;31A:289–294. doi: 10.1016/j.jhsa.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 11**.Chung KCKS, Wilgis EFS, Fox DA, et al. Outcomes of silicone arthroplasty for rheumatoid metacarpophalangeal joints stratified by finger. J Hand Surg. 2009;34A:1647–1652. doi: 10.1016/j.jhsa.2009.06.029. The SMPA Group used the cohort of patients from their prospective, standardized outcomes study to demonstrate that contrary to popular surgical opinion, the radial fingers actually had better outcomes than the ulnar fingers. This study improves both surgeons’ and patients’ knowledge of surgical expectations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12*.Chung KC, Fox DA, Regan M, et al. Differences between the United States and the United Kingdom in the treatment of rheumatoid arthritis: Analyses from a hand arthroplasty trial. Clinical Rheumatology. doi: 10.1007/s10067-009-1314-9. In Press. The authors postulate that the differences in medication intake between the RA patients in the United States and the United Kingdom may be influenced by the private versus socialized health care systems. This study alerts researchers to consider the potential influence of differing healthcare systems as a confounder on treatment outcomes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13**.Chung KC, Burke FD, Wilgis EFS, et al. A comparative prospective outcomes study to evaluate whether more severe ulnar drift deformities in the rheumatoid hands have worse outcomes after reconstruction. Plast Reconstr Surg. 2009;123:1521–1532. doi: 10.1097/PRS.0b013e3181a65b5a. This study provides evidence that challenges the commonly held view among surgeons that silicone metacarpophalangeal joint arthroplasty produces much better outcomes if the hand deformities (extensor lag and ulnar drift) are less severe. Although more severe hand deformities are more difficult to correct, RA patients in late stages of hand deformity should still be referred to a hand surgeon for consultation. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14*.Mandl LA, Burke FD, Shaw Wilgis EFS, et al. Could preoperative preferences and expectations influence surgical decision making? Rheumatoid arthritis patients contemplating metacarpophalangeal joint arthroplasty. Plast Reconstr Surg. 2008;121:175–180. doi: 10.1097/01.prs.0000295376.70930.7e. This study found that improving hand appearance and hand function were most often cited by patients as “very important” in their decision to undergo silicone metacarpophalangeal joint arthroplasty. The medically-treated patients were more bothered by hand weakness. The authors found that patients who were eligible for the arthroplasty procedure but chose not to have it seemed to have different surgical expectations and preferences than the patients who did undergo the procedure. [DOI] [PubMed] [Google Scholar]
- 15.McArthur PA, Milner RH. A prospective randomized comparison of Sutter and Swanson silastic spacers. J Hand Surg. 1998;23B:574–577. doi: 10.1016/s0266-7681(98)80004-1. [DOI] [PubMed] [Google Scholar]
- 16.Rothwell AG, Cragg KJ, O’Neill LB. Hand function following Silastic arthroplasty of the metacarpophalangeal joints in the rheumatoid hand. J Hand Surg. 1997;22B:90–93. doi: 10.1016/s0266-7681(97)80027-7. [DOI] [PubMed] [Google Scholar]
- 17.Sollerman CJ, Geijer M. Polyurethane versus silicone for endoprosthetic replacement of the metacarpophalangeal joints in rheumatoid arthritis. Scand J Plast Reconstr Surg Hand Surg. 1996;30:145–150. doi: 10.3109/02844319609056397. [DOI] [PubMed] [Google Scholar]
- 18.Kozlow J, Chung KC. Rheumatoid and osteoarthritis. In: Serletti J, Losee J, editors. Current Reconstructive Surgery. 1. Pending Publication; [Google Scholar]
- 19.Chung KC. Rheumatoid arthritis. In: Chung KC, editor. Hand Surgery, Plastic Surgery. St. Louis: Mosby; 2008. pp. 1271–1284. [Google Scholar]
- 20.Chung KC. Silicone metacarpophalangeal joint arthroplasty. In: Chung KC, editor. Operative Techniques: Hand and Wrist Surgery. 1. Philadelphia: Saunders/Elsevier; 2007. pp. 725–738. [Google Scholar]
- 21.Chung KC. Total wrist arthroplasty. In: Chung KC, editor. Operative Techniques: Hand and Wrist Surgery. Philadelphia: Saunders/Elsevier; 2007. pp. 739–756. [Google Scholar]
- 22.Chung KC. Tendon transfers for the rheumatoid arthritis patient. In: Chung KC, editor. Operative Techniques: Hand and Wrist Surgery. 1. Philadelphia: Saunders/Elsevier; 2007. pp. 757–770. [Google Scholar]
- 23.Cavaliere CM, Chung KC. A cost utility analysis of non-operative management, total wrist arthroplasty, and total wrist fusion in rheumatoid arthritis. J Hand Surg, Am. doi: 10.1016/j.jhsa.2009.12.013. Submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24**.Cavaliere CM, Chung KC. A systematic review of arthroplasty versus arthrodesis for the rheumatoid wrist. Plastic and Reconstructive Surgery. 2008;122(3):813–825. doi: 10.1097/PRS.0b013e318180ece3. This systematic review evaluated the literature for outcomes of wrist arthroplasty and wrist arthrodesis for RA. This study found that arthrodesis provided more reliable relief than arthroplasty. Complication and revision rates were higher for arthroplasty. The authors concluded that the existing data do not support the adoption of arthroplasty as the standard of care over arthrodesis for patients with end-stage rheumatoid wrist. This study also highlighted the need for prospective randomized trials to evaluate complications, functional outcomes, and patient satisfaction for both procedures. [DOI] [PubMed] [Google Scholar]


