Abstract
The Women’s Recovery Group study was a Stage I randomized clinical trial comparing a new manual-based group treatment for women with substance use disorders with Group Drug Counseling. Data from this study were examined to determine whether co-occurring symptoms of depression and anxiety would improve with treatment and whether these improvements would demonstrate durability over the follow-up period. The sample consisted of 36 women (29 WRG, 7 GDC) who were administered self-report and clinician-rated measures of anxiety, depression, and general psychiatric symptoms. Although there were no group differences in psychiatric symptom improvement, analyses demonstrated significant within-subject improvement in depression, anxiety, and general psychiatric symptoms. Symptom reduction was not mediated by changes in substance use. This study demonstrated significant psychiatric symptom reduction that remained durable through 6 month follow-up for women receiving group therapy focused on substance abuse relapse prevention. Reduction in psychiatric symptoms may be an additional benefit of substance abuse group therapy for women.
Keywords: substance dependence, relapse prevention, co-occurring disorders, gender, depression, anxiety
Psychiatric disorders are highly prevalent among individuals with substance use disorders (Compton, Thomas, Stinson, & Grant, 2007; Grant et al., 2004; Kessler et al., 1997) and can have adverse effects on substance abuse relapse and recovery (for review, see Bradizza, Stasiewicz, & Paas, 2006). The relationship between co-occurring substance use and other psychiatric disorders may be particularly relevant for women, who have both higher overall rates of mood and anxiety disorders (Kessler, Chiu, Demler, & Walters, 2005) as well as higher rates of co-occurring substance use and psychiatric disorders relative to men (Brady, Grice, Dustan, & Randall, 1993). Although results of studies examining the relationship between co-occurring psychiatric disorders or symptoms and substance abuse treatment outcomes have been mixed (e.g., Cacciola, Alterman, Rutherford, McKay, & Mulvaney, 2001; Carroll, Power, Bryant, & Rounsaville, 1993; Charney, Paraherakis, & Gill, 2001; DiSclafani, Finn, & Fein, 2007; Greenfield et al., 1998; Kranzler, DelBoca, & Rounsaville, 1996), the disability associated with co-occurring psychiatric disorders highlights the alleviation of these symptoms as an important treatment target. Indeed, in recent years a consensus has emerged in the field emphasizing the need to attend to co-occurring disorders in the treatment of substance use disorders.
Given the clear need for integrated treatment for substance use and co-occurring depression and anxiety, determining the most effective treatment strategy is of particular importance. Across psychological disorders, little is known about the relative benefits of transdiagnostic or integrated treatments as compared to single-disorder interventions. For example, studies in the anxiety disorders have suggested that co-occurring disorders improve when treating a principle disorder (Brown & Barlow, 1995; Borkovec, Abel, & Newman, 1995), and that adding components to a treatment to target co-occurring disorders may not demonstrate additive benefits to treatment outcome (Craske et al., 2007). However, given the similarities among unipolar mood and anxiety disorders (e.g., Brown, 2007; Brown, Chorpita, & Barlow, 1998), these results may not generalize to more heterogeneous clinical presentations, such as co-occurring substance use and anxiety disorders.
The development of integrated treatments for substance use and mood and anxiety disorders is in relatively early stages of evaluation. Early studies have suggested the potential for improved outcomes with integrated treatments for both depression (e.g., Brown, Evans, Miller, Burgess, & Mueller, 1997; Charney et al., 2001; Curry, Wells, Lochman, Craighead, & Nagy, 2003; Weiss et al., 2007) and anxiety disorders (e.g., Brady, Dansky, Back, Foa, & Carroll, 2001; Fals-Stewart & Schafer, 1992; Najavits, Weiss, Shaw, & Muenz, 1998). However, given the relatively early stage of this research area, few randomized controlled trials have specifically evaluated these approaches in co-occurring substance use and unipolar mood and anxiety disorders. Randomized controlled trials evaluating treatments targeted to co-occurring substance use and anxiety disorders have found improvement in both substance use and anxiety symptoms with treatment; however specialized interventions have not demonstrated additive efficacy over standard substance abuse treatment (e.g., Bowen, D’Arcy, Keegan, & Senthilselvan, 2000; Randall et al. 2001). A recent review of randomized studies of integrated psychosocial treatments for substance use and depression and anxiety indicated that integrated treatments for depression demonstrated modest results for both depression and anxiety, with few studies of integrated treatments for anxiety available (Hesse, 2009). Fewer studies of integrated treatments for anxiety were available, and they were characterized by mixed results.
Studies of symptom changes over time in single-disorder substance use treatment suggest that symptoms of both substance abuse and psychiatric conditions tend to decrease with treatment. An early study of men with alcohol use disorders demonstrated that depressive symptoms, as assessed by semi-structured clinical interview, declined from moderate levels at the start of treatment to normal in almost all subjects achieving abstinence (Brown & Schuckit, 1988). Furthermore, 40% of participants reported clinical levels of depression at pre-treatment and only 6% maintained this level of symptoms following treatment. However, the study included only male participants confined to residential treatment and did not assess co-occurring depressive disorder diagnosis. Indeed, co-occurring depression is less likely to be substance-induced among women relative to men (Schuckit et al., 1997), and thus women may need more treatment to target depression. In a sample of 188 patients (60 women) treated at both day and residential polysubstance abuse treatment programs, change throughout treatment in psychiatric symptom severity as measured by the Addition Severity Index (ASI; McLellan, Kushner, Metzger, & Peters, 1992) psychiatric composite score and the Beck Depression Inventory (BDI; Beck & Steer, 1987) was evaluated (Guydish et al., 1999). BDI scores, but not ASI psychiatric composite scores significantly decreased over the 18-month treatment episode for both the day and residential treatment modalities, in addition to significant improvement in substance use outcomes.
Studies to date suggest that depression and anxiety symptom improvement may be seen in both treatments targeting co-occurring disorders, and those specifically targeting the substance use disorder. Given the importance of determining the most effective interventions for treating co-occurring depression/anxiety and substance use disorders, the benefits of single-disorder relative to integrated treatments is of particular importance. Furthermore, as many studies have examined all or mostly male samples, less is known about this relationship in women, for whom it may be particularly relevant.
The aim of the current exploratory study was to examine the course of psychiatric symptoms among women receiving substance abuse group therapy as part of a Stage I clinical trial. The Women’s Recovery Group (WRG) study was a treatment development trial that examined the efficacy of group psychotherapy for women with women-focused content compared with a group treatment with demonstrated efficacy, Group Drug Counseling (GDC) (see Greenfield, Trucco, McHugh, Lincoln, & Gallop, 2007). The WRG study assessed symptoms prospectively utilizing a general measure of psychiatric symptoms, as well as specific measures of depression and anxiety symptoms. The specific aims of this analysis were to determine: (1) whether psychiatric symptoms in general, and depressive and anxiety symptoms in particular, would improve during substance abuse group therapy, (2) if this change in symptoms would differ between the two group treatments, and (3) whether changes in substance use would mediate the association between time and psychiatric symptom change.
Method
Participants
Thirty-six women identified as meeting Diagnostic and Statistical Manual, 4th Edition (DSM-IV; American Psychological Association, 1994) criteria for a diagnosis of current substance dependence were enrolled in a Stage I group therapy treatment development trial. Participants were recruited from substance abuse treatment facilities and community advertisements. The mean age of the sample was 47.6 years (SD = 11.4). Additionally, participants were highly educated (82.6% held at least a college degree) and all but one participant identified as Caucasian (97.8%). Fifty-eight percent of the sample worked full or part time, 17% reported working as a homemaker, and approximately 8% were students, 8% retired, and 8% were unemployed. Psychiatric diagnoses were assessed at baseline using the Structured Clinical Interview for DSM-IV for Axis I (First, Spitzer, Gibbon, & Williams, 2002) and Axis II (First, Spitzer, Gibbon, & Williams, 1997) disorders. Participants were excluded if they met diagnostic criteria for a current psychotic disorder, bipolar disorder, or post-traumatic stress disorder (for further description of sample, see Greenfield et al., 2007). Despite the common co-occurrence of these disorders with substance use disorders, potential participants with these diagnoses were excluded given the prior existence of efficacious treatment for these co-occurring disorders (e.g., post-traumatic stress disorder; Hien, Cohen, Miele, Litt, & Capstick, 2004; bipolar disorder; Weiss et al, 2007).
Most women were currently dependent on alcohol (92%), with 13% of the total sample meeting for a current drug use disorder. Among those enrolled, 58.3% and 38.9% additionally met diagnostic criteria for current Axis I and Axis II disorders, respectively. Thirty-nine percent (n = 14) of participants met criteria for a current mood disorder and 33.3% (n = 12) for an anxiety disorder. Of these participants, only 1 was diagnosed with a substance-induced mood and 1 with a substance-induced anxiety disorder. Five (13.9%) participants met criteria for obsessive-compulsive personality disorder (PD), 3 (8.3%) for depressive PD, 1 (2.8%) for borderline PD, and 5 (13%) for two or more PDs.
Procedures
Detailed methods for the Women’s Recovery Group (WRG) study, including description of the treatment protocols have been reported previously (see Greenfield et al., 2007). Participants were randomly assigned to in either the WRG (n = 29) or GDC (n = 7) interventions. The GDC group included both men (n = 10) and women (n = 7); only the women were included in this analysis. All participants received 12, 90-minute sessions of outpatient group psychotherapy for substance use disorders. Study therapists were doctoral or master’s level clinicians, who received training and weekly supervision in addition to fidelity ratings assessed by videotape. The WRG is a manualized, cognitive-behavioral group therapy for substance use disorders. The sessions follow a relapse prevention model and provide content related to issues specifically relevant to women. This content (e.g., the effects of drugs and alcohol on women’s health; impact of partners on recovery, etc) would not be expected to target symptoms of anxiety and depression more than the GDC group; however, the WRG group additionally included a session on Axis I disorders and symptoms that commonly co-occur in women (i.e., anxiety, mood, and eating disorders) and patients are encouraged to seek additional support for such problems as needed. The content of this session focused on encouraging participants to identify these symptoms and to understand that unless they are treated, they can be an obstacle to recovery. The GDC intervention is a manualized relapse-prevention group that covers typical recovery group topics with no gender-specific content. It is typically administered to mixed-gender groups and there are no studies of GDC in single-gender group format. No direct intervention for co-occurring psychiatric disorders is included in the GDC protocol.
In this analysis, data from the 36 women enrolled in treatment were examined to determine whether symptoms of depression and anxiety would improve with treatment and whether these improvements would demonstrate durability over the follow-up period. In addition, the WRG and GDC conditions were compared to determine whether the WRG intervention would provide any additive benefits relative to psychiatric symptom outcomes. Results from the primary outcome analysis suggested that there were similar reductions in substance use in the two groups at post-treatment, but by 6-month follow-up the WRG condition demonstrated significantly greater reductions in substance use (Greenfield et al., 2007), and thus the 6-month follow-up time point was examined separately to evaluate any potential differences emerging at that time. All participants were included in the analysis, regardless of psychiatric diagnoses at baseline in order to examine the range of both clinical and sub-clinical symptoms and their progression over time.
Measures
Primary outcome measures included two self-report measures, the Beck Anxiety Inventory (BAI; Beck et al. 1988) and the Beck Depression Inventory (Beck & Steer, 1987); and one interviewer-administered measure, the Addiction Severity Index (McLellan et al., 1992). The BAI and BDI are widely used self-report measures of symptoms of anxiety and depression, respectively. The ASI is a commonly utilized semi-structured interview, which measures functioning across several domains. Composite scores representing the level of functional difficulty can be calculated for each of the seven areas. The ASI has consistently demonstrated strong psychometric properties (e.g., McLellan, Cacciola, Alterman, Rikoon, & Carise, 2006; Stoffelmayr, Mavis & Kasim, 1994). The Timeline Follow-back method (TLFB; Sobell & Sobell, 1992) was utilized to examine the extent of substance use over the 30 days prior to each assessment. The number of days of substance use in the past 30 days was utilized as the measure of substance use for this analysis and was selected because it was the primary outcome measure in the main treatment outcome study. All study measures were administered at baseline, end of treatment and 3 and 6 months following treatment termination.
Statistical Analysis
Prior to examination of the primary study aims, differences between the WRG and GDC groups on baseline values of primary outcome measures were examined utilizing independent samples t-tests and χ2 tests. Both between- and within-subjects changes in symptoms over time were examined using repeated-measures analysis of variance (ANOVA). Additionally, to examine whether changes in psychiatric symptoms were present among those with greater baseline psychiatric severity, participants meeting diagnostic criteria for a current mood disorder (n = 12) or a current anxiety disorder (n = 14) were examined separately. In order to examine greater severity in the interviewer-rated measure, a median split of ASI psychiatric composite scores at baseline was used. Finally, mediational analyses involved evaluation of the association between time and substance use change, between time and psychiatric symptom change, and finally between substance use change and psychiatric symptom change consistent with the recommendations of Baron and Kenny (1986). In the case of significant associations between all of these variables, the association between time and psychiatric symptoms controlling for substance use change would be evaluated.
A conservative approach to missing data was utilized; in the case of a missing value, the value at the previous time point was carried forward (e.g., missing value at 3-month follow-up was replaced with value from post-treatment). Replacement values were provided for 3 participants for the BDI, 1 participant for the BAI, and no participants for the ASI psychiatric composite score. Participants for whom baseline values were missing (n = 2 for the BDI) or for whom more than 1 value was missing (n = 3 for all measures due to treatment drop-out) were excluded from analyses.
Results
Prevalence of Axis I and Axis II disorders and values of outcome measures at each time point are presented in Table 1. No significant differences were found between groups at baseline on the BDI (t(32) = 0. 473, ns), the BAI (t(34) = 0.72, ns), the ASI psychiatric composite score (t(34) = 0.76, ns), or rates of co-occurring Axis I (χ2 = 1.22, ns) or Axis II (χ2 0.01, ns) diagnoses. There were also no differences by group in the proportion of patients in individual psychotherapy at baseline (t(34) = −0.87, ns). Three participants in the WRG condition began individual psychotherapy during treatment, 1 for substance use specifically, 1 for reasons other than substance use or psychiatric problems, and 1 for psychiatric problems. In the GDC condition, no changes in psychotherapy were reported during treatment or in the follow-up phase. The difference in proportion of patients in psychotherapy remained non-significant at all assessment points. GDC women had more self-help attendance during treatment; neither psychotherapy nor self-help attendance mediated the main outcome findings during treatment or in the post-follow-up period. Repeated-measures ANOVAs were conducted comparing symptom reduction in the two treatment conditions and no significant group × time interaction effects were found for the BDI, (F(3,26) = 0.05, ns), the BAI, (F(3,30) = 1.29, ns), or the ASI psychiatric composite, (F(3,31) = 0.01, ns). Moreover, an independent-samples t-test comparing psychiatric symptoms at the 6-month follow-up assessment point indicated no significant differences between groups on the BDI (t(29) = −0.02, ns), the BAI (t(31) = −0.89, ns), or the ASI psychiatric composite (t(31) = 0.36, ns).
Table 1.
Baseline Means (SD) of Symptom Measures and Rates of Current Co-occurring Diagnoses
| Measure | Baseline | Post-treatment | 3 month | 6 month |
|---|---|---|---|---|
| BDI | ||||
| WRG | 12.93 (9.23) | 6.96 (5.25) | 6.19 (5.21) | 8.07 (7.93) |
| GDC | 15.00 (12.84) | 10.67 (8.12) | 11.67 (9.56) | 8.67 (5.47) |
| BAI | ||||
| WRG | 10.21 (12.71) | 6.33 (7.72) | 6.04 (8.24) | 5.30 (4.40) |
| GDC | 14.00 (11.40) | 8.83 (6.34) | 10.33 (12.11) | 7.33 (7.61) |
| ASI Psych | ||||
| WRG | 0.28 (0.22) | 0.29 (0.20) | 0.17 (0.17) | 0.25 (0.17) |
| GDC | 0.35 (0.27) | 0.24 (0.23) | 0.22 (0.20) | 0.22 (0.20) |
| Mood disorders | ||||
| WRG | 37.9% | -- | -- | -- |
| GDC | 42.9% | -- | -- | -- |
| Anxiety disorders | ||||
| WRG | 31.0% | -- | -- | -- |
| GDC | 42.9% | -- | -- | -- |
| Other Axis I disorders | ||||
| WRG | 6.8% | -- | -- | -- |
| GDC | 0.0% | -- | -- | -- |
| Axis II disorders | ||||
| WRG | 34.5% | -- | -- | -- |
| GDC | 57.1% | -- | -- | -- |
Note. BDI = Beck Depression Inventory, BAI = Beck Anxiety Inventory, ASI Psych = Addiction Severity Index Psychiatric Composite score; Axis I and II disorders were assessed only at baseline.
Repeated-measures ANOVA examining the within-subjects change over time indicated a significant effect of time on outcome for the BDI (F(3,28) = 4.65, p < .01), the BAI (F(3,30) = 2.83, p < .05), and the ASI psychiatric composite score (F(3,30) = 2.87, p < .05). These results reflect a significant decrease in both self-reported and clinician-rated measures of psychiatric severity over time.
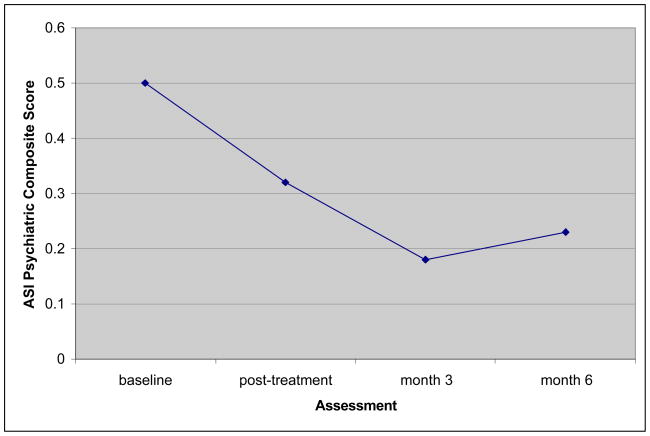
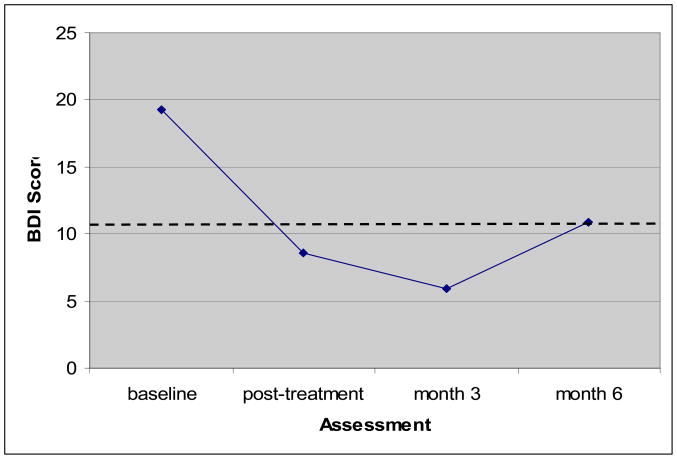
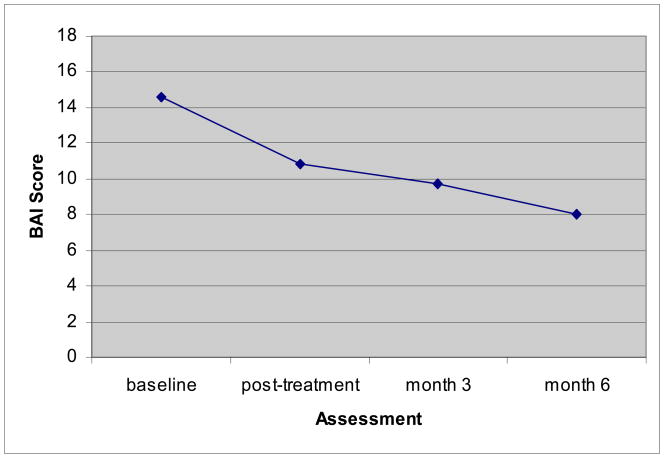
Symptom reduction was particularly notable among women with greater psychiatric symptom severity at baseline. Participants were split based on current mood disorder for the BDI, current anxiety disorder for the BAI, and in order to examine this effect in the interviewer-rated measures, a median split was utilized. Results of a repeated-measures ANOVA suggested a significant severity × time interaction for the BDI (F(3, 27) = 4.81, p < .01) characterized by greater symptom reduction among those with a current mood disorder, but no interaction effect for the BAI (F(3, 29) = 0.76, ns) or the ASI psychiatric composite score (F(3, 29) = 1.42, ns). Given the limited sample size, this data was also plotted to complement traditional significance testing with visual inspection. For the ASI psychiatric composite score symptom reduction was noted at post-treatment and both 3 and 6 months following termination of treatment (see Figure 1). Figure 2 shows the decrease in self-reported symptoms of depression at baseline, post-treatment and 3- and 6-month follow-up. Figure 3 shows the course of self-reported anxiety symptoms over time. Both anxiety and depression symptoms reduced below a clinical level (20 for the BAI; Leyfer, Ruberg, & Woodruff-Borden, 2006 and 11 for the BDI; Furlanetto, Mendlowicz, & Bueno, 2005) by post treatment with maintenance of gains through 6 months following treatment discontinuation, complementing the findings of the interviewer-administered assessment.
Figure 1.
Change in ASI scores among participants with elevated baseline scores (n=13)
Figure 2.
Change in BDI scores among participants with unipolar mood disorders (n=12)
Note. Dashed line represents clinical cutoff score.
Figure 3.
Change in BAI scores among participants with anxiety disorders (n=14)
Note. Clinical cut-off score (BAI = 20) is not listed as all scores fell below this level.
In the mediational analysis, although both substance use and psychiatric symptoms decreased over time, the association between change in substance use symptoms and psychiatric symptoms was not significant at any time point (rs range from −0.29–0.14, all ns). In addition, when evaluating whether substance use change in the previous time period (e.g., baseline to post treatment) was associated with psychiatric symptom reduction in the subsequent time period (e.g., post-treatment to 3-month follow-up), no significant associations were found for any of the measures at any time point. Thus, the final step of evaluating mediation was not conducted given the absence of an association between the potential mediator (substance use) and the outcome variable (psychiatric symptoms).
Discussion
With the high prevalence of co-occurring substance use and psychiatric disorders in women, and their importance in relapse and recovery, understanding the nature of psychiatric symptom change in substance abuse treatment is crucial to maximizing treatment effectiveness. In this study of the course of psychiatric symptoms during 12 weeks of group substance abuse treatment, significant psychiatric symptom reduction was found, which remained durable through 6 months post-treatment. This symptom reduction was particularly notable among individuals with greater baseline psychiatric severity.
The change in psychiatric symptoms was not related to the change in mean days of substance use, implying that decrease in substance use was not a mediator of psychiatric symptom change. However, the small sample size and study design limited may have limited the ability to detect a mediating effect. Evaluation of this effect in larger samples will be necessary to replicate this finding with greater statistical power.
There are several potential explanations for this finding. For example, improvement in the substance use disorder may facilitate change in co-occurring symptoms through reduction in use of psychoactive substances that may alter mood or reduction of life stressors. Alternatively, treatment components, such as building effective problem-solving or improving self-efficacy, may generalize to other symptoms. Additionally, this may be due to common vulnerabilities that might underlie both psychiatric and substance abuse symptoms (e.g., high negative affect, distress intolerance), which may change as a function of treatment and thus lead to improvement across symptoms of each disorder. Future research is needed to examine these and other potential mediators of change in substance abuse treatment.
This study has several limitations. Diagnostic information was not collected at follow-up and thus changes in diagnostic status following treatment are unknown. Future studies in which diagnoses are evaluated post-treatment may provide more information relative to changes in clinical status. Furthermore, the small sample size limited the power to detect change; however the presence of statistically and clinically significant symptom change suggests that the finding of psychiatric symptom reduction was robust. In addition, the analysis was adequately powered (0.80) to detect a large effect size in the between-groups analysis; therefore, more modest effects would not have been detected. Finally, the sample was relatively homogeneous in its sociodemographic composition and this study excluded individuals with co-occurring psychotic, bipolar, or post-traumatic stress disorders and thus the generalizability of these findings to these patient groups is unclear. Thus, further research on the course of co-occurring psychiatric symptoms in women during substance use disorder treatment will be needed to determine whether this finding will extend to other groups.
Given the importance of attending to co-occurring disorders among those with substance use disorders, the evaluation of the most effective treatment modalities is of particular importance. In particular, the degree to which integrated treatments or single-disorder treatments may provide effective strategies for treating co-occurring disorders is an important area for future research. Indeed, if symptom remediation can be achieved in single-disorder treatments (such as the WRG and GDC interventions) among some patients, this may provide a more efficient, and perhaps more cost-efficient, intervention for those patients. However, evaluation of whether integrated treatments may provide greater, more durable, or quicker improvement relative to single-disorder treatments is an important area for evaluation. The field has taken several perspectives on the treatment of co-occurring disorders, including treating the more severe or principal disorder, targeting symptoms of both disorders in an integrated intervention (e.g. substance use disorders and bipolar disorder; Weiss et al., 2007), and treating vulnerabilities that may be associated with multiple disorders (e.g., unified treatment approaches for affective disorders; Barlow, Allen, & Choate, 2004); however, at this time it is unclear which approach will provide the greatest efficacy/effectiveness. Moreover, exciting developments in the area of modular or treatment element-based approaches may have promise for matching treatments to individual clinical presentations (see McHugh, Murray, & Barlow, in press). Further understanding of the etiology of these disorders will allow for better targeted treatments for patients with more than one disorder. The results from this study and others show promise for the efficacy of treatments for co-occurring substance use and psychiatric disorders.
Contributor Information
R. Kathryn McHugh, Department of Psychology, Boston University
Shelly F. Greenfield, McLean Hospital; Department of Psychiatry, Harvard Medical School
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorder. 4. Washington, DC: Author; 1994. [Google Scholar]
- Barlow DH, Allen LB, Choate M. Toward a unified treatment for emotional disorders. Behavior Therapy. 2004;35:205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Manual for the revised Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- Borkovec TD, Abel JL, Newman H. Effects of psychotherapy on comorbid conditions in generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1995;63:479–483. doi: 10.1037//0022-006x.63.3.479. [DOI] [PubMed] [Google Scholar]
- Bowen RC, D’Arcy C, Keegan D, Senthilselvan A. A controlled trial of cognitive behavioral treatment of panic in alcoholic inpatients with comorbid panic disorder. Addictive Behaviors. 2000;25:593–597. doi: 10.1016/s0306-4603(99)00017-9. [DOI] [PubMed] [Google Scholar]
- Brady KT, Dansky BS, Back SE, Foa EB, Carroll KM. Exposure therapy in the treatment of PTSD among cocaine-dependent individuals: preliminary findings. Journal of Substance Abuse Treatment. 2001;21:47–54. doi: 10.1016/s0740-5472(01)00182-9. [DOI] [PubMed] [Google Scholar]
- Brady KT, Grice DE, Dustan L, Randall C. Gender differences in substance use disorders. American Journal of Psychiatry. 1993;150:1707–1711. doi: 10.1176/ajp.150.11.1707. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: A review. Clinical Psychology Review. 2006;26:162–178. doi: 10.1016/j.cpr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Brown RA, Evans M, Miller IM, Burgess ES, Mueller TI. Cognitive-behavioral treatment for depression in alcoholism. Journal of Consulting and Clinical Psychology. 1997;65:715–726. doi: 10.1037//0022-006x.65.5.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Schuckit MA. Changes in depression among abstinent alcoholics. Journal of Studies on Alcohol. 1988;49:412–417. doi: 10.15288/jsa.1988.49.412. [DOI] [PubMed] [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology. 2007;116:313–28. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Long-term outcome in cognitive-behavioral treatment of panic disorder: Clinical predictors and alternative strategies for assessment. Journal of Consulting and Clinical Psychology. 1995;63:754–765. doi: 10.1037//0022-006x.63.5.754. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Cacciola JS, Alterman AI, Rutherford MJ, McKay JR, Mulvaney FD. The relationship of psychiatric comorbidity to treatment outcomes in methadone maintained patients. Drug and Alcohol Dependence. 2001;61:271–280. doi: 10.1016/s0376-8716(00)00148-4. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Power ME, Bryant K, Rounsaville BJ. One-year follow-up status of treatment-seeking cocaine abusers: Psychopathology and dependence severity as predictors of outcome. Journal of Nervous and Mental Disease. 1993;181:71–79. doi: 10.1097/00005053-199302000-00001. [DOI] [PubMed] [Google Scholar]
- Charney DA, Palacios-Boix J, Negrete JC, Dobkin PL, Gill KJ. Association between concurrent depression and anxiety and six-month outcome of addiction treatment. Psychiatric Services. 2005;56:927–933. doi: 10.1176/appi.ps.56.8.927. [DOI] [PubMed] [Google Scholar]
- Charney DA, Paraherakis AM, Gill KJ. Integrated treatment for comorbid depression and substance use disorders. Journal of Clinical Psychiatry. 2001;62:672–677. doi: 10.4088/jcp.v62n0902. [DOI] [PubMed] [Google Scholar]
- Compton WM, Thomas YF, Stinson FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2007;64:566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- Craske MG, Farchione TJ, Allen LB, Barrios V, Stoyanova M, Rose R. Cognitive behavioral therapy for panic disorder and comorbidity: More of the same or less of more? Behaviour Research and Therapy. 2007;45:1095–1109. doi: 10.1016/j.brat.2006.09.006. [DOI] [PubMed] [Google Scholar]
- Curry JF, Wells KC, Lochman JE, Craighead WE, Nagy PD. Cognitive-behavioral intervention for depressed, substance-abusing adolescents: development and pilot testing. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:656–665. doi: 10.1097/01.CHI.0000046861.56865.6C. [DOI] [PubMed] [Google Scholar]
- Di Sclafani V, Finn P, Fein G. Psychiatric comorbidity in long-term abstinent alcoholics. Alcoholism: Clinical and Experimental Research. 2007;31:795–803. doi: 10.1111/j.1530-0277.2007.00361.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fals-Stewart W, Schafer J. The treatment of substance abusers with obsessive-compulsive disorder: An outcome study. Journal of Substance Abuse Treatment. 1992;9:365–370. doi: 10.1016/0740-5472(92)90032-j. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, research version, patient edition with psychotic screen. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV personality disorders (SCID-II) Washington, D.C: American Psychiatric Press; 1997. [Google Scholar]
- Furlanetto LM, Mendlowicz MV, Bueno JR. The validity of the Beck Depression Inventory-Short Form as a screening and diagnostic instrument for moderate and severe depression in medical inpatients. Journal of Affective Disorders. 2005;86:87–91. doi: 10.1016/j.jad.2004.12.011. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders. Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Trucco ET, McHugh RK, Lincoln M, Gallop R. The Women’s Recovery Group Study: A stage I trial of women-focused group therapy for substance use disorders versus mixed-gender Group Drug Counseling. Drug and Alcohol Dependence. 2007;90:39–47. doi: 10.1016/j.drugalcdep.2007.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, et al. The effect of depression on return to drinking: A prospective study. Archives of General Psychiatry. 1998;55:259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Guydish J, Sorensen JL, Chan M, Werdegar D, Bostrom A, Acampora A. A randomized trial comparing day and residential drug abuse treatment: 18-month outcomes. Journal of Consulting and Clinical Psychology. 1999;67:428–434. doi: 10.1037//0022-006x.67.3.428. [DOI] [PubMed] [Google Scholar]
- Hesse M. Integrated psychological treatment for substance use and co-morbid anxiety or depression v. treatment for substance abuse alone. A systematic review of the published literature. BMC Psychiatry. 2009;9:6. doi: 10.1186/1471-244X-9-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hien DA, Cohen LR, Miele GM, Litt LC, Capstick C. Promisingtreatments for women with comorbid PTSD and substance use disorders. American Journal of Psychiatry. 2004;161:1426–1432. doi: 10.1176/appi.ajp.161.8.1426. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: A posttreatment natural history study. Journal of Studies on Alcohol. 1996;57:619–626. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- Leyfer OT, Ruberg JL, Woodruff-Borden J. Examination of the utility of the Beck Anxiety Inventory and its factors as a screener for anxiety disorders. Anxiety Disorders. 2006;20:444–458. doi: 10.1016/j.janxdis.2005.05.004. [DOI] [PubMed] [Google Scholar]
- McHugh RK, Murray HW, Barlow DH. Balancing fidelity and adaptation in the dissemination of empirically-supported treatments: The promise of transdiagnostic interventions. Behaviour Research and Therapy. doi: 10.1016/j.brat.2009.07.005. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan AT, Cacciola JC, Alterman AI, Rikoon SH, Carise D. The addiction severity index at 25: origins, contributions, and transitions. The American Journal on Addiction. 2006;15:113–124. doi: 10.1080/10550490500528316. [DOI] [PubMed] [Google Scholar]
- McLellan A, Kushner H, Metzger D, Peters R. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Blanchard KA, Kahler C, Barbosa KM, McCrady BS, McVeigh KH. Testing mechanisms of action for intensive case management. Addiction. 2008;103:469–477. doi: 10.1111/j.1360-0443.2007.02100.x. [DOI] [PubMed] [Google Scholar]
- Najavits LM, Weiss RD, Shaw ST, Muenz LR. “Seeking Safety”: Outcome of a new cognitive-behavioral psychotherapy for women with posttraumatic stress disorder and substance abuse. Journal of Traumatic Stress. 1998;11:437–456. doi: 10.1023/A:1024496427434. [DOI] [PubMed] [Google Scholar]
- Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: A first step toward developing effective treatments. Alcoholism: Clinical and Experimental Research. 2001;25:210–220. [PubMed] [Google Scholar]
- Schuckit MA, Tipp JE, Bergman M, Reich W, Hesselbrock VM, Smith TL. Comparison of induced and independent major depressive disorders in 2,945 alcoholics. American Journal of Psychiatry. 1997;154:948–957. doi: 10.1176/ajp.154.7.948. [DOI] [PubMed] [Google Scholar]
- Sobell L, Sobell M. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring alcohol consumption: psychosocial and biochemical methods. Totowa, NJ: Humana Press; 1992. [Google Scholar]
- SPSS for Windows. SPSS for Windows, Rel. 15.0.1. Chicago: SPSS Inc; 2006. [Google Scholar]
- Stöffelmayr BE, Mavis BE, Kasim RM. The longitudinal stability of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1994;11:373–378. doi: 10.1016/0740-5472(94)90048-5. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Kolodziej ME, Greenfield SF, Najavits LM, Daley DC, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. American Journal of Psychiatry. 2007;164:100–107. doi: 10.1176/ajp.2007.164.1.100. [DOI] [PubMed] [Google Scholar]