Abstract
Objective
We investigated whether coronary microvascular dysfunction predicts major adverse outcomes during follow-up among women with signs and symptoms of ischemia.
Background
Altered coronary reactivity occurs frequently in women evaluated for suspected ischemia and the endothelium-dependent component is linked with adverse outcomes. Possible links between endothelium-independent microvascular coronary reactivity and adverse outcomes remain uncertain.
Methods
As part of the National Heart, Lung and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE), we investigated relationships between major adverse outcomes and baseline coronary flow reserve (CFR) following intracoronary adenosine in 189 women referred to evaluate suspected ischemia.
Results
At 5.4 (mean) years, we observed significant associations between CFR and major adverse outcomes (death, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for heart failure). An exploratory ROC analysis identified CFR <2.32 as the best discriminating threshold for adverse outcomes (event rate 26.7% and ≥2.32 event rate 12.2%; p = 0.01). Lower CFR was associated with increased risk for major adverse outcomes (HR 1.16, 95% CI 1.04 to 1.30; p = 0.009). This held true among the 152 women without obstructive coronary artery disease (CAD) (HR 1.20, 95% CI 1.05 to 1.38; p = 0.008). CFR significantly improved prediction of adverse outcomes over angiographic CAD severity and other risk conditions.
Conclusions
Among women with suspected ischemia and atherosclerosis risk factors, coronary microvascular reactivity to adenosine significantly improves prediction of major adverse outcomes over angiographic CAD severity and CAD risk factors. These findings suggest coronary microvessels represent novel targets for diagnostic and therapeutic strategies to predict and limit adverse outcomes in women.
Keywords: women, ischemia, adverse outcomes, microcirculation
Introduction
Women with chest discomfort and other findings suggesting myocardial ischemia are diagnostic and therapeutic challenges due, in part, to low likelihood for obstructive coronary artery disease (CAD) and costs of care related to repeated testing, hospitalization, and disability(1). Although knowledge of mechanisms explaining these findings is limited, impaired coronary reactivity (endothelium- and non endothelium-dependent) has been proposed to contribute(2–10). The endothelium-dependent component has been linked to risk factors and proinflammatory processes promoting atherosclerosis(8,9) as well as adverse clinical outcomes(5,7,10). Although the non endothelium-dependent component has received less attention, the concept that patients with risk factors may have evidence for reduced coronary flow reserve is not new(11–17). There is increasing interest in this microvascular response as recently reviewed elsewhere(18), and in particular the response among women(8). For example, hypercholesterolemia abolishes the voltage-dependent K+ channel contribution to adenosine-mediated smooth muscle relaxation, in both endothelium-intact and -denuded coronary arterioles, in a sex-specific manner(19,20). Vascular smooth muscle cells undergo alterations in phenotype in response to physiological and pathophysiological stimuli like hypertension and diabetes, which are highly prevalent in postmenopausal women, as well as estrogen receptor alpha expression(21,22).
Myocardial perfusion alterations during adenosine-induced vasodilation are not infrequent in the absence of significant epicardial CAD(23,24). While there has been long interest in microvascular ischemia, most work has focused on the endothelium-dependent component(25–28) but adenosine-related vascular smooth muscle alterations do not necessarily correlate with dysfunctional endothelium(8,20,29). Thus additional information on adenosine-related coronary microvascular reactivity would facilitate an improved understanding of processes underlying these vascular alterations in women. If these alterations contribute to adverse outcomes they potentially offer a target important for risk stratification and evaluation of preventive treatments among these women, particularly now that coronary microvascular reactivity can be readily assessed non-invasively(30–32).
Accordingly, we investigated the relationship between adenosine-coronary reactivity at baseline and adverse outcomes during follow-up in women referred for coronary angiography.
Methods
The Women's Ischemia Syndrome Evaluation (WISE) is a National Heart, Lung and Blood Institute-sponsored study aimed at improving diagnostic evaluation and understanding of pathological mechanisms of ischemic heart disease in women, and protocol details, including selection criteria, have been previously published(33). Site institutional review boards approved the study and each participant provided written informed consent. Women aged 18–84 years undergoing clinically indicated angiograms were enrolled, underwent a variety of testing, and were followed for clinical outcomes. A subgroup of 189 women from the Universities of Florida and Pittsburgh sites also had evaluation of coronary reactivity to adenosine. Their selection criteria also included informed consent for this additional testing, absence of stenosis warranting coronary revascularization and an appropriate coronary segment for Doppler flow testing.
Baseline evaluation included physical examination and collection of clinical and laboratory data (Table 1). Inflammatory markers were measured in a subgroup of 134 women from blood frozen on site at −70 °C and analyzed at a core lab using validated techniques. Qualitative and quantitative coronary angiographic analyses were done by core lab masked to patient data(34). Any ≥50% diameter stenosis was defined as obstructive CAD, 20–49% as mild CAD, and <20% as no CAD. A CAD severity score was defined as an aggregate of percent stenosis, extent and location of stenosis, and degree of collateral vessels(34).
Table 1.
Baseline characteristics
| Characteristic | All women N=189 | CFR <2.32 N=74 | CFR≥2.32 N=115 | P |
|---|---|---|---|---|
| Age, years | 55 ± 10 | 58 ± 10 | 54 ± 10 | 0.02 |
| Years since last menses | 16 ± 11 | 19 ± 12 | 14 ± 10 | 0.004 |
| White/ Caucasian (%) | 83 | 88 | 80 | 0.16 |
| Body Mass Index (kg/m2) | 31.2 ± 7.4 | 31.2 ± 6.3 | 31.2 ± 8.0 | 0.67 |
| SBP (mmHg) | 136 ± 20 | 139 ± 23 | 134 ± 18 | 0.08 |
| DBP (mmHg) | 77 ± 10 | 77 ± 9 | 76 ± 11 | 0.93 |
| Family history of premature CAD (%) | 69 | 71 | 67 | 0.61 |
| History of: | ||||
| Diabetes (%) | 21 | 26 | 18 | 0.24 |
| Hypertension (%) | 57 | 58 | 56 | 0.79 |
| Dyslipidemia (%) | 50 | 54 | 48 | 0.51 |
| Smoking currently (%) | 19 | 16 | 20 | 0.50 |
| Smoking in past (%) | 37 | 39 | 35 | 0.57 |
| Menopause (%) | 76 | 81 | 72 | 0.18 |
| Blood assays: | ||||
| Total cholesterol (mg/dL) | 185 ± 44 | 188 ± 45 | 183 ± 42 | 0.39 |
| HDL cholesterol (mg/dL) | 52 ± 12 | 53 ± 12 | 52 ± 13 | 0.84 |
| LDL cholesterol (mg/dL) | 107 ± 37 | 111 ± 40 | 104 ± 36 | 0.16 |
| Triglycerides (mg/dL) | 141 ± 141 | 148 ± 118 | 136 ± 155 | 0.72 |
| Plasma glucose (mg/dL) | 105 ± 48 | 108 ± 52 | 102 ± 44 | 0.34 |
| Hemoglobin (g/dL) | 13.0 ± 1.4 | 13.0 ± 1.6 | 13.0 ± 1.3 | 0.35 |
| Serum creatinine (mg/dL) | 0.8 ± 0.5 | 0.8 ± 0.3 | 0.8 ± 0.6 | 0.35 |
| Serum amyloid A (mg/dL) | 1.0 ± 2.3 | 1.1 ± 2.6 | 1.0 ± 2.1 | 0.06 |
| C-reactive protein (mg/L) | 7.8 ± 11.6 | 8.8 ± 13.7 | 7.2 ± 10.2 | 0.22 |
| Interleukin-6 (pg/mL) | 3.7 ± 2.8 | 3.9 ± 3.0 | 3.6 ± 2.6 | 0.72 |
| Medication use, currently: | ||||
| Aspirin (%) | 50 | 57 | 46 | 0.14 |
| Statin (%) | 16 | 19 | 15 | 0.47 |
| ACE-inhibitor (%) | 24 | 27 | 23 | 0.51 |
| Beta-blocker (%) | 29 | 36 | 24 | 0.06 |
| Hormone use, ever: | ||||
| Hormone replacement (%) | 56 | 53 | 58 | 0.53 |
| Oral contraceptives (%) | 60 | 60 | 59 | 0.88 |
| Ejection Fraction (%) | 64.7 ± 9.6 | 64.5 ± 10.9 | 64.9 ± 8.8 | 0.71 |
| Coronary artery disease: | ||||
| None (<20% stenosis) (%) | 51 | 46 | 54 | |
| Mild (20–49% stenosis) (%) | 30 | 28 | 32 | |
| Obstructive (≥50% stenosis) (%) | 19 | 26 | 15 | 0.11 |
| CAD severity score (medians [IQR]) | 5.0(5.0, 9.2) | 7.5(5.0, 11.2) | 5.0(5.0,8.0) | 0.036 |
CFR=coronary flow reserve; SBP=systolic blood pressure; DBP=diastolic blood pressure; HDL=high-density lipoprotein; LDL=low-density lipoprotein; ACE=angiotensin-converting enzyme; CAD=coronary artery disease; IQR=interquartile range.
Data expressed as mean ± SD unless otherwise noted.
Coronary reactivity testing was performed in a stenosis-free area of the left anterior descending coronary artery (n = 138) when possible, with the left circumflex artery as a secondary choice. A Doppler-tipped guidewire (0.014 inch FloWire; JOMED/Cardiometrics, Mountain View, CA) was advanced through the diagnostic catheter. Once a stable velocity signal was obtained baseline recordings were made. Intracoronary bolus injections of 18 μg of adenosine (Adenocard; Fujisawa USA, Deerfield, IL), a predominantly non-endothelium-dependent microvascular dilator, were administered into the left main coronary artery(35). At least three injections were done to assure that a stable average peak coronary flow velocity was obtained after adenosine, with return to baseline flow velocity documented before each bolus. Pulsed-wave Doppler flow spectra were used to calculate time-averaged peak velocity. Recordings were analyzed at a core lab (University of Florida) masked to all other data, and coronary flow reserve was defined as the ratio of average peak velocity after adenosine to average baseline velocity just prior to adenosine. Since this measure correlated closely (r= 0.87, p< 0.001) with volumetric flow(35) it was used to represent coronary flow reserve(CFR).
To access the possible influence of left ventricular (LV) hypertrophy on CFR, 39 of these women without coronary stenosis had quantitative analysis of echocardiograms performed using a standardized protocol within several days of CFR measurements according to American Society of Echocardiography recommendations. These analyses included measurement of LV mass (2D echo) determined by an anatomically validated short axis area length method(36), mass index, and an index of LV concentric remodeling [end diastolic ratio of short axis myocardial to cavity area (MA/CA)]. All echo measurements were done at a core lab masked to patient data.
Adverse Outcomes during Follow-up
During protocol-directed yearly follow-up, records of women reporting an event were reviewed by an events committee and tabulated as death, nonfatal MI, nonfatal stroke, and hospitalization for CHF, angina, and other vascular events. Women sustaining multiple events were counted only once and by the initial event. Those with death, nonfatal MI, nonfatal stroke, or CHF hospitalization were categorized as having major adverse outcomes. Categorization of deaths as cardiovascular (CV) was made only when documentation definitely confirmed that death was due to CV causes.
Statistical Analyses
Values are expressed as means ± standard deviations or percentages as indicated, and t-test or Chi square analysis, where appropriate, was used to evaluate differences among groups. The CAD angiographic severity score was non-normally distributed and was expressed as medians and interquartile ranges with differences among groups evaluated by the Kruskal-Wallis test. To determine the CFR value best predictive of major adverse outcomes (death, MI, stroke, or hospitalization for CHF), we generated a receiver operating characteristic (ROC) curve from the PROC LOGISTICS function in SAS which calculates area under the curve (AUC), indicated by the c-statistic, using the trapezoidal rule. The CFR value corresponding to the point on the curve closest to 100% sensitivity and specificity was matched, first by visual means and then by verification runs of incremental cut-points near this value. The discriminating threshold by ROC analysis was then used to categorize women into low versus high CFR groups. Kaplan-Meier analysis was used to compare time to adverse event by CFR group in all women and in women without obstructive CAD. Multivariate Cox proportional hazards regression was used to examine the role of baseline characteristics including the natural logs of both the CAD severity score and CFR (logCFR ×10) on adverse outcomes. Baseline characteristics (Table 1) were chosen for entry into multivariable Cox models based upon their discrimination between low and high CFR as well as on univariate associations with adverse outcomes of p < 0.20. A combination of forward and backward selection procedures was used to aid in determining the best model of independent predictors. This was followed by forcing potential confounders, including drugs used at baseline and during follow-up, into the models and determining their effect on the relationship of interest. The likelihood ratio test was used to compare the incremental goodness of fit of nested models. All tests were two-sided, and p ≤ 0.05 was considered statistically significant. All analyses were performed using SAS 9.1 software (SAS Institute; Cary, NC).
Results
Baseline Characteristics
Pertinent characteristics of the women are summarized in Table 1. Their mean age was 55 years (standard deviation ±10 years), most were white, about three-quarters were post-menopausal, and more than half were obese (body mass index ≥30), had a history of hypertension or dyslipidemia, had a family history of premature heart disease, or used hormone replacement or oral contraceptive pills. History of diabetes was present in about a fifth. Approximately one-half were currently taking aspirin; about one-quarter, angiotensin-converting enzyme (ACE) inhibitors; less than one-third, beta-blockers; and about one-fifth, statins.
Angiographic CAD, echo LV mass, and CFR
Most (152 or 81%) of the women had either no or <50% obstructive CAD (Table 1) and lower CFR was weakly associated with higher CAD severity score (rs = −0.15, p = 0.04). Comparing groups with obstructive, mild, or no angiographic CAD, the CFRs were 2.3 ± 0.7, 2.5 ± 0.7, and 2.6 ± 0.7, respectively (p = 0.09 for trend). Regression analyses and comparisons of subgroups with normal vs. elevated LV mass, mass index, and MA/CA showed no significant relationships between LV mass variables and CFR (data not shown).
Adverse Outcomes by Risk Factors and CFR
During follow-up (mean 5.4 years), 79 women (42%) had an adverse outcome, and in total there were 138 events including 11 deaths (Table 2). Thirty-four of these 79 women had major adverse outcomes (death, MI, stroke, or hospitalization for CHF). Note that 25 of the women without obstructive CAD had major adverse outcomes.
Table 2.
Index (first) and total adverse events during follow-up
| Events | Number of index (first) events | Total number of events |
|---|---|---|
| Major events | ||
| Death | 8 | 11 |
| Hospitalization for nonfatal event: | ||
| MI | 3 | 7 |
| CHF | 6 | 18 |
| Stroke | 8 | 10 |
| Other events | ||
| PCI | 12 | 23 |
| CABG | 1 | 4 |
| Angina | 36 | 52 |
| Other vascular event | 5 | 13 |
| Total (%)s | 79 (42%) | 138* |
138 total number of events in 79 women.
All analyses summarized below were done with only major adverse outcomes. Substituting definite CV deaths for all-cause deaths produced very similar results.
Among all women in this cohort, those with major adverse events during follow up had at baseline higher SBP (p = 0.01), CRP (p = 0.038), and IL-6 (p = 0.02) levels and CAD severity scores (p = 0.0009) and were more frequently postmenopausal (p = 0.02) compared with those without events. Similar trends were found among the subgroup without obstructive CAD but only postmenopausal status (p = 0.025) and higher CAD severity score (p = 0.0005) reached statistical significance due to smaller sample size with fewer events.
By ROC analysis, a CFR <2.32 provided the best prediction, with a sensitivity of 62% and specificity of 65%, for major adverse outcomes (CFR <2.32 outcomes rate 27.0% and ≥2.32 outcomes rate 12.2%, X2 = 6.73, p = 0.010). The AUC (95% confidence interval) was 0.63 (CI 0.53, 0.73). Similar results were obtained when restricting the analysis to women without obstructive CAD: women with low CFRs experienced significantly more major adverse outcomes (CFR < 2.32 outcome rate 26.6% vs. 9.3%, X2 = 5.84; p = 0.016). Women with low CFR were older (p=0.02) and had a higher CAD severity (p=0.036) versus those with high CFR. There was a significant decline over time in freedom from major events for women with lower (<2.32) CFR compared with those with higher CFR (p = 0.003) (Figure 1), which remained consistent adjusting for risk factors (SBP, CAD severity, age, diabetes, and smoking). The Cox PH-adjusted time-to-event curves are similar to the unadjusted KM curves shown in Figure 1, and the p values remain significant.
Figure 1. Coronary flow reserve (CFR) and event-free survival.
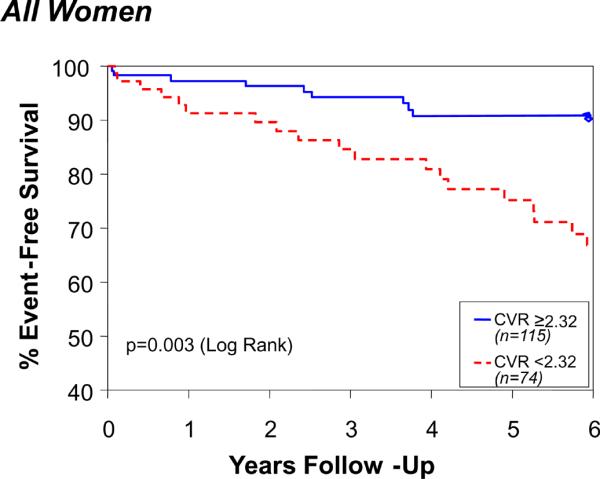
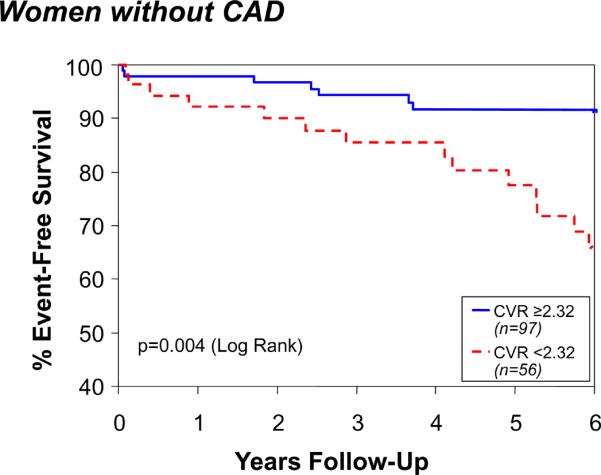
Coronary flow reserve (CFR) and event-free survival among all women (Top) and those without CAD (Bottom). Data represent unadjusted Kaplan-Meier curves for absence of death, nonfatal MI, nonfatal stroke, or hospitalization for CHF during follow-up.
When used as a continuous variable, low CFR also significantly predicted increased risk for major adverse outcomes (Table 3). For each 0.1 unit decrease in logCFR the risk for major adverse outcomes increased by 20% among women without obstructive CAD.
Table 3.
Decreasing LogCFR and risk for adverse outcomes (unadjusted Cox regression analyses)
| All women | |||
|---|---|---|---|
| Outcome | Hazard Ratio | 95% CI | p |
| Major adverse outcome (death, nonfatal MI, nonfatal stroke, or hospitalization for CHF) | 1.16 | 1.04 – 1.30 | 0.009 |
| CV death, nonfatal MI, nonfatal stroke, or hospitalization for CHF | 1.15 | 1.02 – 1.30 | 0.019 |
| CV death, nonfatal MI, or hospitalization for CHF | 1.18 | 1.03 – 1.36 | 0.018 |
| Women without obstructive CAD | |||
|---|---|---|---|
| Outcome | Hazard Ratio | 95% CI | p |
| Major adverse outcome (death, nonfatal MI, nonfatal stroke, or hospitalization for CHF) | 1.20 | 1.05 – 1.38 | 0.008 |
| CV death, nonfatal MI, nonfatal stroke, or hospitalization for CHF | 1.19 | 1.03 – 1.37 | 0.020 |
| CV death, nonfatal MI, or hospitalization for CHF | 1.23 | 1.03 – 1.47 | 0.021 |
MI=myocardial infarction; CHF=congestive heart failure; CV=cardiovascular; CI=confidence interval.
Multivariate Cox regression modeling (Table 4) identified only logCFR (p = 0.043), log CAD severity score (p = 0.058), and systolic blood pressure (p = 0.012) as independent predictors of major adverse outcome. When multiple CAD risk conditions (e.g., age, history of diabetes, and smoking) were forced into the model, potentially overfitting the model, CFR remained a significant predictor (p = 0.038) while the effect of log CAD severity was attenuated. No other risk factors contributed (data not shown). When forcing any statin, ACE inhibitor, and beta-blocker use into the models, use of these drugs was neither a significant predictor of adverse outcome nor did use influence the relationship between CFR and adverse outcome. In the combined model, the likelihood ratio test determined that adding CFR significantly improved prediction of major adverse outcomes over the other variables (X2 = 4.37; p = 0.036).
Table 4.
Multivariate modeling of major events (Cox regression analysis)
| Predictor | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | p | HR (95% CI) | p | HR (95% CI) | p | |
| Log CFR | 1.15 (1.02–1.30) | 0.018 | 1.13 (1.004–1.27) | 0.043 | 1.14 (1.01–1.29) | 0.038 |
| SBP | 1.02 (1.005–1.04) | 0.011 | 1.02 (1.004–1.04) | 0.012 | 1.02 (1.001–1.04) | 0.035 |
| Log CAD Severity | - | 1.68 (0.98–2.88) | 0.058 | 1.61 (0.92–2.81) | 0.10 | |
| Age | - | - | - | - | 1.00 (0.96–1.04) | 0.90 |
| Hx Diabetes | - | - | - | - | 1.44 (0.65–3.20) | 0.37 |
| Ever Smoked | - | - | - | - | 1.22 (0.60–2.46) | 0.58 |
CFR=coronary flow reserve; CAD=coronary artery disease; SBP=systolic blood pressure; Hx=history of; HR=hazard ratio; CI=confidence interval.
Notes: When interpreting these tables, the hazard ratios reflect the % change in events for every 0.1 unit increment in the log CFR. Adjusting for one covariate at a time among other variables in Table 1 did not substantially change the relationship between CFR and major adverse outcome.
Discussion
Many women presenting with ischemic-type symptoms and signs do not have obstructive CAD but have impaired coronary reactivity to adenosine, which has the potential to limit myocardial flow, but an association with adverse outcome is unclear. Most reports did not examine endothelium-independent microvascular responses, few patients had major serious events (most were revascularization), relatively few women were included, and/or gender specific data were not reported.
Nitemberg et al published CV outcome in hypertensive and diabetes patients without CAD, using cold-pressor testing with epicardial coronary diameter measurements, which is related both to endothelial and non endothelial-dependent mechanisms, but no gender stratification or flow responses were reported(3). Halcox et al found a significant association between acetylcholine responses and outcomes(2). Although trends were noted for nitroprusside and adenosine they concluded in this underpowered study that endothelium-independent responses were not predictive of outcome(2). Al Suwaidi et al reported the prognostic value of the response to adenosine and nitroprusside but simply stated that CFR response to adenosine was significantly lower in those with endothelial dysfunction, implying that endothelial-dependent and independent mechanisms show similar responses(6).
Other studies indicate that positron emission tomography (PET) measures of absolute myocardial blood flow (MBF) and CFR or myocardial perfusion reserve(1,2,5,7,10,14) may be abnormal in individuals with risk factors without apparent CAD. Overall these reports document reduced coronary reactivity in individuals with a greater coronary risk factor burden. Except for a report(5) suggesting impaired MBF responses to cold-pressor testing were associated with increased risk of events, the prognostic value of traditional clinical risk assessment versus myocardial perfusion reserve by PET cannot be compared because of lack of follow-up data. Additionally, other studies(37) have demonstrated that maximum MBF and CFR may be impaired in myocardial territories supplied by arteries that do not appear obstructed in patients with obstructive CAD elsewhere. Finally, reduced MBF reserve in patients with hypertrophic(9) or dilated cardiomyopathy(29) has predictive value for prognosis. Thus the overall topic of coronary microvascular dysfunction and its clinical implications has increasing interest(11–13,15–18,38–43).
A better understanding of adverse outcomes associated with dysfunctional microvessels could help to clarify the pathophysiology of ischemic heart disease in women and perhaps identify new targets for both diagnostic testing and therapeutic intervention.
Our findings indicate that endothelium-independent CFR is a predictor of major adverse outcomes in the women studied. The link between CFR and major adverse outcomes remained regardless of presence or absence of obstructive CAD or multiple risk conditions. The low but significant association of this component of coronary reactivity with CAD severity is intriguing, as atherosclerotic plaque is usually localized to conduit arteries and those selected for flow measurement did not have flow-limiting stenoses. Furthermore, among the 152 women without any obstructive stenoses, the link with adverse outcomes remained significant. Although adenosine receptors are present in both endothelial and smooth muscle cells, it is unlikely that dilation of conduit arteries, through either an endothelial or smooth muscle mechanism, could explain our findings. Thus the location of the defect exposed by adenosine in these women is most likely at the microvascular level. This may represent an early manifestation of vascular defects underlying ischemic heart disease in these women, with the potential to contribute to subsequent major adverse outcomes even in the absence of conduit vessel obstruction. Indeed, women in the WISE cohort, including those without obstructive CAD, had a surprisingly high risk for major adverse events during follow-up(44,45). A possible conclusion from this analysis is that non-obstructive CAD (≤49% diameter stenosis) in women is perhaps of greater importance than can be surmised merely from speculation about conduit artery hemodynamic impairment (or lack thereof). Such findings appear to be associated with evidence of microvascular disease and a poorer outcome. Presence of such findings in women might warrant CFR measurements to refine estimates of prognosis. Alternatively, a lower percent narrowing threshold (or CAD score) may be identified in such women that might be useful for prognostic purposes (even if not useful for intervention purposes).
It would be highly desirable to have a simple reliable physiologic measure to identify women at highest risk for adverse outcomes, and this measure could be altered coronary microvascular reactivity. If proven so in other studies, this could lead to more targeted treatment and the reactivity measurement could be non-invasively performed and followed to assess response to treatment and prevention strategies.
Other evidence implicates the coronary microcirculation to explain some findings in ischemic heart disease that are observed in women(46). In the absence of conduit vessel obstruction this includes myocardial metabolic, electrocardiographic, and scintigraphic evidence for ischemia(47); histologic evidence for small vessel disease(48); the predictive value of brain natriuretic peptide and C-reactive protein for adverse outcomes(49); and findings of microvascular obstruction in women dying with acute coronary syndromes (ACS)(50). Even more important is the question, could microvascular dysfunction deteriorate into, or perhaps promote macrovascular disease?
Study Limitations
Although this represents the largest group of women with microvascular reactivity and follow-up data reported, we evaluated a relatively select cohort with ischemic-type symptoms and multiple risk conditions prompting referral for angiography. This indication bias limits generalization of results. Unknown factors, including individual variability in dose responses or in vascular smooth muscle effects of similar CAD risk conditions, could potentially affect CFR. Although adenosine-induced CFR increases are mediated largely via smooth muscle relaxation, endothelium-dependent mechanisms could contribute(51). It is likely that the 18 μg intracoronary adenosine dose may not have achieved near maximal hyperemia in every patient. Similar adenosine doses provide near maximal increase in flow in 90–92% of cases(52), and larger doses used for fractional flow reserve measurement to assess coronary stenosis severity may provide different results. Left ventricular hypertrophy (LVH) may influence coronary microvascular reactivity; however, quantitative echocardiographic analysis from a subgroup of these women without CAD suggested that low CFR could not be explained by LVH. We used only blood flow velocity measurements, but we have previously shown in an analysis from WISE that this measure agrees closely with volumetric flow reserve(35). Finally, despite the relatively large sample of women in this cohort, the low number of major events limits statistical power and creates the risk of over-fitting the models when adding covariates. However, despite this potential problem, the addition of such covariates in no case affected the relationship between CFR and adverse outcomes.
Conclusions
In women undergoing coronary angiography to further evaluate suspected ischemia, a limited coronary microvascular response to adenosine is associated with increased risk for major adverse outcomes even in the absence of significant obstructive CAD. This finding supports the need for more investigation of altered coronary smooth muscle reactivity and the smaller vessels in women with suspected ischemia. Long-term follow-up of new cohorts of women should help to determine if coronary microvascular dysfunction and its link with adverse outcomes can be confirmed and modified.
CONDENSED ABSTRACT.
As part of the National Heart, Lung and Blood Institute-sponsored Women's Ischemia Syndrome Evaluation (WISE), we investigated relationships between coronary flow reserve following adenosine at entry and adverse outcomes over 5.4 years follow-up in 189 women referred to evaluate suspected ischemia. Among these women with suspected ischemia and atherosclerosis risk factors, coronary microvascular reactivity to adenosine significantly improves prediction of adverse outcomes over angiographic CAD severity and CAD risk factors. These findings suggest that coronary microvessels represent a novel target for both diagnostic and therapeutic strategies to predict and limit adverse outcomes in women.
Acknowledgments
Grant Support: This work was supported by contracts from the National Heart, Lung and Blood Institutes, nos. N01-HV-68161, N01-HV-68162, N01-HV-68163, N01-HV-68164, grants U0164829, U01 HL649141, U01 HL649241, 1R01 HL090957-01A1, T32HL69751, GCRC grant MO1-RR00425 from the National Center for Research Resources and grants from the Gustavus and Louis Pfeiffer Research Foundation, Danville, NJ, The Women's Guild of Cedars-Sinai Medical Center, Los Angeles, CA, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, PA, and QMED, Inc., Laurence Harbor, NJ, the Edythe L. Broad Women's Heart Research Fellowship, Cedars-Sinai Medical Center, Los Angeles, California, and the Barbra Streisand Women's Cardiovascular Research and Education Program, Cedars-Sinai Medical Center, Los Angeles.
Abbreviations
- ACS
acute coronary syndromes
- CV
cardiovascular
- CI
confidence intervals
- CAD
coronary artery disease
- CFR
coronary flow reserve
- CHF
congestive heart failure
- HR
hazard ratios
- LV
left ventricular
- MI
myocardial infarction
- ROC
receiver operating characteristic
- WISE
Women's Ischemia Syndrome Evaluation
Footnotes
No authors have a conflict of interest to disclose.
References
- 1.Shaw LJ, Merz CN, Pepine CJ, et al. The economic burden of angina in women with suspected ischemic heart disease: results from the National Institutes of Health--National Heart, Lung, and Blood Institute--sponsored Women's Ischemia Syndrome Evaluation. Circulation. 2006;114:894–904. doi: 10.1161/CIRCULATIONAHA.105.609990. [DOI] [PubMed] [Google Scholar]
- 2.Halcox JP, Schenke WH, Zalos G, et al. Prognostic value of coronary vascular endothelial dysfunction. Circulation. 2002;106:653–8. doi: 10.1161/01.cir.0000025404.78001.d8. [DOI] [PubMed] [Google Scholar]
- 3.Nitenberg A, Pham I, Antony I, Valensi P, Attali JR, Chemla D. Cardiovascular outcome of patients with abnormal coronary vasomotion and normal coronary arteriography is worse in type 2 diabetes mellitus than in arterial hypertension: a 10 year follow-up study. Atherosclerosis. 2005;183:113–20. doi: 10.1016/j.atherosclerosis.2005.02.030. [DOI] [PubMed] [Google Scholar]
- 4.Schachinger V, Britten MB, Zeiher AM. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation. 2000;101:1899–906. doi: 10.1161/01.cir.101.16.1899. [DOI] [PubMed] [Google Scholar]
- 5.Schindler TH, Nitzsche EU, Schelbert HR, et al. Positron emission tomography-measured abnormal responses of myocardial blood flow to sympathetic stimulation are associated with the risk of developing cardiovascular events. J Am Coll Cardiol. 2005;45:1505–12. doi: 10.1016/j.jacc.2005.01.040. [DOI] [PubMed] [Google Scholar]
- 6.Al Suwaidi JA, Hamasaki S, Higano ST, Nishimura RA, Holmes DR, Jr., Lerman A. Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation. 2000;101:948–54. doi: 10.1161/01.cir.101.9.948. [DOI] [PubMed] [Google Scholar]
- 7.von Mering GO, Arant CB, Wessel TR, et al. Abnormal coronary vasomotion as a prognostic indicator of cardiovascular events in women: results from the National Heart, Lung, and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE) Circulation. 2004;109:722–5. doi: 10.1161/01.CIR.0000115525.92645.16. [DOI] [PubMed] [Google Scholar]
- 8.Bottcher M, Botker HE, Sonne H, Nielsen TT, Czernin J. Endothelium-dependent and -independent perfusion reserve and the effect of L-arginine on myocardial perfusion in patients with syndrome X. Circulation. 1999;99:1795–801. doi: 10.1161/01.cir.99.14.1795. [DOI] [PubMed] [Google Scholar]
- 9.Chan NN, Colhoun HM, Vallance P. Cardiovascular risk factors as determinants of endothelium-dependent and endothelium-independent vascular reactivity in the general population. J Am Coll Cardiol. 2001;38:1814–20. doi: 10.1016/s0735-1097(01)01669-2. [DOI] [PubMed] [Google Scholar]
- 10.Schindler TH, Hornig B, Buser PT, et al. Prognostic value of abnormal vasoreactivity of epicardial coronary arteries to sympathetic stimulation in patients with normal coronary angiograms. Arterioscler Thromb Vasc Biol. 2003;23:495–501. doi: 10.1161/01.ATV.0000057571.03012.F4. [DOI] [PubMed] [Google Scholar]
- 11.Di Carli MF, Janisse J, Grunberger G, Ager J. Role of chronic hyperglycemia in the pathogenesis of coronary microvascular dysfunction in diabetes. J Am Coll Cardiol. 2003;41:1387–93. doi: 10.1016/s0735-1097(03)00166-9. [DOI] [PubMed] [Google Scholar]
- 12.Pitkanen OP, Nuutila P, Raitakari OT, et al. Coronary flow reserve is reduced in young men with IDDM. Diabetes. 1998;47:248–54. doi: 10.2337/diab.47.2.248. [DOI] [PubMed] [Google Scholar]
- 13.Pitkanen OP, Raitakari OT, Niinikoski H, et al. Coronary flow reserve is impaired in young men with familial hypercholesterolemia. J Am Coll Cardiol. 1996;28:1705–11. doi: 10.1016/S0735-1097(96)00376-2. [DOI] [PubMed] [Google Scholar]
- 14.Schelbert HR. Coronary circulatory function abnormalities in insulin resistance: insights from positron emission tomography. J Am Coll Cardiol. 2009;53:S3–8. doi: 10.1016/j.jacc.2008.09.053. [DOI] [PubMed] [Google Scholar]
- 15.Yokoyama I, Momomura S, Ohtake T, et al. Reduced myocardial flow reserve in non-insulin-dependent diabetes mellitus. J Am Coll Cardiol. 1997;30:1472–7. doi: 10.1016/s0735-1097(97)00327-6. [DOI] [PubMed] [Google Scholar]
- 16.Yokoyama I, Murakami T, Ohtake T, et al. Reduced coronary flow reserve in familial hypercholesterolemia. J Nucl Med. 1996;37:1937–42. [PubMed] [Google Scholar]
- 17.Yokoyama I, Ohtake T, Momomura S, Nishikawa J, Sasaki Y, Omata M. Reduced coronary flow reserve in hypercholesterolemic patients without overt coronary stenosis. Circulation. 1996;94:3232–8. doi: 10.1161/01.cir.94.12.3232. [DOI] [PubMed] [Google Scholar]
- 18.Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007;356:830–40. doi: 10.1056/NEJMra061889. [DOI] [PubMed] [Google Scholar]
- 19.Heaps CL, Bowles DK. Gender-specific K(+)-channel contribution to adenosine-induced relaxation in coronary arterioles. J Appl Physiol. 2002;92:550–8. doi: 10.1152/japplphysiol.00566.2001. [DOI] [PubMed] [Google Scholar]
- 20.Heaps CL, Tharp DL, Bowles DK. Hypercholesterolemia abolishes voltage-dependent K+ channel contribution to adenosine-mediated relaxation in porcine coronary arterioles. Am J Physiol Heart Circ Physiol. 2005;288:H568–76. doi: 10.1152/ajpheart.00157.2004. [DOI] [PubMed] [Google Scholar]
- 21.Owens GK, Kumar MS, Wamhoff BR. Molecular regulation of vascular smooth muscle cell differentiation in development and disease. Physiol Rev. 2004;84:767–801. doi: 10.1152/physrev.00041.2003. [DOI] [PubMed] [Google Scholar]
- 22.Pepine CJ, Nichols WW, Pauly DF. Estrogen and different aspects of vascular disease in women and men. Circ Res. 2006;99:459–61. doi: 10.1161/01.RES.0000241056.84659.59. [DOI] [PubMed] [Google Scholar]
- 23.Verna E, Ceriani L, Giovanella L, Binaghi G, Garancini S. "False-positive" myocardial perfusion scintigraphy findings in patients with angiographically normal coronary arteries: insights from intravascular sonography studies. J Nucl Med. 2000;41:1935–40. [PubMed] [Google Scholar]
- 24.Wieneke H, Zander C, Eising EG, Haude M, Bockisch A, Erbel R. Non-invasive characterization of cardiac microvascular disease by nuclear medicine using single-photon emission tomography. Herz. 1999;24:515–21. doi: 10.1007/BF03044222. [DOI] [PubMed] [Google Scholar]
- 25.Cannon RO., 3rd Microvascular angina and the continuing dilemma of chest pain with normal coronary angiograms. J Am Coll Cardiol. 2009;54:877–85. doi: 10.1016/j.jacc.2009.03.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mohri M, Koyanagi M, Egashira K, et al. Angina pectoris caused by coronary microvascular spasm. Lancet. 1998;351:1165–9. doi: 10.1016/S0140-6736(97)07329-7. [DOI] [PubMed] [Google Scholar]
- 27.Vita JA, Treasure CB, Nabel EG, et al. Coronary vasomotor response to acetylcholine relates to risk factors for coronary artery disease. Circulation. 1990;81:491–7. doi: 10.1161/01.cir.81.2.491. [DOI] [PubMed] [Google Scholar]
- 28.Zeiher AM, Drexler H, Saurbier B, Just H. Endothelium-mediated coronary blood flow modulation in humans. Effects of age, atherosclerosis, hypercholesterolemia, and hypertension. J Clin Invest. 1993;92:652–62. doi: 10.1172/JCI116634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bottcher M, Madsen MM, Refsgaard J, et al. Peripheral flow response to transient arterial forearm occlusion does not reflect myocardial perfusion reserve. Circulation. 2001;103:1109–14. doi: 10.1161/01.cir.103.8.1109. [DOI] [PubMed] [Google Scholar]
- 30.Lanza GA, Buffon A, Sestito A, et al. Relation between stress-induced myocardial perfusion defects on cardiovascular magnetic resonance and coronary microvascular dysfunction in patients with cardiac syndrome X. J Am Coll Cardiol. 2008;51:466–72. doi: 10.1016/j.jacc.2007.08.060. [DOI] [PubMed] [Google Scholar]
- 31.Pennell DJ. Perfusion abnormality, normal coronaries, and chest pain. J Am Coll Cardiol. 2008;51:473–5. doi: 10.1016/j.jacc.2007.09.049. [DOI] [PubMed] [Google Scholar]
- 32.Tona F, Caforio AL, Montisci R, et al. Coronary flow velocity pattern and coronary flow reserve by contrast-enhanced transthoracic echocardiography predict long-term outcome in heart transplantation. Circulation. 2006;114:I49–55. doi: 10.1161/CIRCULATIONAHA.105.001321. [DOI] [PubMed] [Google Scholar]
- 33.Merz CN, Kelsey SF, Pepine CJ, et al. The Women's Ischemia Syndrome Evaluation (WISE) study: protocol design, methodology and feasibility report. J Am Coll Cardiol. 1999;33:1453–61. doi: 10.1016/s0735-1097(99)00082-0. [DOI] [PubMed] [Google Scholar]
- 34.Sharaf BL, Pepine CJ, Kerensky RA, et al. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation [WISE] Study Angiographic Core Laboratory) Am J Cardiol. 2001;87:937–41. A3. doi: 10.1016/s0002-9149(01)01424-2. [DOI] [PubMed] [Google Scholar]
- 35.Reis SE, Holubkov R, Lee JS, et al. Coronary flow velocity response to adenosine characterizes coronary microvascular function in women with chest pain and no obstructive coronary disease. Results from the pilot phase of the Women's Ischemia Syndrome Evaluation (WISE) study. J Am Coll Cardiol. 1999;33:1469–75. doi: 10.1016/s0735-1097(99)00072-8. [DOI] [PubMed] [Google Scholar]
- 36.Reichek N, Helak J, Plappert T, Sutton MS, Weber KT. Anatomic validation of left ventricular mass estimates from clinical two-dimensional echocardiography: initial results. Circulation. 1983;67:348–52. doi: 10.1161/01.cir.67.2.348. [DOI] [PubMed] [Google Scholar]
- 37.Chauhan A, Mullins PA, Taylor G, Petch MC, Schofield PM. Both endothelium-dependent and endothelium-independent function is impaired in patients with angina pectoris and normal coronary angiograms. Eur Heart J. 1997;18:60–8. doi: 10.1093/oxfordjournals.eurheartj.a015119. [DOI] [PubMed] [Google Scholar]
- 38.Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG. Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med. 2003;349:1027–35. doi: 10.1056/NEJMoa025050. [DOI] [PubMed] [Google Scholar]
- 39.Neglia D, Michelassi C, Trivieri MG, et al. Prognostic role of myocardial blood flow impairment in idiopathic left ventricular dysfunction. Circulation. 2002;105:186–93. doi: 10.1161/hc0202.102119. [DOI] [PubMed] [Google Scholar]
- 40.Sambuceti G, Parodi O, Marzullo P, et al. Regional myocardial blood flow in stable angina pectoris associated with isolated significant narrowing of either the left anterior descending or left circumflex coronary artery. Am J Cardiol. 1993;72:990–4. doi: 10.1016/0002-9149(93)90850-c. [DOI] [PubMed] [Google Scholar]
- 41.Tsagalou EP, Anastasiou-Nana M, Agapitos E, et al. Depressed coronary flow reserve is associated with decreased myocardial capillary density in patients with heart failure due to idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 2008;52:1391–8. doi: 10.1016/j.jacc.2008.05.064. [DOI] [PubMed] [Google Scholar]
- 42.Uren NG, Marraccini P, Gistri R, de Silva R, Camici PG. Altered coronary vasodilator reserve and metabolism in myocardium subtended by normal arteries in patients with coronary artery disease. J Am Coll Cardiol. 1993;22:650–8. doi: 10.1016/0735-1097(93)90172-w. [DOI] [PubMed] [Google Scholar]
- 43.Yokoyama I, Ohtake T, Momomura S, et al. Hyperglycemia rather than insulin resistance is related to reduced coronary flow reserve in NIDDM. Diabetes. 1998;47:119–24. doi: 10.2337/diab.47.1.119. [DOI] [PubMed] [Google Scholar]
- 44.Johnson BD, Shaw LJ, Pepine CJ, et al. Persistent chest pain predicts cardiovascular events in women without obstructive coronary artery disease: results from the NIHNHLBI-sponsored Women's Ischaemia Syndrome Evaluation (WISE) study. Eur Heart J. 2006;27:1408–15. doi: 10.1093/eurheartj/ehl040. [DOI] [PubMed] [Google Scholar]
- 45.Gulati M, Cooper-DeHoff RM, McClure C, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: a report from the Women's Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch Intern Med. 2009;169:843–50. doi: 10.1001/archinternmed.2009.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pepine CJ, Kerensky RA, Lambert CR, et al. Some thoughts on the vasculopathy of women with ischemic heart disease. J Am Coll Cardiol. 2006;47:S30–5. doi: 10.1016/j.jacc.2005.09.023. [DOI] [PubMed] [Google Scholar]
- 47.Buffon A, Rigattieri S, Santini SA, et al. Myocardial ischemia-reperfusion damage after pacing-induced tachycardia in patients with cardiac syndrome X. Am J Physiol Heart Circ Physiol. 2000;279:H2627–33. doi: 10.1152/ajpheart.2000.279.6.H2627. [DOI] [PubMed] [Google Scholar]
- 48.Mosseri M, Yarom R, Gotsman MS, Hasin Y. Histologic evidence for small-vessel coronary artery disease in patients with angina pectoris and patent large coronary arteries. Circulation. 1986;74:964–72. doi: 10.1161/01.cir.74.5.964. [DOI] [PubMed] [Google Scholar]
- 49.Wiviott SD, Cannon CP, Morrow DA, et al. Differential expression of cardiac biomarkers by gender in patients with unstable angina/non-ST-elevation myocardial infarction: a TACTICS-TIMI 18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy-Thrombolysis In Myocardial Infarction 18) substudy. Circulation. 2004;109:580–6. doi: 10.1161/01.CIR.0000109491.66226.26. [DOI] [PubMed] [Google Scholar]
- 50.Burke AP, Farb A, Malcom GT, Liang Y, Smialek J, Virmani R. Effect of risk factors on the mechanism of acute thrombosis and sudden coronary death in women. Circulation. 1998;97:2110–6. doi: 10.1161/01.cir.97.21.2110. [DOI] [PubMed] [Google Scholar]
- 51.Buus NH, Bottcher M, Hermansen F, Sander M, Nielsen TT, Mulvany MJ. Influence of nitric oxide synthase and adrenergic inhibition on adenosine-induced myocardial hyperemia. Circulation. 2001;104:2305–10. doi: 10.1161/hc4401.098293. [DOI] [PubMed] [Google Scholar]
- 52.Jeremias A, Whitbourn RJ, Filardo SD, et al. Adequacy of intracoronary versus intravenous adenosine-induced maximal coronary hyperemia for fractional flow reserve measurements. Am Heart J. 2000;140:651–7. doi: 10.1067/mhj.2000.109920. [DOI] [PubMed] [Google Scholar]


