Abstract
Primary tumours and tumorous lesions of the clavicle are very rare, and little literature is available regarding their characteristics and outcome. We studied the clinical, radiological, and histopathological characteristics, and outcome of management of patients with primary tumours of the clavicle presenting to us from 1996–2005. Twelve cases of primary tumours of the clavicle presented during the above period. Seven patients were treated with partial or complete claviculectomy, and no reconstruction was done. These seven patients were evaluated for functional results with AMSTS scoring. Eight patients out of twelve had a primary malignant bone tumour, four of these being Ewing’s sarcoma. No particular predilection of location of the tumour within the clavicle was seen. Functional and oncological results of claviculectomy were good. The distribution of types of tumours in the clavicle is quite different from long-bone tumours. No reconstruction is required following partial or total claviculectomy.
Résumé
Les tumeurs primaires et les lésions tumorales de la clavicule sont très rares et peu de publications existent sur ce sujet. Nous avons étudié sur le plan clinique, radiologique et histopathologique l’évolution de patients présentant une telle tumeur sur une période s’étalant de 1996 à 2005. 12 cas de tumeurs primitives de la clavicule ont été recensés sur cette période. 7 patients ont été traités par une résection partielle ou complète de la clavicule sans reconstruction. 7 patients ont été évalués sur le plan fonctionnel par le score AMSTS. 8 patients sur 12 présentaient une tumeur maligne primitive des os et 4 d’entre elles étaient un sarcome d’Ewing. Nous n’avons pas mis en évidence de localisation particulière dans ces tumeurs au niveau de la clavicule. Les résultats fonctionnels et étiologiques de la claviculectomie restent satisfaisants. Les tumeurs sont différentes de celles des os longs, il n’est pas utile de reconstruire la clavicule après une résection partielle ou totale de celle-ci.
Introduction
The clavicle is a rare site for bone tumours [2, 7]. Orthopaedic oncologists consequently have limited experience in the diagnosis and management of tumours and tumorous conditions of the clavicle. The clavicle shares its oncological characteristics with flat bones and not with other long bones. Clavicular tumours are important, however, because the majority are malignant [2], and the diagnosis may be delayed because of a low level of suspicion. The clavicle is an unusual bone in more ways than one [3]. It is the only long bone whose anatomical position is in the horizontal axis. It lacks a definite medullary cavity and ossifies by membranous ossification. It has two primary centres of ossification and only one secondary centre of ossification, the sternal end. It is the first bone to ossify in the embryo (fifth month). This bone is subcutaneous throughout its length, and it is occasionally pierced by the middle supraclavicular nerve. Fortunately, the clavicle is a bone that can be resected without causing significant disability [20].
Prompted by the rarity of tumours in this bone and the paucity of literature on the management of tumours in this bone, we studied the presentation, distribution, radiological, and histopathological aspects of 12 cases with primary tumours and tumorous conditions involving the clavicle.
Material and methods
All patients presenting to us with a tumour or tumorous condition of the clavicle from 1996–2005 were included in the study. Patients with osteomyelits (one pyogenic, two tubercular), radiation-induced osteosarcoma (one patient), and metastatic carcinoma (one patient) were excluded from the study. The patients were studied for the various parameters including clinicoradiological characteristics, histopathological diagnosis and outcome of treatment (surgical or nonsurgical). Out of a total of 12 patients, 6 were males and 6 females. Age of the patients ranged from 6–62 years (mean 26 years). The majority of the patients presented with swelling with or without pain, while one patient (patient 12) presented with pain and stiffness of shoulder. None of the patients showed neurovascular deficit, while restriction of shoulder range of motion was present in three patients (patients 2, 11 and 12).
All patients were initially investigated with plain radiographs; an MRI and/or CT scan was obtained in nine cases; and CT of chest was obtained in all cases with malignant lesions. A bone scan was done in cases 9, 10 and 12. None of the lesions showed involvement or encasement of neurovascular structures. All patients were subjected to open incisional biopsy except those with a known diagnosis (cases 7, 9 and 12).
Claviculectomy was performed in seven patients (four partial and three complete) with a horizontal incision over the subcutaneous surface of the clavicle, including the biopsy incision in the specimen. The resection margins were wide in all cases except case 12. None of the patients developed neurovascular deficit following surgery. On follow-up, all patients were asked about any limitation in the activities of daily living and examined for range of motion of shoulder or any neurovascular deficit. All patients with malignant lesions were subjected to monthly radiographs of the extremity and chest radiographs at intervals of every 3 months, and a CT scan of the chest was obtained in those with respiratory symptoms or a suspected lesion on chest X-ray.
Nonoperative treatment was chosen for patients in whom the clavicle tumour was part of a metastatic/multifocal disease or those with a limited life expectancy (cases 3, 4, 7, 9, 12).
Results
The results are summarised in Table 1.
Table 1.
Characteristics and outcome of patients
| Patient no. | Age/sex | Radiological characteristics | Diagnosis | Location | Treatment | Follow-up |
|---|---|---|---|---|---|---|
| 1 | 15/F | Permeative, large soft tissue mass | Ewing’s sarcoma | Mid 1/3rd | Complete claviculectomy + chemo + lobulectomy | DWD |
| 2 | 17/F | Permeative, soft tissue mass | Ewing’s sarcoma | Mid 1/3rd | Complete claviculectomy + chemo | AWOD |
| 3 | 22/F | Permeative, large soft tissue mass | Ewing’s sarcoma | Global | Chemo | DWD |
| 4 | 12/M | Permeative, large soft tissue mass | Ewing’s sarcoma | Global | Chemo | DWD |
| 5 | 15/F | Geographical with sclerotic margin | ABC | Acromial | Partial claviculectomy | AWOD |
| 6 | 12/M | Spherical bony outgrowth, no soft tissue mass, no intraosseous extension | Periosteal desmoid | Mid 1/3rd | Partial claviculectomy | AWOD |
| 7 | 6/M | Geographical without sclerotic margin | Eosinophilic granuloma | Acromial | Chemo | AWOD |
| 8 | 18/F | Geographical with sclerotic margin | ABC | Sternal | Partial claviculectomy | AWOD |
| 9 | 60/F | Geographical with ill-defined margin | Multiple myeloma | Acromial | Chemo | DWD |
| 10 | 28/M | Permeative with large soft tissue mass | Plasmacytoma | Sternal | Partial claviculectomy + chemo | AWOD |
| 11 | 45/M | Huge soft tissue mass, permeative lesion | Chondrosarcoma | Global | Palliative claviculectomy | LFU |
| 12 | 62/M | Geographical with ill-defined margin | Multiple myeloma | Acromial | Chemo | AWOD |
AWOD Alive without disease, DWD died with disease, LFU lost to follow-up
The average follow-up was 3.3 years (range 6 months to 10 years). The patients treated with claviculectomy were assessed for functioning and acceptability of the involved limb [4]. The average score after claviculectomy was 70.5% of expected normal function, and all the patients were satisfied with the outcome. None of the patients treated with claviculectomy complained of any functional deficit, and all had full range of motion at the involved shoulder. None of the patients had any neurological deficit.
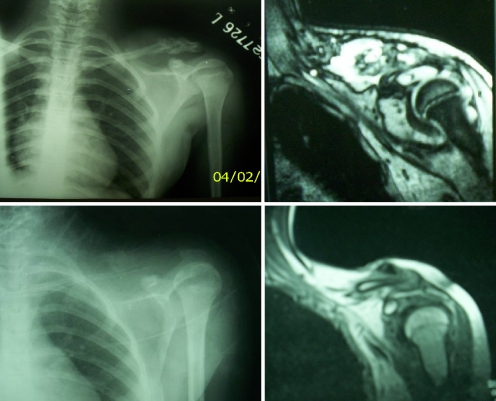
One-third of the patients had Ewing’s sarcoma, including three females and one male. Case 1 underwent complete claviculectomy with neoadjuvant chemotherapy. The patient developed pulmonary metastasis 8 months after claviculectomy and was subjected to lobectomy. The patient died of recurrent pulmonary metastasis 2 years after claviculectomy. Case 2 was subjected to complete claviculectomy and neoadjuvant chemotherapy with vincristine, cyclophosphamide, and doxorubicin. She was free of recurrence and metastasis at final follow-up of 10 years, had full range of motion, and could perform all the activities of daily living (Fig. 1). Cases 3 and 4 both presented with widespread metastatic disease and were both treated by chemotherapy alone. Both the patients died of metastatic disease, at 6 and 12 months after presentation, respectively.
Fig. 1.
Pre- and postoperative radiographs and MRI of 17-year-old female patient with Ewing’s sarcoma involving left clavicle. Patient remains disease-free 10 years postoperatively
Cases 5 and 8 had aneurismal bone cysts in the right and left clavicles, respectively. The patients were treated with partial claviculectomy and were disease-free at final follow-up of 4.5 and 2 years, respectively.
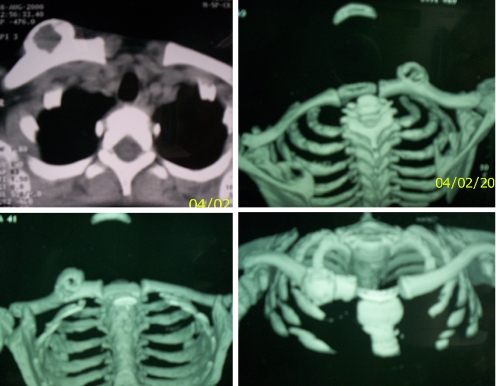
Case 6 was a 12-year-old athletic boy who presented with a painless swelling over the clavicle. On plain X-rays and CT scan (Fig. 2), the tumour proved to be a periosteal lesion. On histopathological examination, it was found to be a desmoid tumour. The patient was treated with partial claviculectomy and was free of disease at last follow-up of 5 years.
Fig. 2.
CT scan images showing a periosteal desmoid tumour of the clavicle
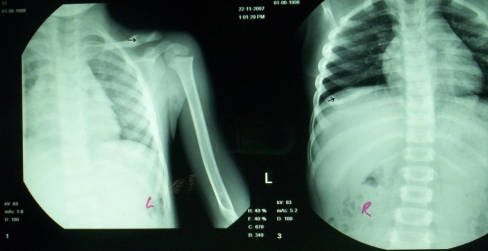
Case 7 was a known case of histiocytosis X, with multiple bony lesions involving the left clavicle, the right fifth rib, and skull (Fig. 3). The rib was excised as it was painful, and the patient was treated with multiagent chemotherapy. The lesion showed spontaneous radiological regression, and the patient had no complaints at final follow-up of 3 years.
Fig. 3.
Eosinophilic granuloma involving left clavicle and right seventh rib in a 6-years old boy
Case 9 was a known case of multiple myeloma who presented with a clavicular lesion on skeletal survey. The patient was treated with chemotherapy and died with widespread disease 6 years after presentation. Case 12 had presented with pain and stiffness of right shoulder and was being treated at another institute for periarthritis of shoulder. A radiograph of the shoulder revealed a lytic lesion of the right acromion, and a bone scan revealed multiple vertebral and pelvic lesions. Urine biochemistry and serum electrophoresis confirmed the diagnosis of multiple myeloma. The patient was disease-free at final follow-up of 1 year.
Case 10 presented with a huge swelling (10 × 8 cm) involving the left clavicle that proved to be a plasmacytoma on histopathological examination. A bone scan failed to reveal any other lesion in the body. The patient was treated with complete claviculectomy and chemotherapy, and was free of disease at final follow-up of 4 years.
Case 12 presented to us with a 12 × 8 cm fungating mass involving the left clavicle, which had been operated on at another institute and recurred (Fig. 4). He was treated with complete claviculectomy with contaminated margins. The swelling recurred 1.5 years after the first operation. The patient was operated on again, this time with palliative radiotherapy. The patient was then lost to follow-up.
Fig. 4.
A large chondrosarcoma involving the right clavicle
Discussion
The clavicle is a rare site of bone tumours in the body [2]. Its incidence has been reported to be from 0.45–1.01% of all bone tumours [2, 7]. Consequently, the experience of most orthopaedic oncologists is limited to a small number of cases. For the same reason, there is a paucity of literature on the management of tumours of this bone, the majority being case reports or series with a small number of patients.
The most commonly reported site of involvement of the clavicle is the acromial end, and tumours of the diaphyseal region are rare [7, 16]. Our series, however, had an equal distribution of tumours in all areas of the bone.
The peculiarities of the clavicle have clinical significance for the orthopaedic oncologist. The overall incidence and relative occurrence of tumours and tumorous lesions of the clavicle resemble those of flat bones and not other long bones [11]. The clavicle is subcutaneous throughout its length, and the cases present quite early as even a small swelling is detected early by the patient. The middle supraclavicular nerve, sometimes entrapped in the tumour or in the operative scar, may give rise to severe pain [10], although this was not found in any of our cases undergoing surgery. Furthermore, the decision in favour of a wide or radical excision of a clavicular tumour is easier to make than in other long bones, as no reconstruction is required.
All the biopsies were done by the open incisional technique. Although needle biopsy would have been easy because the clavicle is a subcutaneous bone, it is recommended that needle biopsy be avoided in clavicle tumours for fear of injury to the neurovascular structures that are in close relation with it [9]; injury is also more likely when the tumour softens the consistency of the bone by way of destruction of the cortex.
That a majority of tumours of the clavicle are malignant is a fact reflected in many of the previous reports [14, 16]. This series had eight primary malignant bone tumours (66%). The commonest histological diagnosis of clavicular tumours has been variously reported as myeloma [14] or osteosarcoma [16]. In our series, however, Ewing’s sarcoma was the most common histological diagnosis. Further, the average age of the patients was higher than the age group in which Ewing’s sarcoma is normally seen in other parts of the body. Ewing’s sarcoma is the commonest sarcoma to occur in flat bones (pelvis, ribs, face) [11], and thus it is logical that it should be common amongst clavicular tumours, the clavicle being a bone with a similar mode of ossification and development. A total claviculectomy is obviously the procedure of choice if a definitive cure is the goal [17]. For patients with sarcomas, the importance of chemotherapy is increasingly being recognised in improving disease-free survival of patients in whom complete resection is not feasible [6].
Clavicular tumours have been previously classified by Natarajan et al. according to the amount of clavicle that had to be resected [13]. Our series included a case (case 6) not included in the above classification, the periosteal tumours, which may be treated adequately by hemicortical claviculectomy. Periosteal desmoids are a result of avulsive cortical microinjuries, commonly found in the lower end of the femur [12]. The authors, after a thorough search of English literature, failed to find a periosteal desmoid tumour reported to occur in the clavicle. The indication for surgery in this case was cosmetic, and in retrospect, we believe that a hemicortical claviculectomy would have sufficed in this case.
Eosinophilic granuloma at this site can be misdiagnosed as a primary lesion, [18], the clavicle being a rare site for bone tumours. Our patient, however, was known to have disseminated histiocytosis X, thus making the diagnosis easy. Chemotherapy is a known form of treatment of this entity, when systemic involvement predominates [8].
Most of the tumours reported in our series have either been reported to occur in the clavicle as rare occurrences in sporadic case series or reports [1, 18, 19] or have not been previously reported (periosteal desmoid). Giant chondrosarcoma similar to our patient has been reported earlier [15].
The function of the involved shoulder girdle was analysed in all the cases. Our study confirmed that total or subtotal excision of the clavicle is rarely associated with a clinically significant loss of function [20], and tedious attempts at reconstruction of the clavicle may not be necessary [5]. That the clavicle is a dispensable bone makes the decision of a subtotal or total excision easier.
To conclude, tumours of the clavicle are rare lesions with a histopathological profile quite different from that seen in other long bones. A high index of suspicion is needed for timely diagnosis and management of tumours at these rare sites. The treatment of clavicular tumours should mostly include partial or complete claviculectomy, the oncological and functional results of which are excellent. A rare case of a periosteal desmoid of clavicle is described.
References
- 1.Amalourde A, Vinayaga P, Naveed N, Jamal A, Looi LM, Sengupta S. A rare case of chondrosarcoma of the clavicle. Med J Malaysia. 2004;59(Suppl F):60–62. [PubMed] [Google Scholar]
- 2.Dahlin DC, Unni KK. Bone tumors: general aspects and data on 8542 cases, 4th edn. Springfield, IL: Thomas; 1986. [Google Scholar]
- 3.Ellis H, Johnson D. Pectoral girdle, shoulder and axilla. In: Standring S, editor. Gray’s anatomy. The anatomical basis of clinical practice. 39th. Edinburgh: Elsevier Churchill Livingstone; 2005. [Google Scholar]
- 4.Enneking WF, Dunham W, Gebhardt MC, Malawer M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop. 1993;286:241–246. [PubMed] [Google Scholar]
- 5.Kalbermatten DF, Haug M, Schaefer DJ, Wolfinger E, Schumacher R, Messmer P, Pierer G. Computer aided designed neo-clavicle out of osteotomized free fibula: case report. Br J Plast Surg. 2004;57(7):668–672. doi: 10.1016/j.bjps.2004.05.013. [DOI] [PubMed] [Google Scholar]
- 6.Kellie SJ, Pratt CB, Parham DM, Fleming ID, Meyer WH, Rao BN. Sarcomas (other than Ewing’s) of flat bones in children and adolescents. A clinicopathologic study. Cancer. 1990;65(4):1011–1016. doi: 10.1002/1097-0142(19900215)65:4<1011::AID-CNCR2820650428>3.0.CO;2-#. [DOI] [PubMed] [Google Scholar]
- 7.Klein MJ, Lusskin R, Becker MH, Antopol SC. Osteoid osteoma of the clavicle. Clin Orthop. 1979;143:162. [PubMed] [Google Scholar]
- 8.Ladisch S. Histiocytosis syndromes of childhood. In: Behrman RE, Kleigman RM, Jenson HB, editors. Nelson textbook of pediatrics. Philadelphia: Saunders; 2004. pp. 1727–1730. [Google Scholar]
- 9.Malawer M, Wittig J. Overview of resections around the shoulder girdle: anatomy, surgical considerations and classification. In: Malawer MM, Sugarbaker PH, editors. Musculoskeletal cancer surgery. Treatment of sarcoma and allied diseases. Dordrecht: Kluwer Academic; 2001. pp. 179–202. [Google Scholar]
- 10.McGregor AL, du Plessis DJ. A synopsis of surgical anatomy. 18th. Bombay: KM Verghese; 1969. [Google Scholar]
- 11.Minard-Colin V, Kalifa C, Guinebretiere JM, Brugieres L, Dubousset J, Habrand JL, Vassal G, Hartmann O. Outcome of flat bone sarcomas (other than Ewing’s) in children and adolescents: a study of 25 cases. Br J Cancer. 2004;90(3):613–619. doi: 10.1038/sj.bjc.6601564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murad M, Bari V, Rafique MZ, Ashraf K. Periosteal desmoid. J Pak Med Assoc. 2007;57(1):44–46. [PubMed] [Google Scholar]
- 13.Natarajan M, Meller I, Malawer MM. Claviculectomy for tumors of the clavicle. Ind J Orthop. 2006;40(2):115–118. doi: 10.4103/0019-5413.34454. [DOI] [Google Scholar]
- 14.Pratt GF, Dahlin DC, Ghormley RJ. Tumors of scapula and clavicle. Surg Gynecol Obstet. 1958;106:536–544. [PubMed] [Google Scholar]
- 15.Rankin KC. Removal of giant chondrosarcoma in the clavicular region. J R Coll Surg Edinb. 1983;28(5):340–342. [PubMed] [Google Scholar]
- 16.Smith J, Yuppa F, Watson RC. Primary tumors and tumor-like lesions of the clavicle. Skeletal Radiol. 1988;17(4):235–246. doi: 10.1007/BF00401804. [DOI] [PubMed] [Google Scholar]
- 17.Turra S, Gigante C. Primary clavicular localisation of Ewing’s tumour treated by total cleidectomy. Case report and review of the literature/ Ital J Orthop Traumatol. 1988;14(3):389–393. [PubMed] [Google Scholar]
- 18.Waldman RS, Powell T. Eosinophilic granuloma of the clavicle simulating primary bone neoplasm. Clin Orthop Relat Res. 1969;64:150–152. [PubMed] [Google Scholar]
- 19.Weber KL, Makimato A, Raymond AK, Pearson MG, Jaffe N. Ewing sarcoma of the clavicle in a 10-month-old patient. Med Pediatr Oncol. 2000;34(6):445–447. doi: 10.1002/(SICI)1096-911X(200006)34:6<445::AID-MPO14>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 20.Wood VE. The results of total claviculectomy. Clin Orthop Relat Res. 1986;207:186–190. [PubMed] [Google Scholar]