Abstract
A new proximal humerus nail (Sirus) for the treatment of proximal humerus fractures has become available. This paper presents the clinical and radiological outcome of the first collective study of 36 patients. Evaluation was performed prospectively. An antero-acromial approach was used for all patients. Three fixed-angle screws were inserted in a locking technique. Thirty-six fractures were fixed with the Sirus nail. These were dislocated 2- and 3-part fractures as described by Neer (J Bone Joint Surg 52:1077–1089). Outcomes were evaluated using the Constant score. Of the 36 patients evaluated 23 had sustained a 2-part fracture and 13 a 3-part fracture. The average age at surgery was 71.2 years (range, 30–93). In 75% of the cases, good to very good outcomes were achieved. Outcomes were satisfactory in 13.8% of the cases. Twenty-five fractures were treated in a closed technique. Average operating time was 41 minutes (range, 19–106) with a fluoroscopy time of 0.6 minutes (range, 0.4–2.6). Secondary fragment dislocation occurred in two cases. After 12.1 months the average Constant score was 79.2 (range, 46–100). Initial clinical experience with the Sirus nail indicates that the procedure is straightforward and has a low complication rate. Functional outcomes are predominantly good to very good. Large fragments of the greater tuberosity and 4-part fractures are beyond the scope of this application.
Résumé
Un nouveau clou (Sirus) a été utilisé pour les fractures proximales de l’humérus. Ce travail fait le point sur les 36 premiers patients traités de cette façon. Le clou est verrouillé par trois vis dans trois directions différentes. 36 fractures ont été traitées de la sorte qu’il s’agisse de fracture de type 2 ou de fracture à 2 ou 3 fragments selon la description de Neer (J Bone Joint Surg 52:1077–1089). Le devenir de ces patients a été évalué selon le score de Constant. Sur les 36 patients évalués, 23 présentaient une fracture à 2 fragments et 13 à 3 fragments. L’âge moyen à l’intervention était de 71.2 ans (30 à 93). Ce traitement a permis d’obtenir également 75% de bons et très bons résultats. Le devenir a été satisfaisant dans 13.8% des cas. 25 fractures ont été traitées à foyers fermés. Le temps opératoire moyen a été de 41 minutes (de 19 à 106) et le temps d’utilisation de l’amplificateur de brillance de 0.6 minute (de 0.4 à 2.6). Un débricolage de la fracture est survenu dans deux cas. Après 12.1 mois d’évolution le score de Constant était en moyenne de 79.2 (de 46 à 100). Cette première expérience clinique montre que le taux de complications était relativement faible avec le traitement de ces fractures par le clou Sirus. Le devenir fonctionnel de ces patients reste bon ou très bon. Les fractures plus importantes de la grosse tubérosité ou les fractures à 4 fragments restent actuellement un sujet à l’étude.
Introduction
Proximal humerus fractures are among the three most frequent fractures of the human skeleton. Epidemiological trends show that the importance of these fractures is continuously on the increase. In addition to conservative and prosthetic management, the majority of these injuries are treated by internal fixation [9, 10, 18, 19, 21, 23, 24].
Joint-preserving, surgical treatment of humeral head fractures has undergone numerous innovations in recent years. The results of conventional plate fixation without fixed-angle locking have been less than satisfactory. Primary reduction loss, implant loosening, and humeral head necrosis have been characteristic of these procedures [1, 5, 14]. The new generation of fixed-angle plate fixators appear to solve the problem of premature implant loosening. The functional outcomes could clearly be improved [10, 12, 13]. Although closed techniques have been described [16], the majority of plate fixators are implanted through a deltopectoral approach. This may however impair the blood supply to the humeral head and affect the functional outcome [7, 16].
Thus, intramedullary load carriers have become increasingly important in the treatment of proximal humerus fractures [2, 8, 11, 12, 19, 21, 23]. Nail systems have been applied in the region of the metaphysis for some time. Their main advantages are the possibility of closed reduction and minimally invasive implantation. Initial clinical investigations have yielded good functional outcomes combined with a relatively low complication rates [12, 17, 23].
The Sirus proximal humerus nail is a new implant for the management of unstable subcapital and humeral head fractures (3-part). The aim of this study was to report both the surgical technique and initial clinical and radiological results.
Materials and methods
Study design and patient sample
From November 2002 to December 2004, 36 patients with dislocated 2- and 3-fragment fractures of the humeral head were treated with a new proximal humerus nail system (Sirus) by one of the authors (B.F.). Pathological fractures as well as non-dislocated and stable impacted fractures were excluded. A total of 36 fractures were operated upon. Nine men and 27 women were affected with an average age of 71.2 years (range, 30–93). Twenty-two patients were over 60 years of age. The dominant side was affected in 21 patients and the non-dominant side in 15 patients (right side: 19, left side: 17). The Neer classification [20] yielded 23 patients with a 2-part and 13 with a 3-part fracture. In 8 of the 13 three-part fractures tension banding of the rotator cuff to the humeral head screw of the Sirus nails was performed with nonresorbable suture. Immediately postoperative, a soft shoulder brace was applied with the arm in 30° abduction and slight anteflexion for 6 weeks. Postoperative functional management in the brace was commenced on the second postoperative day. For the 3-part fractures, abduction was restricted to 30° for the first 3 weeks and then to 60° for another 3 weeks. Patients with 2-part fractures were permitted to move freely below the pain threshold. Clinical and radiological follow-up took place after 6 weeks, and after 3, 6, and 12 months. At these intervals, the clinical outcome was quantified using the absolute Constant score [4]. At final follow-up the patient recorded a subjective level of satisfaction from 1, excellent, to 6, poor.
The implant
The Sirus proximal humerus nail (supplied by Zimmer Holdings, Inc.) is made from Protasul 100. It is 120 mm long and has a curvature of 8°. It has a proximal diameter of 9.3 mm. Proximal locking is achieved by insertion of three 3.9 mm humeral head screws with short cancellous bone thread. The unthreaded part of the screw is positioned within the nail (Fig. 1). The humeral head screws are positioned three-dimensionally in the humeral head. The cranial screw is inserted from posterior at a 40° angle to ensure secure fixation of the greater tuberosity as required. The cranial screw is firmly fixed in the nail by mounting the end cap. For distal locking two 3.9 mm standard locking bolts are inserted.
Fig. 1.
a Cannulated Sirus nail for the stabilisation of humeral head fractures; length 120 mm, diameter 8.5 mm. b Three cancellous bone screws are anchored in the humeral head (diameter 3.9 mm). The solid unthreaded part lies within the nail. c View from caudal showing the spatial orientation of the humeral head screws
Surgical technique
All patients were operated on under general anaesthetic in the beach-chair position through an anterior acromial approach [22]. The incision was made anterolateral to the acromion. The length of the incision varied from 2 cm for the closed technique, 2–5 cm for the “mini-open-technique” and >5 cm for open reduction. The fractures were reduced in the closed technique either by manipulating the arm or by using the joystick technique. Reduction of dislocated fragments of the greater tuberosity was likewise performed either with the joystick technique or by applying tension on the supraspinatus tendon by pulling on a non-resorbable suture thread. After opening the medullary cavity with the cannulated reamer, the nail was introduced over the guide wire. Next, three guide wires were inserted into the head fragment using the aiming device and appropriate guide sleeves (Fig. 2a,b). If necessary, the guide wires were removed and the insertion depth of the nail modified. After extracorporal length measurement, the humeral head screws were inserted through the guide sleeves. Distal locking was performed using the standard technique via the aiming device. Additional tension banding of the rotator cuff was implemented with non-resorbable sutures as required (Fig. 2c). Finally, an end cap was mounted to fix the proximal “greater tubercle” humeral head screw firmly in the nail. Postoperative management commenced on the second postoperative day with functional exercises.
Fig. 2.
a Implantation in a minimally invasive technique through an anterior-acromial approach. The aiming device is radiolucent. b Guide wires are placed initially to determine the level of insertion and the length of the humeral head screws. c The rotator cuff can also be attached to the implant
Follow-up
A series of radiographs in three planes was taken at each follow-up. Implant position, fragment alignment, and bone consolidation were evaluated. From the sixth month onwards evaluation also focussed on the development of humeral head necrosis. In addition, the seating of the proximal humeral head screws was investigated. Pain was evaluated on the visual analog scale (VAS). The pain scale ranges from 0 to 100, whereby 0–25 indicates no symptoms, 26–50 mild symptoms, 51–75 moderate symptoms, and 76–100 severe pain. Clinical outcome was recorded using the Constant score. Evaluation of subjective pain ranges from 0–15 points, activities of daily living 0–20 points, range of motion 0–40 points, and strength 0–25 points. A very good outcome is scored as 86–100 points, good as 71–85 points, satisfactory 51–70 points, and a poor outcome as less than 50 points.
Additionally, the patient was awarded a grade of 1–6 to record overall subjective satisfaction, whereby 1 was excellent and 6 was poor.
Statistical analysis was performed using SPSS 12.0 (SPSS Inc., USA). Testing of the recorded data for normal distribution yielded a negative result with the consequence that only non-parametric statistical procedures were applied to determine correlation. Correlation of the individual parameters was calculated according to Spearman-rho. Comparison between groups was performed with the Mann-Whitney-U test. Statistical significance was accepted for a value of p < 0.05.
Results
General
Thirty-six patients were available for follow-up at 12.1 months (range, 11.2–13.0). According to the Neer fracture classification 23 patients had an unstable 2-part fracture and 13 had a 3-part fracture. Primary nerve damage was not diagnosed. No evidence was found for superficial or deep infections in any patient. The average operating time was 41 minutes (range, 19–106) and fluoroscopy time was 0.6 minutes (range, 0.4–2.6). Reduction in 32 cases was performed in the closed or joystick technique. In two cases a mini-open approach was required, and two other cases used an open technique. Average incision length was 3.4 cm (range, 2–8). Tension banding of the rotator cuff around the screw heads was performed in a total of eight cases. Additional osteosynthesis was not required in any case.
Clinical outcomes
At final follow-up after 12.1 months on average, the mean absolute Constant score was 79.2 (range, 49–100). The score was 83.6 points for 2-part fractures and 71.2 for 3-part fractures (p < 0.02). Nineteen patients (52.8%) achieved a very good outcome, eight patients (22.2%) a good outcome, five patients (13.9%) a satisfactory outcome and four patients (11.1%) a poor outcome. In summary, 75% achieved good to very good outcomes (Table 1). The Constant score improved subsequently. The results were documented as 46 (range, 24–75) after 6 weeks, 59 (range, 28–80) after 3 months, 67 (range, 35–91) after 6 months, and 79.2 (range, 49–100) points after 12 months (Table 2).
Table 1.
Clinical outcomes according to the Constant score (average) at the time of final follow-up and categorised by fracture classification
| 2-fragment | 3-fragment | Total | |
|---|---|---|---|
| n = 23 | n = 13 | n = 36 | |
| Pain (max. 15) | 14.5 | 13.3 | 14.1 |
| ADL (max. 20) | 15.8 | 11.3 | 14.2 |
| Range of motion (max. 40) | 33.5 | 27.3 | 31.3 |
| Strength (max. 25) | 19.8 | 19.3 | 19.6 |
| Absolute Constant score (max. 100) | 83.6 | 71.2 | 79.2 |
| Pain VAS (0–100) | 19.2 | 27.8 | 22.3 |
| Excellent (86–100 points) | 16 | 3 | 19 |
| Good (71–86 points) | 2 | 6 | 8 |
| Satisfactory (51–70 points) | 2 | 3 | 5 |
| Poor (<50 points) | 2 | 2 | 4 |
Table 2.
Absolute Constant score during the course of healing (n = 36)
Pain
The average pain score on the visual analog scale came to 21.6 points (range, 10–46). Twenty-seven patients (75%) showed no sign of pain or only mild pain. Pain levels showed a high positive correlation with range of motion (p < 0.001) and had a negative influence on the Constant score (p = 0.001).
Range of motion
Active abduction in 20 patients (55.5%) was greater than 120°, in eight patients (22.2%) between 90° and 120°, in seven patients (19.4%) between 60° and 90° and in one patient (2.7%) below 60°. In summary, 28 patients (77.7%) could actively raise the arm sideways beyond 90° without pain.
Strength
The average strength value on the Constant score was recorded as 19.6 points (range, 10–25). In eight patients, strength measurement took place with the arm between 90° and 60° because the arm could not be elevated to 90°, and a maximum score of 15 points was achieved. Age was negatively correlated to the strength score(p < 0.004).
Patient satisfaction
Evaluation of patient satisfaction according to grade produced an average grade of 1.91. Twenty-six patients (72.2%) recorded grades 1 and 2, ten patients (27.8%) recorded grades 3 and 4 and no patient recorded less than 4. The grades showed a strong correlation with the Constant score (p < 0.001).
Radiological evaluation
Good reduction with disimpaction of the humeral head and anatomical adaptation of the greater tuberosity fragment was achieved in every case. In two patients the nail protruded at its proximal end over the cortex. Implants were removed prematurely in these two patients. A total of 108 humeral head screws were implanted in 36 patients. A summary of complications within the study for these 36 patients can be found in Table 3. Of these, one screw in three patients penetrated the joint surface. In two of the patients, this led to a significant increase in symptoms and/or functional limitations. The screw had to be removed under local anaesthesia in one patient. In addition, significant screw migration laterally causing painful restriction to movement was observed in two patients. The screw had to be removed prematurely under local anaesthesia in one patient. For the other patient, the screw was extracted during total implant removal. Secondary reduction loss of the head fragment was not observed. None of the patients were affected by nail breakage. Radiological evaluation revealed complete bone consolidation of all fractures. The postoperative reduction was maintained in all cases until healing.
Table 3.
Complications within the study (n = 36)
| Complications | Number | Remarks |
|---|---|---|
| Superficial or deep infections | 0 | |
| Secondary tuberosity migration | 2 | |
| Secondary calvarial dislocation | 0 | |
| Implant loosening | ||
| - Shaft region | 0 | |
| - Head region | 0 | |
| Nail elevation | 2 | |
| Intraarticular screws | 3 | Of a total of 108 implanted screws |
| Screw migration (>5 mm) | 4 | Of a total of 108 implanted screws |
| Screw breakage | 2 | Of a total of 108 implanted screws |
| Pseudarthrosis | 0 | |
| Partial humeral head necrosis | 0 | |
| Periarticular ossifications | 0 | |
Discussion
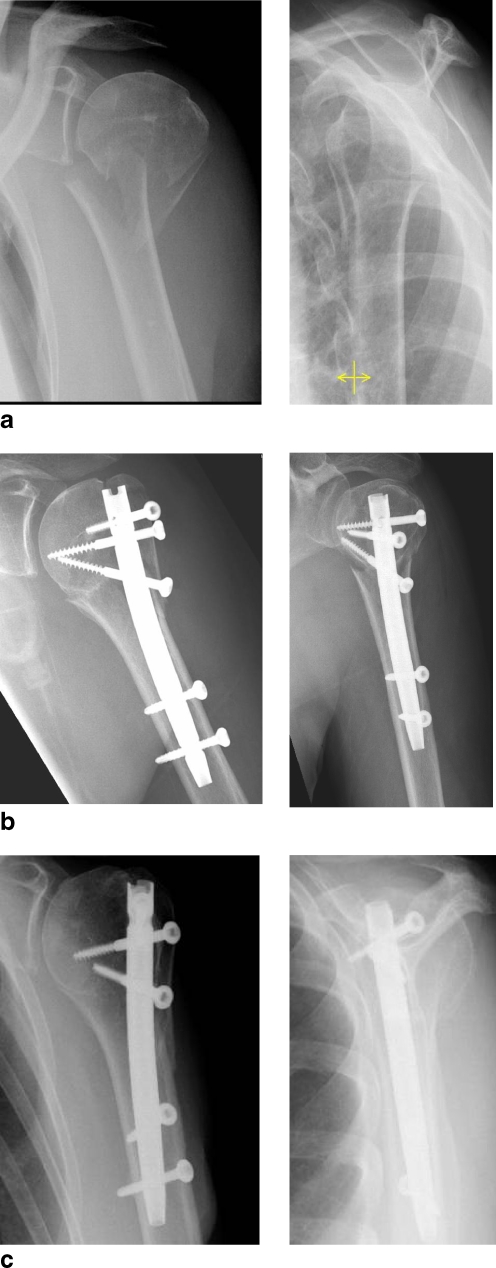
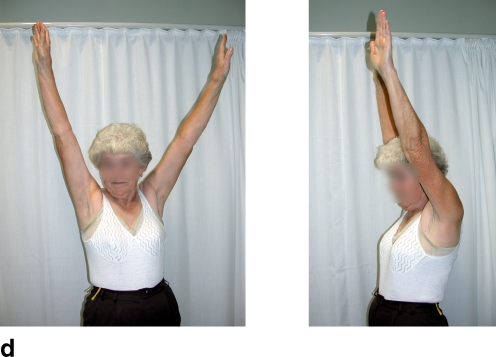
The results of this study show that management of dislocated 2- and 3-part fractures of the humeral head with a proximal intramedullary nail is associated with low complication rates and good functional outcomes (Fig. 3). High primary stability was achieved with this implant even for osteoporotic fractures, a setting that had been investigated biomechanically in advance [6]. Thus, postoperative functional management was possible at low pain levels.
Fig. 3.
a Clinical case of a 70-year-old patient with unstable 2-part fractures. b Fracture stabilized with a Sirus nail. c, d At the one-year postoperative follow-up, the fracture has consolidated and shoulder function is good (Constant score 100)
Exact preoperative classification of the fracture is of crucial importance since all further treatment options depend upon it. These options include the size of the approach and the necessity of rotator cuff tension banding. Since precise, unequivocal classification is not always possible on the basis of conventional radiographs, computed tomography may be required in individual cases.
The antero-acromial approach according to Riemer, applied here is a standard approach for antegrade intramedullary nailing that has produced better functional results than the anterolateral approach [22]. The surgical technique has proven to be straightforward and uncomplicated. Primary wire markers indicating screw orientation in the humeral head have the advantage that the nail insertion depth can be adjusted after radiographic inspection without advanced drilling of large holes. In addition, once inserted and confirmed radiologically they facilitate exact length measurement with an extracorporal measuring device without opening the joint surface. Additional tension banding of the greater tubercle fragment has already proven worthwhile in combination with plate fixators. This technique can also be performed in combination with an intramedullary nail, whereby the rotator cuff must be held by non-resorbable suture threads knotted around the humeral head screws.
In principle, there is a risk of damaging the axillary nerve and/or its branches during insertion of the humeral head screws. It was not observed in this series. Investigations by Blum [3] have shown that the risk is greatest for screws inserted from posterior to anterior. The cranial humeral head screw for the Sirus nail is inserted from posterolateral to anteromedial, but it lies very far cranially and has no direct topographical relationship to the axillary nerve. The two screws inserted more caudally run from lateral to medial and are therefore within the safe zone. Basically, all humeral head screws should be implanted by blunt dissection with application of a tissue protection sleeve.
The intramedullary nail was not seen to fail in this study. In our sample, significant migration of a humeral head screw was diagnosed in two patients. This low rate of screw migration can be attributed to fixed-angle blocking due to the end cap and to the cancellous bone thread of the humeral head screw.
In addition to internal fixation and total joint replacement procedures for the treatment of humeral head fractures, conservative therapy also plays an important role [15, 25]. Apart from factors relating to fracture morphology, the general condition of the patient is an important criterion. Stable, slightly dislocated fractures can be treated conservatively. High comorbidity combined with poor bone stock and low patient expectations in terms of function of the extremity are good indications for conservative treatment. The patient sample reported here consisted predominantly of younger patients with unstable fractures and good bone stock with concomitant disorders. These patients benefit from surgical treatment since active postoperative exercises are possible immediately, which shortens the overall rehabilitation process.
References
- 1.Bathis H, Tingart M, Bouillon B, Tiling T. Surgical treatment of proximal humeral fractures. Is the T-plate still adequate osteosynthesis procedure? Zentralbl Chir. 2001;126:211–216. doi: 10.1055/s-2001-12498. [DOI] [PubMed] [Google Scholar]
- 2.Blum J, Rommens PM, Janzing H. The unreamed humeral nail: a biological osteosynthesis of the upper arm. Acta Chir Belg. 1997;97(4):184–189. [PubMed] [Google Scholar]
- 3.Blum J, Rommens PM. Proximal interlocking of humeral intramedullary nails and risk of axillary nerve injury. Unfallchirurg. 2002;105(1):9–13. doi: 10.1007/s113-002-8158-5. [DOI] [PubMed] [Google Scholar]
- 4.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop. 1987;214:160–164. [PubMed] [Google Scholar]
- 5.Damanakis K, Schaal O, Mann J, Muller KH. Modified treatment concept in fractures of the humeral head in elderly patients. Unfallchirurg. 1996;99:561–568. [PubMed] [Google Scholar]
- 6.Füchtmeier B, May R, Hente R, Maghsudi M, Völk M, Hammer J, Nerlich M, Prantl L (2007) Proximal humerus fractures: a comparative biomechanical analysis of new intra and extramedullary implants. Arch Orthop Traum Surg (April 25; Epub ahead of print) [DOI] [PubMed]
- 7.Gerber C, Schneeberger AG, Vinh TS. The arterial vascularization of the humeral head. An anatomical study. J Bone Joint Surg. 1990;72:1486–1494. [PubMed] [Google Scholar]
- 8.Gregory PR, Sanders RW. Compression plating versus intramedullary fixation of humeral shaft fractures. J Am Acad Orthop Surg. 1997;5(4):215–223. doi: 10.5435/00124635-199707000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Habermeyer P. Fracture of the head of the humerus. Unfallchirurg. 1997;100:820–837. doi: 10.1007/s001130050199. [DOI] [PubMed] [Google Scholar]
- 10.Hente R, Kampshoff J, Kinner B, Füchtmeier B, Nerlich M. Treatment of dislocated 3- and 4-part fractures of the proximal humerus with an angle-stabilizing fixation plate. Unfallchirurg. 2004;107:769–782. doi: 10.1007/s00113-004-0818-7. [DOI] [PubMed] [Google Scholar]
- 11.Herscovici D, Jr, Saunders DT, Johnson MP, Sanders R, Pasquale T. Percutaneous fixation of proximal humeral fractures. Clin Orthop. 2000;375:97–104. doi: 10.1097/00003086-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Hessmann MH, Rommens PM. Osteosynthesis techniques in proximal humeral fractures. Chirurg. 2001;72(11):1235–1245. doi: 10.1007/s001040170026. [DOI] [PubMed] [Google Scholar]
- 13.Köstler W, Strohm PC, Sudkamp NP. New techniques for bone synthesis on the humerus. Chirurg. 2002;73:969–977. doi: 10.1007/s00104-002-0547-9. [DOI] [PubMed] [Google Scholar]
- 14.Kuner EH, Siebler G. Dislocation fractures of the proximal humerus—results following surgical treatment. A follow-up study of 167 cases. Unfallchirurgie. 1987;13:64–71. doi: 10.1007/BF02585983. [DOI] [PubMed] [Google Scholar]
- 15.Lill H, Josten C. Conservative or operative treatment of humeral head fractures in the elderly? Chirurg. 2001;72:1224–1234. doi: 10.1007/s001040170025. [DOI] [PubMed] [Google Scholar]
- 16.Lill H, Hepp P, Rose T, Konig K, Josten C. The angle stable locking-proximal-humerus-plate (LPHP) for proximal humeral fractures using a small anterior-lateral-deltoid-splitting-approach - technique and first results. Zentralbl Chir. 2004;129(1):43–48. doi: 10.1055/s-2004-44870. [DOI] [PubMed] [Google Scholar]
- 17.Mittlmeier TW, Stedtfeld HW, Ewert A, Beck M, Frosch B, Gradl G. Stabilization of proximal humeral fractures with an angular and sliding stable antegrade locking nail (Targon PH) J Bone Joint Surg Am. 2003;85A(Suppl 4):136–146. doi: 10.2106/00004623-200300004-00019. [DOI] [PubMed] [Google Scholar]
- 18.Misra A, Kapur R, Maffulli N. Complex proximal humeral fractures in adults—a systematic review of management. Injury. 2001;32:363–372. doi: 10.1016/S0020-1383(00)00242-4. [DOI] [PubMed] [Google Scholar]
- 19.Müller F, Voithenleitner R, Schuster C, Angele P, Weigel B. Operative treatment of proximal humeral fractures with helix wire. Unfallchirurg. 2006;109(12):1041–1047. doi: 10.1007/s00113-006-1088-3. [DOI] [PubMed] [Google Scholar]
- 20.Neer CS. Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg. 1970;52:1077–1089. [PubMed] [Google Scholar]
- 21.Resch H, Povacz P, Frohlich R, Wambacher M. Percutaneous fixation of three- and four-part fractures of the proximal humerus. J Bone Joint Surg Br. 1997;79:295–300. doi: 10.1302/0301-620X.79B2.6958. [DOI] [PubMed] [Google Scholar]
- 22.Riemer BL, D’Ambrosia R, Kellam JF, Butterfield SL, Burke CJ. The anterior acromial approach for antegrade intramedullary nailing of the humeral diaphysis. Orthopedics. 1993;16(11):1219–1223. doi: 10.3928/0147-7447-19931101-08. [DOI] [PubMed] [Google Scholar]
- 23.Stedtfeld HW, Attmanspacher W, Thaler K, Frosch B. Fixation of humeral head fractures with antegrade intramedullary nailing. Zentralbl Chir. 2003;128(1):6–11. doi: 10.1055/s-2003-37364. [DOI] [PubMed] [Google Scholar]
- 24.Wijgman AJ, Roolker W, Patt TW, Raaymakers EL, Marti RK. Open reduction and internal fixation of three and four-part fractures of the proximal part of the humerus. J Bone Joint Surg Am. 2002;84:1919–1925. [PubMed] [Google Scholar]
- 25.Zyto K, Ahrengart L, Sperber A, Tornkvist H. Treatment of displaced proximal humeral fractures in elderly patients. J Bone Joint Surg Br. 1997;79:412–417. doi: 10.1302/0301-620X.79B3.7419. [DOI] [PubMed] [Google Scholar]