Abstract
The Duraloc cup is a frequently used metal-backed, porous-coated, hemispherical, press-fit acetabular component. Published data on loosening rates are contradictory. In this study we investigated migration patterns with computer-assisted Einzel-Bild-Roentgen-Analyse (EBRA) of 67 Duraloc 100 cups. Cup migration and clinical scores were analysed over a 5-year follow-up period. Median total migration of the Duraloc 100 cup was 1.21 mm at 5 years. Seventy-five percent of implants were radiologically stable at 2 years and 90% at 4 years. One cup loosened aseptically at 60 months, requiring revision. Cup diameters ≥54 mm migrated significantly more than cups <54 mm in diameter (p = 0.029 at 4 years). There was a significant correlation between high polyethylene wear and further migrating cups within the first post-operative year (p = 0.035 at 12 months). Our analysis revealed significantly higher wear in males (p = 0.029 at 4 years). Radiological loosening at two years could be calculated using receiver-operating characteristic curve analysis, and 1.2 mm as an adequate threshold value (sensitivity = 100%, specificity = 89%).
Résumé
La cupule DURALOC est une cupule utilisée de façon fréquente avec un composant acétabulaire sans ciment, porous coated, hémisphérique. Les publications indiquant les taux de descellement de cet implant sont très contradictoires. Dans cette étude, nous avons étudié la migration de cette cupule par méthode informatique avec un logiciel de type EBRA. La migration de la cupule et les scores ont été analysés après une période de cinq ans de suivi. La migration moyenne de 100 cupules DURALOC a été de 1.21mm à 5 ans, 75% des implants étaient stables radiologiquement à 2 ans et 90% à 4 ans. Une cupule s’est descellée de façon aseptique à 60 mois, nécessitant une révision. Les cupules de diamètre ≥54mm migrant de façon plus fréquente que les cupules plus petites (p = 0.029 à 4 ans). De même, a été mis en évidence une corrélation significative entre l’usure du polyéthylène et la migration de la cupule dans les premières années (p = 0.035 à 12 mois). Notre analyse montre qu’il existe une usure significativement plus importante chez les hommes (p = 0.029 à 4 ans). La valeur seuil de l’usure à 2 ans étant de 1.2mm (sensitivité = 100% ; spécificité = 89%)
Introduction
Progressive cup migration is a predictive indicator for later aseptic loosening [10, 12, 14]. The cup used in this study is a metal-backed, porous-coated, hemispherical, press-fit acetabular component [2, 3, 8, 17, 18, 20]. Published data on loosening rates with this cup are contradictory: loosening rates of 35 [18] to 48% [17] at 2 years have been reported, while re-evaluation after 4 years revealed a loosening rate of 16% [18] in one study. On the other hand, 97 [2] to 100% [3] of these prostheses are still in place after 10 years. This contradiction between clinical and radiological results may be attributed to a difference in the definition of loosening and led us to a detailed analysis of our own results using Einzel-Bild-Roentgen-Analyse (EBRA) [11] for migration analysis and sophisticated statistical methods.
Patients and methods
This study included 67 patients allocated for total hip arthroplasty in our department. In each patient a cementless Duraloc 100 cup (DePuy, Warsaw, IN, USA) was implanted. There were 44 women and 23 men, with a median age of 73 years (range: 40–80 years). Diagnosis was primary osteoarthritis (OA) in 79.1% (53/67), avascular necrosis of the femoral head (AVN) in 19.4% (13/67) and hip dysplasia in 1.5% (1/67). Vision 2000 stems and gas plasma sterilised Enduron polyethylene liners (DePuy, Warsaw, IN, USA) were always used.
Patients underwent standardised anteroposterior radiographs of the pelvis centred on the superior border on the symphysis. Prospectively the radiographs were obtained 1 and 6 weeks, 3 and 6 months post-operatively, and annually thereafter. After digitising the radiographs (75 dpi resolution), using a VIDAR Diagnostic Pro Plus digitiser (VIDAR Systems Corporation, Herndon, VA, USA), the cup migration behaviour was analysed using EBRA software [11].
The Harris Hip Score (HHS) [4] was used for clinical assessment and health status was measured by the 36-item short-form health survey [21]. Patients were followed up prospectively for a mean 5-year period (range: 3.9–6.5 years).
As demonstrated by other authors [12, 17, 18] we also used the Pythagorean theorem for calculating the total cup migration. Negative horizontal movement was defined as medial migration. Negative vertical migration values (expressing distal migration) up to 1 mm were caused by the limited accuracy of the EBRA measurement method. Loosening was defined as total migration over 1 mm at 2 years and over 2 mm at 4 years [12]. Radiolucent lines according to DeLee and Charnley [1], tilting of the cup and formation of bone cysts were noted.
For statistical analysis, we used NCSS (Number Cruncher Statistical Systems, Hintze J., Kaysville, UT, USA). The Mann-Whitney U test was used for group comparisons, and correlations were analysed according to Spearman. No adjustments were made for multiple testing. We calculated the receiver-operating characteristic (ROC) to analyse the predictive value of migration after 2 years with respect to loosening. The area under the ROC curve (AUC) was used as an index of diagnostic accuracy.
Results
All patients showed significant improvement in clinical scores. The HHS improved from 43 preoperatively (range: 12–78) to 91 at the final follow-up examination (range: 33–100). The results were rated excellent (HHS 90–100 points) in 73.1% (49/67), good (HHS 80–89 points) in 16.4% (11/67), fair (HHS 70–79 points) in 6% (4/67) and poor (HHS < 70 points) in 4.5% (3/67) of cups. Two of these three patients presenting poor results were over 80 years of age: one had a severe limp (Trendelenburg sign positive) with a high-grade weakness of the gluteal muscles and suffered from mild hip pain. The other patient required a wheelchair because of hemiparesis following a stroke. Hip function was clinically satisfactory. The patient with the lowest HHS (HHS 33 points) was a 68-year-old man suffering from marked pain. Clinically and radiologically the stem and cup showed clear signs of loosening. Both components had to be revised due to aseptic loosening at 60 months. Analysing the migration behaviour of this loosened cup, conspicuous above average migration had appeared by 12 months (1.64 mm total migration).
Migration curves could be calculated for 60 of 67 cups. Median total migration was 1.21 mm at 5 years (Table 1). Migration speed decreased after the first year. Median wear of the Enduron polyethylene liner was 0.20 mm at 1 and 0.75 mm at 5 years.
Table 1.
Median total migration of all cups
| Median total migration over time (mm) | 12 months | 24 months | 36 months | 48 months | 60 months |
|---|---|---|---|---|---|
| Duraloc 100 cups (n = 60) | 0.51 | 0.71 | 0.82 | 1.06 | 1.21 |
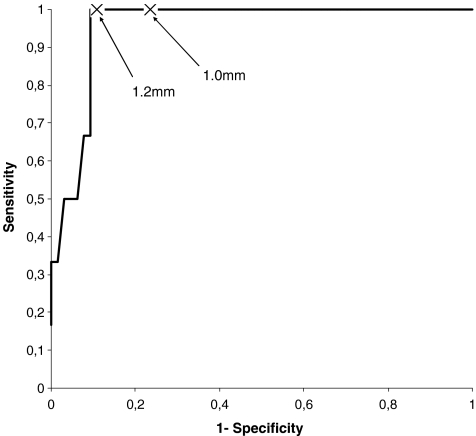
Using the definition of cup loosening as proposed by Krismer (1 mm threshold value at 2 years and 2 mm at 4 years) [12], 75% (45/60) were radiologically stable at 2 and 90% (54/60) of all implants were radiologically stable at 4 years. Using ROC curve analysis (Fig. 1), we established 1.2 mm as an alternative threshold value for loosening at 2 years from our data. The area under the ROC curve was 0.96 (95% confidence interval: 0.86–0.99). Sensitivity of loosening remained 100%, but the specificity of 89% was even higher compared to the 1 mm cut-off, with sensitivity of 100% but specificity of 76% (Fig. 1). Using 1.2 mm as the threshold value for radiological loosening, only 18% (11 of 60) of implants were radiological loose at 2 years.
Fig. 1.
ROC curve analysis (representation of the reciprocal relationship between sensitivity and specificity, calculated for all threshold values) proposes 1.2 mm as an alternative threshold value for the definition of loosening at 2 years (AUC = 0.96)
Statistical evaluations revealed that cups ≥ 54 mm in diameter migrated significantly more than cups with a diameter < 54 mm within 4 years (p = 0.029 at 4 years, Mann-Whitney U test, Table 2). There was a significant correlation between high polyethylene wear and further migrating cups within the first post-operative year (r = 0.31, p = 0.016 at 3 months; r = 0.41, p = 0.001 at 6 months; r = 0.27, p = 0.035 at 12 months). Our analysis revealed significantly higher wear in males (Table 3). Cups with early migration of more than 1 mm at 2 years showed significantly higher migration rates at 4 and 5 years (p < 0.001 at 4 years, p = 0.010 at 5 years, Mann-Whitney U test).
Table 2.
Increased migration of cup diameters ≥ 54 mm over time (*significant value)
| Median total migration over time (mm) | 12 months | 24 months | 48 months |
|---|---|---|---|
| Cup diameters ≥ 54 mm | 0.63 | 0.78 | 1.22 |
| Cup diameters < 54 mm | 0.45 | 0.45 | 0.81 |
| p value (Mann-Whitney U test) | 0.071 | 0.073 | 0.029* |
Table 3.
Increased polyethylene wear in males (*significant values)
| Median polyethylene wear over time (mm) | 12 months | 24 months | 48 months |
|---|---|---|---|
| Male | 0.28 | 0.51 | 0.76 |
| Female | 0.14 | 0.30 | 0.42 |
| p value (Mann-Whitney U test) | 0.116 | 0.044* | 0.029* |
A significant correlation between clinical scores and migration was neither expected nor demonstrated, since 90% of all implants were radiologically stable. Gender, patient’s age (> 70 years), body weight (≥ 80 kg) and preoperative diagnosis (primary OA versus AVN) did not show any significant influence on cup movement (p = 0.13, p = 0.89, p = 0.13 and p = 0.95, respectively, at 4 years, Mann-Whitney U test).
Discussion
Cup migration measurement using EBRA digital software is an accurate method [6, 7, 15] providing sufficient precision for detecting clinically relevant migration [22]. Using EBRA software as a measurement tool for early cup movement, it can be useful for prospective analyses of the migration behaviour [12, 16]. Sophisticated analyses of the results of our study show that cups with early migration (more than 1 mm at 2 years) move significantly more at 4 and 5 years (p < 0.001 at 4 years, p = 0.010 at 5 years). In this study one cup had to be revised due to aseptic loosening at 60 months. Analysing the migration behaviour of this loosened cup, conspicuous above average early movement at 12 months appeared (1.64 mm total migration). Only two acetabular components migrated more within the first post-operative year. Therefore we also state that early migration is a predictor for later loosening [12].
Grobler et al. [3] reviewed 100 Duraloc cups over 10 years and found no aseptic radiological loosening, defining loosening as migration of more than 3 mm or tilting of more than 4°. Kim [8] followed 60 hips with Duraloc cups for a mean of 6 years and found no aseptic loosening. Our results can be compared to the results of Stöckl et al. and Stoeckl et al. [17, 18] since a disproportionately high rate of radiological loosening at 2 years can be found according to Krismer’s definition [12]. A high rate of restabilisation seems to occur between years 2 and 4: Stöckl et al. first regarded 30 of 63 cups (48%) as loose at 2 years [17]. Re-evaluation of the same cups at 4 years and adding of more radiographs leaves 22 of 62 (35%) cups radiologically unstable at 2 years and 9 of 56 (16%) at 4 years [18]. Loose cups, using the same definition (1 mm threshold value at 2 years and 2 mm at 4 years), could be found in our study in 25% (15 of 60) at 2 years and in 10% (6 of 60) at 4 years.
There are several explanations for the high restabilisation rate between years 2 and 4: one might be the phenomenon of secondary stabilisation, described as a specific migration pattern with early onset and subsequent stabilisation, first found in stems [13]. Stoeckl et al. discuss a methodological error in EBRA [18]. The reduction of migration speed after year 1 and the higher rate of wear within the first year can also contribute to that effect.
We found discrepancies in radiological loosening rates at 2 years with 25% radiologically loose cups compared to 10% radiologically loose cups at 4 years. In order to avoid mistaking clinically stable cups for loose ones we made the approach to calculate an adequate threshold value for radiological loosening at 2 years. We performed an ROC curve analysis (Fig. 1) to determine the optimal threshold value: in our study, a cut-off value of 1.2 mm at 2 years seems to be appropriate for the prediction of loosening for the Duraloc press-fit cup (AUC = 0.96). Compared to 1 mm as the cut-off value the sensitivity of 100% is equal but the specificity of 89% instead of 76% is higher. Using this threshold value, only 18% (11 of 60) of implants would be defined as radiologically loose at 2 years.
Investigations have been made in the past to analyse whether cup size of acetabular components affects their migration behaviour. No correlation was found by Stöckl et al. [17]; another author detected consistently more migration of smaller cup diameters [5]. Takatori [19], however, described a significant correlation between increased cup size and the distance of migration. Our sophisticated analyses confirm the finding of Takatori, since large cup diameters (p = 0.029 at 4 years, Mann-Whitney U test) are associated with increased migration (Table 2). We assume that the soft bone of the spongiosa ring at large diameters, offers a major motion surface that might result in increased migration over time.
In our study we made an effort to evaluate the polyethylene wear rate. Significantly higher wear rates were found in male patients (Table 3). Our results confirm observations of previous investigations, where high wear rates were associated with male gender [9]. Vernois et al. found some correlation between wear and age [20], but we could not confirm this observation.
We conclude that the acetabular components used in this study provide a good clinical outcome. Radiologically, the EBRA method showed a high rate of loosening at 2 years, but 90% of implants were stable at 4 years. In view of this tendency, an acceptable long-term outcome appears to be ensured. In our study, a cut-off value of 1.2 mm at 2 years seems to be more practicable for the prediction of loosening for the Duraloc press-fit cup.
References
- 1.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 2.Girard J, Laffargue P, Decoulx J, Migaud H. Reliability of porous coating metal-backed cups: advantages and adverse effect of a posterior elevated rim polyethylene liner (in French) Rev Chir Orthop Reparatrice Appar Mot. 2005;91:432–438. doi: 10.1016/s0035-1040(05)84360-0. [DOI] [PubMed] [Google Scholar]
- 3.Grobler GP, Learmonth ID, Bernstein BP, Dower BJ. Ten-year results of a press-fit, porous-coated acetabular component. J Bone Joint Surg Br. 2005;87:786–789. doi: 10.1302/0301-620X.87B6.15335. [DOI] [PubMed] [Google Scholar]
- 4.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 5.Hintermann B, Morscher EW. Total hip replacement with solid autologous femoral head graft for hip dysplasia. Arch Orthop Trauma Surg. 1995;114:137–144. doi: 10.1007/BF00443387. [DOI] [PubMed] [Google Scholar]
- 6.Ilchmann T, Franzen H, Mjoberg B, Wingstrand H. Measurement accuracy in acetabular cup migration. A comparison of four radiologic methods versus roentgen stereophotogrammetric analysis. J Arthroplasty. 1992;7:121–127. doi: 10.1016/0883-5403(92)90004-A. [DOI] [PubMed] [Google Scholar]
- 7.Ilchmann T, Freeman MA, Mjoberg B. Accuracy of the Nunn method in measuring acetabular cup migration. Ups J Med Sci. 1992;97:67–68. doi: 10.3109/03009739209179283. [DOI] [PubMed] [Google Scholar]
- 8.Kim YH. Cementless total hip arthroplasty with a close proximal fit and short tapered distal stem (third-generation) prosthesis. J Arthroplasty. 2002;17:841–850. doi: 10.1054/arth.2002.33555. [DOI] [PubMed] [Google Scholar]
- 9.Kim YH, Oh SH, Kim JS. Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg Am. 2003;85:109–114. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 10.Krismer M, Fischer M, Mayrhofer P, Stockl F, Bittner C, Trojer C, Stockl B. A prospective study of the migration of two acetabular components. PCA versus RM cups. Int Orthop. 1994;18:23–28. doi: 10.1007/BF00180174. [DOI] [PubMed] [Google Scholar]
- 11.Krismer M, Bauer R, Tschupik J, Mayrhofer P. EBRA: a method to measure migration of acetabular components. J Biomech. 1995;28:1225–1236. doi: 10.1016/0021-9290(94)00177-6. [DOI] [PubMed] [Google Scholar]
- 12.Krismer M, Stockl B, Fischer M, Bauer R, Mayrhofer P, Ogon M. Early migration predicts late aseptic failure of hip sockets. J Bone Joint Surg Br. 1996;78:422–426. [PubMed] [Google Scholar]
- 13.Krismer M, Biedermann R, Stöckl B, Fischer M, Bauer R, Haid C. The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA. J Bone Joint Surg Br. 1999;81:273–280. doi: 10.1302/0301-620X.81B2.8840. [DOI] [PubMed] [Google Scholar]
- 14.Mjoberg B. Fixation and loosening of hip prostheses. A review. Acta Orthop Scand. 1991;62:500–508. doi: 10.3109/17453679108996658. [DOI] [PubMed] [Google Scholar]
- 15.Phillips NJ, Stockley I, Wilkinson JM. Direct plain radiographic methods versus EBRA-Digital for measuring implant migration after total hip arthroplasty. J Arthroplasty. 2002;17:917–925. doi: 10.1054/arth.2002.34529. [DOI] [PubMed] [Google Scholar]
- 16.Stocks GW, Freeman MAR, Evans SJW. Acetabular cup migration. Prediction of aseptic loosening. J Bone Joint Surg Br. 1995;77:853–861. [PubMed] [Google Scholar]
- 17.Stöckl B, Sandow M, Krismer M, Biedermann R, Wimmer C, Frischhut B. Migration of the Duraloc cup at two years. J Bone Joint Surg Br. 1999;81:51–53. doi: 10.1302/0301-620X.81B1.9036. [DOI] [PubMed] [Google Scholar]
- 18.Stoeckl B, Brabec E, Wanner S, Krismer M, Biedermann R. Radiographic evaluation of the Duraloc cup after 4 years. Int Orthop. 2005;29:14–17. doi: 10.1007/s00264-004-0600-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takatori Y, Ninomiya S, Umeyama T, Yamamoto M, Moro T, Nakamura K. Bipolar revision arthroplasty for failed threaded acetabular components: radiographic evaluation of cup migration. J Orthop Sci. 2002;7:467–471. doi: 10.1007/s007760200081. [DOI] [PubMed] [Google Scholar]
- 20.Vernois J, Gabrion A, Havet E, Gaullier O, Mertl P. The cementless Duraloc acetabular component: 100 cases assessed after a minimum five year follow-up (in French) Rev Chir Orthop Reparatrice Appar Mot. 2004;90:434–441. doi: 10.1016/s0035-1040(04)70170-1. [DOI] [PubMed] [Google Scholar]
- 21.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Wilkinson JM, Hamer AJ, Elson RA, Stockley I, Eastell R. Precision of EBRA-Digital software for monitoring implant migration after total hip arthroplasty. J Arthroplasty. 2002;17:910–916. doi: 10.1054/arth.2002.34530. [DOI] [PubMed] [Google Scholar]