Abstract
Fractures of the talar body present a great challenge to surgeons due to their rarity and high incidence of sequelae. This study reports the medium-term results of displaced fractures of the talar body treated by internal fixation. Nineteen patients (13 M, 6 F, mean age 31) with talar body fractures were studied retrospectively to assess outcome after operative treatment. The fractures were classified as coronal (11), sagittal (6) and crush fractures (2). Six patients sustained open fractures and two had associated talar neck fractures. Average follow-up was 26 months (range: 18–43). Clinical outcome based on American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot scoring was excellent function in four patients, good in six, fair in four and poor in five. Early complications included two superficial wound infections, one partial wound dehiscence, one instance of skin necrosis and one deep infection. Other complications included delayed union in one, avascular necrosis in seven and malunion in one patient. Talar injuries are serious because they can compromise motion of the foot and ankle and result in severe disability. Crush fractures of the talar body and those associated with open injuries and talar neck fractures are associated with a less favourable outcome.
Résumé
Les fractures du corps du talus sont difficiles à traiter pour les chirurgiens. Cette étude rapporte le traitement à moyen terme des fractures déplacées du talus par fixation interne. 19 patients (13 garçons, 6 filles d’un âge moyen de 31 ans). Les fractures ont été classées de la façon suivante : fractures coronales 11, fractures saggitales 6 et écrasement, fractures 2. Six patients présentaient une fracture ouverte et deux une fracture du col. Le suivi moyen a été de 26 mois (de 18 à 43 mois). L’évaluation clinique des patients a été réalisée selon le score de la Foot & Ankle Society (AOFAS). Le résultat au niveau de la cheville et de l’arrière pied est excellent sur le plan fonctionnel chez 4 patients, bon chez 6 patients, moyen chez 4 patients et mauvais chez 5 patients. Les complications précoces ont été les suivantes : deux infections superficielles, une nécrose cutanée, et une infection profonde. Les autres complications ont été les suivantes : retard de consolidation chez un patient, nécrose avasculaire chez sept patients et pseudarthrose chez un patient. Les traumatismes du talus sont des lésions relativement sérieuses et peuvent compromettre la mobilité du pied et de la cheville. Lorsqu’il y a association d’une fracture écrasement et de lésions cutanées. De telles fractures entraînent souvent un mauvais résultat fonctionnel.
Introduction
Fractures of the talar body are highly uncommon. Fractures of the talar body, although constituting one of the rare injuries of the body, present a very grave prognosis. They present a greater risk for avascular necrosis than talar neck fractures. They constitute less than 1% of all fractures and 13–23% of talus fractures [2, 9]. They usually follow high-energy injuries and are therefore associated with considerable soft tissue damage. Furthermore, fractures involving the talar body can be difficult to visualise adequately because of the shape of the tibiotalar articulation and the overhang of the anterior and posterior tibial plafond.
Generally, it is well-protected by the tibial plafond superiorly and malleoli on either side. Sneppen et al. found that only certain non-physical forces, e.g. pronounced caudal compression, force during pronation and especially supination trauma, will injure the body of the talus. They found that with regard to talar body fractures, a medial site fracture was typical of supination trauma (compression or shear type), whereas a lateral site fracture was typical of pronation or pronation-external rotation trauma (compression fracture) [18]. The other common mechanism of injury resulting in fracture of the body of the talus is a fall from a height, producing an axial compression of the talus between the tibial plafond and the calcaneus.
These fractures are often associated with other ankle, foot and skeletal injuries which complicate the treatment. Since fastening of seat belts has become mandatory, more patients involved in high-velocity motor vehicle accidents survive, which increases the number of injuries to the distal extremities.
Only few studies in the past have reported on the talar body fractures detailing the results of their management as compared to the more common fractures of the talar neck [6, 7]. Hence the aim of this study was to report the medium-term results of displaced fractures of the talar body treated by internal fixation.
Materials and methods
A retrospective study was performed to analyse the outcomes of patients with talar body fractures between February 1998 and January 2004. Those included in the study were treated by operative methods with a minimum follow-up of 18 months after the injury. The exclusion criteria were patients with an isolated talar neck fracture without talar body fracture, patients with an isolated posterior process fracture and those with solitary transchondral lesions. Nineteen patients who met the inclusion criteria were considered for this study. Six patients were female and 13 were male. The mean age was 31 years with a range of 21–68. Twelve fractures were to the right talus compared to seven on the left side. Seven patients were injured due to a fall, nine as a result of motor vehicle accident (MVA), two after motorcycle accidents and one patient was injured as a pedestrian in a MVA.
The talar body fractures were classified according to Boyd and Knight’s classification [3]. The surgical approach depended upon the fracture pattern and hence a single or combined approach was used. Medial malleolus osteotomy was also performed if a better exposure was needed. Cancellous screws (4 mm) and small Herbert screws were used according to the fracture pattern. Bone grafting was not performed in any cases.
Patients were kept non-weight-bearing by wearing an off-the-shelf fracture boot with early foot and ankle motion for 10–12 weeks, until radiographs and clinical examination revealed evidence of union. Anteroposterior, lateral and mortise radiographs were routinely made at 2 weeks, 6 weeks, 10–12 weeks and 6 months post-operatively. Additional radiography, computed tomography scans and magnetic resonance imaging were performed as often as needed.
Clinical results were evaluated using the clinical rating scale of the American Orthopaedic Foot & Ankle Society (AOFAS) (100 points total) [12]. The questionnaire assessed the level of pain, function and alignment. Patients were asked to rate pain on a scale of 0–40 points. Function was calculated as the total score of activity limitations (0–10), maximum walking distance (0–5), walking surface (0–5), gait abnormality (0–8), sagittal motion (0–8), hindfoot motion (0–6) and ankle-hindfoot stability (0–8). Alignment was rated from 0 to 10 points (good, fair, poor), giving a total score of 100 points. Excellent was defined as a score of 85–100, good as 75–84, fair as 70–74 and poor as less than 70 [12].
Post-traumatic arthritis was defined as a decreased joint space, juxta-articular osteophytes, subchondral sclerosis and/or subchondral cysts seen either on plain radiographs or on computed tomography scans. Osteonecrosis was documented as present or absent as seen on standard radiographs.
Results
The 19 patients who were evaluated in clinic following operative treatment constitute the cohort of this study. The type of talar body fractures according to Boyd and Knight [3] was as follows: 17 type I fractures, 11 coronal and 6 sagittal and 2 crush fractures. Six patients sustained open fractures: one type I, three were type II, one was type IIIA and one was type IIIB. Furthermore, two patients had associated talar neck fractures: one Hawkins type I and another Hawkins type II. The average time from injury to surgery was 2 days with seven patients undergoing surgery less than 24 h after sustaining the fracture; the range was 9 h to 13 days. During surgery, the medial approach was used in six procedures, the lateral approach was used in three and a combined approach was performed in ten. A medial osteotomy was performed in six patients for better exposure of the fracture. No fibular osteotomies were performed.
The average duration of follow-up was 26 months (range: 18–43). According to the AOFAS rating system, four patients had an excellent function, six had good function, four had fair function and five had poor function. The average total score was 68.6 (range: 44–94). (Table 1) Early complications occurred in five patients and included two superficial wound infections, one partial wound dehiscence, one instance of skin necrosis and one deep infection. Late complications were also assessed. One patient had delayed union and another had malunion. Both these patients had a fair outcome. Seven patients suffered from avascular necrosis (AVN); two of these were in patients who had suffered neck and body fractures while the other five were in fractures that only involved the body. In five of the cases of AVN, collapse occurred. Additionally, 11 patients suffered from subsequent ankle arthritis while 6 patients had subtalar arthritis. Fractures with open injuries had a high incidence of complications. Among the six patients (three coronal, one sagittal, two crush fractures) with open fractures, avascular necrosis developed in five, superficial wound necrosis in two, deep infection in one, arthritis of the ankle joint in six and subtalar joint in five. The clinical outcome was poor in four patients and fair in two.
Table 1.
Average American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot score at the last follow-up
| Score | |
|---|---|
| Pain | 27.4 |
| Activity limitations | 6.9 |
| Walking distance | 3.2 |
| Walking surface | 3.0 |
| Gait abnormality | 4.4 |
| Sagittal motion | 5.3 |
| Hindfoot motion | 3.5 |
| Ankle-hindfoot stability | 8 |
| Alignment | 6.9 |
Total score: 68.6 (range: 44–94)
Two patients (both coronal fractures) with associated talar neck fractures had a poor outcome. One patient (Hawkins type I) had an open injury (grade II) and developed AVN along with superficial wound infection. The other patient (Hawkins type II) had skin necrosis and AVN. Radiographs demonstrated osteoarthritic changes in both ankle and subtalar joints.
Among the various talar body fractures, two patients (both had open injuries, grade IIIA and IIIB) with crush fractures had a poor outcome. In the six patients with sagittal fractures (two open injuries, grade I and II), three patients had a good outcome, one excellent, one fair and one poor outcome. Of the 11 patients with coronal fractures (2 open injuries of grade II and 2 talar neck fractures), 3 patients had excellent outcome, 3 good, 3 fair and 2 poor outcome. Radiographs of a patient with a coronal fracture are depicted in Figs. 1, 2 and 3.
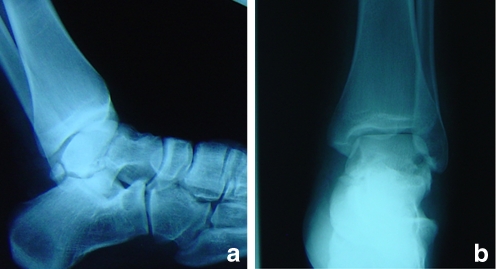
Fig. 1.
Lateral (a) and anteroposterior (AP) (b) radiographs of a patient with fractures of the talar head and lateral process of the posterior tubercle. Anterior talofibular ligament was also disrupted
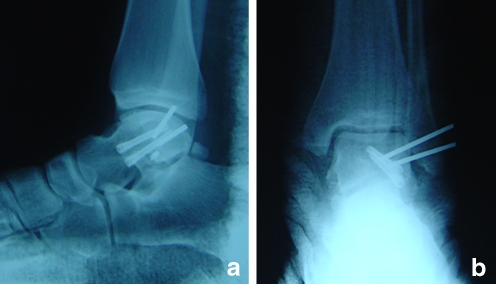
Fig. 2.
Immediate post-operative lateral (a) and AP (b) films show internal fixation with Herbert screws and repair of anterior talofibular ligament
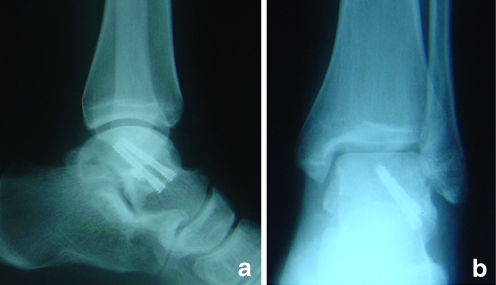
Fig. 3.
Lateral (a) and AP (b) radiographs following 23 months of follow-up. The patient had an excellent clinical outcome
Discussion
Talus is derived from the French word talo which means ankle; its origin is from Greek and Roman gambling games. The Romans used dice that were the heel bones of horses called taxillus. Greeks, however, used the second vertebrae of sheep, which they called the astragalus. Both of these derivations eventually became associated with the foot bone known today as the talus [8]. In 1952, Coltart described the largest series ever reported of injuries of the talus that he collected from the Royal Air Force during World War II, which included 15 cases of fracture of the talar body [4]. A literature search reveals that in many of the previous studies, the majority of patients were treated nonoperatively [5, 11], and talar body fractures were not distinguished from other fractures of the talus [6, 7].
Injuries to the talus are serious because this bone is the critical link between the subtalar, transverse tarsal and ankle joint complex. The variety of coupled actions occurring from the motion of this bone or surrounding bones permits the effortless flexibility of the hindfoot and midfoot. If the talus is damaged, the universal combined motion of the foot and ankle becomes compromised, and severe disability can result [17]. Inokuchi et al. differentiated talar neck and body fractures by critically analysing the inferior surface fracture line. They defined a talar body fracture as one in which the fracture line on the inferior surface extends into the subtalar joint [10].
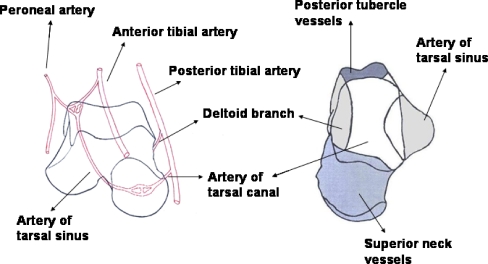
The body of the talus is supplied by vessels that enter through five surfaces: the superior surface of the talar neck, the anterolateral surface of the talar body, the inferior surface of the talar neck, the medial surface of the talar body via the deltoid ligament and the posterior tubercle [16]. The artery of the tarsal canal is the most significant supply of blood to the body of the talus. It supplies the middle one-half to two-thirds directly and through anastomosis potentially supplies the entire body. (Fig. 4). Its largest branches enter through the inferior surface of the neck. The medial one-third of the body is directly supplied by the deltoid branch which enters from the medial surface of the talus and supplies even more due to anastomosis. The artery of the tarsal sinus branches and then enters the anterolateral body and supplies the lateral one-eighth to one-half directly. The superior neck vessels also make a minor contribution. The system of vessels over the posterior tubercles mostly supplies the tubercle itself [14]. The vascular supply varies among the regional sections of the talus with the anterolateral surface of the talar body and the posterior tubercles of the talus being relatively avascular [15].
Fig. 4.
The blood supply to the various regions of the talus. The artery of the tarsal canal provides the predominant blood supply to the talar body
Boyd and Knight have classified talar body fractures according to the plane of the fracture line. A type I fracture is a coronal or sagittal shear fracture, compared to a type II fracture which occurs in the horizontal plane [3]. The most common mechanism of injury resulting in a shearing-type talar body fracture is a fall from a height resulting in axial loading. Nondisplaced or minimally displaced shearing-type fractures of the talar body can be sometimes difficult to recognise on the plain radiographs. A delay in diagnosis and treatment may be associated with an increased risk of osteonecrosis, malunion, secondary osteoarthritis and other complications. Abrahams et al. reported on two cases of nondisplaced shear fractures of the talar body that were not recognised initially and recommended that these fractures should be suspected in patients with a history of axial loading injury and diffuse ankle swelling when no other fracture, particularly calcaneal, is identified on radiographs [1].
Displaced talar body fractures often result in significant morbidity. Vallier et al., reporting on radiographic findings of 26 talar body fractures with a minimum follow-up of 1 year, noted a 38% incidence of AVN, 65% incidence of post-traumatic tibiotalar arthritis and 34% incidence of post-traumatic subtalar arthritis. Worse outcomes were noted in association with comminuted fractures, associated talar neck fractures and open fractures [20]. Lindvall et al., in 2004, reported on 26 isolated talar neck and body fractures with a minimum follow-up of 48 months and found a 50% incidence of AVN and 100% incidence of post-traumatic arthritis. Timing of fixation did not appear to affect the outcome, union or prevalence of AVN in the later study because the fractures that were stabilised within 6 h did not have a lower incidence of AVN than those stabilised after 6 h [13]. Both of these studies concluded that patients with these injuries should be counselled on the long-term complications and that arthritis is an expected outcome in displaced talar body fractures despite accurate reduction with stable fixation.
Sneppen et al. (1997) reviewed 51 patients with talar body fractures. In cases in which significant talar compression occurred they found that 50% of patients had ankle osteoarthritis; if the talus exhibited a shearing pattern of injury, the incidence of post-traumatic arthritis in both the ankle and subtalar joints was 41%, with a further 24% of patients having osteoarthritis in either ankle or subtalar joints. They concluded that results in talar body fractures are directly related to the severity of the initial injury and emphasised that if subluxation and articular damage to the subtalar and talotibial joints occurred at the initial injury, long-term prognosis is poor [18].
Talar body fractures have been associated with a high incidence of complications including osteonecrosis, malunion, nonunion, secondary osteoarthritis, subtalar bony ankylosis, skin infection and skin necrosis. The incidence and severity of these complications appear to relate to several factors including the intrinsic talar vascular supply, the initial extent of displacement, the presence of associated dislocation and the adequacy of reduction [1]. This associated with the fact that more weight per area is borne by the talar dome than any other joint in the body means that post-traumatic arthritis and long-standing disability are frequent complications to fractures of the talus [14].
Avascular necrosis of the posterior fragment of the talar body or the superior fragment in the case of a horizontal fracture is particularly common [19].
Usually the fracture pattern and location will determine the choice of surgical approach [20]. However, the shapes of the tibiotalar articulation and the overhang of the posterior tibial plafond sometimes limit access to the posterior parts of the talus. Distraction of the tibiotalar joint can be used for reconstructive procedures but is risky in the acutely injured situation. When necessary, a medial or lateral osteotomy should be performed to provide exposure to all aspects of the talar body.
There are a few limitations in this study. First, as the study was retrospective in nature, the results were derived from the charts and radiographs. Second, no meaningful statistical derivations were obtained because of the small study sample. Further multi-centre prospective studies are needed to provide better and more definite conclusions on the relationship between type of fracture, open injures and other factors with the clinical outcome.
In conclusion, talar body fractures are unique and very challenging injuries for the surgeon. Crush fractures of the talar body and those associated with open injuries and talar neck fractures are associated with a less favourable outcome.
Footnotes
The authors received nothing of value related to the subject of this article.
References
- 1.Abrahams TG, Gallup L, Avery FL. Nondisplaced shearing-type talar body fractures. Ann Emerg Med. 1994;23(4):891–893. doi: 10.1016/S0196-0644(94)70331-0. [DOI] [PubMed] [Google Scholar]
- 2.Alvarez RG. Talar neck fractures. In: Myerson M, editor. Current therapy in foot and ankle surgery. St. Louis: Mosby; 1993. pp. 243–248. [Google Scholar]
- 3.Boyd HB, Knight RA. Fractures of the astragalus. South Med J. 1942;35:160–167. [Google Scholar]
- 4.Coltart WD. Aviator’s astragalus. J Bone Joint Surg Br. 1952;34:545–566. doi: 10.1302/0301-620X.34B4.545. [DOI] [PubMed] [Google Scholar]
- 5.Elgafy H, Ebraheim NA, Tile M, Stephen D, Kase J. Fractures of the talus: experience of two level 1 trauma centers. Foot Ankle Int. 2000;21:1023–1029. doi: 10.1177/107110070002101208. [DOI] [PubMed] [Google Scholar]
- 6.Frawley PA, Hart JA, Young DA. Treatment outcome of major fractures of the talus. Foot Ankle Int. 1995;16:339–345. doi: 10.1177/107110079501600605. [DOI] [PubMed] [Google Scholar]
- 7.Grob D, Simpson LA, Weber BG, Bray T. Operative treatment of displaced talus fractures. Clin Orthop. 1985;199:88–96. [PubMed] [Google Scholar]
- 8.Haliburton RA, Sullivan CR, Kelly PJ, Peterson LF. The extra-osseous and intra-osseous blood supply of the talus. J Bone Joint Surg Am. 1958;40(5):1115–1120. [PubMed] [Google Scholar]
- 9.Higgins TF, Baumgaertner MR. Diagnosis and treatment of fractures of the talus: a comprehensive review of the literature. Foot Ankle Int. 1999;20:595–605. doi: 10.1177/107110079902000911. [DOI] [PubMed] [Google Scholar]
- 10.Inokuchi S, Ogawa K, Usami N. Classification of fractures of the talus: clear differentiation between neck and body fractures. Foot Ankle Int. 1996;17(12):748–750. doi: 10.1177/107110079601701206. [DOI] [PubMed] [Google Scholar]
- 11.Kenwright J, Taylor RG. Major injuries of the talus. J Bone Joint Surg Br. 1970;52:36–48. [PubMed] [Google Scholar]
- 12.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15(7):349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 13.Lindvall E, Haidukewych G, DiPasquale T, Herscovici D, Jr, Sanders R. Open reduction and stable fixation of isolated, displaced talar neck and body fractures. J Bone Joint Surg Am. 2004;86(10):2229–2234. doi: 10.2106/00004623-200410000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Metzger MJ, Levin JS, Clancy JT. Talar neck fractures and rates of avascular necrosis. J Foot Ankle Surg. 1999;38(2):154–162. doi: 10.1016/s1067-2516(99)80030-1. [DOI] [PubMed] [Google Scholar]
- 15.Pajenda G, Vecsei V, Reddy B, Heinz T. Treatment of talar neck fractures: clinical results of 50 patients. J Foot Ankle Surg. 2000;39(6):365–375. doi: 10.1016/S1067-2516(00)80072-1. [DOI] [PubMed] [Google Scholar]
- 16.Sanders R. Fractures and fracture: dislocations of the talus. In: Coughlin MJ, Mann RA, Saltzman CL, editors. Surgery of the foot and ankle. 8. Philadelphia: Mosby Elsevier; 2007. pp. 2076–2132. [Google Scholar]
- 17.Sarrafian SK. Anatomy of the foot and ankle: descriptive, topographic, functional. Philadelphia: Lippincott; 1983. pp. 400–407. [Google Scholar]
- 18.Sneppen O, Christensen SB, Krogsoe O, Lorentzen J. Fracture of the body of the talus. Acta Orthop Scand. 1977;48:317–324. doi: 10.3109/17453677708988775. [DOI] [PubMed] [Google Scholar]
- 19.Thordarson DB. Talar body fractures. Orthop Clin North Am. 2001;32(1):65–77. doi: 10.1016/S0030-5898(05)70194-2. [DOI] [PubMed] [Google Scholar]
- 20.Vallier HA, Nork SE, Benirschke SK, Sangeorzan BJ. Surgical treatment of talar body fractures. J Bone Joint Surg Am. 2003;85(9):1716–1724. doi: 10.2106/00004623-200309000-00010. [DOI] [PubMed] [Google Scholar]