Abstract
A prospective study is presented of 551 hip fractures treated with the ITST (inter-trochanteric/sub-trochanteric) nail with a minimum mandatory follow-up of 1 year. Of the patients 73% were female, the rest male. The average age was 82.8 years. Fractures were classified according to the AO system, the most common sub-type recorded being the A2 (56%). Clinical and radiographic controls were performed at 1, 3, 6 and 12 months. The system allowed early mobilisation and walking in the majority of our patients, along with fracture consolidation in an acceptable time (12 weeks on average). There were technical complications during the operation in 10.5% of the cases, complications in the immediate postoperative period in 22.3% and late complications were detected in 5.1% of patients at 12 months. The ability to recover previous walking ability was 58%. The ITST nail emerges as a good system of osteosynthesis for fractures of the trochanteric region of the femur, allowing early weight-bearing, which favours bone consolidation. The surgical technique is not complex, the number of complications recorded is acceptable and the overall results obtained are comparable and even superior to those obtained with other osteosynthesis systems available for treatment of this type of fracture.
Keywords: Hip, Fracture, Osteosynthesis
Résumé
Nous présentons une étude prospective de 551 fractures de la hanche traitées par le clou ITST avec un minimum de suivi de 1 an. 73% des patients étaient des femmes, les autres patients des hommes. L’âge moyen était de 82.8 ans. Les fractures ont été classées selon le système AO, le type le plus fréquent étant le type A2 (56%). L’examen clinique et radiographique a été réalisé à 1, 3, 6 et 12 mois. Ce système d’ostéosynthèse permet une mobilisation précoce et la marche pour une grande majorité des patients, avec un temps de consolidation acceptable de 12 semaines en moyenne. Les complications techniques durant l’intervention ont été de 10.5%, post opératoires immédiat de 22.3% et tardives de 5.1% à 12 mois. Les patients ont récupéré une marche identique à celle qu’ils avaient avant l’intervention dans 58% des cas. Le clou ITST nous apparaît comme un bon système d’ostéosynthèse pour ces fractures de la région trochantérienne, permettant un appui précoce avec une bonne consolidation osseuse. La technique chirurgicale est simple, le nombre de complications rapportées est acceptable, les résultats obtenus sont comparables ou souvent supérieurs à ceux obtenus avec d’autres systèmes d’ostéosynthèse pour le même type de fracture.
Introduction
Nowadays trochanteric fractures of the femur constitute a very common pathology in the elderly with an incidence that increases every year [1, 10]. The goals of treatment are early weight-bearing and patients’ recovery of previous function [4, 14]. These fractures constitute a social and economic problem, particularly when progressive ageing of the population is predicted in the foreseeable future, allied to a greater demand for quality of life of these patients [5, 21].
Different osteosynthesis systems exist for the treatment of fractures of the trochanteric region of the femur, those most frequently used at present being the sliding plate-screw systems and closed intramedullary nailing. Stable fractures of the region do not usually present problems of union, irrespective of the fixation method used [11, 17], while in unstable and comminuted fractures, which represent most of the cases in our area, second generation intramedullary nails achieve stable fixation, which allows early weight-bearing and rehabilitation [1, 2, 8, 9, 13, 14, 18, 19].
In principle, the advantages of opting for an intramedullary system of osteosynthesis are, firstly, that both the reduction of the fracture and the insertion of the implant are performed using a closed technique, which (at least theoretically) reduces the operating time and blood loss, without interfering with the formation of the external callus; secondly, an intramedullary device provides a more effective counteraction to the gluteus and psoas muscles, and, finally, the intramedullary distribution of loads more proximal to the calcar, reduces medial torque [18].
A new system of intramedullary osteosynthesis that does not require reaming has been recently introduced, the ITST nail, which has biomechanical modifications compared to existing systems, in an attempt to minimise complications of a technical nature. This study presents the results of our experience with this nail in the treatment of peri- and intertrochanteric fractures of the femur.
Materials and methods
We present a prospective study of 551 hip fractures treated with the ITST nail in the Orthopaedic Surgery and Traumatology Services of the Miguel Servet University Hospital (Zaragoza) with mandatory follow-up of at least 1 year: the fractures were classified according to the AO system [15], because in our opinion it is the best classification to identify a fracture’s instability [6]. Clinical and radiographic controls were performed at the time of admission and in the postoperative follow-up at 1, 3, 6 and 12 months, the corresponding evaluation protocol being completed at the same time.
In the documented protocol for each case, details of the basic situation of the patient were noted (age, sex, concomitant illnesses, previous walking ability), along with the characteristics of the fracture, details of the surgical procedure and of the immediately postoperative radiological examinations. Early and late intra- and postoperative complications were also recorded, as were the final clinical and radiographic results achieved after a follow-up of 12 months.
In the postoperative period, transfusion requirements for each case, hospitalisation time, time to weght-bearing and the time necessary for the consolidation of the fracture were all reviewed. In terms of results, recovery of the previous level of walking ability, deformity in the affected limb and changes in the patients’ mental function compared to the the pre-fracture situation were all studied. A database was created from the information obtained, and statistical analysis of the results was performed.
The operation was performed with the patient in the dorsal decubitus position on the orthopaedic traction table and with the affected limb slightly adducted, to facilitate the insertion of the nail. In all cases antithrombotic prophylaxis was given, using low molecular weight heparin (Enoxaparin), and antibiotic prophylaxis was provided.
The fracture was reduced under radioscopic control. A Kirschner wire was introduced via a small incision approximately 3 cm proximal to the greater trochanter and, using a reamer of 17 mm in diameter, the proximal part of the femoral diaphysis was reamed by hand through this. Subsequently, the selected implant was manually introduced into the medullary canal, with no need for reaming, using an insertion device, through which, using a guide needle, a cervico-cephalic screw was placed angled at 130°. Finally, there is the possibility of distal interlocking through the same device, with two screws, one dynamic and the other static. Implants are available in steel, and for the right and left lower limbs. They are a short nail (standard) of 180 mm and a long nail (300–500 mm); the short nail was used in all of the cases reviewed. The proximal diameter is 17 mm and distal diameter 10–15 mm.
Results
The average age of our patients was 82.8 years, with 87% of the patients over 70. Of the patients, 73% were female, the rest male. The surgical procedures were performed from 2002–2006.
The most frequent cause of fracture was an accidental fall, as was the case in 77.4% of the subjects. There were 21 cases (3.8%) of pathological fractures.
Fractures were classified according to the AO system [15], the most frequent type encountered being the A2 (55.5%), followed by A1 (22.3%) and A3 (22.1%). The most frequent sub-types were A2.2 and A2.3, which represented 19.4 and 24.0% of the total, respectively. The degree of osteoporosis was recorded, using the Singh scale [20], with 78.9% of all cases in levels III and IV.
The average perioperative period was 3.8 days. Of the patients, 28% were operated upon within the first 48 h, 38.2% at 3–4 days, 20.5% at 5–7 days and the remaining 13.1% after more than a week. General anaesthesia was used in 18.5% of the patients and spinal in the rest. The ASA risk was II or III for 84.6% of the patients. The average length of the operation recorded was 40.1 min. In all cases closed reduction was achieved, and the nail was inserted with no need to ream the femoral diaphysis. In 40.9% of cases transfusion of packed red blood cells was necessary during the 1st postoperative week, the average requirement being 1.6 units.
The average time required for consolidation was 12 weeks. There were 25 cases (4.5%) of delayed consolidation, but no pseudoarthroses.
The nail diameter used was 10 mm in 85.3% of the cases, 11 mm in 11.1% and 12 mm in 3.5%. The length of the cervico-cephalic screw varied from 85 and 115 mm, the most commonly used being the 95 and 100 mm lengths in 27.3% and 24.0% of cases, respectively. Distal locking was performed in all but two of the cases, two screws being placed in 11.3% of the patients, the dynamic screw alone in 79.8% and only the static screw in 9.1% of cases.
The fracture reduction achieved in the operating theatre was considered correct in 86.4% of patients (less than 10° of varus/valgus compared to the angulation of the healthy femur). Of the reductions, 5.2% were varus and 8.3% were valgus. Placement of the cervical screw was decided by anteroposterior and axial views, and the most common site was in the mediomedial quadrant, which accounted for 53.6% of the cases, followed by the mediocaudal and posterocaudal with 19.6% and 10%, respectively. The rest of the cases placed in other quadrants owing to technical difficulties. The existence of an average shortening of the affected limb of 5 mm was observed in 8.7% of the cases.
General complications occurring in the immediate postoperative period are listed in Table 1.
Table 1.
Miscellaneous complications
| Miscellaneous complications | ||
|---|---|---|
| Cases | % | |
| Decubitus ulcer | 20 | 3.6 |
| Acute postoperative mental confusion | 63 | 11.3 |
| GI haemorrhage | 4 | 0.7 |
| Urinary infection | 30 | 5.4 |
| Pulmonary embolism | 5 | 0.9 |
| Acute renal insufficiency | 3 | 0.5 |
| Deep vein thrombosis | 8 | 1.4 |
Local complications of a technical nature are reflected in Table 2. There were technical complications during the operation in 10.5% of the cases, although it should be noted that the majority arose in the early cases and the frequency diminished with the learning curve and with improvements in instrumentation. There were complications in the immediate postoperative period in 22.3% of cases and late complications were detected in 5.1% of patients at 1 year.
Table 2.
Local complications
| Cases | % | |
|---|---|---|
| Early local complications | ||
| Fracture of greater trochanter at nail insertions | 23 | 4.1 |
| Seroma | 80 | 14.5 |
| Haematoma | 59 | 10.7 |
| Superficial infection | 9 | 1.6 |
| Deep infection | 3 | 0.5 |
| Late local complications | ||
| “Cut out off” | 8 | 1.4 |
| Secondary varus (>10%) | 22 | 4.0 |
| Muscle pain (due to point effect) | 27 | 4.9 |
| Calcifications in apex of trochanter | 27 | 5.4 |
| Diaphyseal fractures (beneath the nail) | 4 | 0.7 |
The most frequent complications were seromas and haematomas of the surgical wound, which resolved satisfactorily in all cases. The cases of superficial or deep infection also resolved favourably, once the appropriate antibiotic treatment was instituted. No breakages or failures due to implant fatigue were seen. Other complications observed, such as fracture of the greater trochanter during insertion of the nail or secondary varus, were treated conservatively, since they did not evoke clinical consequences for the patients in whom they occurred. Of the patients 4.9% presented with pain in the thigh due to the nail point effect.
Reoperation was necessary in 21 patients (3.8%) due to technical complications. All of them presented unstable fractures, corresponding to AO groups A2 and A3. Of these, there were four cases of poor reduction in the intraoperative radiological control, five cases of rotational defects of the limb, eight cases of intra-articular protrusion of the screws and four diaphyseal fractures beneath the tail of the implant due to new trauma following insertion of the nail. In the cases of poor reduction an incorrect placement of the cephalic screw was observed, as a result of which the implant was removed, a new closed reduction was performed and a new nail was inserted, with good subsequent progress of the patient. In the cases of malrotation, replacing the distal screws was sufficient to solve the problem. The cases of cut-out were revised with the removal of the ITST and a partial hip arthroplasty with a long stem. The patients that suffered diaphyseal fracture were treated with a long ITST nail.
Attempts to seat the patient were initiated in the first 48 h after surgery and succeeded with good tolerance on average at 3.4 days. Patients remained hospitalised for an average of 12.8 days. They were encouraged to begin assisted weight-bearing with crutches or a frame during the 1st postoperative week, and 40.4% of patients succeeded, while the figure for the 2nd week was 54.7% and 65.2% during the 3rd week.
The preoperative situation of the patients in terms of physical condition and walking ability, psychological state and ability to cope with everyday activities is shown in Table 3. The patients’ recovery after suffering the fracture and then surgery was also evaluated. Fifty-eight percent recovered their previous walking ability, while the other 42% suffered some degree of deterioration of this ability, mostly going from unaided walking to the use of one stick.
Table 3.
Patients’s recovery of previous function
| Patients’ recovery of previous function | |
|---|---|
| % | |
| a) Physical state | |
| Recovery | 58 |
| No recovery | 42 |
| b) Mental state | |
| Recovery | 85.3 |
| No recovery | 14.6 |
| c) Handling of everyday tasks | |
| Recovery | 68.2 |
| No recovery | 31.7 |
The overall mortality of the process was 18.87% (104 patients). Of the deaths, 5.62% occurred while in hospital, and the remaining 13.25% during the 12-month follow-up for reasons unrelated to surgery.
Discussion
In our experience, peri-trochanteric fractures in the elderly are in the majority of the cases unstable and comminuted; according to other authors [1, 2, 8, 9, 13, 14], the intramedullary nail seems to us the best method of treatment because it achieves more stability, produces less slide and is less aggressive than sliding plate-screw systems. Greater stability achieved by intramedullary systems allows early weight-bearing and, consequently, faster recovery of previous functional level of the patient.
The main biomechanical characteristics of the ITST nail include greater implant length (compared to the standard Gamma nail), anatomical valgus in the nail (5°), a flexible distal end that reduces the concentration of stresses to a minimum, no need for diaphyseal reaming and several options of distal and proximal locking (less or more aggressive). Figures 1 and 2 show the radiological result at 6 months of a peritrochanteric fracture treated with ITST with excellent patient progress.
Fig. 1.
Peritrochanteric fracture of the femur satisfactorily treated with ITST nail. Radiological control at 6 months
Fig. 2.
Peritrochanteric fracture of the femur satisfactorily treated with ITST nail. Radiological control at 6 months. Axial view
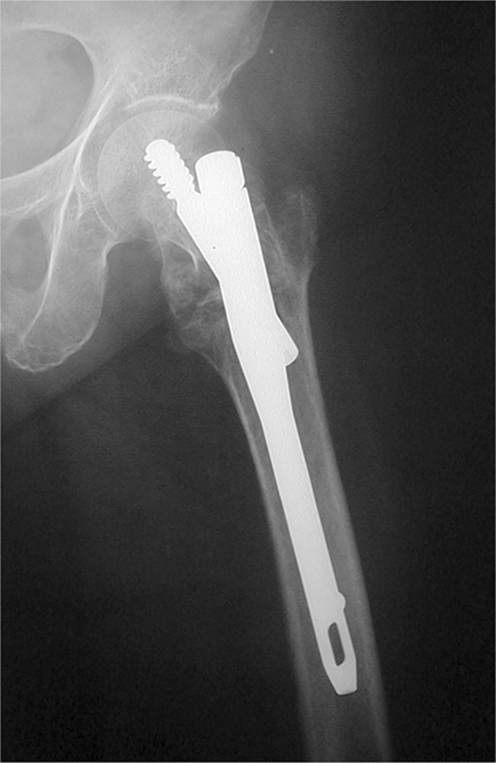
In our study, the incidence of technical complications represented a similar or lower rate than that published in different studies on the use of the Gamma or PFN nail [2, 3, 8, 9, 11–14, 16], which are the main alternative systems used in these fractures. Our cutout cases were related to poor reduction and superior placement of the screw. Revisions for inadequate reduction were also caused by deficiencies in the surgical procedure, and the rate is similar to other series [7, 9, 17], which vary between 2 and 12%. Figure 3 shows one of the cases of cut out reported.
Fig. 3.
Cut out that occurred in a patient with an ITST nail. AP view
With regard to the choice of implants, with experience, we have tended to use progressively smaller diameter nails and to increase the indications for dynamic set-up. No cases of implant breakage or fatigue were observed. We believe, as do other authors [1, 2, 8, 9, 13, 14, 22] that variables such as the period of hospitalisation, commencement of the sitting posture, early weight-bearing and other details are related to the pathology associated with advanced age and the type of fracture, rather than the technique itself. In our study the percentage of local and systemic complications and the ability to recover previously recorded function are similar to those encountered by other authors.
In view of the results obtained from this study, we believe that the ITST emerges as a valid option in the treatment of femoral fractures of the trochanteric region because of the simplicity and lack of aggressiveness of the surgical technique and the low level of complications of a technical nature that are encountered, which is particularly important bearing in mind that the large majority of patients that suffer this kind of fracture are elderly, and their general condition is frequently compromised.
References
- 1.Ahrengart L, Tornkvist H, Fornander P, Thorngren KG, Pasanen L, Wahlstrom P, Honkonen S, Lindgren U. A randomised study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop. 2002;401:209–222. doi: 10.1097/00003086-200208000-00024. [DOI] [PubMed] [Google Scholar]
- 2.Bellabarba C, Herscovivi D, Ricci WM. Percutaneous treatment of pertrochanteric fractures using the Gamma nail. Clin Orthop. 2000;375:30–42. doi: 10.1097/00003086-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Bridle SH, Patel AD, Bircher M, Calvert PT. Fixation of intertrochanteric fractures of the femur. A randomised prospective comparison of the gamma nail and the dynamic hip screw. J Bone Joint Surg. 1991;73B:330–334. doi: 10.1302/0301-620X.73B2.2005167. [DOI] [PubMed] [Google Scholar]
- 4.Calvert PT. The gamma nail: A significant advance or a passing fashion? J Bone Joint Surg. 1992;74B:329–331. doi: 10.1302/0301-620X.74B3.1587869. [DOI] [PubMed] [Google Scholar]
- 5.Cummings SR, Rubin SM, Black D. The future of the hip fractures in the United States: numbers, costs and potential effects of postmenopausal estrogen. Clin Orthop. 1990;252:163–166. [PubMed] [Google Scholar]
- 6.Fung W, Jonsson A, Buhren V, Bhandari M. Classifying intertrochanteric fractures of the proximal femur: does experience matter? Med Princ Pract. 2007;16(3):198–202. doi: 10.1159/000100390. [DOI] [PubMed] [Google Scholar]
- 7.Halder SC. The gamma nail for peritrochanteric fractures. J Bone Joint Surg. 1992;74B:340–344. doi: 10.1302/0301-620X.74B3.1587873. [DOI] [PubMed] [Google Scholar]
- 8.Hardy DC, Descamps PY, Krallis P, Fabeck L, Smets P, Bertens CL, Delince PE. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures. A prospective, randomised study of one hundred patients. J Bone Joint Surg. 1998;80A:618–630. doi: 10.2106/00004623-199805000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Herrera A, Domingo LJ, Calvo A, Martinez A. A comparative study of trochanteric fractures treated with the Gamma nail or the proximal femoral nail. Int Orthop. 2002;26:364–369. doi: 10.1007/s00264-002-0389-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kuenhn BM. Better osteoporosis management, a priority. JAMA. 2005;293:2453–2458. doi: 10.1001/jama.293.20.2453. [DOI] [PubMed] [Google Scholar]
- 11.Landolt M. Comparison and presentation of technique and results of the gamma nail and dynamic hip screw. Helv Chir Acta. 1993;59:965–969. [PubMed] [Google Scholar]
- 12.Leung KS, So WS, Shen WY, Hui PQ. Gamma nails and dynamic hip screw for peritrochanteric fractures: a randomised prospective study in elderly patients. J Bone Joint Surg. 1992;74B:345–351. doi: 10.1302/0301-620X.74B3.1587874. [DOI] [PubMed] [Google Scholar]
- 13.Lichtblau S. Treatment of hip fractures in the elderly. The decision process. The Mount Sinai J of Med. 2002;69(4):250–260. [PubMed] [Google Scholar]
- 14.Lorich DG, Geller DS, Nielson JH. Osteoporotic pertrochanteric hip fractures. J Bone Joint Surg. 2004;86A(2):398–410. [PubMed] [Google Scholar]
- 15.Müller ME, Nazarian S, Koch P, editors. Classification AO des fractures. Berlin Heidelberg New York: Springer; 1987. [Google Scholar]
- 16.Parker MJ, Pryor GA. Gamma nail versus DHS nailing for extracapsular femoral fractures. Meta-analysis of ten randomised trials. Int Orthop. 1996;20:163–168. doi: 10.1007/s002640050055. [DOI] [PubMed] [Google Scholar]
- 17.Radford PJ, Neeedoff M, Webb JK. A prospective randomised comparison of the dynamic hip screw and the gamma locking nail. J Bone Joint Surg. 1993;75B:789–793. doi: 10.1302/0301-620X.75B5.8376441. [DOI] [PubMed] [Google Scholar]
- 18.Rosenblum SF, Zuckerman JD, Kummer FJ, Tom BSA. Biomechanical evaluation of the gamma nail. J Bone Joint Surg. 1992;74B:352–357. doi: 10.1302/0301-620X.74B3.1587875. [DOI] [PubMed] [Google Scholar]
- 19.Simmermacher RKJ, Bosch AM, Werken CHR. The AO/ASIF proximal femoral nail (PFN): a new device for the treatment of unstable femoral fractures. Injury. 1999;30:327–332. doi: 10.1016/S0020-1383(99)00091-1. [DOI] [PubMed] [Google Scholar]
- 20.Singh M, Nagrath AR, MAINI PS. Changes in the trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg. 1970;52A:457–467. [PubMed] [Google Scholar]
- 21.Wallace WA. The increasing incidence of fractures of the proximal femur: an orthopaedic epidemic. Lancet. 1983;i:1413–1414. doi: 10.1016/S0140-6736(83)92358-9. [DOI] [PubMed] [Google Scholar]
- 22.Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg. 1995;77A:1551–1556. doi: 10.2106/00004623-199510000-00010. [DOI] [PubMed] [Google Scholar]